Propranolol
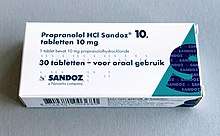
Propranolol, sold under the brand name Inderal among others, is a medication of the beta blocker class.[1] It is used to treat high blood pressure, a number of types of irregular heart rate, thyrotoxicosis, capillary hemangiomas, performance anxiety, and essential tremors.[1][2][3] It is used to prevent migraine headaches, and to prevent further heart problems in those with angina or previous heart attacks.[1] It can be taken by mouth or by injection into a vein.[1] The formulation that is taken by mouth comes in short-acting and long-acting versions.[1] Propranolol appears in the blood after 30 minutes and has a maximum effect between 60 and 90 minutes when taken by mouth.[1][4]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | prəʊˈpranəlɒl |
| Trade names | Inderal, others |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth, rectal, intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 26% |
| Protein binding | 90% |
| Metabolism | Liver (extensive) 1A2, 2D6; minor: 2C19, 3A4 |
| Metabolites | N-desisopropylpropranolol, 4'-hydroxypropanolol |
| Elimination half-life | 4–5 hours |
| Excretion | Kidney (<1%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.007.618 |
| Chemical and physical data | |
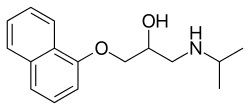
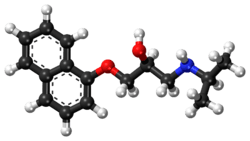
| Formula | C16H21NO2 |
| Molar mass | 259.349 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Melting point | 96 °C (205 °F) |
| |
| |
| (verify) | |
Common side effects include nausea, abdominal pain, and constipation.[1] It should not be used in those with an already slow heart rate and most of those with heart failure.[1] Quickly stopping the medication in those with coronary artery disease may worsen symptoms.[1] It may worsen the symptoms of asthma.[1] Caution is recommended in those with liver or kidney problems.[1] Propranolol may cause harmful effects in the baby if taken during pregnancy.[5] Its use during breastfeeding is probably safe, but the baby should be monitored for side effects.[6] It is a non-selective beta blocker which works by blocking β-adrenergic receptors.[1]
Propranolol was patented in 1962 and approved for medical use in 1964.[7] It is on the World Health Organization's List of Essential Medicines.[8] Propranolol is available as a generic medication.[1] In 2017, it was the 41st most commonly prescribed medication in the United States, with more than 17 million prescriptions.[9][10]
Medical uses


Propranolol is used for treating various conditions, including:
Cardiovascular
- Hypertension
- Angina pectoris (with the exception of variant angina)
- Myocardial infarction
- Tachycardia (and other sympathetic nervous system symptoms, such as muscle tremor) associated with various conditions, including anxiety, panic, hyperthyroidism, and lithium therapy
- Portal hypertension, to lower portal vein pressure
- Prevention of esophageal variceal bleeding and ascites
- Anxiety
- Hypertrophic cardiomyopathy
While once a first-line treatment for hypertension, the role for beta blockers was downgraded in June 2006 in the United Kingdom to fourth-line, as they do not perform as well as other drugs, particularly in the elderly, and evidence is increasing that the most frequently used beta blockers at usual doses carry an unacceptable risk of provoking type 2 diabetes.[11]
Propranolol is not recommended for the treatment of high blood pressure by the Eighth Joint National Committee (JNC 8) because a higher rate of the primary composite outcome of cardiovascular death, myocardial infarction, or stroke compared to an angiotensin receptor blocker was noted in one study.[12]
Psychiatric
Propranolol is occasionally used to treat performance anxiety,[2] although evidence to support its use in any anxiety disorders is poor.[13] Its benefits appear similar to benzodiazepines in panic disorder with potentially fewer side effects such as addiction.[13] Some experimentation has been conducted in other psychiatric areas:[14]
- Post-traumatic stress disorder (PTSD) and specific phobias (see subsection below)
- Aggressive behavior of patients with brain injuries[15]
- Treating the excessive drinking of fluids in psychogenic polydipsia[16][17]
PTSD and phobias
