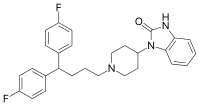
Pimozide
Pimozide (sold under the brand name Orap) is an antipsychotic drug of the diphenylbutylpiperidine class. It was discovered at Janssen Pharmaceutica in 1963. It has a high potency compared to chlorpromazine (ratio 50-70:1). On a weight basis it is even more potent than haloperidol. It also has special neurologic indications for Tourette syndrome and resistant tics. The side effects include akathisia, tardive dyskinesia, and, more rarely, neuroleptic malignant syndrome and prolongation of the QT interval.
 | |
| Clinical data | |
|---|---|
| Trade names | Orap |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a686018 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 40-50% |
| Metabolism | CYP3A4, CYP1A2 and CYP2D6 |
| Elimination half-life | 55 hours (adults), 66 hours (children) |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.016.520 |
| Chemical and physical data | |
| Formula | C28H29F2N3O |
| Molar mass | 461.557 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Medical uses
Pimozide is used in its oral preparation in schizophrenia and chronic psychosis (on-label indications in Europe only), Tourette syndrome,[1] and resistant tics (Europe, USA and Canada).
There have been numerous studies showing Pimozide can be used successfully to treat Delusional parasitosis and traditionally was the drug of choice. However, newer medications have become prevalent recently as the preferred medication. In one case a series of 33 patients with delusional parasitosis (median age, 60 years), pimozide was prescribed for 24 patients, 18 of whom took the drug. The dose ranged from 1 to 5 mg daily. No information regarding initial dosing was specified, although the dose was continued for 6 weeks prior to tapering. Of those patients receiving pimozide, 61% (11/18) experienced improvement in or full remission of symptoms. The use of pimozide for the treatment of delusional parasitosis is based primarily on data from case series/reports that demonstrate some efficacy in the majority of patients. Currently, atypical antipsychotics such as olanzapine or risperidone are used as first line treatment. However, patients who experience negative side-effects with the first line medications are typically given pimozide.[2][3]
Efficacy
A 2013 systematic review compared pimozide with other antipsychotics for schizophrenia or related psychoses:
| Summary | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Enough overall consistency over different outcomes and time scales is present to confirm that pimozide is a drug with effectiveness similar to that of other, more commonly used antipsychotic drugs such as chlorpromazine for people with schizophrenia.[4] | ||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
Pimozide has been used in the treatment of delusional disorder and paranoid personality disorder.[5] It has also been used for delusional parasitosis.[6]
Contraindications
It is contraindicated in individuals with either acquired, congenital or a family history of QT interval prolongation.[7] Its use is advised against in individuals with people with either a personal or a family history of arrhythmias or torsades de pointes.[7] Likewise its use is also advised against in individuals with uncorrected hypokalaemia and hypomagnesaemia or clinical significant cardiac disorders (e.g. a recent myocardial infarction or bradycardia.[7] It is also contraindicated in individuals being cotreated with SSRIs or in those with a known hypersensitivity to pimozide or other diphenylbutyl-piperidine derivatives.[7] Likewise its use is contraindicated in individuals receiving treatment with CYP3A4, CYP1A2, or CYP2D6 inhibitors.[7]
Side effects
Very common (>10% frequency) side effects include:[8][7][9][10]
- Akinesia
- Constipation
- Dizziness
- Dry mouth
- Hyperhidrosis
- Nocturia
- Somnolence
- Speech disorder
Overdose
Pimozide overdose presents with severe extrapyramidal symptoms, hypotension, sedation, QT interval prolongation and ventricular arrhythmias including torsades de pointes.[7] Gastric lavage, establishment of a patent airway and, if necessary, mechanically assisted respiration is the recommended treatment for pimozide overdose.[7] Cardiac monitoring should be continued for at least 4 days due to the long half-life of pimozide.[7]
Pharmacology
Pimozide acts as an antagonist of the D2, D3, and D4 receptors and the 5-HT7 receptor. It is also a hERG blocker.
