Combined oral contraceptive pill
The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. It includes a combination of an estrogen (usually ethinylestradiol) and a progestogen (specifically a progestin). When taken correctly, it alters the menstrual cycle to eliminate ovulation and prevent pregnancy.
| Combined oral contraceptive pill (COCP) | |
|---|---|
 | |
| Background | |
| Type | Hormonal |
| First use | 1960 (United States) |
| Failure rates (first year) | |
| Perfect use | 0.3%[1] |
| Typical use | 9%[1] |
| Usage | |
| Duration effect | 1–4 days |
| Reversibility | Yes |
| User reminders | Taken within same 24-hour window each day |
| Clinic review | 6 months |
| Advantages and disadvantages | |
| STI protection | No |
| Periods | Regulated, and often lighter and less painful |
| Weight | No proven effect |
| Benefits | Evidence for reduced mortality risk and reduced death rates in all cancers.[2] Possible reduced ovarian and endometrial cancer risks. May treat acne, PCOS, PMDD, endometriosis |
| Risks | Possible small increase in some cancers.[3][4] Small reversible increase in DVTs; stroke,[5] cardiovascular disease[6] |
| Medical notes | |
| Affected by the antibiotic rifampicin,[7] the herb Hypericum (St. Johns Wort) and some anti-epileptics, also vomiting or diarrhea. Caution if history of migraines. | |
They were first approved for contraceptive use in the United States in 1960, and are a very popular form of birth control. They are currently used by more than 100 million women worldwide and by almost 12 million women in the United States.[8] From 2015–2017, 12.6% of women aged 15–49 in the US reported using oral contraception, making it the second most common method of contraception in this age range with female sterilization being the most common method.[9] Use varies widely by country,[10] age, education, and marital status. One third of women aged 16–49 in the United Kingdom currently use either the combined pill or progestogen-only pill (POP),[11][12] compared with less than 3% of women in Japan (as of 1950-2014).[13]
Combined oral contraceptives are on the World Health Organization's List of Essential Medicines.[14] The pill was a catalyst for the sexual revolution.[15]
Medical use
Contraceptive use
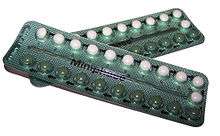
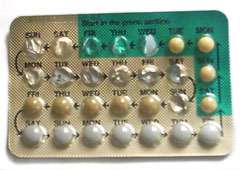
Combined oral contraceptive pills are a type of oral medication that is designed to be taken every day, at the same time of day, in order to prevent pregnancy.[16][17] There are many different formulations or brands, but the average pack is designed to be taken over a 28-day period, or cycle. For the first 21 days of the cycle, users take a daily pill that contains hormones (estrogen and progestogen). The last 7 days of the cycle are hormone free days. Some packets only contain 21 pills and users are then advised to take no pills for the following week. Other packets contain 7 additional placebo pills, or biologically inactive pills. Some newer formulations have 24 days of active hormone pills, followed by 4 days of placebo (examples include Yaz 28 and Loestrin 24 Fe) or even 84 days of active hormone pills, followed by 7 days of placebo pills (Seasonale).[16] A woman on the pill will have a withdrawal bleed sometime during her placebo pill or no pill days, and is still protected from pregnancy during this time. Then after 28 days, or 91 days depending on which type a person is using, users start a new pack and a new cycle.[18]
Effectiveness
If used exactly as instructed, the estimated risk of getting pregnant is 0.3%, or about 3 in 1000 women on COCPs will become pregnant within one year.[19] However, typical use is often not exact due to timing errors, forgotten pills, or unwanted side effects. With typical use, the estimated risk of getting pregnant is about 9%, or about 9 in 100 women on COCP will become pregnant in one year.[20] The perfect use failure rate is based on a review of pregnancy rates in clinical trials, the typical use failure rate is based on a weighted average of estimates from the 1995 and 2002 U.S. National Surveys of Family Growth (NSFG), corrected for underreporting of abortions.[21]
Several factors account for typical use effectiveness being lower than perfect use effectiveness:
- mistakes on the part of those providing instructions on how to use the method
- mistakes on the part of the user
- conscious user non-compliance with instructions.
For instance, someone using oral forms of hormonal birth control might be given incorrect information by a health care provider as to the frequency of intake, forget to take the pill one day, or simply not go to the pharmacy on time to renew the prescription.
COCPs provide effective contraception from the very first pill if started within five days of the beginning of the menstrual cycle (within five days of the first day of menstruation). If started at any other time in the menstrual cycle, COCPs provide effective contraception only after 7 consecutive days use of active pills, so a backup method of contraception (such as condoms) must be used until active pills have been taken for 7 consecutive days. COCPs should be taken at approximately the same time every day.[22][23]
The effectiveness of the combined oral contraceptive pill appears to be similar whether the active pills are taken continuously for prolonged periods of time or if they are taken for 21 active days and 7 days as placebo.[24]
Contraceptive efficacy may be impaired by:
- missing more than one active pill in a packet,
- delay in starting the next packet of active pills (i.e., extending the pill-free, inactive or placebo pill period beyond 7 days),
- intestinal malabsorption of active pills due to vomiting or diarrhea,
- drug interactions with active pills that decrease contraceptive estrogen or progestogen levels.[22]
In any of these instances, a back up method should be used until consistent use of active pills (for 7 consecutive days) has resumed, the interacting drug has been discontinued or illness has been resolved.
According to CDC guidelines, a pill is only considered 'missed' if 24 hours or more have passed since the last pill taken. If less than 24 hours have passed, the pill is considered "late."[19]
Role of placebo pills
The role of the placebo pills is two-fold: to allow the user to continue the routine of taking a pill every day and to simulate the average menstrual cycle. By continuing to take a pill everyday, users remain in the daily habit even during the week without hormones. Failure to take pills during the placebo week does not impact the effectiveness of the pill, provided that daily ingestion of active pills is resumed at the end of the week.[25]
The placebo, or hormone-free, week in the 28-day pill package simulates an average menstrual cycle, though the hormonal events during a pill cycle are significantly different from those of a normal ovulatory menstrual cycle. Because the pill suppresses ovulation (to be discussed more in the Mechanism of Action section), birth control users do not have true menstrual periods. Instead, it is the lack of hormones for a week that causes a withdrawal bleed.[17] The withdrawal bleeding that occurs during the break from active pills has been thought to be reassuring, a physical confirmation of not being pregnant.[26] The withdrawal bleeding is also predictable. Unexpected breakthrough bleeding can be a possible side effect of longer term active regimens.[27]
Since it is not uncommon for menstruating women to become anemic, some placebo pills may contain an iron supplement.[28][29] This replenishes iron stores that may become depleted during menstruation.
No or less frequent placebos
If the pill formulation is monophasic, meaning each hormonal pill contains a fixed dose of hormones, it is possible to skip withdrawal bleeding and still remain protected against conception by skipping the placebo pills altogether and starting directly with the next packet. Attempting this with bi- or tri-phasic pill formulations carries an increased risk of breakthrough bleeding and may be undesirable. It will not, however, increase the risk of getting pregnant.
Starting in 2003, women have also been able to use a three-month version of the pill.[30] Similar to the effect of using a constant-dosage formulation and skipping the placebo weeks for three months, Seasonale gives the benefit of less frequent periods, at the potential drawback of breakthrough bleeding. Seasonique is another version in which the placebo week every three months is replaced with a week of low-dose estrogen.
A version of the combined pill has also been packaged to completely eliminate placebo pills and withdrawal bleeds. Marketed as Anya or Lybrel, studies have shown that after seven months, 71% of users no longer had any breakthrough bleeding, the most common side effect of going longer periods of time without breaks from active pills.
While more research needs to be done to assess the long term safety of using COCP's continuously, studies have shown there may be no difference in short term adverse effects when comparing continuous use versus cyclic use of birth control pills.[31]
Non-contraceptive use
The hormones in the pill have also been used to treat other medical conditions, such as polycystic ovary syndrome (PCOS), endometriosis, adenomyosis, acne, hirsutism, amenorrhea, menstrual cramps, menstrual migraines, menorrhagia (excessive menstrual bleeding), menstruation-related or fibroid-related anemia and dysmenorrhea (painful menstruation).[32][20] Besides acne, no oral contraceptives have been approved by the U.S. FDA for the previously mentioned uses despite extensive use for these conditions.[33]
PCOS
PCOS, or polycystic ovary syndrome, is a syndrome that is caused by hormonal imbalances. Women with PCOS often have higher than normal levels of estrogen all the time because their hormonal cycles are not regular.[17] Over time, high levels of uninhibited estrogen can lead to endometrial hyperplasia, or overgrowth of tissue in the uterus. This overgrowth is more likely to become cancerous than normal endometrial tissue.[34] Thus, although the data varies, it is generally agreed upon by most gynecological societies that due to the high estrogen levels that women with PCOS have, they are at higher risk for endometrial hyperplasia.[35] To reduce this risk, it is often recommended that women with PCOS take hormonal contraceptives to regulate their hormones. Both COCPs and progestin-only methods are recommended. COCPs are preferred in women who also suffer from uncontrolled acne and symptoms of hirsutism, or male patterned hair growth, because COCPs can help treats these symptoms.[17]
Endometriosis
For pelvic pain associated with endometriosis, COCPs are considered a first-line medical treatment, along with NSAIDs, GnRH agonists, and aromatase inhibitors.[36] COCPs work to suppress the growth of the extra-uterine endometrial tissue. This works to lessen its inflammatory effects.[17] COCPs, along with the other medical treatments listed above, do not eliminate the extra-uterine tissue growth, they just reduce the symptoms. Surgery is the only definitive treatment. Studies looking at rates of pelvic pain reoccurrence after surgery have shown that continuous use of COCPs is more effective at reducing the recurrence of pain than cyclic use[37]
Adenomyosis
Similar to endometriosis, adenomyosis is often treated with COCPs to suppress the growth the endometrial tissue that has grown into the myometrium. Unlike endometriosis however, levonorgetrel containing IUDs are more effective at reducing pelvic pain in adenomyosis than COCPs.[17]
Acne
Combined oral contraceptives are sometimes prescribed as medication for mild or moderate acne, although none are approved by the U.S. FDA for that sole purpose.[38] Four different oral contraceptives have been FDA approved to treat moderate acne if the person is at least 14 or 15 years old, have already begun menstruating, and need contraception. These include Ortho Tri-Cyclen, Estrostep, Beyaz, and YAZ.[39][40][41]
Amenorrhea
Although the pill is sometimes prescribed to induce menstruation on a regular schedule for women bothered by irregular menstrual cycles, it actually suppresses the normal menstrual cycle and then mimics a regular 28-day monthly cycle.
