Baclofen
Baclofen, sold under the brand name Lioresal among others, is a medication used to treat muscle spasticity such as from a spinal cord injury or multiple sclerosis.[1][2] It may also be used for hiccups and muscle spasms near the end of life.[2] It is taken by mouth or by delivery into the spinal canal.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lioresal, Liofen, Gablofen, others |
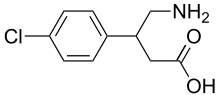
| Other names | β-(4-chlorophenyl)-γ-aminobutyric acid (β-(4-chlorophenyl)-GABA) |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth, intrathecal |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Well-absorbed |
| Protein binding | 30% |
| Metabolism | 85% excreted in urine/faeces unchanged. 15% metabolised by deamination |
| Elimination half-life | 1.5 to 4 hours |
| Excretion | Renal (70–80%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.013.170 |
| Chemical and physical data | |
| Formula | C10H12ClNO2 |
| Molar mass | 213.66 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Common side effects include sleepiness, weakness, and dizziness.[1] Serious side effects may occur if baclofen is rapidly stopped including seizures and rhabdomyolysis.[1] Use in pregnancy is of unclear safety while use during breastfeeding is probably safe.[3] It is believed to work by decreasing neurotransmitters.[1]
Baclofen was approved for medical use in the United States in 1977.[1] It is available as a generic medication.[2] A month supply in the United Kingdom costs the NHS about £1 as of 2019.[2] In the United States the wholesale cost of this amount is about US$8.40.[4] In 2017, it was the 140th most commonly prescribed medication in the United States, with more than four million prescriptions.[5][6]
Medical uses
Baclofen is primarily used for the treatment of spastic movement disorders, especially in instances of spinal cord injury, cerebral palsy, and multiple sclerosis.[7] Its use in people with stroke or Parkinson's disease is not recommended.[7]
Side effects
Briefly, adverse effects may include drowsiness, dizziness, weakness, fatigue, headache, trouble sleeping, nausea and vomiting, urinary retention, or constipation. A complete list of reported adverse effects can be found on the product insert.[8]
Withdrawal syndrome
Discontinuation of baclofen can be associated with a withdrawal syndrome which resembles benzodiazepine withdrawal and alcohol withdrawal. Withdrawal symptoms are more likely if baclofen is administered intrathecally or for long periods of time (more than a couple of months) and can occur from low or high doses.[9] The severity of baclofen withdrawal depends on the rate at which it is discontinued. Thus to minimise withdrawal symptoms, the dose should be tapered down slowly when discontinuing baclofen therapy. Abrupt withdrawal is more likely to result in severe withdrawal symptoms. Acute withdrawal symptoms can be stopped by recommencing baclofen.[10]
Withdrawal symptoms may include auditory hallucinations, visual hallucinations, tactile hallucinations, delusions, confusion, agitation, delirium, disorientation, fluctuation of consciousness, insomnia, dizziness, nausea, inattention, memory impairments, perceptual disturbances, itching, anxiety, depersonalization, hypertonia, hyperthermia (higher than normal temperature without infection), formal thought disorder, psychosis, mania, mood disturbances, restlessness, and behavioral disturbances, tachycardia, seizures, tremors, autonomic dysfunction, hyperpyrexia (fever), extreme muscle rigidity resembling neuroleptic malignant syndrome and rebound spasticity.[10][9]
Abuse
Baclofen, at standard dosing, does not appear to possess addictive properties, and has not been associated with any degree of drug craving.[11][12] Euphoria is however listed as a common to very common side-effect of baclofen in the BNF 75[13] There are very few cases of abuse of baclofen for reasons other than attempted suicide.[11] In contrast to baclofen, another GABAB receptor agonist, γ-hydroxybutyric acid (GHB), has been associated with euphoria, abuse, and addiction.[14] These effects are likely mediated not by activation of the GABAB receptor, but rather by activation of the GHB receptor.[14] Although baclofen does not produce euphoria or other reinforcing effects, which is unlike alcohol and benzodiazepines (as well as GHB), it does similarly possess sedative and antianxiety properties.[12]
Overdose
Reports of overdose indicate that baclofen may cause symptoms including vomiting, general weakness, sedation, respiratory insufficiency, seizures, unusual pupil size, dizziness,[15] headaches,[15] itching, hypothermia, bradycardia, hypertension, hyporeflexia, coma, and death.[16]
Pharmacology
Chemically, baclofen is a derivative of the neurotransmitter γ-aminobutyric acid (GABA). It is believed to work by activating (or agonizing) GABA receptors, specifically the GABAB receptors.[17] Its beneficial effects in spasticity result from its actions in the brain and spinal cord.[18]
Pharmacodynamics
Baclofen produces its effects by activating the GABAB receptor, similar to the drug phenibut which also activates this receptor and shares some of its effects. Baclofen is postulated to block mono-and-polysynaptic reflexes by acting as an inhibitory ligand, inhibiting the release of excitatory neurotransmitters. However, baclofen does not have significant affinity for the GHB receptor, and has no known abuse potential.[19] The modulation of the GABAB receptor is what produces baclofen's range of therapeutic properties.