Propranolol is being investigated as a potential treatment for PTSD.[18][19] Propranolol works to inhibit the actions of norepinephrine, a neurotransmitter that enhances memory consolidation. In one small study individuals given propranolol immediately after trauma experienced fewer stress-related symptoms and lower rates of PTSD than respective control groups who did not receive the drug.[20] Due to the fact that memories and their emotional content are reconsolidated in the hours after they are recalled/re-experienced, propranolol can also diminish the emotional impact of already formed memories; for this reason, it is also being studied in the treatment of specific phobias, such as arachnophobia, dental fear, and social phobia.[13]
Ethical and legal questions have been raised surrounding the use of propranolol-based medications for use as a "memory damper", including: altering memory-recalled evidence during an investigation, modifying behavioral response to past (albeit traumatic) experiences, the regulation of these drugs, and others.[21] However, Hall and Carter have argued that many such objections are "based on wildly exaggerated and unrealistic scenarios that ignore the limited action of propranolol in affecting memory, underplay the debilitating impact that PTSD has on those who suffer from it, and fail to acknowledge the extent to which drugs like alcohol are already used for this purpose."[22]
Others
- Essential tremor. Evidence for use for akathisia however is insufficient[23]
- Migraine and cluster headache prevention[24][25] and in primary exertional headache[26]
- Hyperhidrosis (excessive sweating)
- Proliferating infantile hemangioma
- Glaucoma
- Thyrotoxicosis by deiodinase inhibition
Propranolol may be used to treat severe infantile hemangiomas (IHs). This treatment shows promise as being superior to corticosteroids when treating IHs. Extensive clinical case evidence and a small controlled trial support its efficacy.[27]
Contraindications
Propranolol may be contraindicated in people with:[28]
- Reversible airway diseases, particularly asthma or chronic obstructive pulmonary disease (COPD)
- Slow heart rate (bradycardia) (<60 beats/minute)
- Sick sinus syndrome
- Atrioventricular block (second- or third-degree)
- Shock
- Severe low blood pressure
- Cocaine toxicity
Adverse effects
Propranolol should be used with caution in people with:[28]
- Diabetes mellitus or hyperthyroidism, since signs and symptoms of hypoglycaemia may be masked
- Peripheral artery disease and Raynaud's syndrome, which may be exacerbated
- Phaeochromocytoma, as hypertension may be aggravated without prior alpha blocker therapy
- Myasthenia gravis, which may be worsened
- Other drugs with bradycardic effects
Pregnancy and lactation
Propranolol, like other beta blockers, is classified as pregnancy category C in the United States and ADEC category C in Australia. β-blocking agents in general reduce perfusion of the placenta, which may lead to adverse outcomes for the neonate, including lung or heart complications, or premature birth. The newborn may experience additional adverse effects such as low blood sugar and a slower than normal heart rate.[29]
Most β-blocking agents appear in the milk of lactating women. However, propranolol is highly bound to proteins in the bloodstream and is distributed into breast milk at very low levels.[30] These low levels are not expected to pose any risk to the breastfeeding infant, and the American Academy of Pediatrics considers propranolol therapy "generally compatible with breastfeeding".[29][30][31][32]
Overdose
In overdose propranolol is associated with seizures.[33] Cardiac arrest may occur in propranolol overdose due to sudden ventricular arrhythmias, or cardiogenic shock which may ultimately culminate in bradycardic PEA.[34]
Interactions
Since beta blockers are known to relax the cardiac muscle and to constrict the smooth muscle, beta-adrenergic antagonists, including propranolol, have an additive effect with other drugs which decrease blood pressure, or which decrease cardiac contractility or conductivity. Clinically significant interactions particularly occur with:[28]
- Verapamil
- Epinephrine (adrenaline)
- β2-adrenergic receptor agonists
- Clonidine
- Ergot alkaloids
- Isoprenaline (isoproterenol)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Quinidine
- Cimetidine
- Lidocaine
- Phenobarbital
- Rifampicin
- Fluvoxamine (slows down the metabolism of propranolol significantly, leading to increased blood levels of propranolol)[35]
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| 5-HT1A | 55–272 | Human | [37][38] |