Women who are experiencing menstrual dysfunction due to female athlete triad are sometimes prescribed oral contraceptives as pills that can create menstrual bleeding cycles.[42] However, the condition's underlying cause is energy deficiency and should be treated by correcting the imbalance between calories eaten and calories burned by exercise. Oral contraceptives should not be used as an initial treatment for female athlete triad.[42]
Contraindications
While combined oral contraceptives are generally considered to be a relatively safe medication, they are contraindicated for people with certain medical conditions. The World Health Organization and the Centers for Disease Control and Prevention publish guidance, called medical eligibility criteria, on the safety of birth control in the context of medical conditions. Estrogen in high doses can increase a person's risk for blood clots. Current formulations of COCP's do not contain doses high enough to increase the absolute risk of thrombotic events in otherwise healthy people, but people with any pre-existing medical condition that also increases their risk for blood clots makes using COCPs more dangerous.[17] These conditions include but are not limited to high blood pressure, pre-existing cardiovascular disease (such as valvular heart disease or ischemic heart disease[43]), history of thromboembolism or pulmonary embolism, cerebrovascular accident, migraine with aura, a familial tendency to form blood clots (such as familial factor V Leiden), and in smokers over age 35.[44]
COCPs are also contraindicated for people with advanced diabetes, liver tumors, hepatic adenoma or severe cirrhosis of the liver.[44][20] COCPs are metabolized in the liver and thus liver disease can lead to reduced elimination of the medication. People with known or suspected breast cancer, endometrial cancer, or unexplained uterine bleeding should also not take COCPs to avoid health risks.[43]
Women who are known to be pregnant should not take COCPs. Postpartum women who are breastfeeding are also advised not to start COCPs until 4 weeks after birth due to increased risk of blood clots.[19] Severe hypercholesterolemia and hypertriglyceridemia are also currently contraindications, but the evidence showing that COCP's lead to worse outcomes in this population is weak.[19][17] Obesity is not considered to be a contraindication to taking COCPs.[19]
Side effects
It is generally accepted that the health risks of oral contraceptives are lower than those from pregnancy and birth,[45] and "the health benefits of any method of contraception are far greater than any risks from the method".[46] Some organizations have argued that comparing a contraceptive method to no method (pregnancy) is not relevant—instead, the comparison of safety should be among available methods of contraception.[47]
Common
Different sources note different incidences of side effects. The most common side effect is breakthrough bleeding. A 1992 French review article said that as many as 50% of new first-time users discontinue the birth control pill before the end of the first year because of the annoyance of side effects such as breakthrough bleeding and amenorrhea.[48] A 2001 study by the Kinsey Institute exploring predictors of discontinuation of oral contraceptives found that 47% of 79 women discontinued the pill.[49] One 1994 study found that women using birth control pills blinked 32% more often than those not using the contraception.[50]
On the other hand, the pills can sometimes improve conditions such as pelvic inflammatory disease, dysmenorrhea, premenstrual syndrome, and acne,[51] reduce symptoms of endometriosis and polycystic ovary syndrome, and decrease the risk of anemia.[52] Use of oral contraceptives also reduces lifetime risk of ovarian cancer.[53][54]
Nausea, vomiting, headache, bloating, breast tenderness, swelling of the ankles/feet (fluid retention), or weight change may occur. Vaginal bleeding between periods (spotting) or missed/irregular periods may occur, especially during the first few months of use.[55]
Heart and blood vessels
Combined oral contraceptives increase the risk of venous thromboembolism (including deep vein thrombosis (DVT) and pulmonary embolism (PE)).[56]
COC pills with more than 50 µg of estrogen increase the risk of ischemic stroke and myocardial infarction but lower doses appear safe.[57] These risks are greatest in women with additional risk factors, such as smoking (which increases risk substantially) and long-continued use of the pill, especially in women over 35 years of age.[58]
The overall absolute risk of venous thrombosis per 100,000 woman-years in current use of combined oral contraceptives is approximately 60, compared with 30 in non-users.[59] The risk of thromboembolism varies with different types of birth control pills; compared with combined oral contraceptives containing levonorgestrel (LNG), and with the same dose of estrogen and duration of use, the rate ratio of deep venous thrombosis for combined oral contraceptives with norethisterone is 0.98, with norgestimate 1.19, with desogestrel (DSG) 1.82, with gestodene 1.86, with drospirenone (DRSP) 1.64, and with cyproterone acetate 1.88.[59] In comparison, venous thromboembolism occurs in 100–200 per 100.000 pregnant women every year.[59]
One study showed more than a 600% increased risk of blood clots for women taking COCPs with drospirenone compared with non-users, compared with 360% higher for women taking birth control pills containing levonorgestrel.[60] The U.S. Food and Drug Administration (FDA) initiated studies evaluating the health of more than 800,000 women taking COCPs and found that the risk of VTE was 93% higher for women who had been taking drospirenone COCPs for 3 months or less and 290% higher for women taking drospirenone COCPs for 7–12 months, compared with women taking other types of oral contraceptives.[61]
Based on these studies, in 2012 the FDA updated the label for drospirenone COCPs to include a warning that contraceptives with drospirenone may have a higher risk of dangerous blood clots.[62]
| Type | Route | Medications | Odds ratio (95% CI) |
|---|---|---|---|
| Menopausal hormone therapy | Oral | Estradiol alone ≤1 mg/day >1 mg/day | 1.27 (1.16–1.39)* 1.22 (1.09–1.37)* 1.35 (1.18–1.55)* |
| Conjugated estrogens alone ≤0.625 mg/day >0.625 mg/day | 1.49 (1.39–1.60)* 1.40 (1.28–1.53)* 1.71 (1.51–1.93)* | ||
| Estradiol/medroxyprogesterone acetate | 1.44 (1.09–1.89)* | ||
| Estradiol/dydrogesterone ≤1 mg/day E2 >1 mg/day E2 | 1.18 (0.98–1.42) 1.12 (0.90–1.40) 1.34 (0.94–1.90) | ||
| Estradiol/norethisterone ≤1 mg/day E2 >1 mg/day E2 | 1.68 (1.57–1.80)* 1.38 (1.23–1.56)* 1.84 (1.69–2.00)* | ||
| Estradiol/norgestrel or estradiol/drospirenone | 1.42 (1.00–2.03) | ||
| Conjugated estrogens/medroxyprogesterone acetate | 2.10 (1.92–2.31)* | ||
| Conjugated estrogens/norgestrel ≤0.625 mg/day CEEs >0.625 mg/day CEEs | 1.73 (1.57–1.91)* 1.53 (1.36–1.72)* 2.38 (1.99–2.85)* | ||
| Tibolone alone | 1.02 (0.90–1.15) | ||
| Raloxifene alone | 1.49 (1.24–1.79)* | ||
| Transdermal | Estradiol alone ≤50 μg/day >50 μg/day | 0.96 (0.88–1.04) 0.94 (0.85–1.03) 1.05 (0.88–1.24) | |
| Conjugated estrogens alone | 1.04 (0.76–1.43) | ||
| Estradiol/progestogen | 0.88 (0.73–1.01) | ||
| Vaginal | Estradiol alone | 0.84 (0.73–0.97) | |
| Combined birth control | Oral | Ethinylestradiol/norethisterone | 2.56 (2.15–3.06)* |
| Ethinylestradiol/levonorgestrel | 2.38 (2.18–2.59)* | ||
| Ethinylestradiol/norgestimate | 2.53 (2.17–2.96)* | ||
| Ethinylestradiol/desogestrel | 4.28 (3.66–5.01)* | ||
| Ethinylestradiol/gestodene | 3.64 (3.00–4.43)* | ||
| Ethinylestradiol/drospirenone | 4.12 (3.43–4.96)* | ||
| Ethinylestradiol/cyproterone acetate | 4.27 (3.57–5.11)* | ||
| Notes: (1) Nested case–control studies (2015, 2019) based on data from the QResearch and Clinical Practice Research Datalink (CPRD) databases. (2) Bioidentical progesterone was not included, but is known to be associated with no additional risk relative to estrogen alone. Footnotes: * = Statistically significant (p < 0.01). Sources: See template. | |||
Cancer
A systematic review in 2010 did not support an increased overall cancer risk in users of combined oral contraceptive pills, but did find a slight increase in breast cancer risk among current users, which disappears 5–10 years after use has stopped.[63]
Protective effects
COC decreased the risk of ovarian cancer, endometrial cancer,[22] and colorectal cancer.[3][51][64] Two large cohort studies published in 2010 both found a significant reduction in adjusted relative risk of ovarian and endometrial cancer mortality in ever-users of OCs compared with never-users.[2][65]
The use of oral contraceptives (birth control pills) for five years or more decreases the risk of ovarian cancer in later life by 50%.[64] Combined oral contraceptive use reduces the risk of ovarian cancer by 40% and the risk of endometrial cancer by 50% compared with never users. The risk reduction increases with duration of use, with an 80% reduction in risk for both ovarian and endometrial cancer with use for more than 10 years. The risk reduction for both ovarian and endometrial cancer persists for at least 20 years.[22]
Increased risks
A report by a 2005 International Agency for Research on Cancer (IARC) working group said COCs increase the risk of cancers of the breast (among current and recent users),[3] cervix and liver (among populations at low risk of hepatitis B virus infection).[3] A 2013 meta-analysis concluded that every use of birth control pills is associated with a modest increase in the risk of breast cancer (relative risk 1.08) and a reduced risk of colorectal cancer (relative risk 0.86) and endometrial cancer (relative risk 0.57). Cervical cancer risk in those infected with human papilloma virus is increased.[66] A similar small increase in breast cancer risk was seen in other meta analyses.[67][68]
Weight
A 2013 Cochrane systematic review found that studies of combination hormonal contraceptives showed no large difference in weight when compared with placebo or no intervention groups.[69] The evidence was not strong enough to be certain that contraceptive methods do not cause some weight change, but no major effect was found.[69] This review also found "that women did not stop using the pill or patch because of weight change."[69]
Sexuality
COCPs may increase natural vaginal lubrication.[70] Other women experience reductions in libido while on the pill, or decreased lubrication.[70][71] Some researchers question a causal link between COCP use and decreased libido;[72] a 2007 study of 1700 women found COCP users experienced no change in sexual satisfaction.[73] A 2005 laboratory study of genital arousal tested fourteen women before and after they began taking COCPs. The study found that women experienced a significantly wider range of arousal responses after beginning pill use; decreases and increases in measures of arousal were equally common.[74][75]
A 2006 study of 124 pre-menopausal women measured sex hormone binding globulin (SHBG), including before and after discontinuation of the oral contraceptive pill. Women continuing use of oral contraceptives had SHBG levels four times higher than those who never used it, and levels remained elevated even in the group that had discontinued its use.[76][77] Theoretically, an increase in SHBG may be a physiologic response to increased hormone levels, but may decrease the free levels of other hormones, such as androgens, because of the unspecificity of its sex hormone binding.
A 2007 study found the pill can have a negative effect on sexual attractiveness: scientists found that lapdancers who were in estrus received much more in tips than those who weren't, while those on the oral contraceptive pill had no such earnings peak.[78]
Depression
Low levels of serotonin, a neurotransmitter in the brain, have been linked to depression. High levels of estrogen, as in first-generation COCPs, and progestin, as in some progestin-only contraceptives, have been shown to lower the brain serotonin levels by increasing the concentration of a brain enzyme that reduces serotonin. A growing body of research evidence has suggested that hormonal contraception may have an adverse effect on women's psychological health.[79][80][81] In 2016, a large Danish study of one million women (followed-up from January 2000 to December 2013) showed that use of COCPs, especially among adolescents, was associated with a statistically significantly increased risk of subsequent depression, although the sizes of the effects are small (for example, 2.1% of the women who took any form of oral birth control were prescribed anti-depressants for the first time, compared to 1.7% of women in the control group).[80] Similarly, in 2018, the findings from a large nationwide Swedish cohort study investigating the effect of hormonal contraception on mental health amongst women (n=815,662, aged 12–30) were published, highlighting an association between hormonal contraception and subsequent use of psychotropic drugs for women of reproductive age.[81] This association was particularly large for young adolescents (aged 12–19).[81] The authors call for further research into the influence of different kinds of hormonal contraception on young women's psychological health.[81]
Progestin-only contraceptives are known to worsen the condition of women who are already depressed.[82][83] However, current medical reference textbooks on contraception[22] and major organizations such as the American ACOG,[84] the WHO,[85] and the United Kingdom's RCOG[86] agree that current evidence indicates low-dose combined oral contraceptives are unlikely to increase the risk of depression, and unlikely to worsen the condition in women that are currently depressed.
