Cystine/glutamate transporter
Cystine/glutamate transporter is an antiporter that in humans is encoded by the SLC7A11 gene.[5][6][7]
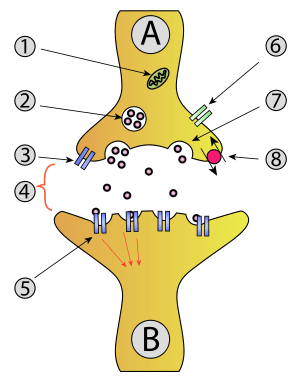
The SLC7A11 gene codes for a sodium-independent cystine-glutamate antiporter that is chloride dependent, known as system Xc- or xCT. It regulates synaptic activity by stimulating extrasynaptic receptors and performs nonvesicular glutamate release. This gene is highly expressed by astrocytes and couples the uptake of one molecule of cystine with the release of one molecule of glutamate. The dimer cystine gets taken up by glial cells and the monomer of cystine, cysteine, is taken up by neurons. The expression of Xc- was detected throughout the brain with higher expression found in the basolateral amygdala, the Retina and the prefrontal cortex. The inhibition of system Xc- has been found to alter a number of behaviors, which suggests that it plays a key role in excitatory signaling.
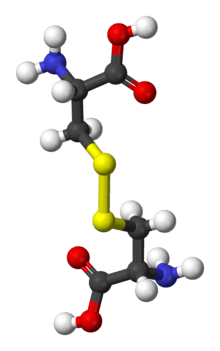
Structure
SLC7A11 is a member of a heterodimeric Na+-independent anionic amino acid transport system highly specific for cystine and glutamate. This antiporter imports cystine and exports glutamate, which are both amino acids. An antiporter functions with a one-to-one counter-transport, which is when one substance is transported across the membrane at the same time another substance is transported across the membrane in the opposite direction. The antiporter is a heterodimeric amino acid transporter.[8] The structure of this protein includes two chains: a specific light chain, xCT, and a heavy chain, 4F2, which are linked by a disulfide bridge.[9] The xCT chain has 12 transmembrane domains consisting of 501 amino acids, and the 4F2 chain appears to be highly conserved among transporters. The human xCT has an 89% similarity of amino acids to a mouse xCT. The complementary DNA, cDNA, has a total of 9648 base pairs. The SLC7A11 gene has been found not only in the brain, but has also been found to be expressed in the spinal cord, pancreas, and in glioma cells.[10][11]
Regulation
There are many mechanisms that exist to regulate the expression of system Xc-, although it is not the sole determinate of extracellular glutamate or intracellular glutathione. An example is amino acid deprivation, which triggers up regulation of the transporter. A key regulator is extracellular glutamate; when it becomes excessive, it goes from an excitatory transmitter to an excitotoxin.[10] The inhibition of uptake of extracellular cystine into cells leads to decreased levels of intracellular glutathione which leads to ferroptosis.[12][13] This regulation may be done through Excitatory Amino Acid Transporters (EAATs), which decrease extracellular glutamate and increase intracellular glutamate in astrocytes. When looking at its structure, xCT seems to be the main determinant for the system's activity. Glutamate and cystine can be transported in both directions, but, generally, more cystine is imported and more glutamate is exported. Extracellular glutamate acts as a competitive inhibitor for cystine uptake via system Xc-.