| 5-HT1B | 56–85 | Rat | [39][40] |
| 5-HT1D | 4,070 | Pig | [41] |
| 5-HT2A | 4,280 | Human | [42] |
| 5-HT2B | 457–513 (+) 166–316 (–) | Human | [43] |
| 5-HT2C | 61,700 (+) 5,010 (–) 736–2,457 | Human Human Rodent | [43] [43] [44][38] |
| 5-HT3 | >10,000 | Human | [45] |
| α1 | ND | ND | ND |
| α2 | 1,297–2,789 | Rat | [46] |
| β1 | 0.02–2.69 | Human | [47][48] |
| β2 | 0.01–0.61 | Human | [47][48] |
| β3 | 450 | Mouse | [49] |
| D1 | >10,000 | Human | [38] |
| D2 | >10,000 | Human | [38] |
| H1 | >10,000 | Human | [50] |
| SERT | 3,700 | Rat | [51] |
| NET | 5,000 (IC50) | Rat | [52] |
| DAT | 29,000 (IC50) | Rat | [52] |
| VDCC | >10,000 | Rat | [53] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | |||
Propranolol is classified as a competitive non-cardioselective sympatholytic beta blocker that crosses the blood–brain barrier. It is lipid soluble and also has sodium channel blocking effects. Propranolol is a non-selective β-adrenergic receptor antagonist, or beta blocker;[54] that is, it blocks the action of epinephrine (adrenaline) and norepinephrine (noradrenaline) at both β1- and β2-adrenergic receptors. It has little intrinsic sympathomimetic activity, but has strong membrane stabilizing activity (only at high blood concentrations, e.g. overdose).[55] Propranolol is able to cross the blood–brain barrier and exert effects in the central nervous system in addition to its peripheral activity.[13]
In addition to blockade of adrenergic receptors, propranolol has very weak inhibitory effects on the norepinephrine transporter and/or weakly stimulates norepinephrine release (i.e., the concentration of norepinephrine is increased in the synapse).[56][52] Since propranolol blocks β-adrenoceptors, the increase in synaptic norepinephrine only results in α-adrenoceptor activation, with the α1-adrenoceptor being particularly important for effects observed in animal models.[56][52] Therefore, it can be looked upon as a weak indirect α1-adrenoceptor agonist in addition to potent β-adrenoceptor antagonist.[56][52] In addition to its effects on the adrenergic system, there is evidence that indicates that propranolol may act as a weak antagonist of certain serotonin receptors, namely the 5-HT1A, 5-HT1B, and 5-HT2B receptors.[57][58][43] The latter may be involved in the effectiveness of propranolol in the treatment of migraine at high doses.[43]
Both enantiomers of propranolol have a local anesthetic (topical) effect, which is normally mediated by blockade of voltage-gated sodium channels. Studies have demonstrated propranolol's ability to block cardiac, neuronal, and skeletal voltage-gated sodium channels, accounting for its known membrane stabilizing effect and antiarrhythmic and other central nervous system effects.[59][60][61]
Mechanism of action
Propranolol is a non-selective beta receptor antagonist.[54] It competes with sympathomimetic neurotransmitters for binding to receptors, which inhibits sympathetic stimulation of the heart. Blockage of neurotransmitter binding to beta 1 receptors on cardiac myocytes inhibits activation of adenylate cyclase, which in turn inhibits cAMP synthesis leading to reduced PKA activation. This results in less calcium influx to cardiac myocytes through voltage gated L-type calcium channels meaning there is a decreased sympathetic effect on cardiac cells, resulting in antihypertensive effects including reduced heart rate and lower arterial blood pressure.[62]
Pharmacokinetics
Propranolol is rapidly and completely absorbed, with peak plasma levels achieved about 1–3 hours after ingestion. More than 90% of the drug is found bound to plasma protein in the blood.[62] Coadministration with food appears to enhance bioavailability.[63] Despite complete absorption, propranolol has a variable bioavailability due to extensive first-pass metabolism. Hepatic impairment therefore increases its bioavailability. The main metabolite 4-hydroxypropranolol, with a longer half-life (5.2–7.5 hours) than the parent compound (3–4 hours), is also pharmacologically active. Most of the metabolites are excreted in the urine.[62]
Propranolol is a highly lipophilic drug achieving high concentrations in the brain. The duration of action of a single oral dose is longer than the half-life and may be up to 12 hours, if the single dose is high enough (e.g., 80 mg).[64] Effective plasma concentrations are between 10 and 100 mg/l. Toxic levels are associated with plasma concentrations above 2000 mg/l.