Similarly to phenibut (β-phenyl-GABA), as well as pregabalin (β-isobutyl-GABA), which are close analogues of baclofen, baclofen (β-(4-chlorophenyl)-GABA) has been found to block α2δ subunit-containing voltage-gated calcium channels (VGCCs).[20] However, it is weaker relative to phenibut in this action (Ki = 23 and 39 μM for R- and S-phenibut and 156 μM for baclofen).[20] Moreover, baclofen is in the range of 100-fold more potent by weight as an agonist of the GABAB receptor in comparison to phenibut, and in accordance, is used at far lower relative dosages. As such, the actions of baclofen on α2δ subunit-containing VGCCs are likely not clinically-relevant.[20]
Pharmacokinetics
The drug is rapidly absorbed after oral administration and is widely distributed throughout the body. Biotransformation is low: the drug is predominantly excreted unchanged by the kidneys.[21] The half-life of baclofen is roughly 2–4 hours; it therefore needs to be administered frequently throughout the day to control spasticity appropriately.
Chemistry
Baclofen is a white (or off-white) mostly odorless crystalline powder, with a molecular weight of 213.66 g/mol. It is slightly soluble in water, very slightly soluble in methanol, and insoluble in chloroform.
History
Historically, baclofen was designed as a drug for treating epilepsy. It was first made at Ciba-Geigy, by the Swiss chemist Heinrich Keberle, in 1962.[22][23] Its effect on epilepsy was disappointing, but it was found that in certain people, spasticity decreased.
Currently, baclofen continues to be given by mouth, with variable effects. In severely affected children, the oral dose is so high that side-effects appear, and the treatment loses its benefit. How and when baclofen came to be used in the spinal sac (intrathecally) remains unclear, but as of 2012, this has become an established method of treating spasticity in many conditions.
In his 2008 book, Le Dernier Verre (translated literally as The Last Glass or The End of my Addiction), French-American cardiologist Olivier Ameisen described how he treated his alcoholism with baclofen. Inspired by this book, an anonymous donor gave $750,000 to the University of Amsterdam in the Netherlands to initiate a clinical trial of high-dose baclofen, which Ameisen had called for since 2004.[24] The trial concluded, "Neither low nor high doses of baclofen were effective in the treatment of [alcohol dependence]. Adverse events were frequent, although generally mild and transient. Therefore, large-scale prescription of baclofen for the treatment of AD seems premature and should be reconsidered."[25]
Society and culture
Routes of administration

Baclofen can be administered transdermally as part of a pain-relieving and muscle-relaxing topical cream mix at a compounding pharmacy, orally[26] or intrathecally[27] (directly into the cerebral spinal fluid) using a pump implanted under the skin.
Intrathecal pumps offer much lower doses of baclofen because they are designed to deliver the medication directly to the spinal fluid rather than going through the digestive and blood system first. They are often preferred in spasticity patients such as those with spastic diplegia, as very little of the oral dose actually reaches the spinal fluid. Besides those with spasticity, intrathecal administration is also used in patients with multiple sclerosis who have severe painful spasms which are not controllable by oral baclofen. With pump administration, a test dose is first injected into the spinal fluid to assess the effect, and if successful in relieving spasticity, a chronic intrathecal catheter is inserted from the spine through the abdomen and attached to the pump which is implanted under the abdomen's skin, usually by the ribcage. The pump is computer-controlled for automatic dosage and the reservoir in the pump can be replenished by percutaneous injection. The pump also has to be replaced about every 5 years due to the battery life and other wear.
Other names
Synonyms include chlorophenibut. Brand names include Beklo, Baclodol, Flexibac, Gablofen, Kemstro, Liofen, Lioresal, Lyflex, Clofen, Muslofen, Bacloren, Baklofen, Sclerofen, Pacifen and others.
