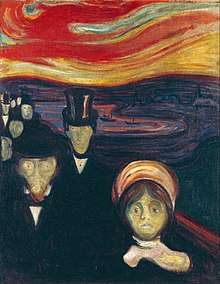
Anxiety
Anxiety is an emotion characterized by an unpleasant state of inner turmoil, often accompanied by nervous behavior such as pacing back and forth, somatic complaints, and rumination.[1] It is the subjectively unpleasant feelings of dread over anticipated events.[2]
Anxiety is a feeling of uneasiness and worry, usually generalized and unfocused as an overreaction to a situation that is only subjectively seen as menacing.[3] It is often accompanied by muscular tension,[4] restlessness, fatigue and problems in concentration. Anxiety is closely related to fear, which is a response to a real or perceived immediate threat; anxiety involves the expectation of future threat.[4] People facing anxiety may withdraw from situations which have provoked anxiety in the past.[5]
Anxiety disorders differ from developmentally normative fear or anxiety by being excessive or persisting beyond developmentally appropriate periods. They differ from transient fear or anxiety, often stress-induced, by being persistent (e.g., typically lasting 6 months or more), although the criterion for duration is intended as a general guide with allowance for some degree of flexibility and is sometimes of shorter duration in children.[4]
Anxiety vs. fear

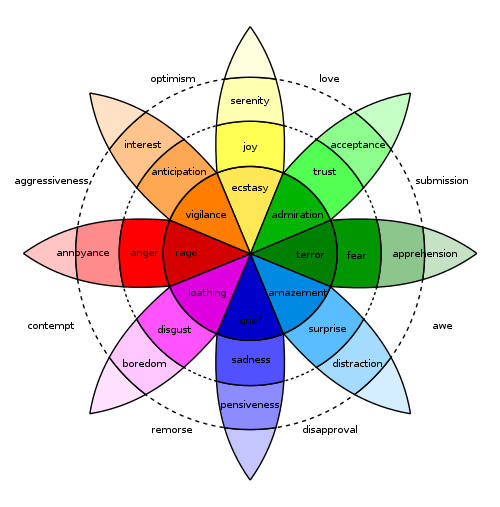
Anxiety is distinguished from fear, which is an appropriate cognitive and emotional response to a perceived threat.[6] Anxiety is related to the specific behaviors of fight-or-flight responses, defensive behavior or escape. It occurs in situations only perceived as uncontrollable or unavoidable, but not realistically so.[7] David Barlow defines anxiety as "a future-oriented mood state in which one is not ready or prepared to attempt to cope with upcoming negative events,"[8] and that it is a distinction between future and present dangers which divides anxiety and fear. Another description of anxiety is agony, dread, terror, or even apprehension.[9] In positive psychology, anxiety is described as the mental state that results from a difficult challenge for which the subject has insufficient coping skills.[10]
Fear and anxiety can be differentiated in four domains: (1) duration of emotional experience, (2) temporal focus, (3) specificity of the threat, and (4) motivated direction. Fear is short-lived, present-focused, geared towards a specific threat, and facilitating escape from threat; anxiety, on the other hand, is long-acting, future-focused, broadly focused towards a diffuse threat, and promoting excessive caution while approaching a potential threat and interferes with constructive coping.[11]
Joseph E. LeDoux and Lisa Feldman Barrett have both sought to separate automatic threat responses from additional associated cognitive activity within anxiety.[12][13]
Symptoms
Anxiety can be experienced with long, drawn-out daily symptoms that reduce quality of life, known as chronic (or generalized) anxiety, or it can be experienced in short spurts with sporadic, stressful panic attacks, known as acute anxiety.[14] Symptoms of anxiety can range in number, intensity, and frequency, depending on the person. While almost everyone has experienced anxiety at some point in their lives, most do not develop long-term problems with anxiety.
Anxiety may cause psychiatric and physiological symptoms.[15][16]
The risk of anxiety leading to depression could possibly even lead to an individual harming themselves, which is why there are many 24-hour suicide prevention hotlines.[17]
The behavioral effects of anxiety may include withdrawal from situations which have provoked anxiety or negative feelings in the past.[5] Other effects may include changes in sleeping patterns, changes in habits, increase or decrease in food intake, and increased motor tension (such as foot tapping).[5]
The emotional effects of anxiety may include "feelings of apprehension or dread, trouble concentrating, feeling tense or jumpy, anticipating the worst, irritability, restlessness, watching (and waiting) for signs (and occurrences) of danger, and, feeling like your mind's gone blank"[18] as well as "nightmares/bad dreams, obsessions about sensations, déjà vu, a trapped-in-your-mind feeling, and feeling like everything is scary."[19]
The cognitive effects of anxiety may include thoughts about suspected dangers, such as fear of dying. "You may ... fear that the chest pains are a deadly heart attack or that the shooting pains in your head are the result of a tumor or an aneurysm. You feel an intense fear when you think of dying, or you may think of it more often than normal, or can't get it out of your mind."[20]
The physiological symptoms of anxiety may include:[15][16]
- Neurological, as headache, paresthesias, fasciculations, vertigo, or presyncope.
- Digestive, as abdominal pain, nausea, diarrhea, indigestion, dry mouth, or bolus.
- Respiratory, as shortness of breath or sighing breathing.
- Cardiac, as palpitations, tachycardia, or chest pain.
- Muscular, as fatigue, tremors, or tetany.
- Cutaneous, as perspiration, or itchy skin.
- Uro-genital, as frequent urination, urinary urgency, dyspareunia, or impotence, chronic pelvic pain syndrome. Stress hormones released in an anxious state have an impact on bowel function and can manifest physical symptoms that may contribute to or exacerbate IBS.
Types
There are various types of anxiety. Existential anxiety can occur when a person faces angst, an existential crisis, or nihilistic feelings. People can also face mathematical anxiety, somatic anxiety, stage fright, or test anxiety. Social anxiety refers to a fear of rejection and negative evaluation by other people.[21]
Existential
The philosopher Søren Kierkegaard, in The Concept of Anxiety (1844), described anxiety or dread associated with the "dizziness of freedom" and suggested the possibility for positive resolution of anxiety through the self-conscious exercise of responsibility and choosing. In Art and Artist (1932), the psychologist Otto Rank wrote that the psychological trauma of birth was the pre-eminent human symbol of existential anxiety and encompasses the creative person's simultaneous fear of – and desire for – separation, individuation, and differentiation.