History
British scientist James W. Black developed propranolol in the 1960s.[65] It was the first beta-blocker effectively used in the treatment of coronary artery disease and hypertension.[66] In 1988, Black was awarded the Nobel Prize in Medicine for this discovery. Propranolol was inspired by the early β-adrenergic antagonists dichloroisoprenaline and pronethalol. The key difference, which was carried through to essentially all subsequent beta blockers, was the inclusion of an oxymethylene group (-O-CH2-) between the aryl and ethanolamine moieties of pronethalol, greatly increasing the potency of the compound. This also apparently eliminated the carcinogenicity found with pronethalol in animal models.
Newer, more cardio-selective beta blockers (such as bisoprolol, nebivolol, carvedilol, or metoprolol) are now used preferentially in the treatment of hypertension.[66]
Society and culture
In a 1987 study by the International Conference of Symphony and Opera Musicians, it was shown that 27% of interviewed members admitted to using beta blockers such as propranolol for musical performances.[67] For about 10–16% of performers, their degree of stage fright is considered pathological.[67][68] Propranolol is used by musicians, actors, and public speakers for its ability to treat anxiety symptoms activated by the sympathetic nervous system.[69] It has also been used as a performance-enhancing drug in sports where high accuracy is required, including archery, shooting, golf[70] and snooker.[70] In the 2008 Summer Olympics, 50-metre pistol silver medalist and 10-metre air pistol bronze medalist Kim Jong-su tested positive for propranolol and was stripped of his medals.[71]
Brand names
Original propranolol was marketed in 1965, under the brand name Inderal and manufactured by ICI Pharmaceuticals (now AstraZeneca). Propranolol is also marketed under brand names Avlocardyl, Deralin, Dociton, Inderalici, InnoPran XL, Sumial, Anaprilin, and Bedranol SR (Sandoz). In India it is marketed under brand names such as Ciplar and Ciplar LA by Cipla. Hemangeol, a 4.28 mg/mL solution of propranolol, is indicated for the treatment of proliferating infantile hemangioma.[72]
References
- "Propranolol hydrochloride". Monograph. The American Society of Health-System Pharmacists. Archived from the original on 1 January 2015. Retrieved 1 January 2015.
- Davidson JR (2006). "Pharmacotherapy of social anxiety disorder: what does the evidence tell us?". The Journal of Clinical Psychiatry. 67 Suppl 12: 20–6. doi:10.1016/j.genhosppsych.2005.07.002. PMID 17092192.
- Chinnadurai S, Fonnesbeck C, Snyder KM, Sathe NA, Morad A, Likis FE, McPheeters ML (February 2016). "Pharmacologic Interventions for Infantile Hemangioma: A Meta-analysis" (PDF). Pediatrics. 137 (2): e20153896. doi:10.1542/peds.2015-3896. PMID 26772662.