Glutamate
There is a copious amount of glutamate in mammalian cells. Glutamate is necessary for excitatory signaling between neurons. The release must be highly organized, due to the large amounts of glutamate at the synaptic cleft, and the fact that it is released at high speeds. This mechanism of release at the synaptic cleft is partially controlled through the active transport of glutamate out of astrocytes by system Xc-. This release also has a physiological role in the regulation of glutamate metabotropic receptors and control of other neurotransmitters.[11]
It has been demonstrated that, in the embryonary retina, Xc- exchanger is responsible for 50% of total glutamate uptake, representing a Sodium-Independent system within this tissue. The high activity of Xc- in the retina is correlated to a neuroprotective role, once it can take up excessive extracellular glutamate and provide precursors for the synthesis of Glutathione.[14]
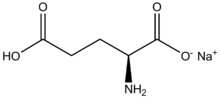
Cystine
Cystine is a dimer consisting of two cysteine molecules and the formation of a disulfide bond. This amino acid is a rate limiting substrate used in the SLC7A11 cystine/glutamate transporter and is usually imported into the cell. Cysteine-158 is specifically used in the formation of the disulfide bridge for the protein structure of system Xc-.[10] There are neurotoxins, such as BMAA, that can prevent the intake of cystine, which can lead to decreased extracellular glutamate levels and an increase in oxidative stress.[11]
Pharmacological Inhibition
System Xc- can be inhibited by many small molecules. Excess amounts of the endogenous substrate glutamate inhibits the function of system Xc-. Synthetic small molecules such as erastin, sulfasalazine, and sorafenib can inhibit system Xc- function and induce ferroptosis.[12]
Clinical applications
Many central nervous system (CNS) disorders are due to a dysfunction in glutamate signaling. Glutamate is transported via EAATs and system Xc-. If either of these transporters are impaired, it could result in a disruption in glutamate homeostasis and lead to a variety of CNS disorders[15]
Drug addiction
It has been found that cocaine produces a decrease in Cystine-Glutamate exchange via system Xc-, leading to a decrease in basal, extra synaptic glutamate levels in the nucleus accumbens core (NAcc) region of the brains of cocaine-withdrawn rats. It has also been observed in withdrawn rats that a decrease in Group 2 mGluR inhibition of vesicular release, most likely due to the decrease in extrasynaptic glutamate levels, leads to an increase in cocaine-evoked glutamate signaling in their NAcc.[15] An infusion of cysteine in the NAcc of withdrawn rats leads to an increase in extrasynaptic glutamate, near the levels of the control rats, and prevents an increase in synaptic glutamate signaling after a cocaine injection. These findings suggest there is a decrease in system Xc- activity in cocaine-withdrawn rats. It has also been found that cocaine increases glutamate signaling in the synaptic cleft, further supporting this conclusion.[15]
Administration of the cysteine prodrugs N-acetylcysteine or L-2-oxothiazolidine-4-carboxylate blocks cocaine reinstatement in rats.[15] N-acetylcysteine has been shown to decrease drug-seeking behavior for nicotine and heroin as well. However, N-acetylcysteine does not alter the cocaine-induced rush or euphoria; it only causes a reduction in drug-seeking behavior. N-acetylcysteine works by increasing levels of cysteine in cells, leading to an increase in system Xc- activity. This increase in system Xc- activity leads to an increase in extrasynaptic glutamate, causing stimulation of Group 2 mGluRs and an inhibition of synaptic release of glutamate. Cysteine prodrugs also lead to an increase in antioxidant properties by increasing levels of glutathione. Increased levels of glutathione lead to a lower toxicity of methamphetamine and alcohol, and cause a decrease in tumor formation after chronic smoking.[15] N-acetylcysteine has been shown to decrease cravings and use of cocaine and tobacco, as well as other compulsive behaviors such as gambling and trichotillomania.[15]
Repeated administration of cocaine causes disruptions in glutamate homeostasis that lead to a decrease in function of EAATs. It is also possible that glutamate is diffusing from surrounding synapses and is stimulating extrasynaptic receptors. All of these factors may be leading to the disruptions in glutamate signaling that are associated with drug addiction.
Schizophrenia
It has been proposed that schizophrenia may be due to an increase or a decrease in glutamate signaling, leading to abnormal excitatory signaling in the prefrontal cortex region of the brain.[15] Glutamate release by astrocytes has been linked to the synchrony of neurons in the hippocampus and cortex. A decrease in system Xc- activity may result in an increase in synaptic glutamate and a decrease in extrasynaptic glutamate. Administration of N-acetylcysteine leads to an increase in extrasynaptic NMDA receptor activation, suggesting that glutamate released from system Xc- may cause the activation of extrasynaptic NMDA receptors. A decrease in system Xc- activity may cause a decrease in the activation of extrasynaptic NMDA receptors due to either a decrease in extrasynaptic Glutamate levels or a decrease in glutathione levels after the decrease in cystine transport. On the other hand, a decrease in system Xc- activity may lead to an increase in the activation of synaptic NMDA receptors due to the decrease in activation of Group 2 mGluRs. A decrease in nonvesicular release of glutamate leads to an increase in expression of postsynaptic glutamate receptors, such as NMDA receptors. A disruption in nonvesicular glutamate release may affect synapse formation, lead to altered release of neurotransmitters, and could even disturb cortical migration during development. All of these seem to be associated with schizophrenia.[15]
An increase in the expression of Group 2 mGluRs, which could arise from a chronic under stimulation of these receptors, has been associated with schizophrenia. An increase in levels of system Xc- has also been found in postmortem schizophrenia patients, indicating that there may have been a decrease in net function of these receptors as well, leading to greater expression. It has been observed that Schizophrenia patients have a decreased level of glutathione in their prefrontal cortex, further supporting the conclusion that system Xc- may not be functioning properly.