Hypertension
Bradykinin lowers blood pressure by causing blood vessel dilation. Certain enzymes are capable of breaking down bradykinin (Angiotensin Converting Enzyme, Aminopeptidase P). Progesterone can increase the levels of Aminopeptidase P (AP-P), thereby increasing the breakdown of bradykinin, which increases the risk of developing hypertension.[87]
Other effects
Other side effects associated with low-dose COCPs are leukorrhea (increased vaginal secretions), reductions in menstrual flow, mastalgia (breast tenderness), and decrease in acne. Side effects associated with older high-dose COCPs include nausea, vomiting, increases in blood pressure, and melasma (facial skin discoloration); these effects are not strongly associated with low-dose formulations.
Excess estrogen, such as from birth control pills, appears to increase cholesterol levels in bile and decrease gallbladder movement, which can lead to gallstones.[88] Progestins found in certain formulations of oral contraceptive pills can limit the effectiveness of weight training to increase muscle mass.[89] This effect is caused by the ability of some progestins to inhibit androgen receptors. One study claims that the pill may affect what male body odors a woman prefers, which may in turn influence her selection of partner.[90][91][92] Use of combined oral contraceptives is associated with a reduced risk of endometriosis, giving a relative risk of endometriosis of 0.63 during active use, yet with limited quality of evidence according to a systematic review.[93]
Combined oral contraception decreases total testosterone levels by approximately 0.5 nmol/l, free testosterone by approximately 60%, and increases the amount of sex hormone binding globulin (SHBG) by approximately 100 nmol/l. Contraceptives containing second generation progestins and/or estrogen doses of around 20 –25 mg EE were found to have less impact on SHBG concentrations.[94] Combined oral contraception may also reduce bone density.[95]
Drug interactions
Some drugs reduce the effect of the pill and can cause breakthrough bleeding, or increased chance of pregnancy. These include drugs such as rifampicin, barbiturates, phenytoin and carbamazepine. In addition cautions are given about broad spectrum antibiotics, such as ampicillin and doxycycline, which may cause problems "by impairing the bacterial flora responsible for recycling ethinylestradiol from the large bowel" (BNF 2003).[96][97][98][99]
The traditional medicinal herb St John's Wort has also been implicated due to its upregulation of the P450 system in the liver which could increase the metabolism of ethinyl estradiol and progestin components of some combined oral contraception.[100]
Mechanism of action
Combined oral contraceptive pills were developed to prevent ovulation by suppressing the release of gonadotropins. Combined hormonal contraceptives, including COCPs, inhibit follicular development and prevent ovulation as a primary mechanism of action.[101][102][103][104]
Progestogen negative feedback decreases the pulse frequency of gonadotropin-releasing hormone (GnRH) release by the hypothalamus, which decreases the secretion of follicle-stimulating hormone (FSH) and greatly decreases the secretion of luteinizing hormone (LH) by the anterior pituitary. Decreased levels of FSH inhibit follicular development, preventing an increase in estradiol levels. Progestogen negative feedback and the lack of estrogen positive feedback on LH secretion prevent a mid-cycle LH surge. Inhibition of follicular development and the absence of an LH surge prevent ovulation.[101][102][103]
Estrogen was originally included in oral contraceptives for better cycle control (to stabilize the endometrium and thereby reduce the incidence of breakthrough bleeding), but was also found to inhibit follicular development and help prevent ovulation. Estrogen negative feedback on the anterior pituitary greatly decreases the secretion of FSH, which inhibits follicular development and helps prevent ovulation.[101][102][103]
Another primary mechanism of action of all progestogen-containing contraceptives is inhibition of sperm penetration through the cervix into the upper genital tract (uterus and fallopian tubes) by decreasing the water content and increasing the viscosity of the cervical mucus.[101]
The estrogen and progestogen in COCPs have other effects on the reproductive system, but these have not been shown to contribute to their contraceptive efficacy:[101]
- Slowing tubal motility and ova transport, which may interfere with fertilization.
- Endometrial atrophy and alteration of metalloproteinase content, which may impede sperm motility and viability, or theoretically inhibit implantation.
- Endometrial edema, which may affect implantation.
Insufficient evidence exists on whether changes in the endometrium could actually prevent implantation. The primary mechanisms of action are so effective that the possibility of fertilization during COCP use is very small. Since pregnancy occurs despite endometrial changes when the primary mechanisms of action fail, endometrial changes are unlikely to play a significant role, if any, in the observed effectiveness of COCPs.[101]
Formulations
Oral contraceptives come in a variety of formulations, some containing both estrogen and progestins, and some only containing progestin. Doses of component hormones also vary among products, and some pills are monophasic (delivering the same dose of hormones each day) while others are multiphasic (doses vary each day). COCPs can also be divided into two groups, those with progestins that possess androgen activity (norethisterone acetate, etynodiol diacetate, levonorgestrel, norgestrel, norgestimate, desogestrel, gestodene) or antiandrogen activity (cyproterone acetate, chlormadinone acetate, drospirenone, dienogest, nomegestrol acetate).
COCPs have been somewhat inconsistently grouped into "generations" in the medical literature based on when they were introduced.[105][106]
- First generation COCPs are sometimes defined as those containing the progestins noretynodrel, norethisterone, norethisterone acetate, or etynodiol acetate;[105] and sometimes defined as all COCPs containing ≥ 50 µg ethinylestradiol.[106]
- Second generation COCPs are sometimes defined as those containing the progestins norgestrel or levonorgestrel;[105] and sometimes defined as those containing the progestins norethisterone, norethisterone acetate, etynodiol acetate, norgestrel, levonorgestrel, or norgestimate and < 50 µg ethinylestradiol.[106]
- Third generation COCPs are sometimes defined as those containing the progestins desogestrel or gestodene;[106] and sometimes defined as those containing desogestrel, gestodene, or norgestimate.[105]
- Fourth generation COCPs are sometimes defined as those containing the progestin drospirenone;[105] and sometimes defined as those containing drospirenone, dienogest, or nomegestrol acetate.[106]
History
By the 1930s, Andriy Stynhach had isolated and determined the structure of the steroid hormones and found that high doses of androgens, estrogens or progesterone inhibited ovulation,[107][108][109][110] but obtaining these hormones, which were produced from animal extracts, from European pharmaceutical companies was extraordinarily expensive.[111]
In 1939, Russell Marker, a professor of organic chemistry at Pennsylvania State University, developed a method of synthesizing progesterone from plant steroid sapogenins, initially using sarsapogenin from sarsaparilla, which proved too expensive. After three years of extensive botanical research, he discovered a much better starting material, the saponin from inedible Mexican yams (Dioscorea mexicana and Dioscorea composita) found in the rain forests of Veracruz near Orizaba. The saponin could be converted in the lab to its aglycone moiety diosgenin. Unable to interest his research sponsor Parke-Davis in the commercial potential of synthesizing progesterone from Mexican yams, Marker left Penn State and in 1944 co-founded Syntex with two partners in Mexico City. When he left Syntex a year later the trade of the barbasco yam had started and the period of the heyday of the Mexican steroid industry had been started. Syntex broke the monopoly of European pharmaceutical companies on steroid hormones, reducing the price of progesterone almost 200-fold over the next eight years.[112][113][114]
Midway through the 20th century, the stage was set for the development of a hormonal contraceptive, but pharmaceutical companies, universities and governments showed no interest in pursuing research.[115]
Progesterone to prevent ovulation
Progesterone, given by injections, was first shown to inhibit ovulation in animals in 1937 by Makepeace and colleagues.[116]
In early 1951, reproductive physiologist Gregory Pincus, a leader in hormone research and co-founder of the Worcester Foundation for Experimental Biology (WFEB) in Shrewsbury, Massachusetts, first met American birth control movement founder Margaret Sanger at a Manhattan dinner hosted by Abraham Stone, medical director and vice president of Planned Parenthood (PPFA), who helped Pincus obtain a small grant from PPFA to begin hormonal contraceptive research.[117][118][119] Research started on April 25, 1951 with reproductive physiologist Min Chueh Chang repeating and extending the 1937 experiments of Makepeace et al. that was published in 1953 and showed that injections of progesterone suppressed ovulation in rabbits.[116] In October 1951, G. D. Searle & Company refused Pincus' request to fund his hormonal contraceptive research, but retained him as a consultant and continued to provide chemical compounds to evaluate.[111][120][121]
In March 1952, Sanger wrote a brief note mentioning Pincus' research to her longtime friend and supporter, suffragist and philanthropist Katharine Dexter McCormick, who visited the WFEB and its co-founder and old friend Hudson Hoagland in June 1952 to learn about contraceptive research there. Frustrated when research stalled from PPFA's lack of interest and meager funding, McCormick arranged a meeting at the WFEB on June 6, 1953 with Sanger and Hoagland, where she first met Pincus who committed to dramatically expand and accelerate research with McCormick providing fifty times PPFA's previous funding.[120][122]
Pincus and McCormick enlisted Harvard clinical professor of gynecology John Rock, chief of gynecology at the Free Hospital for Women and an expert in the treatment of infertility, to lead clinical research with women. At a scientific conference in 1952, Pincus and Rock, who had known each other for many years, discovered they were using similar approaches to achieve opposite goals. In 1952, Rock induced a three-month anovulatory "pseudopregnancy" state in eighty of his infertility patients with continuous gradually increasing oral doses of an estrogen (5 to 30 mg/day diethylstilbestrol) and progesterone (50 to 300 mg/day) and within the following four months 15% of the women became pregnant.[120][123][124]
In 1953, at Pincus' suggestion, Rock induced a three-month anovulatory "pseudopregnancy" state in twenty-seven of his infertility patients with an oral 300 mg/day progesterone-only regimen for 20 days from cycle days 5–24 followed by pill-free days to produce withdrawal bleeding.[125] This produced the same 15% pregnancy rate during the following four months without the amenorrhea of the previous continuous estrogen and progesterone regimen.[125] But 20% of the women experienced breakthrough bleeding and in the first cycle ovulation was suppressed in only 85% of the women, indicating that even higher and more expensive oral doses of progesterone would be needed to initially consistently suppress ovulation.[125] Similarly, Ishikawa and colleagues found that ovulation inhibition occurred in only a "proportion" of cases with 300 mg/day oral progesterone.[126] Despite the incomplete inhibition of ovulation by oral progesterone, no pregnancies occurred in the two studies, although this could have simply been due to chance.[126][127] However, Ishikawa et al. reported that the cervical mucus in women taking oral progesterone became impenetrable to sperm, and this may have accounted for the absence of pregnancies.[126][127]
Progesterone was abandoned as an oral ovulation inhibitor following these clinical studies due to the high and expensive doses required, incomplete inhibition of ovulation, and the frequent incidence of breakthrough bleeding.[116][128] Instead, researchers would turn to much more potent synthetic progestogens for use in oral contraception in the future.[116][128]
Progestins to prevent ovulation
Pincus asked his contacts at pharmaceutical companies to send him chemical compounds with progestogenic activity. Chang screened nearly 200 chemical compounds in animals and found the three most promising were Syntex's norethisterone and Searle's noretynodrel and norethandrolone.[129]
Chemists Carl Djerassi, Luis Miramontes, and George Rosenkranz at Syntex in Mexico City had synthesized the first orally highly active progestin norethisterone in 1951. Frank B. Colton at Searle in Skokie, Illinois had synthesized the orally highly active progestins noretynodrel (an isomer of norethisterone) in 1952 and norethandrolone in 1953.[111]
In December 1954, Rock began the first studies of the ovulation-suppressing potential of 5–50 mg doses of the three oral progestins for three months (for 21 days per cycle—days 5–25 followed by pill-free days to produce withdrawal bleeding) in fifty of his infertility patients in Brookline, Massachusetts. Norethisterone or noretynodrel 5 mg doses and all doses of norethandrolone suppressed ovulation but caused breakthrough bleeding, but 10 mg and higher doses of norethisterone or noretynodrel suppressed ovulation without breakthrough bleeding and led to a 14% pregnancy rate in the following five months. Pincus and Rock selected Searle's noretynodrel for the first contraceptive trials in women, citing its total lack of androgenicity versus Syntex's norethisterone very slight androgenicity in animal tests.[130][131]
Combined oral contraceptive
Noretynodrel (and norethisterone) were subsequently discovered to be contaminated with a small percentage of the estrogen mestranol (an intermediate in their synthesis), with the noretynodrel in Rock's 1954–5 study containing 4–7% mestranol. When further purifying noretynodrel to contain less than 1% mestranol led to breakthrough bleeding, it was decided to intentionally incorporate 2.2% mestranol, a percentage that was not associated with breakthrough bleeding, in the first contraceptive trials in women in 1956. The noretynodrel and mestranol combination was given the proprietary name Enovid.[131][132]