- Bryson PD (1997). Comprehensive review in toxicology for emergency clinicians (3 ed.). Washington, DC: Taylor & Francis. p. 167. ISBN 9781560326120. Archived from the original on 24 March 2017.
- "Prescribing medicines in pregnancy database". Australian Government. 3 March 2014. Archived from the original on 8 April 2014. Retrieved 22 April 2014.
- Briggs GG, Freeman RK, Yaffe SJ (2011). Drugs in pregnancy and lactation : a reference guide to fetal and neonatal risk (9th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1226. ISBN 9781608317080. Archived from the original on 14 February 2017.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 460. ISBN 9783527607495.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Propranolol Hydrochloride - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Ladva S (28 June 2006). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Archived from the original on 24 September 2006. Retrieved 11 October 2009.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. (February 2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- Steenen SA, van Wijk AJ, van der Heijden GJ, van Westrhenen R, de Lange J, de Jongh A (February 2016). "Propranolol for the treatment of anxiety disorders: Systematic review and meta-analysis". Journal of Psychopharmacology. 30 (2): 128–39. doi:10.1177/0269881115612236. PMC 4724794. PMID 26487439.
- Kornischka J, Cordes J, Agelink MW (April 2007). "[40 years beta-adrenoceptor blockers in psychiatry]". Fortschritte der Neurologie-Psychiatrie (in German). 75 (4): 199–210. doi:10.1055/s-2006-944295. PMID 17200914.
- Thibaut F, Colonna L (1993). "[Anti-aggressive effect of beta-blockers]". L'Encephale (in French). 19 (3): 263–7. PMID 7903928.
- Vieweg V, Pandurangi A, Levenson J, Silverman J (1994). "The consulting psychiatrist and the polydipsia-hyponatremia syndrome in schizophrenia". International Journal of Psychiatry in Medicine. 24 (4): 275–303. doi:10.2190/5WG5-VV1V-BXAD-805K. PMID 7737786.
- Kishi Y, Kurosawa H, Endo S (1998). "Is propranolol effective in primary polydipsia?". International Journal of Psychiatry in Medicine. 28 (3): 315–25. doi:10.2190/QPWL-14H7-HPGG-A29D. PMID 9844835.
- "Doctors test a drug to ease traumatic memories - Mental Health - NBC News". Retrieved 30 June 2007.
- Brunet A, Orr SP, Tremblay J, Robertson K, Nader K, Pitman RK (May 2008). "Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder". Journal of Psychiatric Research. 42 (6): 503–6. doi:10.1016/j.jpsychires.2007.05.006. PMID 17588604.
- Vaiva G, Ducrocq F, Jezequel K, Averland B, Lestavel P, Brunet A, Marmar CR (November 2003). "Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma". Biological Psychiatry. 54 (9): 947–9. doi:10.1016/s0006-3223(03)00412-8. PMID 14573324.
- Kolber AJ (2006). "Therapeutic Forgetting: The Legal and Ethical Implications of Memory Dampening". Vanderbilt Law Review, San Diego Legal Studies Paper No. 07-37. 59: 1561.
- Hall W, Carter A (September 2007). "Debunking alarmist objections to the pharmacological prevention of PTSD". The American Journal of Bioethics. 7 (9): 23–5. doi:10.1080/15265160701551244. PMID 17849333.
- Lima AR, Bacalcthuk J, Barnes TR, Soares-Weiser K (October 2004). "Central action beta-blockers versus placebo for neuroleptic-induced acute akathisia". The Cochrane Database of Systematic Reviews (4): CD001946. doi:10.1002/14651858.CD001946.pub2. PMC 6599862. PMID 15495022.
- Shields KG, Goadsby PJ (January 2005). "Propranolol modulates trigeminovascular responses in thalamic ventroposteromedial nucleus: a role in migraine?". Brain. 128 (Pt 1): 86–97. doi:10.1093/brain/awh298. PMID 15574468.
- Eadie M, Tyrer JH (1985). The Biochemistry of Migraine. New York: Springer. p. 148. ISBN 9780852007310. OCLC 11726870. Archived from the original on 24 March 2017.
