Malaria
Malaria is a mosquito-borne infectious disease that affects humans and other animals.[2] Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches.[1] In severe cases it can cause yellow skin, seizures, coma, or death.[1] Symptoms usually begin ten to fifteen days after being bitten by an infected mosquito.[2] If not properly treated, people may have recurrences of the disease months later.[2] In those who have recently survived an infection, reinfection usually causes milder symptoms.[1] This partial resistance disappears over months to years if the person has no continuing exposure to malaria.[1]
| Malaria | |
|---|---|
.jpg) | |
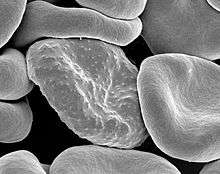
| Malaria parasite connecting to a red blood cell | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Symptoms | Fever, vomiting, headache, yellow skin[1] |
| Complications | Seizures, coma[1] |
| Usual onset | 10–15 days post exposure[2] |
| Causes | Plasmodium spread by mosquitoes[1] |
| Diagnostic method | Examination of the blood, antigen detection tests[1] |
| Prevention | Mosquito nets, insect repellent, mosquito control, medications[1] |
| Medication | Antimalarial medication[2] |
| Frequency | 228 million (2018)[3] |
| Deaths | 405,000 in 2018[3] |
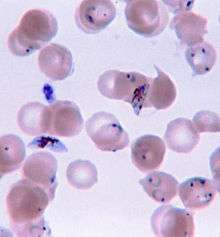
Malaria is caused by single-celled microorganisms of the Plasmodium group.[2] The disease is most commonly spread by an infected female Anopheles mosquito.[2] The mosquito bite introduces the parasites from the mosquito's saliva into a person's blood.[2] The parasites travel to the liver where they mature and reproduce.[1] Five species of Plasmodium can infect and be spread by humans.[1] Most deaths are caused by P. falciparum, whereas P. vivax, P. ovale, and P. malariae generally cause a milder form of malaria.[1][2] The species P. knowlesi rarely causes disease in humans.[2] Malaria is typically diagnosed by the microscopic examination of blood using blood films, or with antigen-based rapid diagnostic tests.[1] Methods that use the polymerase chain reaction to detect the parasite's DNA have been developed, but are not widely used in areas where malaria is common due to their cost and complexity.[4]
The risk of disease can be reduced by preventing mosquito bites through the use of mosquito nets and insect repellents, or with mosquito control measures such as spraying insecticides and draining standing water.[1] Several medications are available to prevent malaria in travellers to areas where the disease is common.[2] Occasional doses of the combination medication sulfadoxine/pyrimethamine are recommended in infants and after the first trimester of pregnancy in areas with high rates of malaria.[2] As of 2020, there is one vaccine which has been shown to reduce the risk of malaria by about 40% in children in Africa.[5][6] Efforts to develop more effective vaccines are ongoing.[6] The recommended treatment for malaria is a combination of antimalarial medications that includes an artemisinin.[1][2] The second medication may be either mefloquine, lumefantrine, or sulfadoxine/pyrimethamine.[7] Quinine along with doxycycline may be used if an artemisinin is not available.[7] It is recommended that in areas where the disease is common, malaria is confirmed if possible before treatment is started due to concerns of increasing drug resistance.[2] Resistance among the parasites has developed to several antimalarial medications; for example, chloroquine-resistant P. falciparum has spread to most malarial areas, and resistance to artemisinin has become a problem in some parts of Southeast Asia.[2]
The disease is widespread in the tropical and subtropical regions that exist in a broad band around the equator.[1] This includes much of sub-Saharan Africa, Asia, and Latin America.[2] In 2018 there were 228 million cases of malaria worldwide resulting in an estimated 405,000 deaths.[3] Approximately 93% of the cases and 94% of deaths occurred in Africa.[3] Rates of disease have decreased from 2010 to 2014, but increased from 2015 to 2017, during which there were 231 million cases.[3] Malaria is commonly associated with poverty and has a major negative effect on economic development.[8][9] In Africa, it is estimated to result in losses of US$12 billion a year due to increased healthcare costs, lost ability to work, and negative effects on tourism.[10]
Signs and symptoms
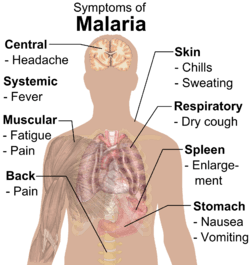
The signs and symptoms of malaria typically begin 8–25 days following infection,[11] but may occur later in those who have taken antimalarial medications as prevention.[4] Initial manifestations of the disease—common to all malaria species—are similar to flu-like symptoms,[12] and can resemble other conditions such as sepsis, gastroenteritis, and viral diseases.[4] The presentation may include headache, fever, shivering, joint pain, vomiting, hemolytic anemia, jaundice, hemoglobin in the urine, retinal damage, and convulsions.[13]
The classic symptom of malaria is paroxysm—a cyclical occurrence of sudden coldness followed by shivering and then fever and sweating, occurring every two days (tertian fever) in P. vivax and P. ovale infections, and every three days (quartan fever) for P. malariae. P. falciparum infection can cause recurrent fever every 36–48 hours, or a less pronounced and almost continuous fever.[14]
Severe malaria is usually caused by P. falciparum (often referred to as falciparum malaria). Symptoms of falciparum malaria arise 9–30 days after infection.[12] Individuals with cerebral malaria frequently exhibit neurological symptoms, including abnormal posturing, nystagmus, conjugate gaze palsy (failure of the eyes to turn together in the same direction), opisthotonus, seizures, or coma.[12]
Complications
Malaria has several serious complications. Among these is the development of respiratory distress, which occurs in up to 25% of adults and 40% of children with severe P. falciparum malaria. Possible causes include respiratory compensation of metabolic acidosis, noncardiogenic pulmonary oedema, concomitant pneumonia, and severe anaemia. Although rare in young children with severe malaria, acute respiratory distress syndrome occurs in 5–25% of adults and up to 29% of pregnant women.[15] Coinfection of HIV with malaria increases mortality.[16] Kidney failure is a feature of blackwater fever, where haemoglobin from lysed red blood cells leaks into the urine.[12]
Infection with P. falciparum may result in cerebral malaria, a form of severe malaria that involves encephalopathy. It is associated with retinal whitening, which may be a useful clinical sign in distinguishing malaria from other causes of fever.[17] An enlarged spleen, enlarged liver or both of these, severe headache, low blood sugar, and haemoglobin in the urine with kidney failure may occur.[12] Complications may include spontaneous bleeding, coagulopathy, and shock.[18]
Malaria in pregnant women is an important cause of stillbirths, infant mortality, abortion and low birth weight,[19] particularly in P. falciparum infection, but also with P. vivax.[20]
Cause
Malaria parasites belong to the genus Plasmodium (phylum Apicomplexa). In humans, malaria is caused by P. falciparum, P. malariae, P. ovale, P. vivax and P. knowlesi.[21][22] Among those infected, P. falciparum is the most common species identified (~75%) followed by P. vivax (~20%).[4] Although P. falciparum traditionally accounts for the majority of deaths,[23] recent evidence suggests that P. vivax malaria is associated with potentially life-threatening conditions about as often as with a diagnosis of P. falciparum infection.[24] P. vivax proportionally is more common outside Africa.[25] There have been documented human infections with several species of Plasmodium from higher apes; however, except for P. knowlesi—a zoonotic species that causes malaria in macaques[22]—these are mostly of limited public health importance.[26]
Life cycle
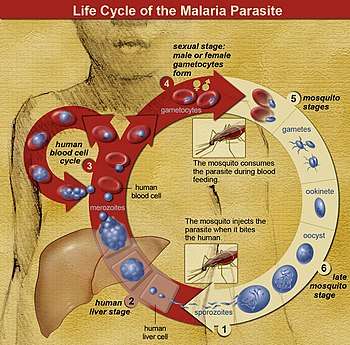
In the life cycle of Plasmodium, a female Anopheles mosquito (the definitive host) transmits a motile infective form (called the sporozoite) to a vertebrate host such as a human (the secondary host), thus acting as a transmission vector. A sporozoite travels through the blood vessels to liver cells (hepatocytes), where it reproduces asexually (tissue schizogony), producing thousands of merozoites. These infect new red blood cells and initiate a series of asexual multiplication cycles (blood schizogony) that produce 8 to 24 new infective merozoites, at which point the cells burst and the infective cycle begins anew.[27]
Other merozoites develop into immature gametocytes, which are the precursors of male and female gametes. When a fertilised mosquito bites an infected person, gametocytes are taken up with the blood and mature in the mosquito gut. The male and female gametocytes fuse and form an ookinete—a fertilised, motile zygote. Ookinetes develop into new sporozoites that migrate to the insect's salivary glands, ready to infect a new vertebrate host. The sporozoites are injected into the skin, in the saliva, when the mosquito takes a subsequent blood meal.[28]
Only female mosquitoes feed on blood; male mosquitoes feed on plant nectar and do not transmit the disease. Females of the mosquito genus Anopheles prefer to feed at night. They usually start searching for a meal at dusk, and continue through the night until they succeed.[29] Malaria parasites can also be transmitted by blood transfusions, although this is rare.[30]
Recurrent malaria
Symptoms of malaria can recur after varying symptom-free periods. Depending upon the cause, recurrence can be classified as either recrudescence, relapse, or reinfection. Recrudescence is when symptoms return after a symptom-free period. It is caused by parasites surviving in the blood as a result of inadequate or ineffective treatment.[31] Relapse is when symptoms reappear after the parasites have been eliminated from the blood but persist as dormant hypnozoites in liver cells.[32] Relapse commonly occurs between 8–24 weeks and is often seen in P. vivax and P. ovale infections.[4] However, relapse-like P. vivax recurrences are probably being over-attributed to hypnozoite activation. Some of them might have an extra-vascular merozoite origin, making these recurrences recrudescences, not relapses.[33] One newly recognised, non-hypnozoite, possible contributing source to recurrent peripheral P. vivax parasitemia is erythrocytic forms in bone marrow.[34] P. vivax malaria cases in temperate areas often involve overwintering by hypnozoites, with relapses beginning the year after the mosquito bite.[35] Reinfection means the parasite that caused the past infection was eliminated from the body but a new parasite was introduced. Reinfection cannot readily be distinguished from recrudescence, although recurrence of infection within two weeks of treatment for the initial infection is typically attributed to treatment failure.[36] People may develop some immunity when exposed to frequent infections.[37]
