Dental fear
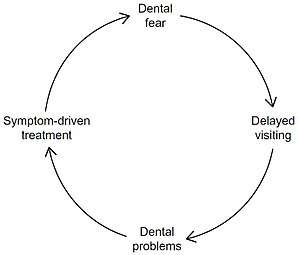
Dental fear is a normal emotional reaction to one or more specific threatening stimuli in the dental situation.[1][2] However, dental anxiety is indicative of a state of apprehension that something dreadful is going to happen in relation to dental treatment, and it is usually coupled with a sense of losing control.[1] Similarly, dental phobia denotes a severe type of dental anxiety, and is characterised by marked and persistent anxiety in relation to either clearly discernible situations or objects (e.g. drilling, local anaesthetic injections) or to the dental setting in general.[1] The term ‘dental fear and anxiety’ (DFA) is often used to refer to strong negative feelings associated with dental treatment among children, adolescents and adults, whether or not the criteria for a diagnosis of dental phobia are met. Dental phobia can include fear of dental procedures, dental environment or setting, fear of dental instruments or fear of the dentist as a person.[3] People with dental phobia often avoid the dentist and neglect oral health, which may lead to painful dental problems and ultimately force a visit to the dentist. The emergency nature of this appointment may serve to worsen the phobia. This phenomenon may also be called the cycle of dental fear.[3] Dental anxiety typically starts in childhood.[1] There is the potential for this to place strains on relationships and negatively impact on employment.[4]
| Dental fear | |
|---|---|
| Other names | Dental anxiety, dental phobia, odontophobia |
 | |
| Cycle of dental fear | |
Signs and symptoms
As with all types of fear and phobias, dental fear can manifest as single or combination of emotional, physiological, cognitive and behavioural symptoms.[5]
Emotional response
- Feeling of fear
- Feeling of anxiety
- Apprehension
- Panic
Physiological response
- Increased heart rate
- Breathlessness
- Sweating
- Nausea
- Shaking
Cognitive response
- "I don't like the feeling of this..."
- "I am choking to death"
- "I am having a heart attack"
- "I am going to die"
Behavioural response
- Agitation
- High vigilance
Cause
Research suggests that there is a complex set of factors that lead to the development and maintenance of significant dental anxiety or dental phobia, which can be grouped as genetic, behavioural and cognitive factors.[6] In comparison to other phobias, literature on odontophobia is relatively limited. There are several theories been proposed, however a 2014 review describes 5 pathways which relate specifically to development dental fear and anxiety: Cognitive Conditioning, Vicarious, Verbal Threat, Informative, and Parental. It is important to note, however, that there may be a variety of background factors common to all general fear and anxiety conditions that may be at play and affect these more specific pathways.[6]
Conditioning
Conditioning is defined as the process by which a person learns through personal experience that an event or stimulus will result in a detrimental outcome, e.g. "if I visit the dentist, it is going to be sore". As, expected dental fear is associated with previous traumatic experiences, especially their first one.[1] It is believed to be the most commonly used pathway for patients to develop dental fear and anxiety.[6]
Informative
This indirect pathway relates to fear acquisition through gaining information and becoming bias to the dental environment from dental phobic elders, negative connotations advertised by media (e.g. television, movies), and friends with personal negative experiences.[6]
Vicarious
The vicarious pathway suggests that fear is acquired through imagination of the feelings, experience or actions of another person. Whether this pathway occurs on its own or in combination with others is still unknown. It has been suggested that dental fear in the very young is passed through this pathway through observation of expressions of fear by elders/parents at the dentist.[6]
Verbal threat
This pathway can be seen as similar to the informative pathway, however it is more reliant on the emotion of fear elicited by "word of mouth" and is heavily modulated by the messenger. In essence the verbal threat pathway is the fear induced when an authority figure threatens an individual with a painful experience. In the case of dental fear, the painful and/or negative experiences linked to dental visits. Although, at a glance, the verbal threat and informative pathway are similar, in odontophobia the two pathways differ in that the verbal threat pathway occurs when a “visit to the dentist” is literally used as a form of punishment for bad behaviour. This does not occur in the informative pathway.[6]
Parental modelling
There is a significant relationship between child and parental dental fear,[7] especially that of the mothers.[6] it has been suggested that this relationship is strongest in children 8 years or younger.[6] However, it is important to note the parental modelling pathway may overlap with the informative or vicarious pathways are all linked in some way.
Diagnosis
Several methods have been developed to diagnose dental fear and anxiety. In addition to identifying the patients with dental fear, different categories of dental fear have been established.[3][8] These include:
- Dental fear survey (DFS) which incapsulates 20 items in relation to various situations, feelings and reaction to dental work which is used to diagnose dental fear.