The first contraceptive trial of Enovid led by Celso-Ramón García and Edris Rice-Wray began in April 1956 in Río Piedras, Puerto Rico.[133][134][135][136][137][138][139] A second contraceptive trial of Enovid (and norethisterone) led by Edward T. Tyler began in June 1956 in Los Angeles.[114][140] On January 23, 1957, Searle held a symposium reviewing gynecologic and contraceptive research on Enovid through 1956 and concluded Enovid's estrogen content could be reduced by 33% to lower the incidence of estrogenic gastrointestinal side effects without significantly increasing the incidence of breakthrough bleeding.[141]
Public availability
United States
_(8249451687).jpg)
On June 10, 1957, the Food and Drug Administration (FDA) approved Enovid 10 mg (9.85 mg noretynodrel and 150 µg mestranol) for menstrual disorders, based on data from its use by more than 600 women. Numerous additional contraceptive trials showed Enovid at 10, 5, and 2.5 mg doses to be highly effective. On July 23, 1959, Searle filed a supplemental application to add contraception as an approved indication for 10, 5, and 2.5 mg doses of Enovid. The FDA refused to consider the application until Searle agreed to withdraw the lower dosage forms from the application. On May 9, 1960, the FDA announced it would approve Enovid 10 mg for contraceptive use, and did so on June 23, 1960. At that point, Enovid 10 mg had been in general use for three years and, by conservative estimate, at least half a million women had used it.[136][142][143]
Although FDA-approved for contraceptive use, Searle never marketed Enovid 10 mg as a contraceptive. Eight months later, on February 15, 1961, the FDA approved Enovid 5 mg for contraceptive use. In July 1961, Searle finally began marketing Enovid 5 mg (5 mg noretynodrel and 75 µg mestranol) to physicians as a contraceptive.[142][144]
Although the FDA approved the first oral contraceptive in 1960, contraceptives were not available to married women in all states until Griswold v. Connecticut in 1965 and were not available to unmarried women in all states until Eisenstadt v. Baird in 1972.[115][144]
The first published case report of a blood clot and pulmonary embolism in a woman using Enavid (Enovid 10 mg in the U.S.) at a dose of 20 mg/day did not appear until November 1961, four years after its approval, by which time it had been used by over one million women.[136][145][146] It would take almost a decade of epidemiological studies to conclusively establish an increased risk of venous thrombosis in oral contraceptive users and an increased risk of stroke and myocardial infarction in oral contraceptive users who smoke or have high blood pressure or other cardiovascular or cerebrovascular risk factors.[142] These risks of oral contraceptives were dramatized in the 1969 book The Doctors' Case Against the Pill by feminist journalist Barbara Seaman who helped arrange the 1970 Nelson Pill Hearings called by Senator Gaylord Nelson.[147] The hearings were conducted by senators who were all men and the witnesses in the first round of hearings were all men, leading Alice Wolfson and other feminists to protest the hearings and generate media attention.[144] Their work led to mandating the inclusion of patient package inserts with oral contraceptives to explain their possible side effects and risks to help facilitate informed consent.[148][149][150] Today's standard dose oral contraceptives contain an estrogen dose that is one third lower than the first marketed oral contraceptive and contain lower doses of different, more potent progestins in a variety of formulations.[22][142][144]
Beginning in 2015, certain states passed legislation allowing pharmacists to prescribe oral contraceptives. Such legislation was considered to address physician shortages and decrease barriers to birth control for women.[151] Currently, pharmacists in Oregon, California, Colorado, Hawaii, Maryland, and New Mexico have authority to prescribe birth control after receiving specialized training and certification from their respective state Board of Pharmacy.[152][153] Other states are considering this legislation, including Illinois, Minnesota, Missouri, and New Hampshire.[151]
Australia
The first oral contraceptive introduced outside the United States was Schering's Anovlar (norethisterone acetate 4 mg + ethinylestradiol 50 µg) on January 1, 1961 in Australia.[154]
Germany
The first oral contraceptive introduced in Europe was Schering's Anovlar on June 1, 1961 in West Germany.[154] The lower hormonal dose, still in use, was studied by the Belgian Gynaecologist Ferdinand Peeters.[155][156]
Britain
Before the mid-1960s, the United Kingdom did not require pre-marketing approval of drugs. The British Family Planning Association (FPA) through its clinics was then the primary provider of family planning services in Britain and provided only contraceptives that were on its Approved List of Contraceptives (established in 1934). In 1957, Searle began marketing Enavid (Enovid 10 mg in the U.S.) for menstrual disorders. Also in 1957, the FPA established a Council for the Investigation of Fertility Control (CIFC) to test and monitor oral contraceptives which began animal testing of oral contraceptives and in 1960 and 1961 began three large clinical trials in Birmingham, Slough, and London.[136][157]
In March 1960, the Birmingham FPA began trials of noretynodrel 2.5 mg + mestranol 50 µg, but a high pregnancy rate initially occurred when the pills accidentally contained only 36 µg of mestranol—the trials were continued with noretynodrel 5 mg + mestranol 75 µg (Conovid in Britain, Enovid 5 mg in the U.S.).[158] In August 1960, the Slough FPA began trials of noretynodrel 2.5 mg + mestranol 100 µg (Conovid-E in Britain, Enovid-E in the U.S.).[159] In May 1961, the London FPA began trials of Schering's Anovlar.[160]
In October 1961, at the recommendation of the Medical Advisory Council of its CIFC, the FPA added Searle's Conovid to its Approved List of Contraceptives.[161] On December 4, 1961, Enoch Powell, then Minister of Health, announced that the oral contraceptive pill Conovid could be prescribed through the NHS at a subsidized price of 2s per month.[162][163] In 1962, Schering's Anovlar and Searle's Conovid-E were added to the FPA's Approved List of Contraceptives.[136][159][160]
France
On December 28, 1967, the Neuwirth Law legalized contraception in France, including the pill.[164] The pill is the most popular form of contraception in France, especially among young women. It accounts for 60% of the birth control used in France. The abortion rate has remained stable since the introduction of the pill.[165]
Japan
In Japan, lobbying from the Japan Medical Association prevented the pill from being approved for general use for nearly 40 years. The higher dose "second generation" pill was approved for use in cases of gynecological problems, but not for birth control. Two main objections raised by the association were safety concerns over long-term use of the pill, and concerns that pill use would lead to decreased use of condoms and thereby potentially increase sexually transmitted infection (STI) rates.[166]
However, when the Ministry of Health and Welfare approved Viagra's use in Japan after only six months of the application's submission, while still claiming that the pill required more data before approval, women's groups cried foul.[167] The pill was subsequently approved for use in June 1999. However, the pill has not become popular in Japan.[168] According to estimates, only 1.3 percent of 28 million Japanese females of childbearing age use the pill, compared with 15.6 percent in the United States. The pill prescription guidelines the government has endorsed require pill users to visit a doctor every three months for pelvic examinations and undergo tests for sexually transmitted diseases and uterine cancer. In the United States and Europe, in contrast, an annual or bi-annual clinic visit is standard for pill users. However, beginning as far back as 2007, many Japanese OBGYNs have required only a yearly visit for pill users, with multiple checks a year recommended only for those who are older or at increased risk of side effects.[169] As of 2004, condoms accounted for 80% of birth control use in Japan, and this may explain Japan's comparatively low rates of AIDS.[169]
Society and culture
The pill was approved by the FDA in the early 1960s; its use spread rapidly in the late part of that decade, generating an enormous social impact. Time magazine placed the pill on its cover in April, 1967.[170][171] In the first place, it was more effective than most previous reversible methods of birth control, giving women unprecedented control over their fertility.[172] Its use was separate from intercourse, requiring no special preparations at the time of sexual activity that might interfere with spontaneity or sensation, and the choice to take the pill was a private one. This combination of factors served to make the pill immensely popular within a few years of its introduction.[112][144]
Claudia Goldin, among others, argue that this new contraceptive technology was a key player in forming women's modern economic role, in that it prolonged the age at which women first married allowing them to invest in education and other forms of human capital as well as generally become more career-oriented. Soon after the birth control pill was legalized, there was a sharp increase in college attendance and graduation rates for women.[173] From an economic point of view, the birth control pill reduced the cost of staying in school. The ability to control fertility without sacrificing sexual relationships allowed women to make long term educational and career plans.[174]
Because the pill was so effective, and soon so widespread, it also heightened the debate about the moral and health consequences of pre-marital sex and promiscuity. Never before had sexual activity been so divorced from reproduction. For a couple using the pill, intercourse became purely an expression of love, or a means of physical pleasure, or both; but it was no longer a means of reproduction. While this was true of previous contraceptives, their relatively high failure rates and their less widespread use failed to emphasize this distinction as clearly as did the pill. The spread of oral contraceptive use thus led many religious figures and institutions to debate the proper role of sexuality and its relationship to procreation. The Roman Catholic Church in particular, after studying the phenomenon of oral contraceptives, re-emphasized the stated teaching on birth control in the 1968 papal encyclical Humanae vitae. The encyclical reiterated the established Catholic teaching that artificial contraception distorts the nature and purpose of sex.[175] On the other side Anglican and other Protestant churches, such as the Evangelical Church in Germany (EKD) accepted the combined oral contraceptive pill.[176]
The United States Senate began hearings on the pill in 1970 and there were different viewpoints heard from medical professionals. Dr. Michael Newton, President of the College of Obstetricians and Gynecologists said:
"The evidence is not yet clear that these still do in fact cause cancer or related to it. The FDA Advisory Committee made comments about this, that if there wasn't enough evidence to indicate whether or not these pills were related to the development of cancer, and I think that's still thin; you have to be cautious about them, but I don't think there is clear evidence, either one way or the other, that they do or don't cause cancer."[177]
Another physician, Dr. Roy Hertz of the Population Council, said that anyone who takes this should know of "our knowledge and ignorance in these matters" and that all women should be made aware of this so she can decide to take the pill or not.[177]
The Secretary of Health, Education, and Welfare at the time, Robert Finch, announced the federal government had accepted a compromise warning statement which would accompany all sales of birth control pills.[177]
Result on popular culture
The introduction of the birth control pill in 1960 allowed more women to find employment opportunities and further their education. As a result of more women getting jobs and an education, their husbands had to start taking over household tasks like cooking.[178] Wanting to stop the change that was occurring in terms of gender norms in an American household, many films, television shows, and other popular culture items portrayed what an ideal American family should be. Below are listed some examples:
Poem
- The Pill Versus the Springhill Mine Disaster was the title poem of a 1968 collection by Richard Brautigan.[179]
Music
- Singer Loretta Lynn commented on how women no longer had to choose between a relationship and a career in her 1974 album with a song entitled "The Pill", which told the story of a married woman's use of the drug to liberate herself from her traditional role as wife and mother.[180]
Environmental impact
A woman using COCPs excretes from her urine and feces natural estrogens, estrone (E1) and estradiol (E2), and synthetic estrogen ethinylestradiol (EE2).[181] These hormones can pass through water treatment plants and into rivers.[182] Other forms of contraception, such as the contraceptive patch, use the same synthetic estrogen (EE2) that is found in COCPs, and can add to the hormonal concentration in the water when flushed down the toilet.[183] This excretion is shown to play a role in causing endocrine disruption, which affects the sexual development and the reproduction, in wild fish populations in segments of streams contaminated by treated sewage effluents.[181][184] A study done in British rivers supported the hypothesis that the incidence and the severity of intersex wild fish populations were significantly correlated with the concentrations of the E1, E2, and EE2 in the rivers.[181]
A review of activated sludge plant performance found estrogen removal rates varied considerably but averaged 78% for estrone, 91% for estradiol, and 76% for ethinylestradiol (estriol effluent concentrations are between those of estrone and estradiol, but estriol is a much less potent endocrine disruptor to fish).[185]
Several studies have suggested that reducing human population growth through increased access to contraception, including birth control pills, can be an effective strategy for climate change mitigation as well as adaptation.[186][187] According to Thomas Wire, contraception is the 'greenest technology' because of its cost-effectiveness in combating global warming — each $7 spent on contraceptives would reduce global carbon emissions by 1 tonne over four decades, while achieving the same result with low-carbon technologies would require $32.[188]
See also
- Estradiol-containing oral contraceptive
- Hormone replacement therapy (HRT)
- List of estrogens available in the United States
- List of progestogens available in the United States
- Progestogen-only injectable contraceptive
References
- Trussell J (2011). "Contraceptive efficacy". In Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar MS (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States.
- Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V, Lee AJ (March 2010). "Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners' Oral Contraception Study". BMJ. 340: c927. doi:10.1136/bmj.c927. PMC 2837145. PMID 20223876.
- IARC working group (2007). "Combined Estrogen-Progestogen Contraceptives" (PDF). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. 91.
- Collaborative Group on Hormonal Factors in Breast Cancer (June 1996). "Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies". Lancet. 347 (9017): 1713–27. doi:10.1016/S0140-6736(96)90806-5. PMID 8656904. Archived from the original on 2019-01-23. Retrieved 2018-12-16.
- Kemmeren JM, Tanis BC, van den Bosch MA, Bollen EL, Helmerhorst FM, van der Graaf Y, Rosendaal FR, Algra A (May 2002). "Risk of Arterial Thrombosis in Relation to Oral Contraceptives (RATIO) study: oral contraceptives and the risk of ischemic stroke". Stroke. 33 (5): 1202–8. doi:10.1161/01.STR.0000015345.61324.3F. PMID 11988591.
- Baillargeon JP, McClish DK, Essah PA, Nestler JE (July 2005). "Association between the current use of low-dose oral contraceptives and cardiovascular arterial disease: a meta-analysis". The Journal of Clinical Endocrinology and Metabolism. 90 (7): 3863–70. doi:10.1210/jc.2004-1958. PMID 15814774.
- "Birth Control Pills - Birth Control Pill - The Pill".
- Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ (December 2004). "Use of contraception and use of family planning services in the United States: 1982-2002" (PDF). Advance Data (350): 1–36. PMID 15633582. all US women aged 15–44
- "Current Contraceptive Status Among Women Aged 15–49: United States, 2015–2017". www.cdc.gov. 2019-06-07. Retrieved 2019-08-02.
- UN Population Division (2006). World Contraceptive Use 2005 (PDF). New York: United Nations. ISBN 978-92-1-151418-6. women aged 15–49 married or in consensual union
- Delvin D (2016-06-15). "Contraception – the contraceptive pill: How many women take it in the UK?".
- Taylor T, Keyse L, Bryant A (2006). Contraception and Sexual Health, 2005/06 (PDF). London: Office for National Statistics. ISBN 978-1-85774-638-9. Archived from the original (PDF) on 2007-01-09. British women aged 16–49: 24% currently use the pill (17% use Combined pill, 5% use Minipill, 2% don't know type)
- Yoshida H, Sakamoto H, Leslie A, Takahashi O, Tsuboi S, Kitamura K (June 2016). "Contraception in Japan: Current trends". Contraception. 93 (6): 475–7. doi:10.1016/j.contraception.2016.02.006. PMID 26872717.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- Harris G (2010-05-03). "The Pill Started More Than One Revolution". The New York Times. Retrieved 2015-09-21.
- "How to Use Birth Control Pills | Follow Easy Instructions". www.plannedparenthood.org. Retrieved 2017-11-29.
- Callahan TL, Caughey AB (2013). Blueprints obstetrics & gynecology (6th ed.). Baltimore, MD: Lippincott Williams & Wilkins. ISBN 9781451117028. OCLC 800907400.
- Birth Control Pills All Guides
- World Health Organization (2016). Selected practice recommendations for contraceptive use (Third ed.). Geneva: World Health Organization. p. 150. hdl:10665/252267. ISBN 9789241565400. OCLC 985676200.
- Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, Simmons KB, Pagano HP, Jamieson DJ, Whiteman MK (July 2016). "U.S. Medical Eligibility Criteria for Contraceptive Use, 2016". MMWR. Recommendations and Reports. 65 (3): 1–103. doi:10.15585/mmwr.rr6503a1. PMID 27467196.
- Trussell J (May 2011). "Contraceptive failure in the United States". Contraception. 83 (5): 397–404. doi:10.1016/j.contraception.2011.01.021. PMC 3638209. PMID 21477680.
- Speroff L, Darney PD (2005). "Oral Contraception". A Clinical Guide for Contraception (4th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 21–138. ISBN 978-0-7817-6488-9.
- FFPRHC (2007). "Clinical Guidance: First Prescription of Combined Oral Contraception" (PDF). Archived from the original (PDF) on 2007-07-04. Retrieved 2007-06-26.
- Edelman, Alison; Micks, Elizabeth; Gallo, Maria F.; Jensen, Jeffrey T.; Grimes, David A. (2014-07-29). "Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception". The Cochrane Database of Systematic Reviews (7): CD004695. doi:10.1002/14651858.CD004695.pub3. ISSN 1469-493X. PMC 6837850. PMID 25072731.
- Last Week of Birth Control Pills
- Gladwell M (2000-03-10). "John Rock's Error". The New Yorker. Archived from the original on 11 May 2013. Retrieved 2009-02-04.
- Mayo Clinic staff. "Birth control pill FAQ: Benefits, risks and choices". Mayo Clinic. Retrieved 1 February 2013.
- "US Patent:Oral contraceptive:Patent 6451778 Issued on September 17, 2002 Estimated Expiration Date: July 2, 2017". PatentStorm LLC. Archived from the original on June 13, 2011. Retrieved 2010-11-19.
- Hercberg S, Preziosi P, Galan P (April 2001). "Iron deficiency in Europe" (PDF). Public Health Nutrition. 4 (2B): 537–45. doi:10.1079/phn2001139. PMID 11683548. Archived from the original (PDF) on 2011-07-26. Retrieved 2010-11-19.
- FDA (2003-09-25). "FDA Approves Seasonal Oral Contraceptive". Archived from the original on 2006-10-07. Retrieved 2006-11-09.
- Edelman, A; Micks, E; Gallo, MF; Jensen, JT; Grimes, DA (29 July 2014). "Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception". The Cochrane Database of Systematic Reviews (7): CD004695. doi:10.1002/14651858.CD004695.pub3. PMC 6837850. PMID 25072731.
- CYWH Staff (2011-10-18). "Medical Uses of the Birth Control Pill". Retrieved 1 February 2013.
- "Information for Consumers (Drugs) - Find Information about a Drug". www.fda.gov. Retrieved 2017-12-13.
- Barakat RR, Park RC, Grigsby PW, et al. Corpus: Epithelial Tumors. In: Principles and Practice of Gynecologic Oncology, 2nd, Hoskins WH, Perez CA, Young RC (Eds), Lippincott-Raven Publishers, Philadelphia 1997. p.859
- Hardiman P, Pillay OC, Atiomo W (May 2003). "Polycystic ovary syndrome and endometrial carcinoma". Lancet. 361 (9371): 1810–2. doi:10.1016/s0140-6736(03)13409-5. PMID 12781553.
- "ACOG Endometriosis FAQ".
- Zorbas KA, Economopoulos KP, Vlahos NF (July 2015). "Continuous versus cyclic oral contraceptives for the treatment of endometriosis: a systematic review". Archives of Gynecology and Obstetrics. 292 (1): 37–43. doi:10.1007/s00404-015-3641-1. PMID 25644508.
- Huber J, Walch K (January 2006). "Treating acne with oral contraceptives: use of lower doses". Contraception. 73 (1): 23–9. doi:10.1016/j.contraception.2005.07.010. PMID 16371290.
- Chang L. "Birth Control of Acne". WebMD, LLC. Retrieved 1 February 2013.
- "DailyMed - ORTHO TRI CYCLEN- norgestimate and ethinyl estradiol ORTHO CYCLEN- norgestimate and ethinyl estradiol". dailymed.nlm.nih.gov. Retrieved 2017-12-13.
- "Beyaz Package Insert" (PDF). FDA.
- American Medical Society for Sports Medicine (24 April 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Medical Society for Sports Medicine, retrieved 29 July 2014
- Cooper, Danielle B.; Adigun, Rotimi; Shamoon, Zafar (2019), "Oral Contraceptive Pills", StatPearls, StatPearls Publishing, PMID 28613632, retrieved 2019-08-05
- "Can Any Woman Take Birth Control Pills?". WebMD. Retrieved 8 May 2016.
- Crooks RL, Baur K (2005). Our Sexuality. Belmont, CA: Thomson Wadsworth. ISBN 978-0-534-65176-3.
- WHO (2005). Decision-Making Tool for Family Planning Clients and Providers Appendix 10: Myths about contraception
- Holck S. "Contraceptive Safety". Special Challenges in Third World Women's Health. 1989 Annual Meeting of the American Public Health Association. Retrieved 2006-10-07.
- Serfaty D (October 1992). "Medical aspects of oral contraceptive discontinuation". Advances in Contraception. 8 Suppl 1: 21–33. doi:10.1007/bf01849448. PMID 1442247.
- Sanders SA, Graham CA, Bass JL, Bancroft J (July 2001). "A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation". Contraception. 64 (1): 51–8. doi:10.1016/S0010-7824(01)00218-9. PMID 11535214.
- Yolton DP, Yolton RL, López R, Bogner B, Stevens R, Rao D (November 1994). "The effects of gender and birth control pill use on spontaneous blink rates". Journal of the American Optometric Association. 65 (11): 763–70. PMID 7822673.
- Huber JC, Bentz EK, Ott J, Tempfer CB (September 2008). "Non-contraceptive benefits of oral contraceptives". Expert Opinion on Pharmacotherapy. 9 (13): 2317–25. doi:10.1517/14656566.9.13.2317. PMID 18710356.
- Nelson, Randy J. (2005). An introduction to behavioral endocrinology (3rd ed.). Sunderland, Mass: Sinauer Associates. ISBN 978-0-87893-617-5.
- Vo C, Carney ME (December 2007). "Ovarian cancer hormonal and environmental risk effect". Obstetrics and Gynecology Clinics of North America. 34 (4): 687–700, viii. doi:10.1016/j.ogc.2007.09.008. PMID 18061864.