Climate change
Global climate change is likely to affect malaria transmission, but the degree of effect and the areas affected is uncertain.[38] Greater rainfall in certain areas of India, and following an El Niño event is associated with increased mosquito numbers.[39]
Pathophysiology
Malaria infection develops via two phases: one that involves the liver (exoerythrocytic phase), and one that involves red blood cells, or erythrocytes (erythrocytic phase). When an infected mosquito pierces a person's skin to take a blood meal, sporozoites in the mosquito's saliva enter the bloodstream and migrate to the liver where they infect hepatocytes, multiplying asexually and asymptomatically for a period of 8–30 days.[40]
After a potential dormant period in the liver, these organisms differentiate to yield thousands of merozoites, which, following rupture of their host cells, escape into the blood and infect red blood cells to begin the erythrocytic stage of the life cycle.[40] The parasite escapes from the liver undetected by wrapping itself in the cell membrane of the infected host liver cell.[41]
Within the red blood cells, the parasites multiply further, again asexually, periodically breaking out of their host cells to invade fresh red blood cells. Several such amplification cycles occur. Thus, classical descriptions of waves of fever arise from simultaneous waves of merozoites escaping and infecting red blood cells.[40]
Some P. vivax sporozoites do not immediately develop into exoerythrocytic-phase merozoites, but instead, produce hypnozoites that remain dormant for periods ranging from several months (7–10 months is typical) to several years.[35] After a period of dormancy, they reactivate and produce merozoites. Hypnozoites are responsible for long incubation and late relapses in P. vivax infections,[35] although their existence in P. ovale is uncertain.[42]
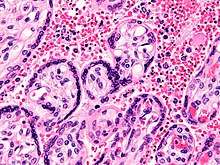
The parasite is relatively protected from attack by the body's immune system because for most of its human life cycle it resides within the liver and blood cells and is relatively invisible to immune surveillance. However, circulating infected blood cells are destroyed in the spleen. To avoid this fate, the P. falciparum parasite displays adhesive proteins on the surface of the infected blood cells, causing the blood cells to stick to the walls of small blood vessels, thereby sequestering the parasite from passage through the general circulation and the spleen.[43] The blockage of the microvasculature causes symptoms such as those in placental malaria.[44] Sequestered red blood cells can breach the blood–brain barrier and cause cerebral malaria.[45]
Genetic resistance
According to a 2005 review, due to the high levels of mortality and morbidity caused by malaria—especially the P. falciparum species—it has placed the greatest selective pressure on the human genome in recent history. Several genetic factors provide some resistance to it including sickle cell trait, thalassaemia traits, glucose-6-phosphate dehydrogenase deficiency, and the absence of Duffy antigens on red blood cells.[46][47]
The impact of sickle cell trait on malaria immunity illustrates some evolutionary trade-offs that have occurred because of endemic malaria. Sickle cell trait causes a change in the haemoglobin molecule in the blood. Normally, red blood cells have a very flexible, biconcave shape that allows them to move through narrow capillaries; however, when the modified haemoglobin S molecules are exposed to low amounts of oxygen, or crowd together due to dehydration, they can stick together forming strands that cause the cell to distort into a curved sickle shape. In these strands, the molecule is not as effective in taking or releasing oxygen, and the cell is not flexible enough to circulate freely. In the early stages of malaria, the parasite can cause infected red cells to sickle, and so they are removed from circulation sooner. This reduces the frequency with which malaria parasites complete their life cycle in the cell. Individuals who are homozygous (with two copies of the abnormal haemoglobin beta allele) have sickle-cell anaemia, while those who are heterozygous (with one abnormal allele and one normal allele) experience resistance to malaria without severe anaemia. Although the shorter life expectancy for those with the homozygous condition would tend to disfavour the trait's survival, the trait is preserved in malaria-prone regions because of the benefits provided by the heterozygous form.[47][48]
Liver dysfunction
Liver dysfunction as a result of malaria is uncommon and usually only occurs in those with another liver condition such as viral hepatitis or chronic liver disease. The syndrome is sometimes called malarial hepatitis.[49] While it has been considered a rare occurrence, malarial hepatopathy has seen an increase, particularly in Southeast Asia and India. Liver compromise in people with malaria correlates with a greater likelihood of complications and death.[49]
Diagnosis
Owing to the non-specific nature of the presentation of symptoms, diagnosis of malaria in non-endemic areas requires a high degree of suspicion, which might be elicited by any of the following: recent travel history, enlarged spleen, fever, low number of platelets in the blood, and higher-than-normal levels of bilirubin in the blood combined with a normal level of white blood cells.[4] Reports in 2016 and 2017 from countries where malaria is common suggest high levels of over diagnosis due to insufficient or inaccurate laboratory testing.[50][51][52]
Malaria is usually confirmed by the microscopic examination of blood films or by antigen-based rapid diagnostic tests (RDT).[53][54] In some areas, RDTs must be able to distinguish whether the malaria symptoms are caused by Plasmodium falciparum or by other species of parasites since treatment strategies could differ for non-P. falciparum infections.[55] Microscopy is the most commonly used method to detect the malarial parasite—about 165 million blood films were examined for malaria in 2010.[56] Despite its widespread usage, diagnosis by microscopy suffers from two main drawbacks: many settings (especially rural) are not equipped to perform the test, and the accuracy of the results depends on both the skill of the person examining the blood film and the levels of the parasite in the blood. The sensitivity of blood films ranges from 75–90% in optimum conditions, to as low as 50%. Commercially available RDTs are often more accurate than blood films at predicting the presence of malaria parasites, but they are widely variable in diagnostic sensitivity and specificity depending on manufacturer, and are unable to tell how many parasites are present.[56] However, incorporating RDTs into the diagnosis of malaria can reduce antimalarial prescription. Although RDT does not improve the health outcomes of those infected with malaria, it also does not lead to worse outcomes when compared to presumptive antimalarial treatment.[57]
In regions where laboratory tests are readily available, malaria should be suspected, and tested for, in any unwell person who has been in an area where malaria is endemic. In areas that cannot afford laboratory diagnostic tests, it has become common to use only a history of fever as the indication to treat for malaria—thus the common teaching "fever equals malaria unless proven otherwise". A drawback of this practice is overdiagnosis of malaria and mismanagement of non-malarial fever, which wastes limited resources, erodes confidence in the health care system, and contributes to drug resistance.[58] Although polymerase chain reaction-based tests have been developed, they are not widely used in areas where malaria is common as of 2012, due to their complexity.[4]
Classification
Malaria is classified into either "severe" or "uncomplicated" by the World Health Organization (WHO).[4] It is deemed severe when any of the following criteria are present, otherwise it is considered uncomplicated.[59]
- Decreased consciousness
- Significant weakness such that the person is unable to walk
- Inability to feed
- Two or more convulsions
- Low blood pressure (less than 70 mmHg in adults and 50 mmHg in children)
- Breathing problems
- Circulatory shock
- Kidney failure or haemoglobin in the urine
- Bleeding problems, or hemoglobin less than 50 g/L (5 g/dL)
- Pulmonary oedema
- Blood glucose less than 2.2 mmol/L (40 mg/dL)
- Acidosis or lactate levels of greater than 5 mmol/L
- A parasite level in the blood of greater than 100,000 per microlitre (µL) in low-intensity transmission areas, or 250,000 per µL in high-intensity transmission areas
Cerebral malaria is defined as a severe P. falciparum-malaria presenting with neurological symptoms, including coma (with a Glasgow coma scale less than 11, or a Blantyre coma scale less than 3), or with a coma that lasts longer than 30 minutes after a seizure.[60]
Various types of malaria have been called by the names below:[61]
| Name | Pathogen | Notes |
|---|---|---|
| algid malaria | Plasmodium falciparum | severe malaria affecting the cardiovascular system and causing chills and circulatory shock |
| bilious malaria | Plasmodium falciparum | severe malaria affecting the liver and causing vomiting and jaundice |
| cerebral malaria | Plasmodium falciparum | severe malaria affecting the cerebrum |
| congenital malaria | various plasmodia | plasmodium introduced from the mother via the fetal circulation |
| falciparum malaria, Plasmodium falciparum malaria, pernicious malaria | Plasmodium falciparum | |
| ovale malaria, Plasmodium ovale malaria | Plasmodium ovale | |
| quartan malaria, malariae malaria, Plasmodium malariae malaria | Plasmodium malariae | paroxysms every fourth day (quartan), counting the day of occurrence as the first day |
| quotidian malaria | Plasmodium falciparum, Plasmodium vivax, Plasmodium knowlesi | paroxysms daily (quotidian) |
| tertian malaria | Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax | paroxysms every third day (tertian), counting the day of occurrence as the first |
| transfusion malaria | various plasmodia | plasmodium introduced by blood transfusion, needle sharing, or needlestick injury |
| vivax malaria, Plasmodium vivax malaria | Plasmodium vivax | |
Prevention

Methods used to prevent malaria include medications, mosquito elimination and the prevention of bites. As of 2020, there is one vaccine for malaria (known as RTS,S) which is licensed for use.[6][5] The presence of malaria in an area requires a combination of high human population density, high anopheles mosquito population density and high rates of transmission from humans to mosquitoes and from mosquitoes to humans. If any of these is lowered sufficiently, the parasite eventually disappears from that area, as happened in North America, Europe, and parts of the Middle East. However, unless the parasite is eliminated from the whole world, it could re-establish if conditions revert to a combination that favors the parasite's reproduction. Furthermore, the cost per person of eliminating anopheles mosquitoes rises with decreasing population density, making it economically unfeasible in some areas.[62]