Clinical trials have shown therapeutic potential for N-acetylcysteine in treating schizophrenia. Again, changes in EAATs due to disruptions in Glutamate homeostasis may also be involved.
Recent study showed that mRNA expression levels of both SLC3A2 and SLC7A11 in WBCs of schizophrenia patients are lower than that of healthy individuals. The finding supports the hypo-glutamatergic neurotransmission hypothesis in schizophrenia.[16]
Neurodegenerative disorders
The release of glutamate by system Xc- may lead to excitotoxicity, which is initiated by extrasynaptic NMDA receptors and can cause neuronal death.[17][18] It has been observed that glutamate released from microglia leads to oligodendrocyte death in culture and in the rat optic nerve.[15] However, an increase in system Xc- activity also has a protective effect by increasing levels of glutathione. Oxidative stress has been shown to lead to an increase in system Xc- expression, therefore there must be a balance between the positive protective effects of increased glutathione levels and the negative excitotoxicity effects of increased extrasynaptic glutamate levels.
Gliomas
A glioma is essentially a glial-derived tumor. These can be induced by an increase in glutamate levels due to an increase in system Xc- activity. Using inhibitors of system Xc- as a treatment for gliomas is currently under active investigation.[15]
Amyotrophic lateral sclerosis
It has been shown that amyotrophic lateral sclerosis (ALS) is clearly linked to changes in glutamate signaling and glutathione levels; there is also an astrocytic component linked to the disease. All of these factors suggest that a dysfunction in system Xc- may contribute to ALS. It has been observed that an increase in the expression of Nrf2, a transcription factor for system Xc-, leads to a protective effect in mice with ALS symptoms.[15]
Alzheimer's
There is indirect evidence to suggest that system Xc- might be upregulated in Alzheimer's patients.[15] It has been found in Alzheimer's patients that there is an increase in phosphorylation of the alpha subunit of eukaryotic initiation factor 2 and in expression of transcription factor 4, both of which increase system Xc- expression.[15] It has also been shown that administration of N-acetylcysteine leads to a significant improvement in certain cognitive tasks for Alzheimer's patients.[15]
Parkinson's disease
Parkinson's disease may be due to mitochondrial dysfunction or oxidative stress, both of which could be caused by a decrease in glutathione levels. Administration of N-acetylcysteine has been shown to counter age-related damage to mitochondria. The therapeutic effects of N-acetylcysteine in the treatment of Parkinson's disease has not been examined yet, though there is a clinical trial that is currently ongoing.[15]
Neurotoxins
There is evidence that system Xc- may serve as an entry point for neurotoxins and viruses.[15] β-N-methyl-L-alanine (BMAA) is an environmental neurotoxin that can act on system Xc- and inhibit cystine uptake. This leads to a decrease in glutathione levels and an increase in oxidative stress. BMAA can also be transported by system Xc- and lead to an increase in glutamate release and an increase in excitotoxicity. Therefore, BMAA prevents the positive effects of cystine uptake and creates the negative effects of increasing glutamate release.[15]
References
- GRCh38: Ensembl release 89: ENSG00000151012 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000027737 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Sato H, Tamba M, Ishii T, Bannai S (April 1999). "Cloning and expression of a plasma membrane cystine/glutamate exchange transporter composed of two distinct proteins". The Journal of Biological Chemistry. 274 (17): 11455–8. doi:10.1074/jbc.274.17.11455. PMID 10206947.
- Wang H, Tamba M, Kimata M, Sakamoto K, Bannai S, Sato H (June 2003). "Expression of the activity of cystine/glutamate exchange transporter, system x(c)(-), by xCT and rBAT". Biochemical and Biophysical Research Communications. 305 (3): 611–8. doi:10.1016/S0006-291X(03)00808-8. PMID 12763038.
- "Entrez Gene: SLC7A11 solute carrier family 7, (cationic amino acid transporter, y+ system) member 11".