The theologian Paul Tillich characterized existential anxiety[22] as "the state in which a being is aware of its possible nonbeing" and he listed three categories for the nonbeing and resulting anxiety: ontic (fate and death), moral (guilt and condemnation), and spiritual (emptiness and meaninglessness). According to Tillich, the last of these three types of existential anxiety, i.e. spiritual anxiety, is predominant in modern times while the others were predominant in earlier periods. Tillich argues that this anxiety can be accepted as part of the human condition or it can be resisted but with negative consequences. In its pathological form, spiritual anxiety may tend to "drive the person toward the creation of certitude in systems of meaning which are supported by tradition and authority" even though such "undoubted certitude is not built on the rock of reality".[22]
According to Viktor Frankl, the author of Man's Search for Meaning, when a person is faced with extreme mortal dangers, the most basic of all human wishes is to find a meaning of life to combat the "trauma of nonbeing" as death is near.[23]
Depending on the source of the threat, psychoanalytic theory distinguishes the following types of anxiety:
- realistic
- neurotic
- moral[24]
Test and performance
According to Yerkes-Dodson law, an optimal level of arousal is necessary to best complete a task such as an exam, performance, or competitive event. However, when the anxiety or level of arousal exceeds that optimum, the result is a decline in performance.[25]
Test anxiety is the uneasiness, apprehension, or nervousness felt by students who have a fear of failing an exam. Students who have test anxiety may experience any of the following: the association of grades with personal worth; fear of embarrassment by a teacher; fear of alienation from parents or friends; time pressures; or feeling a loss of control. Sweating, dizziness, headaches, racing heartbeats, nausea, fidgeting, uncontrollable crying or laughing and drumming on a desk are all common. Because test anxiety hinges on fear of negative evaluation,[26] debate exists as to whether test anxiety is itself a unique anxiety disorder or whether it is a specific type of social phobia.[27] The DSM-IV classifies test anxiety as a type of social phobia.[28]
While the term "test anxiety" refers specifically to students,[29] many workers share the same experience with regard to their career or profession. The fear of failing at a task and being negatively evaluated for failure can have a similarly negative effect on the adult.[30] Management of test anxiety focuses on achieving relaxation and developing mechanisms to manage anxiety.[29]
Stranger, social, and intergroup anxiety
Humans generally require social acceptance and thus sometimes dread the disapproval of others. Apprehension of being judged by others may cause anxiety in social environments.[31]
Anxiety during social interactions, particularly between strangers, is common among young people. It may persist into adulthood and become social anxiety or social phobia. "Stranger anxiety" in small children is not considered a phobia. In adults, an excessive fear of other people is not a developmentally common stage; it is called social anxiety. According to Cutting,[32] social phobics do not fear the crowd but the fact that they may be judged negatively.
Social anxiety varies in degree and severity. For some people, it is characterized by experiencing discomfort or awkwardness during physical social contact (e.g. embracing, shaking hands, etc.), while in other cases it can lead to a fear of interacting with unfamiliar people altogether. Those suffering from this condition may restrict their lifestyles to accommodate the anxiety, minimizing social interaction whenever possible. Social anxiety also forms a core aspect of certain personality disorders, including avoidant personality disorder.[33]
To the extent that a person is fearful of social encounters with unfamiliar others, some people may experience anxiety particularly during interactions with outgroup members, or people who share different group memberships (i.e., by race, ethnicity, class, gender, etc.). Depending on the nature of the antecedent relations, cognitions, and situational factors, intergroup contact may be stressful and lead to feelings of anxiety. This apprehension or fear of contact with outgroup members is often called interracial or intergroup anxiety.[34]
As is the case the more generalized forms of social anxiety, intergroup anxiety has behavioral, cognitive, and affective effects. For instance, increases in schematic processing and simplified information processing can occur when anxiety is high. Indeed, such is consistent with related work on attentional bias in implicit memory.[35][36][37] Additionally recent research has found that implicit racial evaluations (i.e. automatic prejudiced attitudes) can be amplified during intergroup interaction.[38] Negative experiences have been illustrated in producing not only negative expectations, but also avoidant, or antagonistic, behavior such as hostility.[39] Furthermore, when compared to anxiety levels and cognitive effort (e.g., impression management and self-presentation) in intragroup contexts, levels and depletion of resources may be exacerbated in the intergroup situation.
Trait
Anxiety can be either a short-term 'state' or a long-term personality "trait". Trait anxiety reflects a stable tendency across the lifespan of responding with acute, state anxiety in the anticipation of threatening situations (whether they are actually deemed threatening or not).[40] A meta-analysis showed that a high level of neuroticism is a risk factor for development of anxiety symptoms and disorders.[41] Such anxiety may be conscious or unconscious.[42]
Personality can also be a trait leading to anxiety and depression. Through experience, many find it difficult to collect themselves due to their own personal nature.[43]
Choice or decision
Anxiety induced by the need to choose between similar options is increasingly being recognized as a problem for individuals and for organizations.[44] In 2004, Capgemini wrote: "Today we're all faced with greater choice, more competition and less time to consider our options or seek out the right advice."[45]
In a decision context, unpredictability or uncertainty may trigger emotional responses in anxious individuals that systematically alter decision-making.[46] There are primarily two forms of this anxiety type. The first form refers to a choice in which there are multiple potential outcomes with known or calculable probabilities. The second form refers to the uncertainty and ambiguity related to a decision context in which there are multiple possible outcomes with unknown probabilities.[46]
Panic Disorder
Panic disorder may share symptoms of stress and anxiety, but it is actually very different. Panic disorder is an anxiety disorder that occurs without any triggers. According to the U.S Department of Health and Human Services, this disorder can be distinguished by unexpected and repeated episodes of intense fear.[47] Someone who suffers from panic disorder will eventually develop constant fear of another attack and as this progresses it will begin to affect daily functioning and an individual's general quality of life. It is reported by the Cleveland Clinic that panic disorder affects 2 to 3 percent of adult Americans and can begin around the time of the teenage and early adult years. Some symptoms include: difficulty breathing, chest pain, dizziness, trembling or shaking, feeling faint, nausea, fear that you are losing control or are about to die. Even though they suffer from these symptoms during an attack, the main symptom is the persistent fear of having future panic attacks.[48]
Anxiety disorders
Anxiety disorders are a group of mental disorders characterized by exaggerated feelings of anxiety and fear responses.[49] Anxiety is a worry about future events and fear is a reaction to current events. These feelings may cause physical symptoms, such as a fast heart rate and shakiness. There are a number of anxiety disorders: including generalized anxiety disorder, specific phobia, social anxiety disorder, separation anxiety disorder, agoraphobia, panic disorder, and selective mutism. The disorder differs by what results in the symptoms. People often have more than one anxiety disorder.[49]
Anxiety disorders are caused by a complex combination of genetic and environmental factors. To be diagnosed, symptoms typically need to be present for at least six months, be more than would be expected for the situation, and decrease a person's ability to function in their daily lives. Other problems that may result in similar symptoms include hyperthyroidism, heart disease, caffeine, alcohol, or cannabis use, and withdrawal from certain drugs, among others.
Without treatment, anxiety disorders tend to remain.[49][50] Treatment may include lifestyle changes, counselling, and medications. Counselling is typically with a type of cognitive behavioural therapy.[51] Medications, such as antidepressants or beta blockers, may improve symptoms.[50]
About 12% of people are affected by an anxiety disorder in a given year and between 5–30% are affected at some point in their life.[51][52] They occur about twice as often in women than they do in men, and generally begin before the age of 25.[49][51] The most common are specific phobia which affects nearly 12% and social anxiety disorder which affects 10% at some point in their life. They affect those between the ages of 15 and 35 the most and become less common after the age of 55. Rates appear to be higher in the United States and Europe.[51]
Short- and long-term anxiety
Anxiety can be either a short-term "state" or a long-term "trait". Whereas trait anxiety represents worrying about future events, anxiety disorders are a group of mental disorders characterized by feelings of anxiety and fear.[49]
Co-morbidity
Anxiety disorders often occur with other mental health disorders, particularly major depressive disorder, bipolar disorder, eating disorders, or certain personality disorders. It also commonly occurs with personality traits such as neuroticism. This observed co-occurrence is partly due to genetic and environmental influences shared between these traits and anxiety.[53][54]
Anxiety is often experienced by those with obsessive–compulsive disorder and is an acute presence in panic disorder.