- Modified child dental anxiety scale (MCDAS), used for children and it has 8 items with a voting system from 1-5 where 1 is not worried and 5 is very worried.
- The index of dental anxiety and fear (IDAF-4C+), used for adults and it is separated into 8 item module and then a further 10 item module.
- Corahs dental anxiety scale 1-4 questions and then 1-26 question. This scale has a ranking system and the second section with 26 questions has 1-4 options ranging from 'low' to 'don't know' which is used to assess dental concern. The first section with 1-4 questions has 5 Likert scale options which are worth 1-5 points with the possible amount of maximum points is 20. Then depending on the result you rate the dental anxiety. 9-12 being moderate 13-14 being high, and 15-20 being severe.
- Spielberger State Trait Anxiety Index (STA): an instrument for measuring anxiety in adults. It differentiates between temporary condition of “state anxiety” and the more general and long-lasting quality of “trait anxiety”. It can also help differentiate between anxiety and depression[9]
- Anxiety Sensitivity Index (ASI): a 16-item scale that focuses on apprehension about the symptoms of anxiety itself[10]
- Seattle System: consists of four diagnostic types in which such individuals are categorised according to the main source of their dear regarding dental treatment[3]
- Type 1: simple conditioned phobia—fear of dental procedures
- Type 2: fear of catastrophe—anxiety about somatic reactions during dental treatment e.g. fainting, panic attack, heart attack
- Type 3: Generalized anxiety—nervous person in general
- Type 4: distrust of dentists—fear of the dentist
Management
Dental fear varies across a continuum, from very mild fear to severe. Therefore, in a dental setting, it is also the case where the technique and management that works for one patient might not work for another. Some individuals may require a tailored management and treatment approach.[5]
The management of people with dental fear can be done using shorter term methods such as hypnosis and general anesthetic, or longer term methods such as cognitive behavioral therapy and the development of coping skills. Short term methods have been proven to be ineffective for long-term treatment of the phobia, since many return to a pattern of treatment avoidance afterwards. Psychological approaches are more effective at maintaining regular dental care, but demand more knowledge from the dentist and motivation from the patient[3]
Similarly, distraction techniques can also be utilised to divert the patient's attention to allow them to avoid supposed negativity and be more comfortable. This can be achieved through television or movies, or a physical distraction such as focusing on another body part such as wiggling the toes or fingers.[5]
Psychocognitive
Modelling
Modelling is a form of psycho-behavioural therapy used to alleviate dental fear. Commonly used in paediatric dentistry, it involves the showing of a procedure under a simulated environment. It allows the patient to observe the behaviour of a friend, family member, or other patient when put in a similar situation, therefore, accommodating for the learning of new coping mechanisms.[5] Modelling can be presented live using a parent or actor as well as virtually through pre-recorded films.[4]
Tell-Show-Do
Tell-show-do is a common non-pharmacological practice used to manage behaviour such as dental fear, especially in paediatric dentistry.[5] The purpose of this intervention is to promote a positive attitude towards dentistry and to build a relationship with the patient to improve compliance. The patient is gradually introduced to the treatment. Firstly, the dentist “tells” the patient what the dental procedure will be using words. In ‘show’ phase, the patient is familiarized with dental treatment using demonstrations. Lastly, in ‘do’ phase, the dentist proceeds with the treatment following the same procedure and demonstrations illustrated to the patient.[11]
Behavioural techniques
A technique known as behavioral control involves the person giving a signal to the clinician when to stop the procedure. This could be simply raising a hand to let the clinician know, however, the signal that is chosen will be discussed prior. This technique provides the people with a sense of control over the appointment and as so, instills trust in the dentist.[4]
Cognitive behavioural therapy
Cognitive behavioral therapy (CBT) appears to decrease dental fear and improve the frequency people go to the dentist.[12] Other measures that may be useful include distraction, guided imagery, relaxation techniques, and music therapy.[4][13] Behavior techniques are believed to be sufficient for the majority of people with mild anxiety.[14] The quality of the evidence to support this, however, is low.[15]
Environment changes
It has been suggested that the ambience created by the dental practice can play a significant role in initiating dental fear and anxiety by triggering sensory stimuli. It has been suggested that the front of house staff, e.g. receptionist and dental nurses contribute to elicit a better cognitive and emotional experience for anxious patients by showing a positive and caring attitude and by adopting good communication techniques. [5] Anxious patients should not be made to wait too long in waiting rooms, so that they have less time to recall and absorb negative feelings. There is some small evidence that the waiting areas with soft music playing and dimmer lights and cooler in temperature produces a more calming effect. It as also been stipulated that masking strong clinical smells like eugenol with more pleasant smells can help to reduce anxiety, however this is more likely to be effective in moderate rather than severe anxiety.[5]
Hypnosis
Hypnosis may be useful in certain people.[4] Hypnosis may improve a person's level of cooperation and decrease gagging.[16]
Progressive muscle relaxation
Ideally done in a sitting position, this relaxation technique for certain muscle groups can be implemented in the waiting room. The major muscles groups include
- feet, calves, thighs, and buttocks
- hands, forearms, and biceps
- chest, stomach, and lower back; and
- head, face, throat, and shoulders [5]
The steps according to Edmund Jacobson are as follows:
- Gently inhale, hold and exhale, being aware of the rise and fall of the chest.