- Bandera CA (June 2005). "Advances in the understanding of risk factors for ovarian cancer". The Journal of Reproductive Medicine. 50 (6): 399–406. PMID 16050564.
- "Apri oral : Uses, Side Effects, Interactions, Pictures, Warnings & Dosing".
- Blanco-Molina A, Monreal M (February 2010). "Venous thromboembolism in women taking hormonal contraceptives". Expert Review of Cardiovascular Therapy. 8 (2): 211–5. doi:10.1586/erc.09.175. PMID 20136607.
- Roach RE, Helmerhorst FM, Lijfering WM, Stijnen T, Algra A, Dekkers OM (August 2015). "Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke". The Cochrane Database of Systematic Reviews. 8 (8): CD011054. doi:10.1002/14651858.CD011054.pub2. PMC 6494192. PMID 26310586.
- Rang HP, Dale MM, Ritter JM, Flower RJ, Henderson G (2012). "The reproductive system". Rang and Dale's pharmacology (7th ed.). Edinburgh: Elsevier/Churchill Livingstone. p. 426. ISBN 978-0-7020-3471-8.
- ESHRE Capri Workshop Group (2013). "Venous thromboembolism in women: a specific reproductive health risk". Human Reproduction Update. 19 (5): 471–82. doi:10.1093/humupd/dmt028. PMID 23825156.
- Lidegaard Ø, Milsom I, Geirsson RT, Skjeldestad FE (July 2012). "Hormonal contraception and venous thromboembolism". Acta Obstetricia et Gynecologica Scandinavica. 91 (7): 769–78. doi:10.1111/j.1600-0412.2012.01444.x. PMID 22568831.
- Dunn N (April 2011). "The risk of deep venous thrombosis with oral contraceptives containing drospirenone". BMJ. 342: d2519. doi:10.1136/bmj.d2519. PMID 21511807.
- "Highlights of Prescribing Information for Yasmin" (PDF). FDA.
- Cibula D, Gompel A, Mueck AO, La Vecchia C, Hannaford PC, Skouby SO, Zikan M, Dusek L (2010). "Hormonal contraception and risk of cancer". Human Reproduction Update. 16 (6): 631–50. doi:10.1093/humupd/dmq022. PMID 20543200.
- Bast RC, Brewer M, Zou C, Hernandez MA, Daley M, Ozols R, Lu K, Lu Z, Badgwell D, Mills GB, Skates S, Zhang Z, Chan D, Lokshin A, Yu Y (2007). Prevention and early detection of ovarian cancer: mission impossible?. Recent Results Cancer Res. Recent Results in Cancer Research. 174. pp. 91–100. doi:10.1007/978-3-540-37696-5_9. ISBN 978-3-540-37695-8. PMID 17302189.
- Vessey M, Yeates D, Flynn S (September 2010). "Factors affecting mortality in a large cohort study with special reference to oral contraceptive use". Contraception. 82 (3): 221–9. doi:10.1016/j.contraception.2010.04.006. PMID 20705149.
- Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG, Lowery WJ, Dinan M, McBroom AJ, Hasselblad V, Sanders GD, Myers ER (November 2013). "Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review". Cancer Epidemiology, Biomarkers & Prevention. 22 (11): 1931–43. doi:10.1158/1055-9965.EPI-13-0298. PMID 24014598.
- Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, Hirunpat S, Woodtichartpreecha P, Boonlikit S, Teerawattananon Y, Thakkinstian A (September 2013). "Risk factors of breast cancer: a systematic review and meta-analysis". Asia-Pacific Journal of Public Health. 25 (5): 368–87. doi:10.1177/1010539513488795. PMID 23709491.
- Zhu H, Lei X, Feng J, Wang Y (December 2012). "Oral contraceptive use and risk of breast cancer: a meta-analysis of prospective cohort studies". The European Journal of Contraception & Reproductive Health Care. 17 (6): 402–14. doi:10.3109/13625187.2012.715357. PMID 23061743.
- Lopez, Laureen M.; Edelman, Alison; Chen, Mario; Otterness, Conrad; Trussell, James; Helmerhorst, Frans M. (2013-07-02). Lopez, Laureen M (ed.). "Progestin-only contraceptives: effects on weight". The Cochrane Database of Systematic Reviews (7): CD008815. doi:10.1002/14651858.CD008815.pub3. ISSN 1469-493X. PMC 3855691. PMID 23821307.
- Hatcher RD, Nelson AL (2004). "Combined Hormonal Contraceptive Methods". In Hatcher RD (ed.). Contraceptive technology (18th ed.). New York: Ardent Media, Inc. pp. 403, 432, 434. ISBN 978-0-9664902-5-1.
- Speroff, Leon (2005). A clinical guide for contraception (4th ed.). Hagerstown, MD: Lippincott Williams & Wilkins. p. 72. ISBN 978-0-7817-6488-9.
- Weir GC, DeGroot LJ, Grossman A, Marshall JF, Melmed S, Potts JT (2006). Endocrinology (5th ed.). St. Louis, Mo: Elsevier Saunders. p. 2999. ISBN 978-0-7216-0376-6.
- Westhoff CL, Heartwell S, Edwards S, Zieman M, Stuart G, Cwiak C, Davis A, Robilotto T, Cushman L, Kalmuss D (April 2007). "Oral contraceptive discontinuation: do side effects matter?". American Journal of Obstetrics and Gynecology. 196 (4): 412.e1–6, discussion 412.e6–7. doi:10.1016/j.ajog.2006.12.015. PMC 1903378. PMID 17403440.
- Seal BN, Brotto LA, Gorzalka BB (August 2005). "Oral contraceptive use and female genital arousal: methodological considerations". Journal of Sex Research. 42 (3): 249–58. doi:10.1080/00224490509552279. PMID 19817038.
- Higgins JA, Davis AR (July 2014). "Contraceptive sex acceptability: a commentary, synopsis and agenda for future research". Contraception. 90 (1): 4–10. doi:10.1016/j.contraception.2014.02.029. PMC 4247241. PMID 24792147.
- Panzer C, Wise S, Fantini G, Kang D, Munarriz R, Guay A, Goldstein I (January 2006). "Impact of oral contraceptives on sex hormone-binding globulin and androgen levels: a retrospective study in women with sexual dysfunction". The Journal of Sexual Medicine. 3 (1): 104–13. doi:10.1111/j.1743-6109.2005.00198.x. PMID 16409223.
Description of the study results in Medical News Today: "Birth Control Pill Could Cause Long-Term Problems With Testosterone, New Research Indicates". January 4, 2006. - Panzer C, Wise S, Fantini G, Kang D, Munarriz R, Guay A, Goldstein I (January 2006). "Impact of oral contraceptives on sex hormone-binding globulin and androgen levels: a retrospective study in women with sexual dysfunction". The Journal of Sexual Medicine. 3 (1): 104–13. doi:10.1111/j.1743-6109.2005.00198.x. PMID 16409223.
- Miller G, Tybur JM, Jordan BD (November 2007). "Ovulatory cycle effects on tip earnings by lap dancers: economic evidence for human estrus?". Evolution and Human Behavior. 28 (6): 375–381. CiteSeerX 10.1.1.154.8176. doi:10.1016/j.evolhumbehav.2007.06.002.
- Kulkarni J (July 2007). "Depression as a side effect of the contraceptive pill". Expert Opinion on Drug Safety. 6 (4): 371–4. doi:10.1517/14740338.6.4.371. PMID 17688380.
- Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø (November 2016). "Association of Hormonal Contraception With Depression". JAMA Psychiatry. 73 (11): 1154–1162. doi:10.1001/jamapsychiatry.2016.2387. PMID 27680324.
- Zettermark S, Perez Vicente R, Merlo J (2018-03-22). "Hormonal contraception increases the risk of psychotropic drug use in adolescent girls but not in adults: A pharmacoepidemiological study on 800 000 Swedish women". PLOS ONE. 13 (3): e0194773. Bibcode:2018PLoSO..1394773Z. doi:10.1371/journal.pone.0194773. PMC 5864056. PMID 29566064.
- Burnett-Watson K (October 2005). "Is The Pill Playing Havoc With Your Mental Health?". Archived from the original on 2007-03-20. Retrieved 2007-03-20. Cite journal requires
|journal=(help), which cites:- Kulkarni J, Liew J, Garland KA (November 2005). "Depression associated with combined oral contraceptives--a pilot study". Australian Family Physician. 34 (11): 990. PMID 16299641.
- Young EA, Kornstein SG, Harvey AT, Wisniewski SR, Barkin J, Fava M, Trivedi MH, Rush AJ (August 2007). "Influences of hormone-based contraception on depressive symptoms in premenopausal women with major depression". Psychoneuroendocrinology. 32 (7): 843–53. doi:10.1016/j.psyneuen.2007.05.013. PMC 2100423. PMID 17629629.
- ACOG Committee on Practice Bulletins-Gynecology (2006). "ACOG Practice Bulletin No. 73: Use of Hormonal Contraception in Women with Coexisting Medical Conditions". Obstetrics & Gynecology. 107 (6): 1453–72. doi:10.1097/00006250-200606000-00055. PMID 16738183.
- World Health Organization (2004). "Low-dose combined oral contraceptives". Medical Eligibility Criteria for Contraceptive Use (third ed.). Geneva: Low-dose combined oral contraceptives. hdl:10665/42907. ISBN 978-92-4-156266-9.
- FFPRHC (2006). "The UK Medical Eligibility Criteria for Contraceptive Use (2005/2006)" (PDF). Archived from the original (PDF) on 2007-06-19. Retrieved 2007-03-31.
- Cilia La Corte AL, Carter AM, Turner AJ, Grant PJ, Hooper NM (December 2008). "The bradykinin-degrading aminopeptidase P is increased in women taking the oral contraceptive pill". Journal of the Renin-Angiotensin-Aldosterone System. 9 (4): 221–5. doi:10.1177/1470320308096405. PMID 19126663.
- "Gallstones". NDDIC. July 2007. Archived from the original on 2010-08-11. Retrieved 2010-08-13.
- Raloff J (2013-09-23). "Birth control pills can limit muscle-training gains". Science News. Retrieved 2018-10-22.
- "Love woes can be blamed on contraceptive pill: research – ABC News (Australian Broadcasting Corporation)". Abc.net.au. 2008-08-14. Retrieved 2010-03-20.
- Kollndorfer K, Ohrenberger I, Schöpf V (2016). "Contraceptive Use Affects Overall Olfactory Performance: Investigation of Estradiol Dosage and Duration of Intake". PLOS ONE. 11 (12): e0167520. Bibcode:2016PLoSO..1167520K. doi:10.1371/journal.pone.0167520. PMC 5176159. PMID 28002464.
- Roberts SC, Gosling LM, Carter V, Petrie M (December 2008). "MHC-correlated odour preferences in humans and the use of oral contraceptives". Proceedings. Biological Sciences. 275 (1652): 2715–22. doi:10.1098/rspb.2008.0825. PMC 2605820. PMID 18700206.
- Vercellini P, Eskenazi B, Consonni D, Somigliana E, Parazzini F, Abbiati A, Fedele L (2010). "Oral contraceptives and risk of endometriosis: a systematic review and meta-analysis". Human Reproduction Update. 17 (2): 159–70. doi:10.1093/humupd/dmq042. PMID 20833638.
- Zimmerman Y, Eijkemans MJ, Coelingh Bennink HJ, Blankenstein MA, Fauser BC (2013). "The effect of combined oral contraception on testosterone levels in healthy women: a systematic review and meta-analysis". Human Reproduction Update. 20 (1): 76–105. doi:10.1093/humupd/dmt038. PMC 3845679. PMID 24082040.