Risk factors
Anxiety disorders are partly genetic, with twin studies suggesting 30-40% genetic influence on individual differences in anxiety.[56] Environmental factors are also important. Twin studies show that individual-specific environments have a large influence on anxiety, whereas shared environmental influences (environments that affect twins in the same way) operate during childhood but decline through adolescence.[57] Specific measured ‘environments’ that have been associated with anxiety include child abuse, family history of mental health disorders, and poverty.[58] Anxiety is also associated with drug use, including alcohol, caffeine, and benzodiazepines (which are often prescribed to treat anxiety).
Neuroanatomy
Neural circuitry involving the amygdala (which regulates emotions like anxiety and fear, stimulating the HPA Axis and sympathetic nervous system) and hippocampus (which is implicated in emotional memory along with the amygdala) is thought to underlie anxiety.[59] People who have anxiety tend to show high activity in response to emotional stimuli in the amygdala.[60] Some writers believe that excessive anxiety can lead to an overpotentiation of the limbic system (which includes the amygdala and nucleus accumbens), giving increased future anxiety, but this does not appear to have been proven.[61][62]
Research upon adolescents who as infants had been highly apprehensive, vigilant, and fearful finds that their nucleus accumbens is more sensitive than that in other people when deciding to make an action that determined whether they received a reward.[63] This suggests a link between circuits responsible for fear and also reward in anxious people. As researchers note, "a sense of 'responsibility', or self-agency, in a context of uncertainty (probabilistic outcomes) drives the neural system underlying appetitive motivation (i.e., nucleus accumbens) more strongly in temperamentally inhibited than noninhibited adolescents".[63]
The gut-brain axis
The microbes of the gut can connect with the brain to affect anxiety. There are various pathways along which this communication can take place. One is through the major neurotransmitters.[64] The gut microbes such as Bifidobacterium and Bacillus produce the neurotransmitters GABA and dopamine, respectively.[65] The neurotransmitters signal to the nervous system of the gastrointestinal tract, and those signals will be carried to the brain through the vagus nerve or the spinal system.[64][65][66] This is demonstrated by the fact that altering the microbiome has shown anxiety- and depression-reducing effects in mice, but not in subjects without vagus nerves.[67]
Another key pathway is the HPA axis, as mentioned above.[66] The microbes can control the levels of cytokines in the body, and altering cytokine levels creates direct effects on areas of the brain such as the hypothalmus, the area that triggers HPA axis activity. The HPA axis regulates production of cortisol, a hormone that takes part in the body's stress response.[66] When HPA activity spikes, cortisol levels increase, processing and reducing anxiety in stressful situations. These pathways, as well as the specific effects of individual taxa of microbes, are not yet completely clear, but the communication between the gut microbiome and the brain is undeniable, as is the ability of these pathways to alter anxiety levels.
With this communication comes the potential to treat anxiety. Prebiotics and probiotics have been shown to reduced anxiety. For example, experiments in which mice were given fructo- and galacto-oligosaccharide prebiotics[68] and Lactobacillus probiotics[67] have both demonstrated a capability to reduce anxiety. In humans, results are not as concrete, but promising.[69][70]
Genetics
Genetics and family history (e.g. parental anxiety) may put an individual at increased risk of an anxiety disorder, but generally external stimuli will trigger its onset or exacerbation.[57] Estimates of genetic influence on anxiety, based on studies of twins, range from 25–40% depending on the specific type and age-group under study. For example, genetic differences account for about 43% of variance in panic disorder and 28% in generalized anxiety disorder. Longitudinal twin studies have shown the moderate stability of anxiety from childhood through to adulthood is mainly influenced by stability in genetic influence.[71][72] When investigating how anxiety is passed on from parents to children, it is important to account for sharing of genes as well as environments, for example using the intergenerational children-of-twins design.[73]
Many studies in the past used a candidate gene approach to test whether single genes were associated with anxiety. These investigations were based on hypotheses about how certain known genes influence neurotransmitters (such as serotonin and norepinephrine) and hormones (such as cortisol) that are implicated in anxiety. None of these findings are well replicated, with the possible exception of TMEM132D, COMT and MAO-A.[74] The epigenetic signature of BDNF, a gene that codes for a protein called brain derived neurotrophic factor that is found in the brain, has also been associated with anxiety and specific patterns of neural activity. and a receptor gene for BDNF called NTRK2 was associated with anxiety in a large genome-wide investigation.[75] The reason that most candidate gene findings have not replicated is that anxiety is a complex trait that is influenced by many genomic variants, each of which has a small effect on its own. Increasingly, studies of anxiety are using a hypothesis-free approach to look for parts of the genome that are implicated in anxiety using big enough samples to find associations with variants that have small effects. The largest explorations of the common genetic architecture of anxiety have been facilitated by the UK Biobank, the ANGST consortium and the CRC Fear, Anxiety and Anxiety Disorders.[75][76][77]
Medical conditions
Many medical conditions can cause anxiety. This includes conditions that affect the ability to breathe, like COPD and asthma, and the difficulty in breathing that often occurs near death.[78][79][80] Conditions that cause abdominal pain or chest pain can cause anxiety and may in some cases be a somatization of anxiety;[81][82] the same is true for some sexual dysfunctions.[83][84] Conditions that affect the face or the skin can cause social anxiety especially among adolescents,[85] and developmental disabilities often lead to social anxiety for children as well.[86] Life-threatening conditions like cancer also cause anxiety.[87]
Furthermore, certain organic diseases may present with anxiety or symptoms that mimic anxiety.[15][88] These disorders include certain endocrine diseases (hypo- and hyperthyroidism, hyperprolactinemia),[88][89] metabolic disorders (diabetes),[88][90][91] deficiency states (low levels of vitamin D, B2, B12, folic acid),[88] gastrointestinal diseases (celiac disease, non-celiac gluten sensitivity, inflammatory bowel disease),[92][93][94] heart diseases, blood diseases (anemia),[88] cerebral vascular accidents (transient ischemic attack, stroke),[88] and brain degenerative diseases (Parkinson's disease, dementia, multiple sclerosis, Huntington's disease), among others.[88][95][96][97]
Substance-induced
Several drugs can cause or worsen anxiety, whether in intoxication, withdrawal or as side effect. These include alcohol, tobacco, cannabis, sedatives (including prescription benzodiazepines), opioids (including prescription pain killers and illicit drugs like heroin), stimulants (such as caffeine, cocaine and amphetamines), hallucinogens, and inhalants.[98] While many often report self-medicating anxiety with these substances, improvements in anxiety from drugs are usually short-lived (with worsening of anxiety in the long term, sometimes with acute anxiety as soon as the drug effects wear off) and tend to be exaggerated. Acute exposure to toxic levels of benzene may cause euphoria, anxiety, and irritability lasting up to 2 weeks after the exposure.[99]
Psychological
Poor coping skills (e.g., rigidity/inflexible problem solving, denial, avoidance, impulsivity, extreme self-expectation, negative thoughts, affective instability, and inability to focus on problems) are associated with anxiety. Anxiety is also linked and perpetuated by the person's own pessimistic outcome expectancy and how they cope with feedback negativity.[100] Temperament (e.g., neuroticism)[41] and attitudes (e.g. pessimism) have been found to be risk factors for anxiety.[98][101]
Cognitive distortions such as overgeneralizing, catastrophizing, mind reading, emotional reasoning, binocular trick, and mental filter can result in anxiety. For example, an overgeneralized belief that something bad "always" happens may lead someone to have excessive fears of even minimally risky situations and to avoid benign social situations due to anticipatory anxiety of embarrassment. In addition, those who have high anxiety can also create future stressful life events.[102] Together, these findings suggest that anxious thoughts can lead to anticipatory anxiety as well as stressful events, which in turn cause more anxiety. Such unhealthy thoughts can be targets for successful treatment with cognitive therapy.