- Lutgen V, Resch J, Qualmann K, Raddatz NJ, Panhans C, Olander EM, Kong L, Choi S, Mantsch JR, Baker DA (December 2014). "Behavioral assessment of acute inhibition of system xc (-) in rats". Psychopharmacology. 231 (24): 4637–47. doi:10.1007/s00213-014-3612-4. PMC 4474164. PMID 24828877.
- Lewerenz J, Maher P, Methner A (January 2012). "Regulation of xCT expression and system x (c) (-) function in neuronal cells". Amino Acids. 42 (1): 171–9. doi:10.1007/s00726-011-0862-x. PMID 21369940.
- Lewerenz J, Hewett SJ, Huang Y, Lambros M, Gout PW, Kalivas PW, Massie A, Smolders I, Methner A, Pergande M, Smith SB, Ganapathy V, Maher P (February 2013). "The cystine/glutamate antiporter system x(c)(-) in health and disease: from molecular mechanisms to novel therapeutic opportunities". Antioxidants & Redox Signaling. 18 (5): 522–55. doi:10.1089/ars.2011.4391. PMC 3545354. PMID 22667998.
- Bridges RJ, Natale NR, Patel SA (January 2012). "System xc⁻ cystine/glutamate antiporter: an update on molecular pharmacology and roles within the CNS". British Journal of Pharmacology. 165 (1): 20–34. doi:10.1111/j.1476-5381.2011.01480.x. PMC 3252963. PMID 21564084.
- Dixon SJ, Patel DN, Welsch M, Skouta R, Lee ED, Hayano M, Thomas AG, Gleason CE, Tatonetti NP, Slusher BS, Stockwell BR (May 2014). "Pharmacological inhibition of cystine-glutamate exchange induces endoplasmic reticulum stress and ferroptosis". eLife. 3: e02523. doi:10.7554/eLife.02523. PMC 4054777. PMID 24844246.
- Cao JY, Dixon SJ (June 2016). "Mechanisms of ferroptosis". Cellular and Molecular Life Sciences. 73 (11–12): 2195–209. doi:10.1007/s00018-016-2194-1. PMC 4887533. PMID 27048822.
- Oliveira KR, Herculano AM, Crespo-López ME, do Nascimento JL (January 2010). "Pharmacological characterization of glutamate Na+-independent transport in retinal cell cultures: implications in the glutathione metabolism". Neurochemistry International. 56 (1): 59–66. doi:10.1016/j.neuint.2009.09.002. PMID 19751785.
- Bridges R, Lutgen V, Lobner D, Baker DA (July 2012). "Thinking outside the cleft to understand synaptic activity: contribution of the cystine-glutamate antiporter (System xc-) to normal and pathological glutamatergic signaling". Pharmacological Reviews. 64 (3): 780–802. doi:10.1124/pr.110.003889. PMC 3400835. PMID 22759795.
- Lin CH, Lin PP, Lin CY, Lin CH, Huang CH, Huang YJ, Lane HY (January 2016). "Decreased mRNA expression for the two subunits of system xc(-), SLC3A2 and SLC7A11, in WBC in patients with schizophrenia: Evidence in support of the hypo-glutamatergic hypothesis of schizophrenia". Journal of Psychiatric Research. 72: 58–63. doi:10.1016/j.jpsychires.2015.10.007. PMID 26540405.
- Hardingham GE, Fukunaga Y, Bading H (May 2002). "Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB shut-off and cell death pathways". Nature Neuroscience. 5 (5): 405–14. doi:10.1038/nn835. PMID 11953750.
- Bading H (March 2017). "Therapeutic targeting of the pathological triad of extrasynaptic NMDA receptor signaling in neurodegenerations". The Journal of Experimental Medicine. 214 (3): 569–578. doi:10.1084/jem.20161673. PMC 5339681. PMID 28209726.
Further reading
- Bridges CC, Kekuda R, Wang H, Prasad PD, Mehta P, Huang W, Smith SB, Ganapathy V (January 2001). "Structure, function, and regulation of human cystine/glutamate transporter in retinal pigment epithelial cells". Investigative Ophthalmology & Visual Science. 42 (1): 47–54. PMID 11133847.