Research
Baclofen is being studied for the treatment of alcoholism.[11] Evidence as of 2019 is not conclusive enough to recommend its use for this purpose.[11][28] In 2014, the French drug agency ANSM issued a 3-year temporary recommendation allowing the use of baclofen in alcoholism.[29] In 2018, baclofen received a Marketing Authorization for use in alcoholism treatment from the agency if all other treatments are not effective.[30]
It is being studied along with naltrexone and sorbitol for Charcot-Marie-Tooth disease (CMT), a hereditary disease that causes peripheral neuropathy.[31] It is also being studied for cocaine addiction.[32] Baclofen and other muscle relaxants are being studied for potential use for persistent hiccups.[33][34]
From 2014 to 2017 baclofen misuse, toxicity and use in suicide attempts among adults in the US increased.[35]
References
- "Baclofen Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 3 March 2019.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 1092. ISBN 9780857113382.
- "Baclofen Pregnancy and Breastfeeding Warnings". Drugs.com. Retrieved 3 March 2019.
- "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Retrieved 3 March 2019.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Baclofen - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- "Baclofen". The American Society of Health-System Pharmacists. Retrieved 2011-12-06.
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022462s000lbl.pdf
- Grenier, B.; Mesli, A.; Cales, J.; Castel, J. P.; Maurette, P. (1996). "[Severe hyperthermia caused by sudden withdrawal of continuous intrathecal administration of baclofen]". Ann Fr Anesth Reanim. 15 (5): 659–62. doi:10.1016/0750-7658(96)82130-7. PMID 9033759.
- Leo, R. J.; Baer, D. (Nov–Dec 2005). "Delirium Associated With Baclofen Withdrawal: A Review of Common Presentations and Management Strategies". Psychosomatics. 46 (6): 503–07. doi:10.1176/appi.psy.46.6.503. PMID 16288128. Archived from the original on 2006-02-09.
- Leggio, L.; Garbutt, J. C.; Addolorato, G. (Mar 2010). "Effectiveness and safety of baclofen in the treatment of alcohol dependent patients". CNS & Neurological Disorders Drug Targets. 9 (1): 33–44. doi:10.2174/187152710790966614. PMID 20201813.
- Agabio, Roberta; Preti, Antonio; Gessa, Gian Luigi (2013). "Efficacy and Tolerability of Baclofen in Substance Use Disorders: A Systematic Review". European Addiction Research. 19 (6): 325–45. doi:10.1159/000347055. ISSN 1421-9891. PMID 23775042.
- "BNF is only available in the UK". NICE. Retrieved 2019-04-16.
- van Nieuwenhuijzen, P.S.; McGregor, I.S.; Hunt, G.E. (2009). "The distribution of γ-hydroxybutyrate-induced Fos expression in rat brain: Comparison with baclofen". Neuroscience. 158 (2): 441–55. doi:10.1016/j.neuroscience.2008.10.011. ISSN 0306-4522. PMID 18996447.
- "Gablofen (Baclofen) FDA Full Prescribing Information" (PDF). US Food and Drug Administration. Retrieved 2016-01-21.
- Perry, H. E.; Wright, R. O.; Shannon, M. W.; Woolf, A. D. (1998). "Baclofen Overdose: Drug Experimentation in a Group of Adolescents". Pediatrics. 101 (6): 1045–48. doi:10.1542/peds.101.6.1045. ISSN 0031-4005. PMID 9606233.
- "Product Information Clofen". TGA eBusiness Services. Millers Point, Australia: Alphapharm Pty Limited. 7 June 2017. Retrieved 15 August 2017.
- Brayfield, A, ed. (9 January 2017). "Baclofen: Martindale: The Complete Drug Reference". MedicinesComplete. London, UK: Pharmaceutical Press. Retrieved 15 August 2017.
- Carter, L. P.; Koek, W.; France, C. P. (October 2008). "Behavioral analyses of GHB: Receptor mechanisms". Pharmacol. Ther. 121 (1): 100–14. doi:10.1016/j.pharmthera.2008.10.003. PMC 2631377. PMID 19010351.
- Zvejniece L, Vavers E, Svalbe B, Veinberg G, Rizhanova K, Liepins V, Kalvinsh I, Dambrova M (2015). "R-phenibut binds to the α2-δ subunit of voltage-dependent calcium channels and exerts gabapentin-like anti-nociceptive effects". Pharmacol. Biochem. Behav. 137: 23–29. doi:10.1016/j.pbb.2015.07.014. PMID 26234470.