Psychodynamic theory posits that anxiety is often the result of opposing unconscious wishes or fears that manifest via maladaptive defense mechanisms (such as suppression, repression, anticipation, regression, somatization, passive aggression, dissociation) that develop to adapt to problems with early objects (e.g., caregivers) and empathic failures in childhood. For example, persistent parental discouragement of anger may result in repression/suppression of angry feelings which manifests as gastrointestinal distress (somatization) when provoked by another while the anger remains unconscious and outside the individual's awareness. Such conflicts can be targets for successful treatment with psychodynamic therapy. While psychodynamic therapy tends to explore the underlying roots of anxiety, cognitive behavioral therapy has also been shown to be a successful treatment for anxiety by altering irrational thoughts and unwanted behaviors.
Evolutionary psychology
An evolutionary psychology explanation is that increased anxiety serves the purpose of increased vigilance regarding potential threats in the environment as well as increased tendency to take proactive actions regarding such possible threats. This may cause false positive reactions but an individual suffering from anxiety may also avoid real threats. This may explain why anxious people are less likely to die due to accidents.[103]
When people are confronted with unpleasant and potentially harmful stimuli such as foul odors or tastes, PET-scans show increased blood flow in the amygdala.[104][105] In these studies, the participants also reported moderate anxiety. This might indicate that anxiety is a protective mechanism designed to prevent the organism from engaging in potentially harmful behaviors.
Social
Social risk factors for anxiety include a history of trauma (e.g., physical, sexual or emotional abuse or assault), bullying, early life experiences and parenting factors (e.g., rejection, lack of warmth, high hostility, harsh discipline, high parental negative affect, anxious childrearing, modelling of dysfunctional and drug-abusing behaviour, discouragement of emotions, poor socialization, poor attachment, and child abuse and neglect), cultural factors (e.g., stoic families/cultures, persecuted minorities including the disabled), and socioeconomics (e.g., uneducated, unemployed, impoverished although developed countries have higher rates of anxiety disorders than developing countries).[98][106] A 2019 comprehensive systematic review of over 50 studies showed that food insecurity in the United States is strongly associated with depression, anxiety, and sleep disorders.[107] Food-insecure individuals had an almost 3 fold risk increase of testing positive for anxiety when compared to food-secure individuals.
Gender socialization
Contextual factors that are thought to contribute to anxiety include gender socialization and learning experiences. In particular, learning mastery (the degree to which people perceive their lives to be under their own control) and instrumentality, which includes such traits as self-confidence, self-efficacy, independence, and competitiveness fully mediate the relation between gender and anxiety. That is, though gender differences in anxiety exist, with higher levels of anxiety in women compared to men, gender socialization and learning mastery explain these gender differences.[108]
Treatment
The first step in the management of a person with anxiety symptoms involves evaluating the possible presence of an underlying medical cause, whose recognition is essential in order to decide the correct treatment.[15][88] Anxiety symptoms may mask an organic disease, or appear associated with or as a result of a medical disorder.[15][88][109][16]
Cognitive behavioral therapy (CBT) is effective for anxiety disorders and is a first line treatment.[110][111][112][113][114] CBT appears to be equally effective when carried out via the internet.[114] While evidence for mental health apps is promising, it is preliminary.[115]
Psychopharmacological treatment can be used in parallel to CBT or can be used alone. As a general rule, most anxiety disorders respond well to first-line agents. First-line drugs are the selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors. Benzodiazepines are not recommended for routine use. Other treatment options include pregabalin, tricyclic antidepressants, buspirone, moclobemide, and others.[116]
Prevention
The above risk factors give natural avenues for prevention. A 2017 review found that psychological or educational interventions have a small yet statistically significant benefit for the prevention of anxiety in varied population types.[117][118][119]
Pathophysiology
Anxiety disorder appears to be a genetically inherited neurochemical dysfunction that may involve autonomic imbalance; decreased GABA-ergic tone; allelic polymorphism of the catechol-O-methyltransferase (COMT) gene; increased adenosine receptor function; increased cortisol.[120]
In the central nervous system (CNS), the major mediators of the symptoms of anxiety disorders appear to be norepinephrine, serotonin, dopamine, and gamma-aminobutyric acid (GABA). Other neurotransmitters and peptides, such as corticotropin-releasing factor, may be involved. Peripherally, the autonomic nervous system, especially the sympathetic nervous system, mediates many of the symptoms. Increased flow in the right parahippocampal region and reduced serotonin type 1A receptor binding in the anterior and posterior cingulate and raphe of patients are the diagnostic factors for prevalence of anxiety disorder.
The amygdala is central to the processing of fear and anxiety, and its function may be disrupted in anxiety disorders. Anxiety processing in the basolateral amygdala has been implicated with dendritic arborization of the amygdaloid neurons. SK2 potassium channels mediate inhibitory influence on action potentials and reduce arborization.[121]
See also
- List of people with an anxiety disorder – Wikipedia list article
- Angst – Intense feeling of apprehension, anxiety, or inner turmoil
- Fear – Basic emotion induced by a perceived threat
- Tripartite Model of Anxiety and Depression
- Uncanny
References
- Seligman ME, Walker EF, Rosenhan DL. Abnormal psychology (4th ed.). New York: W.W. Norton & Company.
- Davison GC (2008). Abnormal Psychology. Toronto: Veronica Visentin. p. 154. ISBN 978-0-470-84072-6.
- Bouras N, Holt G (2007). Psychiatric and Behavioral Disorders in Intellectual and Developmental Disabilities (2nd ed.). Cambridge University Press. ISBN 9781139461306.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (Fifth ed.). Arlington, VA: American Psychiatric Publishing. p. 189. ISBN 978-0-89042-555-8.
- Barker P (2003). Psychiatric and Mental Health Nursing: The Craft of Caring. London 0: Edward Arnold. ISBN 978-0-340-81026-2.CS1 maint: location (link)
- Andreas Dorschel, Furcht und Angst. In: Dietmar Goltschnigg (ed.), Angst. Lähmender Stillstand und Motor des Fortschritts. Stauffenburg, Tübingen 2012, pp. 49–54
- Öhman A (2000). "Fear and anxiety: Evolutionary, cognitive, and clinical perspectives". In Lewis M, Haviland-Jones JM (eds.). Handbook of emotions. New York: The Guilford Press. pp. 573–93. ISBN 978-1-57230-529-8.
- Barlow DH (November 2000). "Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory". The American Psychologist. 55 (11): 1247–63. doi:10.1037/0003-066X.55.11.1247. PMID 11280938.
- Iacovou, Susan (2011). "What is the difference between existential anxiety and so called neurotic anxiety? 'The sine qua non of true vitality' an examination of the difference between existential anxiety and neurotic anxiety". Existential Analysis. 22 (2). Gale A288874227.