Prevention of malaria may be more cost-effective than treatment of the disease in the long run, but the initial costs required are out of reach of many of the world's poorest people. There is a wide difference in the costs of control (i.e. maintenance of low endemicity) and elimination programs between countries. For example, in China—whose government in 2010 announced a strategy to pursue malaria elimination in the Chinese provinces—the required investment is a small proportion of public expenditure on health. In contrast, a similar programme in Tanzania would cost an estimated one-fifth of the public health budget.[63]
In areas where malaria is common, children under five years old often have anaemia, which is sometimes due to malaria. Giving children with anaemia in these areas preventive antimalarial medication improves red blood cell levels slightly but does not affect the risk of death or need for hospitalisation.[64]
Mosquito control

Vector control refers to methods used to decrease malaria by reducing the levels of transmission by mosquitoes. For individual protection, the most effective insect repellents are based on DEET or picaridin.[65] However, there is insufficient evidence that mosquito repellants can prevent malaria infection.[66] Insecticide-treated mosquito nets (ITNs) and indoor residual spraying (IRS) have been shown highly effective in preventing malaria among children in areas where malaria is common.[67][68] Prompt treatment of confirmed cases with artemisinin-based combination therapies (ACTs) may also reduce transmission.[69]
Insectide treated nets
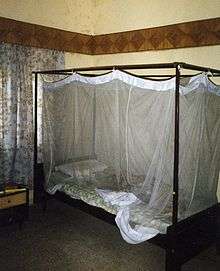
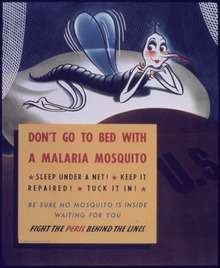
Mosquito nets help keep mosquitoes away from people and reduce infection rates and transmission of malaria. Nets are not a perfect barrier and are often treated with an insecticide designed to kill the mosquito before it has time to find a way past the net. Insecticide-treated nets are estimated to be twice as effective as untreated nets and offer greater than 70% protection compared with no net.[70] Between 2000 and 2008, the use of ITNs saved the lives of an estimated 250,000 infants in Sub-Saharan Africa.[71] About 13% of households in Sub-Saharan countries owned ITNs in 2007[72] and 31% of African households were estimated to own at least one ITN in 2008. In 2000, 1.7 million (1.8%) African children living in areas of the world where malaria is common were protected by an ITN. That number increased to 20.3 million (18.5%) African children using ITNs in 2007, leaving 89.6 million children unprotected[73] and to 68% African children using mosquito nets in 2015.[74] Most nets are impregnated with pyrethroids, a class of insecticides with low toxicity. They are most effective when used from dusk to dawn.[75] It is recommended to hang a large "bed net" above the center of a bed and either tuck the edges under the mattress or make sure it is large enough such that it touches the ground.[76] ITN is beneficial towards pregnancy outcomes in malaria-endemic regions in Africa but more data is needed in Asia and Latin America.[77]
In areas of high malaria resistance, Piperonyl Butoxide combined with Pyrethroids in ITN is effective in reducing malaria infection rates.[78]
Indoor residual spraying
Indoor residual spraying is the spraying of insecticides on the walls inside a home. After feeding, many mosquitoes rest on a nearby surface while digesting the bloodmeal, so if the walls of houses have been coated with insecticides, the resting mosquitoes can be killed before they can bite another person and transfer the malaria parasite.[79] As of 2006, the World Health Organization recommends 12 insecticides in IRS operations, including DDT and the pyrethroids cyfluthrin and deltamethrin.[80] This public health use of small amounts of DDT is permitted under the Stockholm Convention, which prohibits its agricultural use.[81] One problem with all forms of IRS is insecticide resistance. Mosquitoes affected by IRS tend to rest and live indoors, and due to the irritation caused by spraying, their descendants tend to rest and live outdoors, meaning that they are less affected by the IRS.[82] It is uncertain whether the use of IRS together with ITN is effective in reducing malaria cases due to wide geographical variety of malaria distribution, malaria transmission, and insecticide resistance.[83]
Other mosquito control methods
People have tried a number of other methods to reduce mosquito bites and slow the spread of malaria. Efforts to decrease mosquito larvae by decreasing the availability of open water where they develop, or by adding substances to decrease their development, are effective in some locations.[84] Electronic mosquito repellent devices, which make very high-frequency sounds that are supposed to keep female mosquitoes away, have no supporting evidence of effectiveness.[85] There is a low certainty evidence that fogging may have an effect on malaria transmission.[86] Larviciding by hand delivery of chemical or microbial insecticides into water bodies containing low larval distribution may reduce malarial transmission.[87] There is insufficient evidence to determine whether larvivorous fish can decrease mosquito density and transmission in the area.[88]
Medications
There are a number of medications that can help prevent or interrupt malaria in travellers to places where infection is common. Many of these medications are also used in treatment. In places where Plasmodium is resistant to one or more medications, three medications—mefloquine, doxycycline, or the combination of atovaquone/proguanil (Malarone)—are frequently used for prevention.[89] Doxycycline and the atovaquone/proguanil are better tolerated while mefloquine is taken once a week.[89] Areas of the world with chloroquine-sensitive malaria are uncommon.[90] Antimalarial mass drug administration to an entire population at the same time may reduce the risk of contracting malaria in the population.[91]
The protective effect does not begin immediately, and people visiting areas where malaria exists usually start taking the drugs one to two weeks before they arrive, and continue taking them for four weeks after leaving (except for atovaquone/proguanil, which only needs to be started two days before and continued for seven days afterward).[92] The use of preventative drugs is often not practical for those who live in areas where malaria exists, and their use is usually given only to pregnant women and short-term visitors. This is due to the cost of the drugs, side effects from long-term use, and the difficulty in obtaining antimalarial drugs outside of wealthy nations.[93] During pregnancy, medication to prevent malaria has been found to improve the weight of the baby at birth and decrease the risk of anaemia in the mother.[94] The use of preventative drugs where malaria-bearing mosquitoes are present may encourage the development of partial resistance.[95]
Giving antimalarial drugs to infants through intermittent preventive therapy can reduce the risk of having malaria infection, hospital admission, and anaemia.[96]
Mefloquine is more effective than sulfadoxine-pyrimethamine in preventing malaria for HIV-negative pregnant women. Cotrimoxazole is effective in preventing malaria infection and reduce the risk of getting anaemia in HIV-positive women.[97] Giving sulfadoxine-pyrimethamine for three or more doses as intermittent preventive therapy is superior than two doses for HIV-positive women living in malaria-endemic areas.[98]
Others
Community participation and health education strategies promoting awareness of malaria and the importance of control measures have been successfully used to reduce the incidence of malaria in some areas of the developing world.[99] Recognising the disease in the early stages can prevent it from becoming fatal. Education can also inform people to cover over areas of stagnant, still water, such as water tanks that are ideal breeding grounds for the parasite and mosquito, thus cutting down the risk of the transmission between people. This is generally used in urban areas where there are large centers of population in a confined space and transmission would be most likely in these areas.[100] Intermittent preventive therapy is another intervention that has been used successfully to control malaria in pregnant women and infants,[101] and in preschool children where transmission is seasonal.[102]
Treatment
Malaria is treated with antimalarial medications; the ones used depends on the type and severity of the disease. While medications against fever are commonly used, their effects on outcomes are not clear.[103] Providing free antimalarial drugs to households may reduce childhood deaths when used appropriately. Programmes which presumptively treat all causes of fever with antimalarial drugs may lead to overuse of antimalarials and undertreat other causes of fever. Nevertheless, the use of malaria rapid-diagnostic kits can help to reduce over-usage of antimalarials.[104]
Uncomplicated malaria
Simple or uncomplicated malaria may be treated with oral medications. Arteminisin drugs are effective and safe in treating uncomplicated malaria.[105] Arteminisim in combination with other antimalarials (known as artemisinin-combination therapy, or ACT) is about 90% effective when used to treat uncomplicated malaria.[71] The most effective treatment for P. falciparum infection is the use of ACT, which decreases resistance to any single drug component.[106] Artemether-lumefantrine (six-dose regimen) is more effective than the artemether-lumefantrine (four-dose regimen) or other regimens not containing artemisinin derivatives in treating falciparum malaria.[107][108] Another recommended combination is dihydroartemisinin and piperaquine.[109][110][111] Artemisinin-naphthoquine combination therapy showed promising results in treating falciparum malaria. However, more research need to establish its efficacy as a reliable treatment.[112] Artesunate plus mefloquine performs better than mefloquine alone in treating uncomplicated falciparum malaria in low transmission settings.[113] There is limited data to show atovaquone-proguanil is more effective than chloroquine, amodiaquine, and mefloquine in treating falciparum malaria.[114] Azithromycin monotherapy or combination therapy has not shown effectiveness in treating plasmodium or vivax malaria.[115] Amodiaquine plus sulfadoxine-pyrimethamine may achieve less treatment failures when compared to sulfadoxine-pyrimethamine alone in uncomplicated falciparum malaria.[116] There is insufficient data on chlorproguanil-dapsone in treating uncomplicated falciparum malaria.[117] The addition of primaquine with artemisinin-based combination therapy for falciparum malaria reduces its transmission at day 3-4 and day 8 of infection.[118] Sulfadoxine-pyrimethamine plus artesunate is better than sulfadoxine-pyrimethamine plus amodiaquine in controlling treatment failure at day 28. However, the latter is better than the former in reducing gametocytes in blood at day 7.[119]
