Steroid ester
A steroid ester is an ester of a steroid.[1][2] They include androgen esters, estrogen esters, progestogen esters, and corticosteroid esters.[1] Steroid esters may be naturally occurring/endogenous like DHEA sulfate or synthetic like estradiol valerate.[1][2] Esterification is useful because it is often able to render the parent steroid into a prodrug of itself with altered chemical properties such as improved metabolic stability, water solubility, and/or lipophilicity.[2] This, in turn, can enhance pharmacokinetics, for instance by improving the steroid's bioavailability and/or conferring depot activity and hence an extended duration with intramuscular or subcutaneous injection.[1][3]
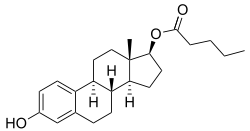
Esterification of steroids with fatty acids was developed to prolong the duration of effect of steroid hormones.[4] By 1957, more than 500 steroid esters had been synthesized, most frequently of androgens.[4] The longer the fatty acid chain, up to a certain optimal length, the longer the duration when prepared as an oil solution and injected.[4] Across a chain length range of 6 to 12 carbon atoms, a length of 9 or 10 carbon atoms (nonanoate or decanoate ester) was found to be optimal in rodents in the case of testosterone esters.[4] Fatty acid esters increase the lipophilicity of steroids, with longer fatty acids resulting in greater lipophilicity.[4] The greater solubility in oil allows the steroid esters to be dissolved in a smaller oil volume, thereby allowing for larger doses with intramuscular injection.[4] In addition, the greater the lipophilicity of the steroid, as measured by the octanol/water partition coefficient (logP), the slower its release from the oily depot at the injection site and the longer its duration.[5]
Steroid esters can also be prepared as crystalline aqueous suspensions.[4] Aqueous suspensions of steroid crystals result in prolongation of duration with intramuscular injection similarly to oil solutions.[4] The duration is longer than that of oil solutions, intermediate between oil solutions and subcutaneous pellet implants.[4] The sizes of crystals in suspensions varies and can range from 0.1 μm to some hundreds of μm.[6] The duration of crystalline steroid suspensions increases directly with the size of the crystals.[4][6] However, crystalline suspensions have an irritating effect in the body, and intramuscular injections of crystalline steroid suspensions result in painful local reactions.[4][6] These reactions worsen with larger crystals, and for this reason, crystal sizes must be limited to minimize local reactions.[4][6] Particle sizes of more than 300 μg in the case of estradiol benzoate by intramuscular injection have been found to be too painful for use.[6]
In some cases, crystalline steroid suspensions are used not for prolongation of effect, but because the solubility of the steroid result in this preparation being the only practical way to deliver the steroid in a reasonable injection volume.[4][6] Examples include cortisone acetate and hydrocortisone and its esters.[6] A requirement of long-lasting crystalline steroid administration is that the steroid be sufficiently water-insoluble, so that it dissolves slowly and thereby attains a prolonged therapeutic effect.[4] The crystals in suspensions can sometimes clump together or aggregate and grow in size.[6][4] This can be avoided by careful formulation.[6][4] Crystalline suspensions of steroids are prepared either by precipitation or by dispersing finely divided material in an aqueous suspension medium.[6] Desired particle size can be achieved by grinding, for instance through the use of an atomizer.[6]
Adolf Butenandt reported in 1932 that estrone benzoate in oil solution had a prolonged duration with injection in animals.[7][8][9] No such prolongation of action occurred if it was given by intravenous injection.[8] Estradiol benzoate was synthesized in 1933 and was marketed for use the same year.[10][11][12]
Sulfur-based esters
Certain sulfur-based steroid esters have a sulfamate or sulfonamide moiety as the ester, typically at the C3 and/or C17β positions. Like many other steroid esters, they are prodrugs. Unlike other steroid esters however, they bypass first-pass metabolism with oral administration and have high oral bioavailability and potency, abolished first-pass hepatic impact, and long elimination half-lives and durations of action. They are under development for potential clinical use. Examples include the estradiol esters estradiol sulfamate (E2MATE; also a potent steroid sulfatase inhibitor) and EC508 (estradiol 17β-(1-(4-(aminosulfonyl)benzoyl)-L-proline)),[13][14] the testosterone ester EC586 (testosterone 17β-(1-((5-(aminosulfonyl)-2-pyridinyl)carbonyl)-L-proline)),[14] and sulfonamide esters of levonorgestrel and etonogestrel.[15]
See also
References
- Vermeulen A (1975). "Longacting steroid preparations". Acta Clin Belg. 30 (1): 48–55. doi:10.1080/17843286.1975.11716973. PMID 1231448.