- Csíkszentmihályi M (1997). Finding Flow.
- Sylvers P, Lilienfeld SO, LaPrairie JL (February 2011). "Differences between trait fear and trait anxiety: implications for psychopathology". Clinical Psychology Review. 31 (1): 122–37. doi:10.1016/j.cpr.2010.08.004. PMID 20817337.
- Emory, Margaret (June 7, 2018). "On Fear, Emotions, and Memory: An Interview with Dr. Joseph LeDoux". Brain World. Retrieved September 11, 2019.
- Barrett, Lisa Feldman (October 19, 2016). "The theory of constructed emotion: an active inference account of interoception and categorization". Social Cognitive and Affective Neuroscience. 12 (1): 1–23. doi:10.1093/scan/nsw154. PMC 5390700. PMID 27798257.
- Rynn MA, Brawman-Mintzer O (October 2004). "Generalized anxiety disorder: acute and chronic treatment". CNS Spectrums. 9 (10): 716–23. doi:10.1017/S1092852900022367. PMID 15448583.
- World Health Organization (2009). Pharmacological Treatment of Mental Disorders in Primary Health Care (PDF). Geneva. ISBN 978-92-4-154769-7. Archived (PDF) from the original on November 20, 2016.
- Testa A, Giannuzzi R, Sollazzo F, Petrongolo L, Bernardini L, Daini S (February 2013). "Psychiatric emergencies (part I): psychiatric disorders causing organic symptoms". European Review for Medical and Pharmacological Sciences. 17 Suppl 1: 55–64. PMID 23436668.

- "Depression Hotline | Call Our Free, 24 Hour Depression Helpline". PsychGuides.com. Retrieved October 11, 2018.
- Smith, Melinda (June 2008). Anxiety attacks and disorders: Guide to the signs, symptoms, and treatment options. Retrieved March 3, 2009, from Helpguide Web site: "HelpGuide.org". Archived from the original on March 7, 2009. Retrieved March 4, 2009.
- (1987–2008). Anxiety Symptoms, Anxiety Attack Symptoms (Panic Attack Symptoms), Symptoms of Anxiety. Retrieved March 3, 2009, from Anxiety Centre Website: "Anxiety Symptoms and Signs – over 100 listed". Archived from the original on March 7, 2009. Retrieved March 4, 2009.
- (1987–2008). Anxiety symptoms – Fear of dying. Retrieved March 3, 2009, from Anxiety Centre Website: "Fear of dying anxiety symptom". Archived from the original on March 5, 2009. Retrieved March 4, 2009.
- Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). American Psychiatric Association. ISBN 978-0890425558.
- Tillich P (1952). The Courage To Be. New Haven: Yale University Press. p. 76. ISBN 978-0-300-08471-9.
- Abulof U (2015). The Mortality and Morality of Nations. New York: Cambridge University Press. p. 26. ISBN 978-1-107-09707-0.
- Hjelle, Larry; Ziegler, Daniel (1981). Personality Theories: Basic Assumptions, Research, and Applications. McGraw-Hill. p. 494. ISBN 9780070290631.
- Teigen KH (1994). "Yerkes-Dodson: A Law for all Seasons". Theory & Psychology. 4 (4): 525–547. doi:10.1177/0959354394044004.
- Liebert RM, Morris LW (June 1967). "Cognitive and emotional components of test anxiety: a distinction and some initial data". Psychological Reports. 20 (3): 975–8. doi:10.2466/pr0.1967.20.3.975. PMID 6042522.
- Beidel DC, Turner SM (June 1988). "Comorbidity of test anxiety and other anxiety disorders in children". Journal of Abnormal Child Psychology. 16 (3): 275–87. doi:10.1007/BF00913800. PMID 3403811.
- Rapee RM, Heimberg RG (August 1997). "A cognitive-behavioral model of anxiety in social phobia". Behaviour Research and Therapy. 35 (8): 741–56. doi:10.1016/S0005-7967(97)00022-3. PMID 9256517.
- Mathur S, Khan W (2011). "Impact of Hypnotherapy on Examination Anxiety and Scholastic Performance among School" (PDF). Delhi Psychiatry Journal. 14 (2): 337–42. CiteSeerX 10.1.1.1027.7497.
- Hall-Flavin DK. "Is it possible to overcome test anxiety?". Mayo Clinic. Mayo Foundation for Medical Education and Research. Archived from the original on September 5, 2015. Retrieved August 11, 2015.
- Hofmann SG, Dibartolo PM (2010). "Introduction: Toward an Understanding of Social Anxiety Disorder". Social Anxiety. pp. xix–xxvi. doi:10.1016/B978-0-12-375096-9.00028-6. ISBN 978-0-12-375096-9.
- Thomas B, Hardy S, Cutting P, eds. (1997). Mental Health Nursing: Principles and Practice. London: Mosby. ISBN 978-0-7234-2590-8.
- Settipani CA, Kendall PC (February 2013). "Social functioning in youth with anxiety disorders: association with anxiety severity and outcomes from cognitive-behavioral therapy". Child Psychiatry and Human Development. 44 (1): 1–18. doi:10.1007/s10578-012-0307-0. PMID 22581270.
- Stephan WG, Stephan CW (1985). "Intergroup Anxiety". Journal of Social Issues. 41 (3): 157–175. doi:10.1111/j.1540-4560.1985.tb01134.x.
- Richeson JA, Trawalter S (February 2008). "The threat of appearing prejudiced and race-based attentional biases". Psychological Science. 19 (2): 98–102. doi:10.1111/j.1467-9280.2008.02052.x. PMID 18271854. S2CID 11212529.
- Mathews A, Mogg K, May J, Eysenck M (August 1989). "Implicit and explicit memory bias in anxiety". Journal of Abnormal Psychology. 98 (3): 236–40. doi:10.1037/0021-843x.98.3.236. PMID 2768658.
- Richards A, French CC (1991). "Effects of encoding and anxiety on implicit and explicit memory performance". Personality and Individual Differences. 12 (2): 131–139. doi:10.1016/0191-8869(91)90096-t.
- Amodio DM, Hamilton HK (December 2012). "Intergroup anxiety effects on implicit racial evaluation and stereotyping". Emotion. 12 (6): 1273–80. CiteSeerX 10.1.1.659.5717. doi:10.1037/a0029016. PMID 22775128.
- Plant EA, Devine PG (June 2003). "The antecedents and implications of interracial anxiety". Personality & Social Psychology Bulletin. 29 (6): 790–801. doi:10.1177/0146167203029006011. PMID 15189634. S2CID 8581417.
- "Anxiety". MacArthur SES & Health Network.
- Jeronimus BF, Kotov R, Riese H, Ormel J (October 2016). "Neuroticism's prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants". Psychological Medicine. 46 (14): 2883–2906. doi:10.1017/S0033291716001653. PMID 27523506.
- Giddey M, Wright H. Mental Health Nursing: From first principles to professional practice. Stanley Thornes.
- "Gulf Bend MHMR Center". Retrieved October 11, 2018.
- Downey J (April 27, 2008). "Premium choice anxiety". The Times. London. Archived from the original on February 3, 2014. Retrieved April 25, 2010.
- Is choice anxiety costing british 'blue chip' business? Archived December 22, 2015, at the Wayback Machine, Capgemini, August 16, 2004
- Hartley CA, Phelps EA (July 2012). "Anxiety and decision-making". Biological Psychiatry. 72 (2): 113–8. doi:10.1016/j.biopsych.2011.12.027. PMC 3864559. PMID 22325982.