Infection with P. vivax, P. ovale or P. malariae usually does not require hospitalisation. Treatment of P. vivax requires both treatment of blood stages (with chloroquine or ACT) and clearance of liver forms with primaquine.[120] Arteminisin-based combination therapy is as effective as chloroquine in treating uncomplicated P. vivax malaria.[121] Treatment with tafenoquine prevents relapses after confirmed P. vivax malaria.[122] However, for those treated with chloroquine for blood stage infection, 14 days of primaquine treatment is required to prevent relapse. Shorter primaquine regimens may lead to higher relapse rates.[123] There is no difference in effectiveness between primaquine given for seven or 14 days for prevention of relapse in vivax malaria. The shorter regimen may be useful for those with treatment compliance problems.[124]
To treat malaria during pregnancy, the WHO recommends the use of quinine plus clindamycin early in the pregnancy (1st trimester), and ACT in later stages (2nd and 3rd trimesters).[125] There is limited safety data on the antimalarial drugs in pregnancy.[126]
Severe and complicated malaria
Cases of severe and complicated malaria are almost always caused by infection with P. falciparum. The other species usually cause only febrile disease.[127] Severe and complicated malaria cases are medical emergencies since mortality rates are high (10% to 50%).[128]
Recommended treatment for severe malaria is the intravenous use of antimalarial drugs. For severe malaria, parenteral artesunate was superior to quinine in both children and adults.[129] In another systematic review, artemisinin derivatives (artemether and arteether) were as efficacious as quinine in the treatment of cerebral malaria in children.[130] Treatment of severe malaria involves supportive measures that are best done in a critical care unit. This includes the management of high fevers and the seizures that may result from it. It also includes monitoring for poor breathing effort, low blood sugar, and low blood potassium.[23] Artemisinin derivatives have the same or better efficacy than quinolones in preventing deaths in severe or complicated malaria.[131] Quinine loading dose helps to shorten the duration of fever and increases parasite clearance from the body.[132] There is no difference in effectiveness when using intrarectal quinine compared to intravenous or intramuscular quinine in treating uncomplicated/complicated falciparum malaria.[133] There is insufficient evidence for intramuscular arteether to treat severe malaria.[134] The provision of rectal artesunate before transfer to hospital may reduce the rate of death for children with severe malaria.[135]
Cerebral malaria is the form of severe and complicated malaria with the worst neurological symptoms.[136] There is insufficient data on whether osmotic agents such as mannitol or urea are effective in treating cerebral malaria.[137] Routine phenobarbitone in cerebral malaria is associated with fewer convulsions but possibly more deaths.[138] There is no evidence that steroids would bring treatment benefits for cerebral malaria.[139]
There is insufficient evidence to show that blood transfusion is useful in either reducing deaths for children with severe anaemia or in improving their haematocrit in one month.[140] There is insufficient evidence that iron chelating agents such as deferoxamine and deferiprone improve outcomes of those with malaria falciparum infection.[141]
Resistance
Drug resistance poses a growing problem in 21st-century malaria treatment.[142] In the 2000s (decade), malaria with partial resistance to artemisins emerged in Southeast Asia.[143][144] Resistance is now common against all classes of antimalarial drugs apart from artemisinins. Treatment of resistant strains became increasingly dependent on this class of drugs. The cost of artemisinins limits their use in the developing world.[145] Malaria strains found on the Cambodia–Thailand border are resistant to combination therapies that include artemisinins, and may, therefore, be untreatable.[146] Exposure of the parasite population to artemisinin monotherapies in subtherapeutic doses for over 30 years and the availability of substandard artemisinins likely drove the selection of the resistant phenotype.[147] Resistance to artemisinin has been detected in Cambodia, Myanmar, Thailand, and Vietnam,[148] and there has been emerging resistance in Laos.[149][150] Resistance to the combination of artemisinin and piperaquine was first detected in 2013 in Cambodia, and by 2019 had spread across Cambodia and into Laos, Thailand and Vietnam (with up to 80 percent of malaria parasites resistant in some regions).[151]
There is insufficient evidence in unit packaged antimalarial drugs in preventing treatment failures of malaria infection. However, if supported by training of healthcare providers and patient information, there is improvement in compliance of those receiving treatment.[152]
Prognosis
When properly treated, people with malaria can usually expect a complete recovery.[153] However, severe malaria can progress extremely rapidly and cause death within hours or days.[154] In the most severe cases of the disease, fatality rates can reach 20%, even with intensive care and treatment.[4] Over the longer term, developmental impairments have been documented in children who have suffered episodes of severe malaria.[155] Chronic infection without severe disease can occur in an immune-deficiency syndrome associated with a decreased responsiveness to Salmonella bacteria and the Epstein–Barr virus.[156]
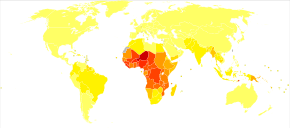
During childhood, malaria causes anaemia during a period of rapid brain development, and also direct brain damage resulting from cerebral malaria.[155] Some survivors of cerebral malaria have an increased risk of neurological and cognitive deficits, behavioural disorders, and epilepsy.[157] Malaria prophylaxis was shown to improve cognitive function and school performance in clinical trials when compared to placebo groups.[155]
Epidemiology
♦ Occurrence of chloroquine-resistant malaria
♦ No Plasmodium falciparum or chloroquine-resistance
♦ No malaria
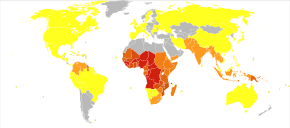
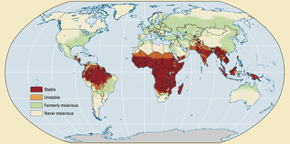
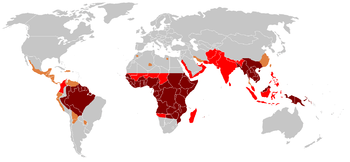
The WHO estimates that in 2018 there were 228 million new cases of malaria resulting in 405,000 deaths.[3] Children under 5 years old are the most affected, accounting for 67% (272,000) of malaria deaths worldwide in 2018.[3] About 125 million pregnant women are at risk of infection each year; in Sub-Saharan Africa, maternal malaria is associated with up to 200,000 estimated infant deaths yearly.[19] There are about 10,000 malaria cases per year in Western Europe, and 1300–1500 in the United States.[15] The United States eradicated malaria in 1951.[159] About 900 people died from the disease in Europe between 1993 and 2003.[65] Both the global incidence of disease and resulting mortality have declined in recent years. According to the WHO and UNICEF, deaths attributable to malaria in 2015 were reduced by 60%[74] from a 2000 estimate of 985,000, largely due to the widespread use of insecticide-treated nets and artemisinin-based combination therapies.[71] In 2012, there were 207 million cases of malaria. That year, the disease is estimated to have killed between 473,000 and 789,000 people, many of whom were children in Africa.[2] Efforts at decreasing the disease in Africa since 2000 have been partially effective, with rates of the disease dropping by an estimated forty percent on the continent.[160]
Malaria is presently endemic in a broad band around the equator, in areas of the Americas, many parts of Asia, and much of Africa; in Sub-Saharan Africa, 85–90% of malaria fatalities occur.[161] An estimate for 2009 reported that countries with the highest death rate per 100,000 of population were Ivory Coast (86.15), Angola (56.93) and Burkina Faso (50.66).[162] A 2010 estimate indicated the deadliest countries per population were Burkina Faso, Mozambique and Mali.[163] The Malaria Atlas Project aims to map global levels of malaria, providing a way to determine the global spatial limits of the disease and to assess disease burden.[164][165] This effort led to the publication of a map of P. falciparum endemicity in 2010 and an update in 2019.[166][167][168] As of 2010, about 100 countries have endemic malaria.[169][170] Every year, 125 million international travellers visit these countries, and more than 30,000 contract the disease.[65]
The geographic distribution of malaria within large regions is complex, and malaria-afflicted and malaria-free areas are often found close to each other.[171] Malaria is prevalent in tropical and subtropical regions because of rainfall, consistent high temperatures and high humidity, along with stagnant waters where mosquito larvae readily mature, providing them with the environment they need for continuous breeding.[172] In drier areas, outbreaks of malaria have been predicted with reasonable accuracy by mapping rainfall.[173] Malaria is more common in rural areas than in cities. For example, several cities in the Greater Mekong Subregion of Southeast Asia are essentially malaria-free, but the disease is prevalent in many rural regions, including along international borders and forest fringes.[174] In contrast, malaria in Africa is present in both rural and urban areas, though the risk is lower in the larger cities.[175]
History

Although the parasite responsible for P. falciparum malaria has been in existence for 50,000–100,000 years, the population size of the parasite did not increase until about 10,000 years ago, concurrently with advances in agriculture[176] and the development of human settlements. Close relatives of the human malaria parasites remain common in chimpanzees. Some evidence suggests that the P. falciparum malaria may have originated in gorillas.[177]