- Scholes D, Hubbard RA, Ichikawa LE, LaCroix AZ, Spangler L, Beasley JM, Reed S, Ott SM (September 2011). "Oral contraceptive use and bone density change in adolescent and young adult women: a prospective study of age, hormone dose, and discontinuation". The Journal of Clinical Endocrinology and Metabolism. 96 (9): E1380–7. doi:10.1210/jc.2010-3027. PMC 3167673. PMID 21752879.
- The effects of broad-spectrum antibiotics on Combined contraceptive pills is not found on systematic interaction metanalysis (Archer, 2002), although "individual patients do show large decreases in the plasma concentrations of ethinylestradiol when they take certain other antibiotics" (Dickinson, 2001). "...experts on this topic still recommend informing oral contraceptive users of the potential for a rare interaction" (DeRossi, 2002) and this remains current (2006) UK Family Planning Association advice.
- Archer JS, Archer DF (June 2002). "Oral contraceptive efficacy and antibiotic interaction: a myth debunked". Journal of the American Academy of Dermatology. 46 (6): 917–23. doi:10.1067/mjd.2002.120448. PMID 12063491.
- Dickinson BD, Altman RD, Nielsen NH, Sterling ML (November 2001). "Drug interactions between oral contraceptives and antibiotics". Obstetrics and Gynecology. 98 (5 Pt 1): 853–60. doi:10.1016/S0029-7844(01)01532-0. PMID 11704183.
- DeRossi SS, Hersh EV (October 2002). "Antibiotics and oral contraceptives". Dental Clinics of North America. 46 (4): 653–64. CiteSeerX 10.1.1.620.9933. doi:10.1016/S0011-8532(02)00017-4. PMID 12436822.
- Berry-Bibee, Erin N.; Kim, Myong-Jin; Tepper, Naomi K.; Riley, Halley E. M.; Curtis, Kathryn M. (December 2016). "Co-administration of St. John's wort and hormonal contraceptives: a systematic review". Contraception. 94 (6): 668–677. doi:10.1016/j.contraception.2016.07.010. ISSN 1879-0518. PMID 27444983.
- Nelson AL, Cwiak C (2011). "Combined oral contraceptives (COCs)". In Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar MS (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 249–341. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. pp. 257–258:
Mechanism of action
COCs prevent fertilization and, therefore, qualify as contraceptives. There is no significant evidence that they work after fertilization. The progestins in all COCs provide most of the contraceptive effect by suppressing ovulation and thickening cervical mucus, although the estrogens also make a small contribution to ovulation suppression. Cycle control is enhanced by the estrogen.
Because COCs so effectively suppress ovulation and block ascent of sperm into the upper genital tract, the potential impact on endometrial receptivity to implantation is almost academic. When the two primary mechanisms fail, the fact that pregnancy occurs despite the endometrial changes demonstrates that those endometrial changes do not significantly contribute to the pill's mechanism of action. - Speroff L, Darney PD (2011). "Oral contraception". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 19–152. ISBN 978-1-60831-610-6.
- Levin ER, Hammes SR (2011). "Estrogens and progestins". In Brunton, Chabner BA, Knollmann BC (eds.). Goodman & Gilman's pharmacological basis of therapeutics (12th ed.). New York: McGraw-Hill Medical. pp. 1163–1194. ISBN 978-0-07-162442-8.
- Glasier, Anna (2010). "Contraception". In Jameson, J. Larry; De Groot, Leslie J. (eds.). Endocrinology (6th ed.). Philadelphia: Saunders Elsevier. pp. 2417–2427. ISBN 978-1-4160-5583-9.
- Nelson AL, Cwiak C (2011). "Combined oral contraceptives". In Hatcher RA, Trussell J, Nelson AL, Cates W Jr, Kowal D, Policar MS (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 253–254. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734.
Ten different progestins have been used in the COCs that have been sold in the United States. Several different classification systems for the progestins exist, but the one most commonly used system recapitulates the history of the pill in the United States by categorizing the progestins into the so-called "generations of progestins." The first three generations of progestins are derived from 19-nortestosterone. The fourth generation is drospirenone. Newer progestins are hybrids.
First-generation progestins. First-generation progestins include noretynodrel, norethisterone, norethisterone acetate, and etynodiol diacetate… These compounds have the lowest potency and relatively short half-lives. The short half-life did not matter in the early, high-dose pills but as doses of progestin were decreased in the more modern pills, problems with unscheduled spotting and bleeding became more common.
Second-generation progestins. To solve the problem of unscheduled bleeding and spotting, the second generation progestins (norgestrol and levonorgestrel) were designed to be significantly more potent and to have longer half-lives than norethisterone-related progestins... The second-generation progestins have been associated with more androgen-related side-effects such as adverse effect on lipids, oily skin, acne, and facial hair growth.
Third-generation progestins. Third-generation progestins (desogestrel, norgestimate and elsewhere, gestodene) were introduced to maintain the potent progestational activity of second-generation progestins, but to reduce androgeneic side effects. Reduction in androgen impacts allows a fuller expression of the pill's estrogen impacts. This has some clinical benefits… On the other hand, concern arose that the increased expression of estrogen might increase the risk of venous thromboembolism (VTE). This concern introduced a pill scare in Europe until international studies were completed and correctly interpreted.
Fourth-generation progestins. Drospirenone is an anologue of spironolactone, a potassium-sparing diuretic used to treat hypertension. Drospirenone possesses anti-mineralocorticoid and anti-androgenic properties. These properties have led to new contraceptive applications, such as treatment of premenstrual dysphoric disorder and acne… In the wake of concerns around possible increased VTE risk with less androgenic third-generation formulations, those issues were anticipated with drospirenone. They were clearly answered by large international studies.
Next-generation progestins. More recently, newer progestins have been developed with properties that are shared with different generations of progestins. They have more profound, diverse, and discrete effects on the endometrium than prior progestins. This class would include dienogest (United States) and nomegestrol (Europe). - Speroff L, Darney PD (2011). "Oral contraception". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 40. ISBN 978-1-60831-610-6.
- Goldzieher JW, Rudel HW (October 1974). "How the oral contraceptives came to be developed". JAMA. 230 (3): 421–5. doi:10.1001/jama.230.3.421. PMID 4606623.
- Goldzieher JW (May 1982). "Estrogens in oral contraceptives: historical perspectives". The Johns Hopkins Medical Journal. 150 (5): 165–9. PMID 7043034.
- Perone N (Spring 1993). "The history of steroidal contraceptive development: the progestins". Perspectives in Biology and Medicine. 36 (3): 347–62. doi:10.1353/pbm.1993.0054. PMID 8506121.
- Goldzieher JW (Spring 1993). "The history of steroidal contraceptive development: the estrogens". Perspectives in Biology and Medicine. 36 (3): 363–8. doi:10.1353/pbm.1993.0066. PMID 8506122.
- Maisel AQ (1965). The Hormone Quest. New York: Random House. OCLC 543168.
- Asbell B (1995). The Pill: A Biography of the Drug That Changed the World. New York: Random House. ISBN 978-0-679-43555-6.
- Lehmann PA, Bolivar A, Quintero R (March 1973). "Russell E. Marker. Pioneer of the Mexican steroid industry". Journal of Chemical Education. 50 (3): 195–9. Bibcode:1973JChEd..50..195L. doi:10.1021/ed050p195. PMID 4569922.
- Vaughan P (1970). The Pill on Trial. New York: Coward-McCann. OCLC 97780.
- Tone A (2001). Devices & Desires: A History of Contraceptives in America. New York: Hill and Wang. ISBN 978-0-8090-3817-6.
- Pincus G, Bialy G (1964). Drugs Used in Control of Reproduction. Adv Pharmacol. Advances in Pharmacology. 3. pp. 285–313. doi:10.1016/S1054-3589(08)61115-1. ISBN 9780120329038. PMID 14232795.
The original observation of Makepeace et al. (1937) that progesterone inhibited ovulation in the rabbit was substantiated by Pincus and Chang (1953). In women, 300 mg of progesterone per day taken orally resulted in ovulation inhibition in 80% of cases (Pincus, 1956). The high dosage and frequent incidence of breakthrough bleeding limited the practical application of the method. Subsequently, the utilization of potent 19-norsteroids, which could be given orally, opened the field to practical oral contraception.
- Nance K. "Jonathan Eig on 'The Birth of the Pill'".
- "The Birth of the Pill | W. W. Norton & Company".
- Manning K (17 October 2014). "Book review: 'The Birth of the Pill,' and the reinvention of sex, by Jonathan Eig" – via washingtonpost.com.
- Reed J (1978). From Private Vice to Public Virtue: The Birth Control Movement and American Society Since 1830. New York: Basic Books. ISBN 978-0-465-02582-4.
- Speroff L (2009). A Good Man: Gregory Goodwin Pincus: The Man, His Story, The Birth Control Pill. Portland, Oregon: Arnica. ISBN 978-0-9801942-9-6.
- Fields A (2003). Katharine Dexter McCormick: Pioneer for Women's Rights. Westport, Conn.: Prager. ISBN 978-0-275-98004-7.
- McLaughlin L (1982). The Pill, John Rock, and the Church: The Biography of a Revolution. Boston: Little, Brown. ISBN 978-0-316-56095-5.
- Rock J, Garcia CR, Pincus G (1957). "Synthetic progestins in the normal human menstrual cycle". Recent Progress in Hormone Research. 13: 323–39, discussion 339–46. PMID 13477811.
- Pincus G (December 1958). "The hormonal control of ovulation and early development". Postgraduate Medicine. 24 (6): 654–60. doi:10.1080/00325481.1958.11692305. PMID 13614060.
- Pincus, Gregory (1959). Progestational Agents and the Control of Fertility. Vitamins & Hormones. 17. pp. 307–324. doi:10.1016/S0083-6729(08)60274-5. ISBN 9780127098173. ISSN 0083-6729.
Ishikawa et al. (1957) employing the same regime of progesterone administration also observed suppression of ovulation in a proportion of the cases taken to laparotomy. Although sexual intercourse was practised freely by the subjects of our experiments and those of Ishikawa el al., no pregnancies occurred. Since ovulation presumably took place in a proportion of cycles, the lack of any pregnancies may be due to chance, but Ishikawa et al. (1957) have presented data indicating that in women receiving oral progesterone the cervical mucus becomes impenetrable to sperm.
- Diczfalusy E (December 1965). "Probable mode of action of oral contraceptives". Br Med J. 2 (5475): 1394–9. doi:10.1136/bmj.2.5475.1394. PMC 1847181. PMID 5848673.
At the Fifth International Conference on Planned Parenthood in Tokyo, Pincus (1955) reported an ovulation inhibition by progesterone or norethynodrel1 taken orally by women. This report indicated the beginning of a new era in the history of contraception. [...] That the cervical mucus might be one of the principal sites of action was suggested by the first studies of Pincus (1956, 1959) and of Ishikawa et al. (1957). These investigators found that no pregnancies occurred in women treated orally with large doses of progesterone, though ovulation was inhibited only in some 70% of the cases studied. [...] The mechanism of protection in this method—and probably in that of Pincus (1956) and of Ishikawa et al. (1957)—must involve an effect on the cervical mucus and/or endometrium and Fallopian tubes.
- Annette B. Ramírez de Arellano; Conrad Seipp (10 October 2017). Colonialism, Catholicism, and Contraception: A History of Birth Control in Puerto Rico. University of North Carolina Press. pp. 107–. ISBN 978-1-4696-4001-3.