- "What are the five major types of anxiety disorders?". June 8, 2015.
- "Panic Disorder & Panic Attacks".
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington: American Psychiatric Publishing. pp. 189–195. ISBN 978-0-89042-555-8.
- "Anxiety Disorders". NIMH. March 2016. Archived from the original on July 27, 2016. Retrieved August 14, 2016.
- Craske MG, Stein MB (December 2016). "Anxiety". Lancet. 388 (10063): 3048–3059. doi:10.1016/S0140-6736(16)30381-6. PMID 27349358.
- Kessler RC, Angermeyer M, Anthony JC, DE Graaf R, Demyttenaere K, Gasquet I, et al. (October 2007). "Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative". World Psychiatry. 6 (3): 168–76. PMC 2174588. PMID 18188442.
- Smoller, Jordan W.; Andreassen, Ole A.; Edenberg, Howard J.; Faraone, Stephen V.; Glatt, Stephen J.; Kendler, Kenneth S. (March 14, 2018). "Correction to: Psychiatric genetics and the structure of psychopathology". Molecular Psychiatry. 24 (3): 471. doi:10.1038/s41380-018-0026-4. PMID 29540840.
- Kendler, Kenneth S. (July 2004). "Major Depression and Generalised Anxiety Disorder". FOCUS. 2 (3): 416–425. doi:10.1176/foc.2.3.416.
- Scarre C (1995). Chronicle of the Roman Emperors. Thames & Hudson. pp. 168–9. ISBN 978-5-00-050775-9.
- Reynolds, Chandra A. (June 16, 2013). "Robert Plomin, John C. DeFries, Valerie S. Knopik, Jenae M. Neiderhiser, Behavioral Genetics (6th Edition)". Behavior Genetics. 43 (4): 360–361. doi:10.1007/s10519-013-9598-6.
- Smoller, Jordan W.; Block, Stefanie R.; Young, Mirella M. (November 2009). "Genetics of anxiety disorders: the complex road from DSM to DNA". Depression and Anxiety. 26 (11): 965–975. doi:10.1002/da.20623. PMID 19885930. S2CID 35349081.
- Craske, Michelle G.; Stein, Murray B.; Eley, Thalia C.; Milad, Mohammed R.; Holmes, Andrew; Rapee, Ronald M.; Wittchen, Hans-Ulrich (May 4, 2017). "Anxiety disorders". Nature Reviews Disease Primers. 3 (1): 17024. doi:10.1038/nrdp.2017.24. PMID 28470168.
- Rosen JB, Schulkin J (April 1998). "From normal fear to pathological anxiety". Psychological Review. 105 (2): 325–50. doi:10.1037/0033-295X.105.2.325. PMID 9577241.
- Nolen-Hoeksema, S. (2013). (Ab)normal Psychology (6th edition). McGraw Hill.
- Fricchione G (2011). Compassion and Healing in Medicine and Society: On the Nature and Use of Attachment Solutions to Separation Challenges. Johns Hopkins University Press. p. 172. ISBN 978-1-4214-0220-8.
- Harris J (1998). How the Brain Talks to Itself: A Clinical Primer of Psychotherapeutic Neuroscience. Haworth. p. 284. ISBN 978-0-7890-0408-6.
- Bar-Haim Y, Fox NA, Benson B, Guyer AE, Williams A, Nelson EE, et al. (August 2009). "Neural correlates of reward processing in adolescents with a history of inhibited temperament". Psychological Science. 20 (8): 1009–18. doi:10.1111/j.1467-9280.2009.02401.x. PMC 2785902. PMID 19594857.
- Kennedy, P.J.; Cryan, J.F.; Dinan, T.G.; Clarke, G. (January 2017). "Kynurenine pathway metabolism and the microbiota-gut-brain axis". Neuropharmacology. 112 (Pt B): 399–412. doi:10.1016/j.neuropharm.2016.07.002. PMID 27392632.
- Dinan, Timothy G.; Stilling, Roman M.; Stanton, Catherine; Cryan, John F. (April 2015). "Collective unconscious: How gut microbes shape human behavior". Journal of Psychiatric Research. 63: 1–9. doi:10.1016/j.jpsychires.2015.02.021. PMID 25772005.
- de Weerth, Carolina (December 2017). "Do bacteria shape our development? Crosstalk between intestinal microbiota and HPA axis". Neuroscience & Biobehavioral Reviews. 83: 458–471. doi:10.1016/j.neubiorev.2017.09.016. PMID 28918360.
- Bravo, J. A.; Forsythe, P.; Chew, M. V.; Escaravage, E.; Savignac, H. M.; Dinan, T. G.; Bienenstock, J.; Cryan, J. F. (August 29, 2011). "Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve". Proceedings of the National Academy of Sciences. 108 (38): 16050–16055. doi:10.1073/pnas.1102999108. PMC 3179073. PMID 21876150.
- Burokas, Aurelijus; Arboleya, Silvia; Moloney, Rachel D.; Peterson, Veronica L.; Murphy, Kiera; Clarke, Gerard; Stanton, Catherine; Dinan, Timothy G.; Cryan, John F. (October 2017). "Targeting the Microbiota-Gut-Brain Axis: Prebiotics Have Anxiolytic and Antidepressant-like Effects and Reverse the Impact of Chronic Stress in Mice". Biological Psychiatry. 82 (7): 472–487. doi:10.1016/j.biopsych.2016.12.031. PMID 28242013.
- Benton, D; Williams, C; Brown, A (December 6, 2006). "Impact of consuming a milk drink containing a probiotic on mood and cognition". European Journal of Clinical Nutrition. 61 (3): 355–361. doi:10.1038/sj.ejcn.1602546. PMID 17151594.
- Schmidt, Kristin; Cowen, Philip J.; Harmer, Catherine J.; Tzortzis, George; Errington, Steven; Burnet, Philip W. J. (December 3, 2014). "Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers". Psychopharmacology. 232 (10): 1793–1801. doi:10.1007/s00213-014-3810-0. PMC 4410136. PMID 25449699.
- Waszczuk, Monika A.; Zavos, Helena M. S.; Gregory, Alice M.; Eley, Thalia C. (August 1, 2014). "The Phenotypic and Genetic Structure of Depression and Anxiety Disorder Symptoms in Childhood, Adolescence, and Young Adulthood". JAMA Psychiatry. 71 (8): 905–16. doi:10.1001/jamapsychiatry.2014.655. PMID 24920372.
- Nivard, M. G.; Dolan, C. V.; Kendler, K. S.; Kan, K.-J.; Willemsen, G.; van Beijsterveldt, C. E. M.; Lindauer, R. J. L.; van Beek, J. H. D. A.; Geels, L. M.; Bartels, M.; Middeldorp, C. M.; Boomsma, D. I. (September 4, 2014). "Stability in symptoms of anxiety and depression as a function of genotype and environment: a longitudinal twin study from ages 3 to 63 years". Psychological Medicine. 45 (5): 1039–1049. doi:10.1017/S003329171400213X. PMID 25187475.