References to the unique periodic fevers of malaria are found throughout history.[178] Hippocrates described periodic fevers, labelling them tertian, quartan, subtertian and quotidian.[179] The Roman Columella associated the disease with insects from swamps.[179] Malaria may have contributed to the decline of the Roman Empire,[180] and was so pervasive in Rome that it was known as the "Roman fever".[181] Several regions in ancient Rome were considered at-risk for the disease because of the favourable conditions present for malaria vectors. This included areas such as southern Italy, the island of Sardinia, the Pontine Marshes, the lower regions of coastal Etruria and the city of Rome along the Tiber. The presence of stagnant water in these places was preferred by mosquitoes for breeding grounds. Irrigated gardens, swamp-like grounds, run-off from agriculture, and drainage problems from road construction led to the increase of standing water.[182] In Medieval West Africa, the people of Djenné successfully identified the mosquito as the vector and cause of malaria.[183]
The term malaria originates from Mediaeval Italian: mala aria—"bad air"; the disease was formerly called ague or marsh fever due to its association with swamps and marshland.[184] The term first appeared in the English literature about 1829.[179] Malaria was once common in most of Europe and North America,[185] where it is no longer endemic,[186] though imported cases do occur.[187]
Scientific studies on malaria made their first significant advance in 1880, when Charles Louis Alphonse Laveran—a French army doctor working in the military hospital of Constantine in Algeria—observed parasites inside the red blood cells of infected people for the first time. He, therefore, proposed that malaria is caused by this organism, the first time a protist was identified as causing disease.[188] For this and later discoveries, he was awarded the 1907 Nobel Prize for Physiology or Medicine. A year later, Carlos Finlay, a Cuban doctor treating people with yellow fever in Havana, provided strong evidence that mosquitoes were transmitting disease to and from humans.[189] This work followed earlier suggestions by Josiah C. Nott,[190] and work by Sir Patrick Manson, the "father of tropical medicine", on the transmission of filariasis.[191]

In April 1894, a Scottish physician, Sir Ronald Ross, visited Sir Patrick Manson at his house on Queen Anne Street, London. This visit was the start of four years of collaboration and fervent research that culminated in 1897 when Ross, who was working in the Presidency General Hospital in Calcutta, proved the complete life-cycle of the malaria parasite in mosquitoes.[192] He thus proved that the mosquito was the vector for malaria in humans by showing that certain mosquito species transmit malaria to birds. He isolated malaria parasites from the salivary glands of mosquitoes that had fed on infected birds.[192] For this work, Ross received the 1902 Nobel Prize in Medicine. After resigning from the Indian Medical Service, Ross worked at the newly established Liverpool School of Tropical Medicine and directed malaria-control efforts in Egypt, Panama, Greece and Mauritius.[193] The findings of Finlay and Ross were later confirmed by a medical board headed by Walter Reed in 1900. Its recommendations were implemented by William C. Gorgas in the health measures undertaken during construction of the Panama Canal. This public-health work saved the lives of thousands of workers and helped develop the methods used in future public-health campaigns against the disease.[194]
In 1896, Amico Bignami discussed the role of mosquitoes in malaria.[195] In 1898, Bignami, Giovanni Battista Grassi and Giuseppe Bastianelli succeeded in showing experimentally the transmission of malaria in humans, using infected mosquitoes to contract malaria themselves which they presented in November 1898 to the Accademia dei Lincei.[192]

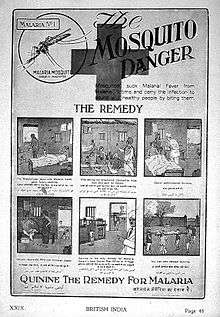
The first effective treatment for malaria came from the bark of cinchona tree, which contains quinine. This tree grows on the slopes of the Andes, mainly in Peru. The indigenous peoples of Peru made a tincture of cinchona to control fever. Its effectiveness against malaria was found and the Jesuits introduced the treatment to Europe around 1640; by 1677, it was included in the London Pharmacopoeia as an antimalarial treatment.[196] It was not until 1820 that the active ingredient, quinine, was extracted from the bark, isolated and named by the French chemists Pierre Joseph Pelletier and Joseph Bienaimé Caventou.[197][198]
Quinine was the predominant malarial medication until the 1920s when other medications began to appear. In the 1940s, chloroquine replaced quinine as the treatment of both uncomplicated and severe malaria until resistance supervened, first in Southeast Asia and South America in the 1950s and then globally in the 1980s.[199]
The medicinal value of Artemisia annua has been used by Chinese herbalists in traditional Chinese medicines for 2,000 years. In 1596, Li Shizhen recommended tea made from qinghao specifically to treat malaria symptoms in his "Compendium of Materia Medica". Artemisinins, discovered by Chinese scientist Tu Youyou and colleagues in the 1970s from the plant Artemisia annua, became the recommended treatment for P. falciparum malaria, administered in severe cases in combination with other antimalarials.[200] Tu says she was influenced by a traditional Chinese herbal medicine source, The Handbook of Prescriptions for Emergency Treatments, written in 340 by Ge Hong.[201] For her work on malaria, Tu Youyou received the 2015 Nobel Prize in Physiology or Medicine.[202]
Plasmodium vivax was used between 1917 and the 1940s for malariotherapy—deliberate injection of malaria parasites to induce a fever to combat certain diseases such as tertiary syphilis. In 1927, the inventor of this technique, Julius Wagner-Jauregg, received the Nobel Prize in Physiology or Medicine for his discoveries. The technique was dangerous, killing about 15% of patients, so it is no longer in use.[203]
The first pesticide used for indoor residual spraying was DDT.[204] Although it was initially used exclusively to combat malaria, its use quickly spread to agriculture. In time, pest control, rather than disease control, came to dominate DDT use, and this large-scale agricultural use led to the evolution of pesticide-resistant mosquitoes in many regions. The DDT resistance shown by Anopheles mosquitoes can be compared to antibiotic resistance shown by bacteria. During the 1960s, awareness of the negative consequences of its indiscriminate use increased, ultimately leading to bans on agricultural applications of DDT in many countries in the 1970s.[81] Before DDT, malaria was successfully eliminated or controlled in tropical areas like Brazil and Egypt by removing or poisoning the breeding grounds of the mosquitoes or the aquatic habitats of the larval stages, for example by applying the highly toxic arsenic compound Paris Green to places with standing water.[205]
Malaria vaccines have been an elusive goal of research. The first promising studies demonstrating the potential for a malaria vaccine were performed in 1967 by immunising mice with live, radiation-attenuated sporozoites, which provided significant protection to the mice upon subsequent injection with normal, viable sporozoites. Since the 1970s, there has been a considerable effort to develop similar vaccination strategies for humans.[206] The first vaccine, called RTS,S, was approved by European regulators in 2015.[207]
Society and culture
Economic impact

Malaria is not just a disease commonly associated with poverty: some evidence suggests that it is also a cause of poverty and a major hindrance to economic development.[8][9] Although tropical regions are most affected, malaria's furthest influence reaches into some temperate zones that have extreme seasonal changes. The disease has been associated with major negative economic effects on regions where it is widespread. During the late 19th and early 20th centuries, it was a major factor in the slow economic development of the American southern states.[208]
A comparison of average per capita GDP in 1995, adjusted for parity of purchasing power, between countries with malaria and countries without malaria gives a fivefold difference (US$1,526 versus US$8,268). In the period 1965 to 1990, countries where malaria was common had an average per capita GDP that increased only 0.4% per year, compared to 2.4% per year in other countries.[209]
Poverty can increase the risk of malaria since those in poverty do not have the financial capacities to prevent or treat the disease. In its entirety, the economic impact of malaria has been estimated to cost Africa US$12 billion every year. The economic impact includes costs of health care, working days lost due to sickness, days lost in education, decreased productivity due to brain damage from cerebral malaria, and loss of investment and tourism.[10] The disease has a heavy burden in some countries, where it may be responsible for 30–50% of hospital admissions, up to 50% of outpatient visits, and up to 40% of public health spending.[210]
.jpg)
Cerebral malaria is one of the leading causes of neurological disabilities in African children.[157] Studies comparing cognitive functions before and after treatment for severe malarial illness continued to show significantly impaired school performance and cognitive abilities even after recovery.[155] Consequently, severe and cerebral malaria have far-reaching socioeconomic consequences that extend beyond the immediate effects of the disease.[211]
Counterfeit and substandard drugs
Sophisticated counterfeits have been found in several Asian countries such as Cambodia,[212] China,[213] Indonesia, Laos, Thailand, and Vietnam, and are an important cause of avoidable death in those countries.[214] The WHO said that studies indicate that up to 40% of artesunate-based malaria medications are counterfeit, especially in the Greater Mekong region. They have established a rapid alert system to rapidly report information about counterfeit drugs to relevant authorities in participating countries.[215] There is no reliable way for doctors or lay people to detect counterfeit drugs without help from a laboratory. Companies are attempting to combat the persistence of counterfeit drugs by using new technology to provide security from source to distribution.[216]
Another clinical and public health concern is the proliferation of substandard antimalarial medicines resulting from inappropriate concentration of ingredients, contamination with other drugs or toxic impurities, poor quality ingredients, poor stability and inadequate packaging.[217] A 2012 study demonstrated that roughly one-third of antimalarial medications in Southeast Asia and Sub-Saharan Africa failed chemical analysis, packaging analysis, or were falsified.[218]
War