- Clinical summary Archived 24 March 2008 at the Wayback Machine
- Hogeling, M. (2012). "Propranolol for Infantile Hemangiomas: A Review". Current Dermatology Reports. 1 (4): Online-first. doi:10.1007/s13671-012-0026-6.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006.
- Sweetman SC, ed. (2009). "Cardiovascular Drugs". Martindale: The complete drug reference (36th ed.). London: Pharmaceutical Press. pp. 1226–1381. ISBN 978-0-85369-840-1.
- [No authors listed] (2007). "Propranolol". In: Drugs and Lactation Database. U.S. National Library of Medicine Toxicology Data Network. Retrieved 25 February 2013.
- American Academy of Pediatrics Committee on Drugs (September 2001). "Transfer of drugs and other chemicals into human milk". Pediatrics. 108 (3): 776–89. doi:10.1542/peds.108.3.776. PMID 11533352.
- Spencer JP, Gonzalez LS, Barnhart DJ (July 2001). "Medications in the breast-feeding mother". American Family Physician. 64 (1): 119–26. PMID 11456429.
- Reith DM, Dawson AH, Epid D, Whyte IM, Buckley NA, Sayer GP (1996). "Relative toxicity of beta blockers in overdose". Journal of Toxicology. Clinical Toxicology. 34 (3): 273–8. doi:10.3109/15563659609013789. PMID 8667464.
- Holstege CP, Eldridge DL, Rowden AK (February 2006). "ECG manifestations: the poisoned patient". Emergency Medicine Clinics of North America. 24 (1): 159–77, vii. doi:10.1016/j.emc.2005.08.012. PMID 16308118.
- van Harten J (1995). "Overview of the pharmacokinetics of fluvoxamine". Clinical Pharmacokinetics. 29 Suppl 1 (Suppl 1): 1–9. doi:10.2165/00003088-199500291-00003. PMID 8846617.
- Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- Hamon M, Lanfumey L, el Mestikawy S, Boni C, Miquel MC, Bolaños F, et al. (1990). "The main features of central 5-HT1 receptors". Neuropsychopharmacology. 3 (5–6): 349–60. PMID 2078271.
- Toll L, Berzetei-Gurske IP, Polgar WE, Brandt SR, Adapa ID, Rodriguez L, et al. (March 1998). "Standard binding and functional assays related to medications development division testing for potential cocaine and opiate narcotic treatment medications". NIDA Research Monograph. 178: 440–66. PMID 9686407.
- Tsuchihashi H, Nakashima Y, Kinami J, Nagatomo T (February 1990). "Characteristics of 125I-iodocyanopindolol binding to beta-adrenergic and serotonin-1B receptors of rat brain: selectivity of beta-adrenergic agents". Japanese Journal of Pharmacology. 52 (2): 195–200. doi:10.1254/jjp.52.195. PMID 1968985.
- Engel G, Göthert M, Hoyer D, Schlicker E, Hillenbrand K (January 1986). "Identity of inhibitory presynaptic 5-hydroxytryptamine (5-HT) autoreceptors in the rat brain cortex with 5-HT1B binding sites". Naunyn-Schmiedeberg's Archives of Pharmacology. 332 (1): 1–7. doi:10.1007/bf00633189. PMID 2936965.
- Schlicker E, Fink K, Göthert M, Hoyer D, Molderings G, Roschke I, Schoeffter P (July 1989). "The pharmacological properties of the presynaptic serotonin autoreceptor in the pig brain cortex conform to the 5-HT1D receptor subtype". Naunyn-Schmiedeberg's Archives of Pharmacology. 340 (1): 45–51. doi:10.1007/bf00169206. PMID 2797214.
- Elliott JM, Kent A (July 1989). "Comparison of [125I]iodolysergic acid diethylamide binding in human frontal cortex and platelet tissue". Journal of Neurochemistry. 53 (1): 191–6. doi:10.1111/j.1471-4159.1989.tb07313.x. PMID 2723656.