- Eley, Thalia C.; McAdams, Tom A.; Rijsdijk, Fruhling V.; Lichtenstein, Paul; Narusyte, Jurgita; Reiss, David; Spotts, Erica L.; Ganiban, Jody M.; Neiderhiser, Jenae M. (July 2015). "The Intergenerational Transmission of Anxiety: A Children-of-Twins Study". American Journal of Psychiatry. 172 (7): 630–637. doi:10.1176/appi.ajp.2015.14070818. PMID 25906669.
- Howe, A S; Buttenschøn, H N; Bani-Fatemi, A; Maron, E; Otowa, T; Erhardt, A; Binder, E B; Gregersen, N O; Mors, O; Woldbye, D P; Domschke, K; Reif, A; Shlik, J; Kõks, S; Kawamura, Y; Miyashita, A; Kuwano, R; Tokunaga, K; Tanii, H; Smoller, J W; Sasaki, T; Koszycki, D; De Luca, V (September 22, 2015). "Candidate genes in panic disorder: meta-analyses of 23 common variants in major anxiogenic pathways". Molecular Psychiatry. 21 (5): 665–679. doi:10.1038/mp.2015.138. PMID 26390831.
- Purves, Kirstin L.; Coleman, Jonathan R. I.; Meier, Sandra M.; Rayner, Christopher; Davis, Katrina A. S.; Cheesman, Rosa; Bækvad-Hansen, Marie; Børglum, Anders D.; Wan Cho, Shing; Jürgen Deckert, J.; Gaspar, Héléna A.; Bybjerg-Grauholm, Jonas; Hettema, John M.; Hotopf, Matthew; Hougaard, David; Hübel, Christopher; Kan, Carol; McIntosh, Andrew M.; Mors, Ole; Bo Mortensen, Preben; Nordentoft, Merete; Werge, Thomas; Nicodemus, Kristin K.; Mattheisen, Manuel; Breen, Gerome; Eley, Thalia C. (November 20, 2019). "A major role for common genetic variation in anxiety disorders". Molecular Psychiatry. doi:10.1038/s41380-019-0559-1. PMC 7237282. PMID 31748690.
- Martin, Nick; Otowa, Takeshi; Lee, Minyoung; Hartman, Catharina; Oldehinkel, Albertine; Preisig, Martin; Jörgen Grabe, Hans; Middeldorp, Christel; Penninx, Brenda (2017). "Meta-Analysis of Genome-Wide Association Studies of Anxiety Disorders". European Neuropsychopharmacology. 27 (10): 1391–1399. doi:10.1016/j.euroneuro.2016.09.604. PMC 4940340. PMID 26754954.
- Deckert, Jurgen; Weber, Heike; Pauli, Paul; Reif, Andreas (2017). "Glrb Allelic Variation Associated with Agoraphobic Cognitions, Increased Startle Response and Fear Network Activation". European Neuropsychopharmacology. 27 (10): 1431–1439. doi:10.1016/j.euroneuro.2016.09.607. PMID 28167838.
- Baldwin J, Cox J (September 2016). "Treating Dyspnea: Is Oxygen Therapy the Best Option for All Patients?". The Medical Clinics of North America. 100 (5): 1123–30. doi:10.1016/j.mcna.2016.04.018. PMID 27542431.
- Vanfleteren LE, Spruit MA, Wouters EF, Franssen FM (November 2016). "Management of chronic obstructive pulmonary disease beyond the lungs". The Lancet. Respiratory Medicine. 4 (11): 911–924. doi:10.1016/S2213-2600(16)00097-7. PMID 27264777.
- Tselebis A, Pachi A, Ilias I, Kosmas E, Bratis D, Moussas G, Tzanakis N (2016). "Strategies to improve anxiety and depression in patients with COPD: a mental health perspective". Neuropsychiatric Disease and Treatment. 12: 297–328. doi:10.2147/NDT.S79354. PMC 4755471. PMID 26929625.
- Muscatello MR, Bruno A, Mento C, Pandolfo G, Zoccali RA (July 2016). "Personality traits and emotional patterns in irritable bowel syndrome". World Journal of Gastroenterology. 22 (28): 6402–15. doi:10.3748/wjg.v22.i28.6402. PMC 4968122. PMID 27605876.
- Remes-Troche JM (December 2016). "How to Diagnose and Treat Functional Chest Pain". Current Treatment Options in Gastroenterology. 14 (4): 429–443. doi:10.1007/s11938-016-0106-y. PMID 27709331.
- Brotto L, Atallah S, Johnson-Agbakwu C, Rosenbaum T, Abdo C, Byers ES, et al. (April 2016). "Psychological and Interpersonal Dimensions of Sexual Function and Dysfunction". The Journal of Sexual Medicine. 13 (4): 538–71. doi:10.1016/j.jsxm.2016.01.019. PMID 27045257.
- McMahon CG, Jannini EA, Serefoglu EC, Hellstrom WJ (August 2016). "The pathophysiology of acquired premature ejaculation". Translational Andrology and Urology. 5 (4): 434–49. doi:10.21037/tau.2016.07.06. PMC 5001985. PMID 27652216.
- Nguyen CM, Beroukhim K, Danesh MJ, Babikian A, Koo J, Leon A (2016). "The psychosocial impact of acne, vitiligo, and psoriasis: a review". Clinical, Cosmetic and Investigational Dermatology. 9: 383–392. doi:10.2147/CCID.S76088. PMC 5076546. PMID 27799808.
- Caçola P (2016). "Physical and Mental Health of Children with Developmental Coordination Disorder". Frontiers in Public Health. 4: 224. doi:10.3389/fpubh.2016.00224. PMC 5075567. PMID 27822464.
- Mosher CE, Winger JG, Given BA, Helft PR, O'Neil BH (November 2016). "Mental health outcomes during colorectal cancer survivorship: a review of the literature". Psycho-Oncology. 25 (11): 1261–1270. doi:10.1002/pon.3954. PMC 4894828. PMID 26315692.
- Testa A, Giannuzzi R, Daini S, Bernardini L, Petrongolo L, Gentiloni Silveri N (February 2013). "Psychiatric emergencies (part III): psychiatric symptoms resulting from organic diseases". European Review for Medical and Pharmacological Sciences. 17 Suppl 1: 86–99. PMID 23436670.

- Samuels MH (October 2008). "Cognitive function in untreated hypothyroidism and hyperthyroidism". Current Opinion in Endocrinology, Diabetes and Obesity. 15 (5): 429–33. doi:10.1097/MED.0b013e32830eb84c. PMID 18769215.
- Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A (August 2016). "Symptoms of depression and anxiety in youth with type 1 diabetes: A systematic review and meta-analysis". Psychoneuroendocrinology. 70: 70–84. doi:10.1016/j.psyneuen.2016.04.019. PMID 27179232.
- Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ (December 2002). "Prevalence of anxiety in adults with diabetes: a systematic review". Journal of Psychosomatic Research. 53 (6): 1053–60. doi:10.1016/S0022-3999(02)00417-8. PMID 12479986.
- Zingone F, Swift GL, Card TR, Sanders DS, Ludvigsson JF, Bai JC (April 2015). "Psychological morbidity of celiac disease: A review of the literature". United European Gastroenterology Journal. 3 (2): 136–45. doi:10.1177/2050640614560786. PMC 4406898. PMID 25922673.
- Molina-Infante J, Santolaria S, Sanders DS, Fernández-Bañares F (May 2015). "Systematic review: noncoeliac gluten sensitivity". Alimentary Pharmacology & Therapeutics. 41 (9): 807–20. doi:10.1111/apt.13155. PMID 25753138. S2CID 207050854.
- Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H (August 2016). "Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review". Journal of Psychosomatic Research. 87: 70–80. doi:10.1016/j.jpsychores.2016.06.001. PMID 27411754.
- Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, et al. (January 2016). "The prevalence of neuropsychiatric symptoms in Alzheimer's disease: Systematic review and meta-analysis". Journal of Affective Disorders. 190: 264–271. doi:10.1016/j.jad.2015.09.069. PMID 26540080.
- Wen MC, Chan LL, Tan LC, Tan EK (June 2016). "Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies". European Journal of Neurology. 23 (6): 1001–19. doi:10.1111/ene.13002. PMC 5084819. PMID 27141858.
- Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M, Sorensen PS, et al. (March 2015). "The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review". Multiple Sclerosis. 21 (3): 305–17. doi:10.1177/1352458514564487. PMC 4429164. PMID 25583845.
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
- "CDC – The Emergency Response Safety and Health Database: Systemic Agent: BENZENE – NIOSH". www.cdc.gov. Archived from the original on January 17, 2016. Retrieved January 27, 2016.
- Gu R, Huang YX, Luo YJ (September 2010). "Anxiety and feedback negativity". Psychophysiology. 47 (5): 961–7. doi:10.1111/j.1469-8986.2010.00997.x. PMID 20374540.
- Bienvenu OJ, Ginsburg GS (December 2007). "Prevention of anxiety disorders". International Review of Psychiatry. 19 (6): 647–54. doi:10.1080/09540260701797837. PMID 18092242.
- Phillips AC, Carroll D, Der G (2015). "Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation". Anxiety, Stress, and Coping. 28 (4): 357–71. doi:10.1080/10615806.2015.1005078. PMC 4772121. PMID 25572915.
- Andrews PW, Thomson JA (July 2009). "The bright side of being blue: depression as an adaptation for analyzing complex problems". Psychological Review. 116 (3): 620–54. doi:10.1037/a0016242. PMC 2734449. PMID 19618990.
- Zald DH, Pardo JV (April 1997). "Emotion, olfaction, and the human amygdala: amygdala activation during aversive olfactory stimulation". Proceedings of the National Academy of Sciences of the United States of America. 94 (8): 4119–24. Bibcode:1997PNAS...94.4119Z. doi:10.1073/pnas.94.8.4119. PMC 20578. PMID 9108115.
- Zald DH, Hagen MC, Pardo JV (February 2002). "Neural correlates of tasting concentrated quinine and sugar solutions". Journal of Neurophysiology. 87 (2): 1068–75. doi:10.1152/jn.00358.2001. PMID 11826070. S2CID 6278342.
- National Research Council (Us) Institute Of Medicine (Us) Committee On The Prevention Of Mental Disorders Substance Abuse Among Children, Youth, and Young Adults (2009). "Table E-4 Risk Factors for Anxiety". In O'Connell ME, Boat T, Warner KE (eds.). Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective. National Academies Press. p. 530. doi:10.17226/12480. ISBN 978-0-309-12674-8. PMID 20662125. S2CID 142581788.
- Arenas, Daniel J.; Thomas, Arthur; Wang, JiCi; DeLisser, Horace M. (August 5, 2019). "A Systematic Review and Meta-analysis of Depression, Anxiety, and Sleep Disorders in US Adults with Food Insecurity". Journal of General Internal Medicine. 34 (12): 2874–2882. doi:10.1007/s11606-019-05202-4. PMC 6854208. PMID 31385212.
- Behnke RR, Sawyer CR (2000). "Anticipatory anxiety patterns for male and female public speakers". Communication Education. 49 (2): 187–195. doi:10.1080/03634520009379205.
- Testa A, Giannuzzi R, Sollazzo F, Petrongolo L, Bernardini L, Dain S (February 2013). "Psychiatric emergencies (part II): psychiatric disorders coexisting with organic diseases". European Review for Medical and Pharmacological Sciences. 17 Suppl 1: 65–85. PMID 23436669.

- Stein, MB; Sareen, J (November 19, 2015). "Clinical Practice: Generalized Anxiety Disorder". The New England Journal of Medicine. 373 (21): 2059–68. doi:10.1056/nejmcp1502514. PMID 26580998.
- Cuijpers, P; Sijbrandij, M; Koole, S; Huibers, M; Berking, M; Andersson, G (March 2014). "Psychological treatment of generalized anxiety disorder: A meta-analysis". Clinical Psychology Review. 34 (2): 130–140. doi:10.1016/j.cpr.2014.01.002. PMID 24487344.
- Otte, C (2011). "Cognitive behavioral therapy in anxiety disorders: current state of the evidence". Dialogues in Clinical Neuroscience. 13 (4): 413–21. PMC 3263389. PMID 22275847.
- Pompoli, A; Furukawa, TA; Imai, H; Tajika, A; Efthimiou, O; Salanti, G (April 13, 2016). "Psychological therapies for panic disorder with or without agoraphobia in adults: a network meta-analysis" (PDF). The Cochrane Database of Systematic Reviews. 4: CD011004. doi:10.1002/14651858.CD011004.pub2. PMC 7104662. PMID 27071857.
- Olthuis, JV; Watt, MC; Bailey, K; Hayden, JA; Stewart, SH (March 12, 2016). "Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults". The Cochrane Database of Systematic Reviews. 3: CD011565. doi:10.1002/14651858.cd011565.pub2. PMC 7077612. PMID 26968204.
- Donker, T; Petrie, K; Proudfoot, J; Clarke, J; Birch, MR; Christensen, H (November 15, 2013). "Smartphones for smarter delivery of mental health programs: a systematic review". Journal of Medical Internet Research. 15 (11): e247. doi:10.2196/jmir.2791. PMC 3841358. PMID 24240579.
- Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017;19(2):93‐107.
- Moreno-Peral, Patricia; Conejo-Cerón, Sonia; Rubio-Valera, Maria; Fernández, Anna; Navas-Campaña, Desirée; Rodríguez-Morejón, Alberto; Motrico, Emma; Rigabert, Alina; Luna, Juan de Dios; Martín-Pérez, Carlos; Rodríguez-Bayón, Antonina; Ballesta-Rodríguez, María Isabel; Luciano, Juan Vicente; Bellón, Juan Ángel (October 1, 2017). "Effectiveness of Psychological and/or Educational Interventions in the Prevention of Anxiety". JAMA Psychiatry. 74 (10): 1021–1029. doi:10.1001/jamapsychiatry.2017.2509. PMC 5710546. PMID 28877316.
- Pote, Inês (February 19, 2018). "Preventing anxiety with psychological and educational interventions". National Elf Service.
- Schmidt, Norman B.; Allan, Nicholas P.; Knapp, Ashley A.; Capron, Dan (2019). "Targeting anxiety sensitivity as a prevention strategy". The Clinician's Guide to Anxiety Sensitivity Treatment and Assessment. pp. 145–178. doi:10.1016/B978-0-12-813495-5.00008-5. ISBN 978-0-12-813495-5.
- Anxiety Disorders at eMedicine
- Shelton, Charles I. (March 1, 2004). "Diagnosis and Management of Anxiety Disorders". The Journal of the American Osteopathic Association. 104 (3 Suppl 1): S2–S5. PMID 16493143.
External links
| Classification | |
|---|---|
| External resources |
| Library resources about Anxiety |
.jpg)