Throughout history, the contraction of malaria has played a prominent role in the fates of government rulers, nation-states, military personnel, and military actions.[219] In 1910, Nobel Prize in Medicine-winner Ronald Ross (himself a malaria survivor), published a book titled The Prevention of Malaria that included a chapter titled "The Prevention of Malaria in War." The chapter's author, Colonel C. H. Melville, Professor of Hygiene at Royal Army Medical College in London, addressed the prominent role that malaria has historically played during wars: "The history of malaria in war might almost be taken to be the history of war itself, certainly the history of war in the Christian era. ... It is probably the case that many of the so-called camp fevers, and probably also a considerable proportion of the camp dysentery, of the wars of the sixteenth, seventeenth and eighteenth centuries were malarial in origin."[220] In British-occupied India the cocktail gin and tonic may have come about as a way of taking quinine, known for its antimalarial properties.[221]
Malaria was the most significant health hazard encountered by U.S. troops in the South Pacific during World War II, where about 500,000 men were infected.[222] According to Joseph Patrick Byrne, "Sixty thousand American soldiers died of malaria during the African and South Pacific campaigns."[223]
Significant financial investments have been made to procure existing and create new antimalarial agents. During World War I and World War II, inconsistent supplies of the natural antimalaria drugs cinchona bark and quinine prompted substantial funding into research and development of other drugs and vaccines. American military organisations conducting such research initiatives include the Navy Medical Research Center, Walter Reed Army Institute of Research, and the U.S. Army Medical Research Institute of Infectious Diseases of the US Armed Forces.[224]
Additionally, initiatives have been founded such as Malaria Control in War Areas (MCWA), established in 1942, and its successor, the Communicable Disease Center (now known as the Centers for Disease Control and Prevention, or CDC) established in 1946. According to the CDC, MCWA "was established to control malaria around military training bases in the southern United States and its territories, where malaria was still problematic".[225]
Eradication efforts

Several notable attempts are being made to eliminate the parasite from sections of the world, or to eradicate it worldwide. In 2006, the organisation Malaria No More set a public goal of eliminating malaria from Africa by 2015, and the organization claimed they planned to dissolve if that goal was accomplished. In 2007, World Malaria Day was established by the 60th session of World Health Assembly. As of 2018 they are still functioning.[226] One malaria vaccine is currently licensed for use and several others are in clinical trials,[6] which are intended to provide protection for children in endemic areas and reduce the speed of transmission of the disease. As of 2012, The Global Fund to Fight AIDS, Tuberculosis and Malaria has distributed 230 million insecticide-treated nets intended to stop mosquito-borne transmission of malaria.[227] The U.S.-based Clinton Foundation has worked to manage demand and stabilise prices in the artemisinin market.[228] Other efforts, such as the Malaria Atlas Project, focus on analysing climate and weather information required to accurately predict the spread of malaria based on the availability of habitat of malaria-carrying parasites.[164] The Malaria Policy Advisory Committee (MPAC) of the World Health Organization (WHO) was formed in 2012, "to provide strategic advice and technical input to WHO on all aspects of malaria control and elimination".[229] In November 2013, WHO and the malaria vaccine funders group set a goal to develop vaccines designed to interrupt malaria transmission with the long-term goal of malaria eradication.[230]
Malaria has been successfully eliminated or greatly reduced in certain areas. Malaria was once common in the United States and southern Europe, but vector control programs, in conjunction with the monitoring and treatment of infected humans, eliminated it from those regions. Several factors contributed, such as the draining of wetland breeding grounds for agriculture and other changes in water management practices, and advances in sanitation, including greater use of glass windows and screens in dwellings.[231] Malaria was eliminated from most parts of the United States in the early 20th century by such methods, and the use of the pesticide DDT and other means eliminated it from the remaining pockets in the South in the 1950s as part of the National Malaria Eradication Program.[232]
In 2015 the WHO targeted a 90% reduction in deaths from malaria by 2030[233] and Bill Gates said in 2016 that he thought global eradication would be possible by 2040.[234]
In 2018, WHO announced that Paraguay was free of malaria, after an eradication effort that began in 1950.[235]
As of 2019, the eradication process is ongoing, but with the current approaches and tools, it will be very hard to achieve a world free of malaria. Approaches may require investing more in research and greater universal health care.[236] Continuing surveillance will also be important to prevent return of malaria in countries where the disease has been eliminated.[237]
Research
The Malaria Eradication Research Agenda (malERA) initiative was a consultative process to identify which areas of research and development (R&D) must be addressed for worldwide eradication of malaria.[238][239]
Vaccine
A vaccine against malaria called RTS,S/AS01 (RTS,S) was approved by European regulators in 2015.[207] As of 2019 it is undergoing pilot trials in 3 sub-Saharan African countries – Ghana, Kenya and Malawi – as part of the WHO's Malaria Vaccine Implementation Programme (MVIP).[240]
Immunity (or, more accurately, tolerance) to P. falciparum malaria does occur naturally, but only in response to years of repeated infection.[37] An individual can be protected from a P. falciparum infection if they receive about a thousand bites from mosquitoes that carry a version of the parasite rendered non-infective by a dose of X-ray irradiation.[241] The highly polymorphic nature of many P. falciparum proteins results in significant challenges to vaccine design. Vaccine candidates that target antigens on gametes, zygotes, or ookinetes in the mosquito midgut aim to block the transmission of malaria. These transmission-blocking vaccines induce antibodies in the human blood; when a mosquito takes a blood meal from a protected individual, these antibodies prevent the parasite from completing its development in the mosquito.[242] Other vaccine candidates, targeting the blood-stage of the parasite's life cycle, have been inadequate on their own.[243] For example, SPf66 was tested extensively in areas where the disease was common in the 1990s, but trials showed it to be insufficiently effective.[244]
Medications
Malaria parasites contain apicoplasts, organelles usually found in plants, complete with their own genomes. These apicoplasts are thought to have originated through the endosymbiosis of algae and play a crucial role in various aspects of parasite metabolism, such as fatty acid biosynthesis. Over 400 proteins have been found to be produced by apicoplasts and these are now being investigated as possible targets for novel antimalarial drugs.[245]
With the onset of drug-resistant Plasmodium parasites, new strategies are being developed to combat the widespread disease. One such approach lies in the introduction of synthetic pyridoxal-amino acid adducts, which are taken up by the parasite and ultimately interfere with its ability to create several essential B vitamins.[246][247] Antimalarial drugs using synthetic metal-based complexes are attracting research interest.[248][249]
- (+)-SJ733: Part of a wider class of experimental drugs called spiroindolone. It inhibits the ATP4 protein of infected red blood cells that cause the cells to shrink and become rigid like the aging cells. This triggers the immune system to eliminate the infected cells from the system as demonstrated in a mouse model. As of 2014, a Phase 1 clinical trial to assess the safety profile in human is planned by the Howard Hughes Medical Institute.[250]
- NITD246 and NITD609: Also belonged to the class of spiroindolone and target the ATP4 protein.[250]
Other
A non-chemical vector control strategy involves genetic manipulation of malaria mosquitoes. Advances in genetic engineering technologies make it possible to introduce foreign DNA into the mosquito genome and either decrease the lifespan of the mosquito, or make it more resistant to the malaria parasite. Sterile insect technique is a genetic control method whereby large numbers of sterile male mosquitoes are reared and released. Mating with wild females reduces the wild population in the subsequent generation; repeated releases eventually eliminate the target population.[70]
Genomics is central to malaria research. With the sequencing of P. falciparum, one of its vectors Anopheles gambiae, and the human genome, the genetics of all three organisms in the malaria lifecycle can be studied.[251] Another new application of genetic technology is the ability to produce genetically modified mosquitoes that do not transmit malaria, potentially allowing biological control of malaria transmission.[252]
In one study, a genetically-modified strain of Anopheles stephensi was created that no longer supported malaria transmission, and this resistance was passed down to mosquito offspring.[253]
Gene drive is a technique for changing wild populations, for instance to combat or eliminate insects so they cannot transmit diseases (in particular mosquitoes in the cases of malaria, zika,[254] dengue and yellow fever).[233]
Other animals
Nearly 200 parasitic Plasmodium species have been identified that infect birds, reptiles, and other mammals,[255] and about 30 species naturally infect non-human primates.[256] Some malaria parasites that affect non-human primates (NHP) serve as model organisms for human malarial parasites, such as P. coatneyi (a model for P. falciparum) and P. cynomolgi (P. vivax). Diagnostic techniques used to detect parasites in NHP are similar to those employed for humans.[257] Malaria parasites that infect rodents are widely used as models in research, such as P. berghei.[258] Avian malaria primarily affects species of the order Passeriformes, and poses a substantial threat to birds of Hawaii, the Galapagos, and other archipelagoes. The parasite P. relictum is known to play a role in limiting the distribution and abundance of endemic Hawaiian birds. Global warming is expected to increase the prevalence and global distribution of avian malaria, as elevated temperatures provide optimal conditions for parasite reproduction.[259]
References
- Caraballo H (2014). "Emergency department management of mosquito-borne illness: Malaria, dengue, and west nile virus". Emergency Medicine Practice. 16 (5): 1–23, quiz 23–4. PMID 25207355. Archived from the original on 2016-08-01.