Similarly to other typical antipsychotics pimozide has a high affinity for the Dopamine D2 receptor and this likely results in its sexual (due to prolactin hypersecretion) and extrapyramidal side effects as well as its therapeutic efficacy against the positive symptoms of schizophrenia.[11]
| Protein | Ki (nM)[12] | Notes |
|---|---|---|
| 5-HT1A | 650 | |
| 5-HT2A | 48.4 | This receptor is believed to be responsible for the atypicality of other antipsychotics like clozapine, olanzapine and quetiapine. Pimozide's affinity towards this receptor is low compared to its affinity for the D2 receptor and hence this receptor unlikely contributes to its effects to any meaningful extent. |
| 5-HT2C | 2,112 | |
| 5-HT6 | 71 | |
| 5-HT7 | 0.5 | Relatively high affinity for this receptor may explain its supposed antidepressant-like effects in animal models of depression.[13] |
| α1A | 197.7 | Low affinity towards this receptor may explain why pimozide has a lower liability for producing orthostatic hypotension.[11] |
| α2A | 1,593 | |
| α2B | 821 | |
| α2C | 376.5 | |
| M3 | 1,955 | This receptor is believed to be responsible for the interference with glucose homeostasis seen with some of the atypical antipsychotics such as clozapine and olanzapine.[14] Pimozide's low affinity for this receptor likely contributes to the comparatively mild effects on glucose homeostasis. |
| D1 | >10,000 | |
| D2 | 0.33 | Likely the receptor responsible for the therapeutic effects against the positive symptoms of schizophrenia of antipsychotics like pimozide as well as the prolactin-elevating and extrapyramidal side effect-generating effects of typical antipsychotics like pimozide.[14] |
| D3 | 0.25 | |
| D4 | 1.8 | |
| hERG | 18 | May be responsible for pimozide's high liability for prolonging the QT interval.[14] |
| H1 | 692 | Likely responsible for why pimozide tends to produce so little sedation.[14] |
| σ | 508 |
| Pharmacokinetic parameter | Value |
|---|---|
| Time to peak plasma concentration (Tmax) | 6-8 hr |
| Peak plasma concentration (Cmax) | 4-19 ng/mL |
| Elimination half-life (t1/2) | 55 hours (adults), 66 hours (children) |
| Metabolising enzymes | CYP3A4, CYP1A2 and CYP2D6 |
| Excretion pathways | Urine |
History
In 1985 the pimozide was approved by the FDA for marketing as an orphan drug for the treatment of Tourette's syndrome.[1]
See also
Notes
- A lower Ki value indicates a stronger binding
References
- Colvin CL, Tankanow RM (June 1985). "Pimozide: use in Tourette's syndrome". Drug Intelligence & Clinical Pharmacy. 19 (6): 421–4. doi:10.1177/106002808501900602. PMID 3891283.
- Generali JA, Cada DJ (February 2014). "Pimozide: parasitosis (delusional)". Hospital Pharmacy. 49 (2): 134–5. doi:10.1310/hpj4902-134. PMC 3940679. PMID 24623867.
- Meehan WJ, Badreshia S, Mackley CL (March 2006). "Successful treatment of delusions of parasitosis with olanzapine". Archives of Dermatology. 142 (3): 352–5. doi:10.1001/archderm.142.3.352. PMID 16549712.
- Mothi M, Sampson S (November 2013). "Pimozide for schizophrenia or related psychoses". The Cochrane Database of Systematic Reviews. 11 (11): CD001949. doi:10.1002/14651858.CD001949.pub3. PMID 24194433. Archived from the original on 27 November 2017.
- Munro A (1999). Delusional disorder. Cambridge: Cambridge University Press. ISBN 0-521-58180-X.
- van Vloten WA (March 2003). "Pimozide: use in dermatology". Dermatology Online Journal. 9 (2): 3. PMID 12639456. Archived from the original on 19 August 2003.
- "Oral 4 mg tablets. - Summary of Product Characteristics". electronic Medicines Compendium. Janssen-Cilag Ltd. 2 April 2013. Archived from the original on 3 March 2016. Retrieved 4 December 2013.
- "Oral (pimozide) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 4 December 2013. Retrieved 4 December 2013.
- Brayfield A (12 February 2013). Pimozide. Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. Retrieved 4 December 2013.
- "ORAP (pimozide) tablet [Teva Select Brands]". DailyMed. Teva Select Brands. July 2012. Archived from the original on 3 July 2013. Retrieved 4 December 2013.
- Taylor D, Paton C, Shitij K (2012). The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. ISBN 978-0-470-97948-8.
- Roth BL, Driscol J (12 January 2011). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 8 November 2013. Retrieved 4 December 2013.
- Mahesh R, Pandey DK, Bhatt S, Gautam BK (January–March 2011). "Anti-depressant like Effect of Pimozide in Acute and Chronic Animal Models of Depression". Indian Journal of Pharmaceutical Education and Research. 45 (1): 46–53.
- Brunton L, Chabner B, Knollman B (2010). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill Professional. ISBN 978-0-07-162442-8.