- Schmuck K, Ullmer C, Kalkman HO, Probst A, Lubbert H (May 1996). "Activation of meningeal 5-HT2B receptors: an early step in the generation of migraine headache?". The European Journal of Neuroscience. 8 (5): 959–67. doi:10.1111/j.1460-9568.1996.tb01583.x. PMID 8743744.
- Yagaloff KA, Hartig PR (December 1985). "125I-lysergic acid diethylamide binds to a novel serotonergic site on rat choroid plexus epithelial cells". The Journal of Neuroscience. 5 (12): 3178–83. doi:10.1523/JNEUROSCI.05-12-03178.1985. PMC 6565215. PMID 4078623.
- Barnes JM, Barnes NM, Costall B, Ironside JW, Naylor RJ (December 1989). "Identification and characterisation of 5-hydroxytryptamine 3 recognition sites in human brain tissue". Journal of Neurochemistry. 53 (6): 1787–93. doi:10.1111/j.1471-4159.1989.tb09244.x. PMID 2809591.
- Boyajian CL, Leslie FM (June 1987). "Pharmacological evidence for alpha-2 adrenoceptor heterogeneity: differential binding properties of [3H]rauwolscine and [3H]idazoxan in rat brain". The Journal of Pharmacology and Experimental Therapeutics. 241 (3): 1092–8. PMID 2885406.
- Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS, et al. (March 1996). "Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding". Psychopharmacology. 124 (1–2): 57–73. doi:10.1007/bf02245606. PMID 8935801.
- Fraundorfer PF, Fertel RH, Miller DD, Feller DR (August 1994). "Biochemical and pharmacological characterization of high-affinity trimetoquinol analogs on guinea pig and human beta adrenergic receptor subtypes: evidence for partial agonism". The Journal of Pharmacology and Experimental Therapeutics. 270 (2): 665–74. PMID 7915318.
- Nahmias C, Blin N, Elalouf JM, Mattei MG, Strosberg AD, Emorine LJ (December 1991). "Molecular characterization of the mouse beta 3-adrenergic receptor: relationship with the atypical receptor of adipocytes". The EMBO Journal. 10 (12): 3721–7. doi:10.1002/j.1460-2075.1991.tb04940.x. PMC 453106. PMID 1718744.
- Kanba S, Richelson E (June 1984). "Histamine H1 receptors in human brain labelled with [3H]doxepin". Brain Research. 304 (1): 1–7. doi:10.1016/0006-8993(84)90856-4. PMID 6146381.
- Kovachich GB, Aronson CE, Brunswick DJ, Frazer A (June 1988). "Quantitative autoradiography of serotonin uptake sites in rat brain using [3H]cyanoimipramine". Brain Research. 454 (1–2): 78–88. doi:10.1016/0006-8993(88)90805-0. PMID 2970277.
- Tuross N, Patrick RL (June 1986). "Effects of propranolol on catecholamine synthesis and uptake in the central nervous system of the rat". The Journal of Pharmacology and Experimental Therapeutics. 237 (3): 739–45. PMID 2872325.
- Zobrist RH, Mecca TE (May 1990). "[3H]TA-3090, a selective benzothiazepine-type calcium channel receptor antagonist: in vitro characterization". The Journal of Pharmacology and Experimental Therapeutics. 253 (2): 461–5. PMID 2338642.
- Al-Majed AA, Bakheit AH, Abdel Aziz HA, Alajmi FM, AlRabiah H (2017). "Propranolol". Profiles of Drug Substances, Excipients, and Related Methodology. 42: 287–338. doi:10.1016/bs.podrm.2017.02.006. ISBN 9780128122266. PMID 28431779.
- Naish J, Court DS (2014). Medical sciences (Second ed.). p. 150. ISBN 978-0702052491.