- "Malaria Fact sheet N°94". WHO. March 2014. Archived from the original on 3 September 2014. Retrieved 28 August 2014.
- WHO (2019). World Malaria Report 2019. Switzerland: World Health Organization. pp. xii–xiii, 4–10. ISBN 978-92-4-156572-1.
- Nadjm B, Behrens RH (2012). "Malaria: An update for physicians". Infectious Disease Clinics of North America. 26 (2): 243–59. doi:10.1016/j.idc.2012.03.010. PMID 22632637.
- "Fact sheet about Malaria". www.who.int. Retrieved 6 May 2020.
- "Malaria vaccine: WHO position paper – January 2016" (PDF). Weekly Epidemiological Record. 91 (4): 33–52. 4 Nov 2016. PMID 26829826. Lay summary (PDF).
- Guidelines for the treatment of malaria (2nd ed.). Geneva: World Health Organization. 2010. p. ix. ISBN 978-92-4-154792-5.
- Gollin D, Zimmermann C (August 2007). Malaria: Disease Impacts and Long-Run Income Differences (PDF) (Report). Institute for the Study of Labor. Archived (PDF) from the original on 2016-03-18.
- Worrall E, Basu S, Hanson K (2005). "Is malaria a disease of poverty? A review of the literature". Tropical Health and Medicine. 10 (10): 1047–59. doi:10.1111/j.1365-3156.2005.01476.x. PMID 16185240.
- Greenwood BM, Bojang K, Whitty CJ, Targett GA (2005). "Malaria". Lancet. 365 (9469): 1487–98. doi:10.1016/S0140-6736(05)66420-3. PMID 15850634.
- Fairhurst RM, Wellems TE (2010). "Chapter 275. Plasmodium species (malaria)". In Mandell GL, Bennett JE, Dolin R (eds.). Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 2 (7th ed.). Philadelphia: Churchill Livingstone/Elsevier. pp. 3437–62. ISBN 978-0-443-06839-3.
- Bartoloni A, Zammarchi L (2012). "Clinical aspects of uncomplicated and severe malaria". Mediterranean Journal of Hematology and Infectious Diseases. 4 (1): e2012026. doi:10.4084/MJHID.2012.026. PMC 3375727. PMID 22708041.
- Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME (2006). "Malarial retinopathy: A newly established diagnostic sign in severe malaria". American Journal of Tropical Medicine and Hygiene. 75 (5): 790–97. doi:10.4269/ajtmh.2006.75.790. PMC 2367432. PMID 17123967.
- Ferri FF (2009). "Chapter 332. Protozoal infections". Ferri's Color Atlas and Text of Clinical Medicine. Elsevier Health Sciences. p. 1159. ISBN 978-1-4160-4919-7. Archived from the original on 2016-06-03.
- Taylor WR, Hanson J, Turner GD, White NJ, Dondorp AM (2012). "Respiratory manifestations of malaria". Chest. 142 (2): 492–505. doi:10.1378/chest.11-2655. PMID 22871759.
- Korenromp E, Williams B, de Vlas S, Gouws E, Gilks C, Ghys P, Nahlen B (2005). "Malaria attributable to the HIV-1 epidemic, sub-Saharan Africa". Emerging Infectious Diseases. 11 (9): 1410–19. doi:10.3201/eid1109.050337. PMC 3310631. PMID 16229771.
- Beare NA, Lewallen S, Taylor TE, Molyneux ME (2011). "Redefining cerebral malaria by including malaria retinopathy". Future Microbiology. 6 (3): 349–55. doi:10.2217/fmb.11.3. PMC 3139111. PMID 21449844.
- Davidson's Principles and Practice of Medicine/21st/351
- Hartman TK, Rogerson SJ, Fischer PR (2010). "The impact of maternal malaria on newborns". Annals of Tropical Paediatrics. 30 (4): 271–82. doi:10.1179/146532810X12858955921032. PMID 21118620.
- Rijken MJ, McGready R, Boel ME, Poespoprodjo R, Singh N, Syafruddin D, Rogerson S, Nosten F (2012). "Malaria in pregnancy in the Asia-Pacific region". Lancet Infectious Diseases. 12 (1): 75–88. doi:10.1016/S1473-3099(11)70315-2. PMID 22192132.
- Mueller I, Zimmerman PA, Reeder JC (2007). "Plasmodium malariae and Plasmodium ovale—the "bashful" malaria parasites". Trends in Parasitology. 23 (6): 278–83. doi:10.1016/j.pt.2007.04.009. PMC 3728836. PMID 17459775.
- Collins WE (2012). "Plasmodium knowlesi: A malaria parasite of monkeys and humans". Annual Review of Entomology. 57: 107–21. doi:10.1146/annurev-ento-121510-133540. PMID 22149265.
- Sarkar PK, Ahluwalia G, Vijayan VK, Talwar A (2009). "Critical care aspects of malaria". Journal of Intensive Care Medicine. 25 (2): 93–103. doi:10.1177/0885066609356052. PMID 20018606.
- Baird JK (2013). "Evidence and implications of mortality associated with acute Plasmodium vivax malaria". Clinical Microbiology Reviews. 26 (1): 36–57. doi:10.1128/CMR.00074-12. PMC 3553673. PMID 23297258.
- Arnott A, Barry AE, Reeder JC (2012). "Understanding the population genetics of Plasmodium vivax is essential for malaria control and elimination". Malaria Journal. 11: 14. doi:10.1186/1475-2875-11-14. PMC 3298510. PMID 22233585.
- Collins WE, Barnwell JW (2009). "Plasmodium knowlesi: finally being recognized". Journal of Infectious Diseases. 199 (8): 1107–08. doi:10.1086/597415. PMID 19284287.
- Schlagenhauf-Lawlor 2008, pp. 70–1
- Cowman AF, Berry D, Baum J (2012). "The cellular and molecular basis for malaria parasite invasion of the human red blood cell". Journal of Cell Biology. 198 (6): 961–71. doi:10.1083/jcb.201206112. PMC 3444787. PMID 22986493.
- Arrow KJ, Panosian C, Gelband H (2004). Saving Lives, Buying Time: Economics of Malaria Drugs in an Age of Resistance. National Academies Press. p. 141. ISBN 978-0-309-09218-0. Archived from the original on 2016-05-15.
- Owusu-Ofori AK, Parry C, Bates I (2010). "Transfusion-transmitted malaria in countries where malaria is endemic: A review of the literature from sub-Saharan Africa". Clinical Infectious Diseases. 51 (10): 1192–8. doi:10.1086/656806. PMID 20929356.
- WHO 2010, p. vi
- Markus MB (2011). "Malaria: origin of the term "hypnozoite"". Journal of the History of Biology. 44 (4): 781–6. doi:10.1007/s10739-010-9239-3. PMID 20665090.
- Markus MB (November 2018). "Biological concepts in recurrent Plasmodium vivax malaria". Parasitology. 145 (13): 1765–1771. doi:10.1017/S003118201800032X. PMID 29564998.
- Markus MB (July 2017). "Malaria Eradication and the Hidden Parasite Reservoir". Trends in Parasitology. 33 (7): 492–495. doi:10.1016/j.pt.2017.03.002. PMID 28366603.
- White NJ (2011). "Determinants of relapse periodicity in Plasmodium vivax malaria". Malaria Journal. 10: 297. doi:10.1186/1475-2875-10-297. PMC 3228849. PMID 21989376.
- WHO 2010, p. 17
- Tran TM, Samal B, Kirkness E, Crompton PD (2012). "Systems immunology of human malaria". Trends in Parasitology. 28 (6): 248–57. doi:10.1016/j.pt.2012.03.006. PMC 3361535. PMID 22592005.
- "Climate Change And Infectious Diseases" (PDF). Climate Change and Human Health—Risk and Responses. World Health Organization. Archived (PDF) from the original on 2016-03-04.
- "Climate change and human health – risks and responses. Summary". www.who.int. Retrieved 29 October 2018.
- Bledsoe GH (2005). "Malaria primer for clinicians in the United States". Southern Medical Journal. 98 (12): 1197–204, quiz 1205, 1230. doi:10.1097/01.smj.0000189904.50838.eb. PMID 16440920.
- Vaughan AM, Aly AS, Kappe SH (2008). "Malaria parasite pre-erythrocytic stage infection: Gliding and hiding". Cell Host & Microbe. 4 (3): 209–18. doi:10.1016/j.chom.2008.08.010. PMC 2610487. PMID 18779047.
- Richter J, Franken G, Mehlhorn H, Labisch A, Häussinger D (2010). "What is the evidence for the existence of Plasmodium ovale hypnozoites?". Parasitology Research. 107 (6): 1285–90. doi:10.1007/s00436-010-2071-z. PMID 20922429.
- Tilley L, Dixon MW, Kirk K (2011). "The Plasmodium falciparum-infected red blood cell". International Journal of Biochemistry & Cell Biology. 43 (6): 839–42. doi:10.1016/j.biocel.2011.03.012. PMID 21458590.
- Mens PF, Bojtor EC, Schallig HD (October 2010). "Molecular interactions in the placenta during malaria infection". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 152 (2): 126–32. doi:10.1016/j.ejogrb.2010.05.013. PMID 20933151.