- Slightly extend and stretch toes towards knees, hold briefly and then let go. Recognize the difference in sensation.
- Press heels of feet into the floor, hold and let go.
- Press knees together hold briefly before letting them drift apart. Be aware of the change.
- Squeeze buttocks together, hold before letting go.
- Pull in stomach muscles towards the spine, hold briefly before releasing. Feel the difference.
- Gently pull shoulders towards ears, enough to feel some tension in them, hold briefly before letting go.
- Press upper arms and elbows into sides of the body, hold and then let go. Recognize a difference in feeling.
- Gently clench hands, hold and let go.
- Extend head forward slightly, hold briefly before releasing the tension and allowing for the head to return to the resting position.
- Press the lips together before letting go until they are barely touching. Purse lips and let go, feeling the tension being let go.
- Push the tongue to the roof of the mouth, hold briefly before letting it drop loosely.[5]
Systematic desensitisation
Desensitisation in dentistry refers to the gradual exposure of a new procedure to the patient in order to calm their anxiety. It is based on the principle that a patient can overcome their anxiety if they are gradually exposed to the feared stimuli, whether imagined or real, in a controlled and systematic way. Exposure to the feared stimuli or situation is recognised as a central treatment component for specific phobias.[17][18]
Medication
Pharmacological techniques to manage dental fear range from conscious sedation to general anaesthesia; these are often used and work best in conjunction with behavioural (non-pharmacological) techniques.[19]
Premedication
Premedication refers to medication given prior to initiation of dental treatment.[20] Benzodiazepines, a class of sedative drugs, are commonly used as premedication, in the form of a tablet, to aid anxiety management before dental treatment.[21] Benzodiazepines are however addictive and subject to abuse, therefore only the minimum number of tablets required should be prescribed. Patients may also be required to be accompanied to their dental appointment by an escort.[22] In the UK, temazepam used to be the drug of choice however, lately, midazolam has become much more popular. In children, a recent meta-analysis comparing oral midazolam against placebo showed some improvement in co-operation in children using midazolam.[21] One of the disadvantages of oral premedication is that it is not titratable (i.e. it is difficult to adjust the dose to control the level of sedation desired) and therefore this technique should be only be used when other titratable sedation techniques are inappropriate.[13]
Conscious sedation
Conscious sedation refers to the use of a single or combination of drugs to help relax and reduce pain during a medical or dental procedure. There are a range of techniques and drugs that can be used ; these need to be tailored to the individual need of the patient taking into account the medical history, the skill and training of the dentist/sedationist and the facilities and equipment available.
General anaesthesia
General anaesthesia for dentistry can only be carried out in a hospital setting.[23]
The use of general anaesthesia to reduce the pain and anxiety associated with dental treatment should be discouraged and general anaesthesia should be undertaken only when absolutely necessary.[5]
Epidemiology
Individuals who are highly anxious about undergoing dental treatment comprise approximately one in six of the population.[4] Middle aged women appear to have higher rates of dental anxiety compared to men.[4]
See also
References
- Seligman LD, Hovey JD, Chacon K, Ollendick TH (July 2017). "Dental anxiety: An understudied problem in youth". Clinical Psychology Review. 55: 25–40. doi:10.1016/j.cpr.2017.04.004. PMID 28478271.
- Anthonappa RP, Ashley PF, Bonetti DL, Lombardo G, Riley P (2017). "Non-pharmacological interventions for managing dental anxiety in children". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD012676.
- Moore R (1991). The Phenomenon of Dental Fear - Studies in Clinical Diagnosis, Measurement and Treatment (Ph.D. thesis). Fællestrykeriet, Aarhus University; Aarhus Denmark. doi:10.13140/rg.2.1.3647.5363/1.
- Armfield JM, Heaton LJ (December 2013). "Management of fear and anxiety in the dental clinic: a review". Australian Dental Journal. 58 (4): 390–407, quiz 531. doi:10.1111/adj.12118. PMID 24320894.