- Young R, Glennon RA (April 2009). "S(-)Propranolol as a discriminative stimulus and its comparison to the stimulus effects of cocaine in rats". Psychopharmacology. 203 (2): 369–82. doi:10.1007/s00213-008-1317-2. PMID 18795268.
- Davids E, Lesch KP (November 1996). "[The 5-HT1A receptor: a new effective principle in psychopharmacologic therapy?]". Fortschritte der Neurologie-Psychiatrie (in German). 64 (11): 460–72. doi:10.1055/s-2007-996592. PMID 9064274.
- Hoyer D, Clarke DE, Fozard JR, Hartig PR, Martin GR, Mylecharane EJ, et al. (June 1994). "International Union of Pharmacology classification of receptors for 5-hydroxytryptamine (Serotonin)". Pharmacological Reviews. 46 (2): 157–203. PMID 7938165.
- Wang DW, Mistry AM, Kahlig KM, Kearney JA, Xiang J, George AL (2010). "Propranolol blocks cardiac and neuronal voltage-gated sodium channels". Frontiers in Pharmacology. 1: 144. doi:10.3389/fphar.2010.00144. PMC 3153018. PMID 21833183.
- Bankston JR, Kass RS (January 2010). "Molecular determinants of local anesthetic action of beta-blocking drugs: Implications for therapeutic management of long QT syndrome variant 3". Journal of Molecular and Cellular Cardiology. 48 (1): 246–53. doi:10.1016/j.yjmcc.2009.05.012. PMC 2813422. PMID 19481549.
- Desaphy JF, Pierno S, De Luca A, Didonna P, Camerino DC (March 2003). "Different ability of clenbuterol and salbutamol to block sodium channels predicts their therapeutic use in muscle excitability disorders" (PDF). Molecular Pharmacology. 63 (3): 659–70. doi:10.1124/mol.63.3.659. PMID 12606775.
- "Propranolol". www.drugbank.ca. Retrieved 31 January 2019.
- Rang HP (2011). Rang & Dale's pharmacology (7th ed.). Edinburgh: Churchill Livingstone. p. 106. ISBN 9780702034718.
- "Propranolol". pubchem.ncbi.nlm.nih.gov. Retrieved 31 January 2019.
- Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC (May 1964). "A New Adrenergic". Lancet. 1 (7342): 1080–1. doi:10.1016/S0140-6736(64)91275-9. PMID 14132613.
- Benowitz NL (2017). "Antihypertensive Agents". In Katzung BG (ed.). Basic & Clinical Pharmacology (14th ed.). McGraw-Hill. ISBN 9781259641152.
- Fishbein M, Middlestadt SE, Ottati V, Straus S, Ellis A (1988). "Medical problems among ICSOM musicians: overview of a national survey". Med Probl Perform Artist. 3: 1–8.
- Steptoe A, Malik F, Pay C, Pearson P, Price C, Win Z (1995). "The impact of stage fright on student actors". Br J Psychol. 86: 27–39. doi:10.1111/j.2044-8295.1995.tb02544.x.
- Lockwood AH (January 1989). "Medical problems of musicians". The New England Journal of Medicine. 320 (4): 221–7. doi:10.1056/nejm198901263200405. PMID 2643048.
- Tim Glover. "Golf: O'Grady says players use beta-blockers: Drugs 'helped win majors'". The Independent. Archived from the original on September 25, 2015. Retrieved March 28, 2017.
- Scott M (15 August 2008). "Olympics: North Korea's Kim Jong-su loses medals after positive drugs test". The Guardian. Guardian News and Media Limited. Retrieved 7 March 2018.
- "Hemangeol - Food and Drug Administration" (PDF). 1 March 2014. Archived (PDF) from the original on 2 April 2015. Retrieved 23 March 2015.
External links
- Stapleton MP (1997). "Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology". Texas Heart Institute Journal. 24 (4): 336–42. PMC 325477. PMID 9456487.
- "Propranolol". Drug Information Portal. U.S. National Library of Medicine.