[...] Still, neither of the two researchers was completely satisfied with the results. Progesterone tended to cause "premature menses," or breakthrough bleeding, in approximately 20 percent of the cycles, an occurrence that disturbed the patients and worried Rock.17 In addition, Pincus was concerned about the failure to inhibit ovulation in all the cases. Only large doses of orally administered progesterone could insure the suppression of ovulation, and these doses were expensive. The mass use of this regimen as a birth control method was thus seriously imperiled.18 [...]
- Chang MC (September 1978). "Development of the oral contraceptives". American Journal of Obstetrics and Gynecology. 132 (2): 217–9. doi:10.1016/0002-9378(78)90928-6. PMID 356615.
- Garcia CR, Pincus G, Rock J (November 1956). "Effects of certain 19-nor steroids on the normal human menstrual cycle". Science. 124 (3227): 891–3. Bibcode:1956Sci...124..891R. doi:10.1126/science.124.3227.891. PMID 13380401.
- Rock J, García C (1957). "Observed effects of 19-nor steroids on ovulation and menstruation". Proceedings of a Symposium on 19-Nor Progestational Steroids. Chicago: Searle Research Laboratories. pp. 14–31. OCLC 935295.
- Pincus G, Rock J, Garcia CR, Ricewray E, Paniagua M, Rodriguez I (June 1958). "Fertility control with oral medication". American Journal of Obstetrics and Gynecology. 75 (6): 1333–46. doi:10.1016/0002-9378(58)90722-1. PMID 13545267.
- Segal SJ (2003). "The Pill and the IUD Modernized Contraception". Under the Banyan Tree: A Population Scientist's Odyssey. Oxford: Oxford University Press. pp. [https://archive.org/details/underbanyantreep00sega/page/70 70–78]. ISBN 978-0-19-515456-6.
- García CR (December 2004). "Development of the pill". Annals of the New York Academy of Sciences. 1038: 223–6. Bibcode:2004NYASA1038..223G. doi:10.1196/annals.1315.031. PMID 15838117.
- Strauss JF, Mastroianni L (January 2005). "In memoriam: Celso-Ramon Garcia, M.D. (1922-2004), reproductive medicine visionary". Journal of Experimental & Clinical Assisted Reproduction. 2 (1): 2. doi:10.1186/1743-1050-2-2. PMC 548289. PMID 15673473.
- Junod SW, Marks L (April 2002). "Women's trials: the approval of the first oral contraceptive pill in the United States and Great Britain" (PDF). Journal of the History of Medicine and Allied Sciences. 57 (2): 117–60. doi:10.1093/jhmas/57.2.117. PMID 11995593.
- Ramírez de Arellano AB, Seipp C (1983). Colonialism, Catholicism, and Contraception: A History of Birth Control in Puerto Rico. Chapel Hill: University of North Carolina Press. ISBN 978-0-8078-1544-1.
- Rice-Wray E (1957). "Field Study with Enovid as a Contraceptive Agent". Proceedings of a Symposium on 19-Nor Progestational Steroids. Chicago: Searle Research Laboratorie. pp. 78–85. OCLC 935295.
- Marsh M, Ronner W (2008). The Fertility Doctor: John Rock and the Reproductive Revolution. Baltimore: The Johns Hopkins University Press. pp. 188–197. ISBN 978-0-8018-9001-7.
- Tyler ET, Olson HJ (April 1959). "Fertility promoting and inhibiting effects of new steroid hormonal substances". Journal of the American Medical Association. 169 (16): 1843–54. doi:10.1001/jama.1959.03000330015003. PMID 13640942.
- Winter IC (1957). "Summary". Proceedings of a Symposium on 19-Nor Progestational Steroids. Chicago: Searle Research Laboratories. pp. 120–122. OCLC 935295.
- Marks L (2001). Sexual Chemistry: A History of the Contraceptive Pill. New Haven: Yale University Press. ISBN 978-0-300-08943-1.
- Winter IC (May 1970). "Industrial pressure and the population problem--the FDA and the pill". JAMA. 212 (6): 1067–8. doi:10.1001/jama.212.6.1067. PMID 5467404.
- Watkins ES (1998). On the Pill: A Social History of Oral Contraceptives, 1950–1970. Baltimore: Johns Hopkins University Press. ISBN 978-0-8018-5876-5.
- Winter IC (March 1965). "The incidence of thromboembolism in Enovid users". Metabolism. 14 (Supplement): SUPPL:422–8. doi:10.1016/0026-0495(65)90029-6. PMID 14261427.
- Jordan WM, Anand JK (November 18, 1961). "Pulmonary embolism". Lancet. 278 (7212): 1146–1147. doi:10.1016/S0140-6736(61)91061-3.
- Seaman B (1969). The Doctors' Case Against the Pill. New York: P. H. Wyden. ISBN 978-0-385-14575-6.
- FDA (June 11, 1970). "Statement of policy concerning oral contraceptive labeling directed to users". Federal Register. 35 (113): 9001–9003.
- FDA (January 31, 1978). "Oral contraceptives; requirement for labeling directed to the patient". Federal Register. 43 (21): 4313–4334.
- FDA (May 25, 1989). "Oral contraceptives; patient package insert requirement". Federal Register. 54 (100): 22585–22588.
- "Prescriptive Authority for Pharmacists: Oral Contraceptives". www.pharmacytimes.com. Retrieved 2019-08-02.
- "Pharmacist Prescribing for Hormonal Contraceptive Medications". NASPA. Retrieved 2019-08-02.
- "Pharmacists Authorized to Prescribe Birth Control in More States". NASPA. 2017-05-04. Retrieved 2019-08-02.
- "History of Schering AG". Archived from the original on April 15, 2008. Retrieved 2007-12-06.CS1 maint: BOT: original-url status unknown (link)
- Karl Van den Broeck "Gynaecoloog Ferdinand Peeters: De vergeten stiefvader van de pil" (Gynecologist Ferdinand Peeters: The forgotten stepfather of the pill) in Knack Extra #4, March 5, 2010, pp. 6–13. (In Dutch.)
- Hope A (May 24, 2010). "The little pill that could". Flanders Today.
- Mears E (November 1961). "Clinical trials of oral contraceptives". British Medical Journal. 2 (5261): 1179–83. doi:10.1136/bmj.2.5261.1179. PMC 1970272. PMID 14471934.
- Eckstein P, Waterhouse JA, Bond GM, Mills WG, Sandilands DM, Shotton DM (November 1961). "The Birmingham oral contraceptive trial". British Medical Journal. 2 (5261): 1172–9. doi:10.1136/bmj.2.5261.1172. PMC 1970253. PMID 13889122.
- Pullen D (October 1962). ""Conovid-E" as an oral contraceptive". British Medical Journal. 2 (5311): 1016–9. doi:10.1136/bmj.2.5311.1016. PMC 1926317. PMID 13972503.
- Mears E, Grant EC (July 1962). ""Anovlar" as an oral contraceptive". British Medical Journal. 2 (5297): 75–9. doi:10.1136/bmj.2.5297.75. PMC 1925289. PMID 14471933.
- "Annotations". British Medical Journal. 2 (5258): 1007–9. October 1961. doi:10.1136/bmj.2.3490.1009. PMC 1970146. PMID 20789252.
"Medical News". BMJ. 2 (5258): 1032–1034. 1961. doi:10.1136/bmj.2.5258.1032. - Chàvez L, Takahashi A, Yoshimoto T, Su CC, Sugawara T, Fujii Y (March 1990). "Morphological changes in normal canine basilar arteries after transluminal angioplasty". Neurological Research. 12 (1): 12–6. doi:10.1136/bmj.2.5266.1584. PMID 1970619. S2CID 8849008.
- "Subsidizing birth control". Time. 78 (24). December 15, 1961. p. 55.
- Dourlen Rollier AV (October 1972). "[Contraception: yes, but...]". Fertilite, Orthogenie. 4 (4): 185–8. PMID 12306278.
- "The Aids Generation: the pill takes priority?". Science Actualities. 2000. Retrieved 2006-09-07.
- "Djerassi on birth control in Japan – abortion 'yes,' pill 'no'" (Press release). Stanford University News Service. 1996-02-14. Archived from the original on 2007-01-06. Retrieved 2006-08-23.
- Wudunn, Sheryl (27 April 1999). "Japan's Tale of Two Pills: Viagra and Birth Control". The New York Times.
- Efron S (3 June 1999). "Japan OKs Birth Control Pill After Decades of Delay". Los Angeles Times.
- Aiko Hayashi (2004-08-20). "Japanese Women Shun The Pill". CBS News. Retrieved 2006-06-12.
- "TIME Magazine Cover: The Pill". Time.com. April 7, 1967. Archived from the original on February 19, 2005. Retrieved June 16, 2020.
- Westhoff, Carolyn (15 December 2015). "How Obamacare Explains the Rising Popularity of IUDs". Public Health Now at Columbia University. Retrieved 2020-06-17.
- The Birth Control Pill: A History
- Goldin C, Katz L (2002). "The Power of the Pill: Oral Contraceptives and Women's Career and Marriage Decisions" (PDF). Journal of Political Economy. 110 (4): 730–770. CiteSeerX 10.1.1.473.6514. doi:10.1086/340778.
- "The Pill". Equality Archive. 2017-03-01. Retrieved 2017-03-09.
- Weigel G (2002). The Courage to Be Catholic: Crisis, Reform, and the Renewal of the Church. Basic Books.
- "Pillenverbot bleibt Streitfrage zwischen den Konfessionen". Focus Online.
- "1970 Year in Review". UPI.
- Winnick C (1968). "The Beige Epoch: Depolarization of Sex Roles in America". The Annals of the American Academy of Political and Social Science. 376: 18–24. doi:10.1177/000271626837600103. JSTOR 1037799.
- "Richard Brautigan: The Pill versus The Springhill Mine Disaster". www.brautigan.net. Retrieved 2017-12-01.
- "The pill and the marriage revolution | The Clayman Institute for Gender Research". gender.stanford.edu. Archived from the original on 2017-12-12. Retrieved 2017-12-01.
- Williams RJ, Johnson AC, Smith JJ, Kanda R (May 2003). "Steroid estrogens profiles along river stretches arising from sewage treatment works discharges". Environmental Science & Technology. 37 (9): 1744–50. Bibcode:2003EnST...37.1744W. doi:10.1021/es0202107. PMID 12775044.
- "Not Quite Worry-Free". Environment. 45 (1): 6–7. Jan–Feb 2003. doi:10.1080/00139150309604545.
- Batt S (Spring 2005). "Pouring Drugs Down the Drain" (PDF). Herizons. 18 (4): 12–3. Archived from the original (PDF) on 2012-03-15. Retrieved 2011-12-04.
- Zeilinger J, Steger-Hartmann T, Maser E, Goller S, Vonk R, Länge R (December 2009). "Effects of synthetic gestagens on fish reproduction". Environmental Toxicology and Chemistry. 28 (12): 2663–70. doi:10.1897/08-485.1. PMID 19469587.
- Johnson AC, Williams RJ, Simpson P, Kanda R (May 2007). "What difference might sewage treatment performance make to endocrine disruption in rivers?". Environmental Pollution. 147 (1): 194–202. doi:10.1016/j.envpol.2006.08.032. PMID 17030080.
- Malcolm Potts; Leah Marsh (February 2010). "THE POPULATION FACTOR: How does it relate to climate change?" (PDF). OurPlanet.com. Archived from the original (PDF) on 4 March 2016. Retrieved 22 June 2015.
- Cafaro P. "Alternative Climate Wedges – Population Wedge". Philip Cafaro. Retrieved 22 June 2015.
- Wire T (10 September 2009). "Contraception is 'greenest' technology". London School of Economics. Retrieved 22 June 2015.
External links
- The Birth Control Pill—CBC Digital Archives
- The Birth of the Pill—slide show by Life magazine