- Appukuttan DP (March 2016). "Strategies to manage patients with dental anxiety and dental phobia: literature review". Clinical, Cosmetic and Investigational Dentistry. 8: 35–50. doi:10.2147/CCIDE.S63626. PMC 4790493. PMID 27022303.
- Carter AE, Carter G, Boschen M, AlShwaimi E, George R (November 2014). "Pathways of fear and anxiety in dentistry: A review". World Journal of Clinical Cases. 2 (11): 642–53. doi:10.12998/wjcc.v2.i11.642. PMC 4233415. PMID 25405187.
- Themessl-Huber M, Freeman R, Humphris G, MacGillivray S, Terzi N (March 2010). "Empirical evidence of the relationship between parental and child dental fear: a structured review and meta-analysis". International Journal of Paediatric Dentistry. 20 (2): 83–101. doi:10.1111/j.1365-263X.2009.00998.x. PMID 20384823.
- De Jongh A, Adair P, Meijerink-Anderson M (April 2005). "Clinical management of dental anxiety: what works for whom?". International Dental Journal. 55 (2): 73–80. doi:10.1111/j.1875-595X.2005.tb00037.x. PMID 15880961.
- "The State-Trait Anxiety Inventory (STAI)". American Psychological Association. Retrieved 2019-02-19.
- Gilbert C (2014). "Chapter 6.4 - Psychological assessment of breathing problems". In Chaitow L, Dinah Bradley D, Gilbert C (eds.). Recognizing and Treating Breathing Disorders (2nd ed.). Elsevier. pp. 129–136. doi:10.1016/b978-0-7020-4980-4.00011-3. ISBN 9780702049804.
- sitecore\lewis.ashman@rcseng.ac.uk. "Non-pharmacological Behaviour Management". Royal College of Surgeons. Retrieved 2020-01-30.
- Newton T, Asimakopoulou K, Daly B, Scambler S, Scott S (September 2012). "The management of dental anxiety: time for a sense of proportion?". British Dental Journal. 213 (6): 271–4. doi:10.1038/sj.bdj.2012.830. PMID 22996472.
- Ibbetson R, Blayney M, Rookes V, Cowpe J, Craig D, Felix D, et al. (Intercollegiate Advisory Committee for Sedation in Dentistry) (2015). Standards for Conscious Sedation in the Provision of Dental Care (PDF). United Kingdom: RCS Publications. p. 11. OCLC 915494772.
- Department of Health. Salaried Primary Dental Care Services: Toolkit for Commissioners. p9. London: Department of Health, 2009
- Wide Boman U, Carlsson V, Westin M, Hakeberg M (June 2013). "Psychological treatment of dental anxiety among adults: a systematic review". European Journal of Oral Sciences. 121 (3 Pt 2): 225–34. doi:10.1111/eos.12032. PMID 23659254.
- Allison N (October 2015). "Hypnosis in modern dentistry: Challenging misconceptions". Faculty Dental Journal. 6 (4): 172–175. doi:10.1308/rcsfdj.2015.172.
- ten Berg M (February 2008). "Dental fear in children: clinical consequences. Suggested behaviour management strategies in treating children with dental fear". European Archives of Paediatric Dentistry. 9 Suppl 1 (S1): 41–6. doi:10.1007/BF03262655. PMID 18328248.
- Klinberg G (February 2008). "Dental anxiety and behaviour management problems in paediatric dentistry--a review of background factors and diagnostics". European Archives of Paediatric Dentistry. 9 Suppl 1 (S1): 11–5. doi:10.1007/BF03262650. PMID 18328243.
- Milgrom P, Heaton LJ (January 2007). "Enhancing sedation treatment for the long- term: pre-treatment behavioural exposure". SAAD Digest. 23: 29–34. PMID 17265912.
- "BNF is only available in the UK". NICE. Retrieved 2020-02-19.
- Ashley PF, Chaudhary M, Lourenço-Matharu L (December 2018). "Sedation of children undergoing dental treatment". The Cochrane Database of Systematic Reviews. 12: CD003877. doi:10.1002/14651858.CD003877.pub5. PMC 6517004. PMID 30566228. Retrieved 2020-02-19.
- Richards D (June 2012). "SDCEP Dental Prescribing app". Evidence-Based Dentistry. 13 (2): 61–2. doi:10.1038/sj.ebd.6400867. PMID 22722422.
- Lim MA, Borromeo GL (June 2017). "The use of general anesthesia to facilitate dental treatment in adult patients with special needs". Journal of Dental Anesthesia and Pain Medicine. 17 (2): 91–103. doi:10.17245/jdapm.2017.17.2.91. PMC 5564153. PMID 28879336.