- Valentino Stella; Ronald Borchardt; Michael Hageman; Reza Oliyai, Hans Maag, Jefferson Tilley (12 March 2007). Prodrugs: Challenges and Rewards. Springer Science & Business Media. pp. 220–. ISBN 978-0-387-49782-2.CS1 maint: multiple names: authors list (link)
- William N. Taylor, M.D. (16 January 2002). Anabolic Steroids and the Athlete, 2d ed. McFarland. pp. 39–. ISBN 978-0-7864-1128-3.
- Edkins, Robert Patrick (1959). "The Modification of the Duration of Drug Action". Journal of Pharmacy and Pharmacology. 11 (S1): 54T–66T. doi:10.1111/j.2042-7158.1959.tb10412.x. ISSN 0022-3573.
- Florence, Alexander T. (2011). "A Short History of Controlled Drug Release and an Introduction". Controlled Release in Oral Drug Delivery. pp. 1–26. doi:10.1007/978-1-4614-1004-1_1. ISBN 978-1-4614-1003-4.
- Polderman J (February 1962). "Suspensions in pharmaceutical practice". Boll Chim Farm. 101 (12): 105–22. doi:10.1093/ajhp/19.12.611. PMID 14487508.
- A. Labhart (6 December 2012). Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. pp. 512–. ISBN 978-3-642-96158-8.
- Parkes AS (February 1938). "Effective Absorption of Hormones". Br Med J. 1 (4024): 371–3. doi:10.1136/bmj.1.4024.371. PMC 2085798. PMID 20781252.
- Butenandt, Adolf; Störmer, Inge (1932). "Über isomere Follikelhormone. Untersuchungen über das weibliche Sexualhormon, 7. Mitteilung" [About isomeric follicle hormones. Studies on the female sex hormone, 7th communication.]. Hoppe-Seyler's Zeitschrift für physiologische Chemie. 208 (4): 129–148. doi:10.1515/bchm2.1932.208.4.129. ISSN 0018-4888.
- Michael Oettel; Ekkehard Schillinger (6 December 2012). Estrogens and Antiestrogens I: Physiology and Mechanisms of Action of Estrogens and Antiestrogens. Springer Science & Business Media. pp. 8–. ISBN 978-3-642-58616-3.
- Miescher K, Scholz C, Tschopp E (1938). "The activation of female sex hormones: Mono-esters of alpha-oestradiol". Biochem. J. 32 (8): 1273–80. doi:10.1042/bj0321273b. PMC 1264184. PMID 16746750.
- Kaufman, C. (1933). "Die Behandlung der Amenorrhöe mit Hohen Dosen der Ovarialhormone". Klinische Wochenschrift. 12 (40): 1557–1562. doi:10.1007/BF01765673. ISSN 0023-2173.
- Elger W, Wyrwa R, Ahmed G, Meece F, Nair HB, Santhamma B, Killeen Z, Schneider B, Meister R, Schubert H, Nickisch K (January 2017). "Estradiol prodrugs (EP) for efficient oral estrogen treatment and abolished effects on estrogen modulated liver functions". J. Steroid Biochem. Mol. Biol. 165 (Pt B): 305–311. doi:10.1016/j.jsbmb.2016.07.008. PMID 27449818.
- Ahmed G, Elger W, Meece F, Nair HB, Schneider B, Wyrwa R, Nickisch K (October 2017). "A prodrug design for improved oral absorption and reduced hepatic interaction". Bioorg. Med. Chem. 25 (20): 5569–5575. doi:10.1016/j.bmc.2017.08.027. PMID 28886996.
- Meece FA, Ahmed G, Nair H, Santhamma B, Tekmal RR, Zhao C, Pollok NE, Lara J, Shaked Z, Nickisch K (September 2018). "Esters of levonorgestrel and etonogestrel intended as single, subcutaneous-injection, long-lasting contraceptives". Steroids. 137: 47–56. doi:10.1016/j.steroids.2018.07.010. PMC 6137153. PMID 30086356.
Further reading
- Vermeulen A (1975). "Longacting steroid preparations". Acta Clin Belg. 30 (1): 48–55. doi:10.1080/17843286.1975.11716973. PMID 1231448.