- Wuis, E. W.; Dirks, M. J. M.; Termond, E. F. S.; Vree, T. B.; Kleijn, E. (1989). "Plasma and urinary excretion kinetics of oral baclofen in healthy subjects". European Journal of Clinical Pharmacology. 37 (2): 181–84. doi:10.1007/BF00558228. PMID 2792173.
- Froestl, Wolfgang (2010). "Chemistry and Pharmacology of GABAb Receptor Ligands". In Blackburn, Thomas P. (ed.). GABAb Receptor Pharmacology – A Tribute to Norman Bowery. Advances in Pharmacology. 58. pp. 19–62. doi:10.1016/S1054-3589(10)58002-5. ISBN 978-0-12-378647-0. PMID 20655477.
- Yogeeswari, P.; Ragavendran, J. V.; Sriram, D. (2006). "An update on GABA analogs for CNS drug discovery" (PDF). Recent Patents on CNS Drug Discovery. 1 (1): 113–18. doi:10.2174/157488906775245291. PMID 18221197. Archived from the original (PDF) on 2010-06-16.
- Enserink, M. (2011). "Anonymous Alcoholic Bankrolls Trial of Controversial Therapy". Science. 332 (6030): 653. Bibcode:2011Sci...332..653E. doi:10.1126/science.332.6030.653. PMID 21551041.
- Beraha, EM; Salemink, E; Goudriaan, AE; Bakker, A; de Jong, D; Smits, N; Zwart, JW; Geest, DV; Bodewits, P; Schiphof, T; Defourny, H; van Tricht, M; van den Brink, W; Wiers, RW (December 2016). "Efficacy and safety of high-dose baclofen for the treatment of alcohol dependence: A multicentre, randomised, double-blind controlled trial". European Neuropsychopharmacology. 26 (12): 1950–1959. doi:10.1016/j.euroneuro.2016.10.006. PMID 27842939.
- CID 3738, Tablet
- CID 2284
- Liu, Jia; Wang, Lu-Ning (6 November 2019). "Baclofen for alcohol withdrawal". The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.CD008502.pub6. ISSN 1469-493X. PMC 6831488. PMID 31689723.
- "Une recommandation temporaire d’utilisation (RTU) est accordée pour le baclofène – Point d'information", ANSM, 14 March 2014.
- "Autorisation du baclofène : des conditions d'utilisation trop restrictives ? - A la une". Destination Santé (in French). 25 October 2018.
- Attarian, Shahram; Vallat, Jean-Michel; Magy, Laurent; Funalot, Benoît; Gonnaud, Pierre-Marie; Lacour, Arnaud; Péréon, Yann; Dubourg, Odile; Pouget, Jean; Micallef, Joëlle; Franques, Jérôme; Lefebvre, Marie-Noëlle; Ghorab, Karima; Al-Moussawi, Mahmoud; Tiffreau, Vincent; Preudhomme, Marguerite; Magot, Armelle; Leclair-Visonneau, Laurène; Stojkovic, Tanya; Bossi, Laura; Lehert, Philippe; Gilbert, Walter; Bertrand, Viviane; Mandel, Jonas; Milet, Aude; Hajj, Rodolphe; Boudiaf, Lamia; Scart-Grès, Catherine; Nabirotchkin, Serguei; Guedj, Mickael; Chumakov, Ilya; Cohen, Daniel (2014). "An exploratory randomised double-blind and placebo-controlled phase 2 study of a combination of baclofen, naltrexone and sorbitol (PXT3003) in patients with Charcot-Marie-Tooth disease type 1A". Orphanet Journal of Rare Diseases. 9 (1): 199. doi:10.1186/s13023-014-0199-0. PMC 4311411. PMID 25519680.
- Kampman, KM (2005). "New medications for the treatment of cocaine dependence". Psychiatry (Edgmont). 2 (12): 44–48. PMC 2994240. PMID 21120115.
- "What Is the Latest on Treatment for Hiccups?". Medscape. Retrieved July 29, 2018.
- Walker, Paul; Watanabe, Sharon; Bruera, Eduardo (1998). "Baclofen, A Treatment for Chronic Hiccup". Journal of Pain and Symptom Management. 16 (2): 125–132. doi:10.1016/S0885-3924(98)00039-6. PMID 9737104.
- Reynolds, Kimberly; Kaufman, Robert; Korenoski, Amanda; Fennimore, Laura; Shulman, Joshua; Lynch, Michael (2019-12-01). "Trends in gabapentin and baclofen exposures reported to U.S. poison centers". Clinical Toxicology. 0: 1–10. doi:10.1080/15563650.2019.1687902. ISSN 1556-3650. PMID 31786961.