- Sato H, Tamba M, Kuriyama-Matsumura K, Okuno S, Bannai S (2001). "Molecular cloning and expression of human xCT, the light chain of amino acid transport system xc-". Antioxidants & Redox Signaling. 2 (4): 665–71. doi:10.1089/ars.2000.2.4-665. PMID 11213471.
- Shih AY, Murphy TH (April 2001). "xCt cystine transporter expression in HEK293 cells: pharmacology and localization". Biochemical and Biophysical Research Communications. 282 (5): 1132–7. doi:10.1006/bbrc.2001.4703. PMID 11302733.
- Kim JY, Kanai Y, Chairoungdua A, Cha SH, Matsuo H, Kim DK, Inatomi J, Sawa H, Ida Y, Endou H (June 2001). "Human cystine/glutamate transporter: cDNA cloning and upregulation by oxidative stress in glioma cells". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1512 (2): 335–44. doi:10.1016/S0005-2736(01)00338-8. PMID 11406111.
- Bassi MT, Gasol E, Manzoni M, Pineda M, Riboni M, Martín R, Zorzano A, Borsani G, Palacín M (May 2001). "Identification and characterisation of human xCT that co-expresses, with 4F2 heavy chain, the amino acid transport activity system xc-". Pflügers Archiv. 442 (2): 286–96. doi:10.1007/s004240100537. PMID 11417227.
- Sasaki H, Sato H, Kuriyama-Matsumura K, Sato K, Maebara K, Wang H, Tamba M, Itoh K, Yamamoto M, Bannai S (November 2002). "Electrophile response element-mediated induction of the cystine/glutamate exchange transporter gene expression". The Journal of Biological Chemistry. 277 (47): 44765–71. doi:10.1074/jbc.M208704200. PMID 12235164.
- Jiménez-Vidal M, Gasol E, Zorzano A, Nunes V, Palacín M, Chillarón J (March 2004). "Thiol modification of cysteine 327 in the eighth transmembrane domain of the light subunit xCT of the heteromeric cystine/glutamate antiporter suggests close proximity to the substrate binding site/permeation pathway". The Journal of Biological Chemistry. 279 (12): 11214–21. doi:10.1074/jbc.M309866200. PMID 14722095.
- Gasol E, Jiménez-Vidal M, Chillarón J, Zorzano A, Palacín M (July 2004). "Membrane topology of system xc- light subunit reveals a re-entrant loop with substrate-restricted accessibility". The Journal of Biological Chemistry. 279 (30): 31228–36. doi:10.1074/jbc.M402428200. PMID 15151999.
- Bridges CC, Hu H, Miyauchi S, Siddaramappa UN, Ganapathy ME, Ignatowicz L, Maddox DM, Smith SB, Ganapathy V (September 2004). "Induction of cystine-glutamate transporter xc- by human immunodeficiency virus type 1 transactivator protein tat in retinal pigment epithelium". Investigative Ophthalmology & Visual Science. 45 (9): 2906–14. doi:10.1167/iovs.03-1355. PMC 2735043. PMID 15326101.
- Rual JF, Venkatesan K, Hao T, Hirozane-Kishikawa T, Dricot A, Li N, Berriz GF, Gibbons FD, Dreze M, Ayivi-Guedehoussou N, Klitgord N, Simon C, Boxem M, Milstein S, Rosenberg J, Goldberg DS, Zhang LV, Wong SL, Franklin G, Li S, Albala JS, Lim J, Fraughton C, Llamosas E, Cevik S, Bex C, Lamesch P, Sikorski RS, Vandenhaute J, Zoghbi HY, Smolyar A, Bosak S, Sequerra R, Doucette-Stamm L, Cusick ME, Hill DE, Roth FP, Vidal M (October 2005). "Towards a proteome-scale map of the human protein-protein interaction network". Nature. 437 (7062): 1173–8. doi:10.1038/nature04209. PMID 16189514.
- Kaleeba JA, Berger EA (March 2006). "Kaposi's sarcoma-associated herpesvirus fusion-entry receptor: cystine transporter xCT". Science. 311 (5769): 1921–4. doi:10.1126/science.1120878. PMID 16574866.
- Olsen JV, Blagoev B, Gnad F, Macek B, Kumar C, Mortensen P, Mann M (November 2006). "Global, in vivo, and site-specific phosphorylation dynamics in signaling networks". Cell. 127 (3): 635–48. doi:10.1016/j.cell.2006.09.026. PMID 17081983.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.