- Rénia L, Wu Howland S, Claser C, Charlotte Gruner A, Suwanarusk R, Hui Teo T, Russell B, Ng LF (2012). "Cerebral malaria: mysteries at the blood-brain barrier". Virulence. 3 (2): 193–201. doi:10.4161/viru.19013. PMC 3396698. PMID 22460644.
- Kwiatkowski DP (2005). "How malaria has affected the human genome and what human genetics can teach us about malaria". American Journal of Human Genetics. 77 (2): 171–92. doi:10.1086/432519. PMC 1224522. PMID 16001361.
- Hedrick PW (2011). "Population genetics of malaria resistance in humans". Heredity. 107 (4): 283–304. doi:10.1038/hdy.2011.16. PMC 3182497. PMID 21427751.
- Weatherall DJ (2008). "Genetic variation and susceptibility to infection: The red cell and malaria". British Journal of Haematology. 141 (3): 276–86. doi:10.1111/j.1365-2141.2008.07085.x. PMID 18410566.
- Bhalla A, Suri V, Singh V (2006). "Malarial hepatopathy". Journal of Postgraduate Medicine. 52 (4): 315–20. PMID 17102560. Archived from the original on 2013-09-21.

- Manguin S, Foumane V, Besnard P, Fortes F, Carnevale P (July 2017). "Malaria overdiagnosis and subsequent overconsumption of antimalarial drugs in Angola: Consequences and effects on human health". Acta Tropica. 171: 58–63. doi:10.1016/j.actatropica.2017.03.022. PMID 28356231.
- Orish VN, Ansong JY, Onyeabor OS, Sanyaolu AO, Oyibo WA, Iriemenam NC (October 2016). "Overdiagnosis and overtreatment of malaria in children in a secondary healthcare centre in Sekondi-Takoradi, Ghana". Tropical Doctor. 46 (4): 191–198. doi:10.1177/0049475515622861. PMID 26738767.
- Yegorov S, Galiwango RM, Ssemaganda A, Muwanga M, Wesonga I, Miiro G, et al. (November 2016). "Low prevalence of laboratory-confirmed malaria in clinically diagnosed adult women from the Wakiso district of Uganda". Malaria Journal. 15 (1): 555. doi:10.1186/s12936-016-1604-z. PMC 5109652. PMID 27842555.
- Abba K, Deeks JJ, Olliaro P, Naing CM, Jackson SM, Takwoingi Y, Donegan S, Garner P (2011). Abba K (ed.). "Rapid diagnostic tests for diagnosing uncomplicated P. falciparum malaria in endemic countries". Cochrane Database of Systematic Reviews (7): CD008122. doi:10.1002/14651858.CD008122.pub2. PMC 6532563. PMID 21735422.
- Kattenberg JH, Ochodo EA, Boer KR, Schallig HD, Mens PF, Leeflang MM (2011). "Systematic review and meta-analysis: Rapid diagnostic tests versus placental histology, microscopy and PCR for malaria in pregnant women". Malaria Journal. 10: 321. doi:10.1186/1475-2875-10-321. PMC 3228868. PMID 22035448.
- Abba K, Kirkham AJ, Olliaro PL, Deeks JJ, Donegan S, Garner P, Takwoingi Y (December 2014). "Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries". The Cochrane Database of Systematic Reviews. 12 (12): CD011431. doi:10.1002/14651858.cd011431. PMC 4453861. PMID 25519857.
- Wilson ML (2012). "Malaria rapid diagnostic tests". Clinical Infectious Diseases. 54 (11): 1637–41. doi:10.1093/cid/cis228. PMID 22550113.
- Odaga J, Sinclair D, Lokong JA, Donegan S, Hopkins H, Garner P, et al. (Cochrane Infectious Diseases Group) (April 2014). "Rapid diagnostic tests versus clinical diagnosis for managing people with fever in malaria endemic settings". The Cochrane Database of Systematic Reviews (4): CD008998. doi:10.1002/14651858.CD008998.pub2. PMC 4468923. PMID 24740584.
- Perkins MD, Bell DR (2008). "Working without a blindfold: The critical role of diagnostics in malaria control". Malaria Journal. 1 (Suppl 1): S5. doi:10.1186/1475-2875-7-S1-S5. PMC 2604880. PMID 19091039.
- WHO 2010, p. 35
- WHO 2010, p. v
- Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- World Health Organization (1958). "Malaria" (PDF). The First Ten Years of the World Health Organization. World Health Organization. pp. 172–87. Archived (PDF) from the original on 2011-07-08.
- Sabot O, Cohen JM, Hsiang MS, Kahn JG, Basu S, Tang L, Zheng B, Gao Q, Zou L, Tatarsky A, Aboobakar S, Usas J, Barrett S, Cohen JL, Jamison DT, Feachem RG (2010). "Costs and financial feasibility of malaria elimination". Lancet. 376 (9752): 1604–15. doi:10.1016/S0140-6736(10)61355-4. PMC 3044845. PMID 21035839.
- Athuman M, Kabanywanyi AM, Rohwer AC (January 2015). "Intermittent preventive antimalarial treatment for children with anaemia". The Cochrane Database of Systematic Reviews. 1: CD010767. doi:10.1002/14651858.CD010767.pub2. PMC 4447115. PMID 25582096.
- Kajfasz P (2009). "Malaria prevention". International Maritime Health. 60 (1–2): 67–70. PMID 20205131. Archived from the original on 2017-08-30.

- Maia MF, Kliner M, Richardson M, Lengeler C, Moore SJ, et al. (Cochrane Infectious Diseases Group) (February 2018). "Mosquito repellents for malaria prevention". The Cochrane Database of Systematic Reviews. 2: CD011595. doi:10.1002/14651858.CD011595.pub2. PMC 5815492. PMID 29405263.
- Pryce J, Richardson M, Lengeler C (November 2018). "Insecticide-treated nets for preventing malaria". The Cochrane Database of Systematic Reviews. 11: CD000363. doi:10.1002/14651858.CD000363.pub3. PMC 6418392. PMID 30398672.
- Tanser FC, Lengeler C, Sharp BL (2010). Lengeler C (ed.). "Indoor residual spraying for preventing malaria". Cochrane Database of Systematic Reviews (4): CD006657. doi:10.1002/14651858.CD006657.pub2. PMC 6532743. PMID 20393950.
- Palmer J. "WHO gives indoor use of DDT a clean bill of health for controlling malaria". WHO. Archived from the original on 2012-10-22.
- Raghavendra K, Barik TK, Reddy BP, Sharma P, Dash AP (2011). "Malaria vector control: From past to future". Parasitology Research. 108 (4): 757–79. doi:10.1007/s00436-010-2232-0. PMID 21229263.
- Howitt P, Darzi A, Yang GZ, Ashrafian H, Atun R, Barlow J, Blakemore A, Bull AM, Car J, Conteh L, Cooke GS, Ford N, Gregson SA, Kerr K, King D, Kulendran M, Malkin RA, Majeed A, Matlin S, Merrifield R, Penfold HA, Reid SD, Smith PC, Stevens MM, Templeton MR, Vincent C, Wilson E (2012). "Technologies for global health". The Lancet. 380 (9840): 507–35. doi:10.1016/S0140-6736(12)61127-1. PMID 22857974.
- Miller JM, Korenromp EL, Nahlen BL, W Steketee R (2007). "Estimating the number of insecticide-treated nets required by African households to reach continent-wide malaria coverage targets". Journal of the American Medical Association. 297 (20): 2241–50. doi:10.1001/jama.297.20.2241. PMID 17519414.
- Noor AM, Mutheu JJ, Tatem AJ, Hay SI, Snow RW (2009). "Insecticide-treated net coverage in Africa: Mapping progress in 2000–07". Lancet. 373 (9657): 58–67. doi:10.1016/S0140-6736(08)61596-2. PMC 2652031. PMID 19019422.
- Achieving the malaria MDG target: reversing the incidence of malaria 2000–2015 (PDF). UNICEF. WHO. September 2015. ISBN 978-92-4-150944-2. Archived (PDF) from the original on 5 January 2016. Retrieved 26 December 2015.
- Schlagenhauf-Lawlor 2008, p. 215
- Instructions for treatment and use of insecticide-treated mosquito nets (PDF). World Health Organization. 2002. p. 34. Archived (PDF) from the original on 2015-07-06.
- Gamble C, Ekwaru JP, ter Kuile FO, et al. (Cochrane Infectious Diseases Group) (April 2006). "Insecticide-treated nets for preventing malaria in pregnancy". The Cochrane Database of Systematic Reviews (2): CD003755. doi:10.1002/14651858.CD003755.pub2. PMC 6532581. PMID 16625591.
- Gleave K, Lissenden N, Richardson M, Choi L, Ranson H, et al. (Cochrane Infectious Diseases Group) (November 2018). "Piperonyl butoxide (PBO) combined with pyrethroids in insecticide-treated nets to prevent malaria in Africa". The Cochrane Database of Systematic Reviews. 11: CD012776. doi:10.1002/14651858.CD012776.pub2. PMC 6262905. PMID 30488945.
- Enayati A, Hemingway J (2010). "Malaria management: Past, present, and future". Annual Review of Entomology. 55: 569–91. doi:10.1146/annurev-ento-112408-085423. PMID 19754246.
- Indoor Residual Spraying: Use of Indoor Residual Spraying for Scaling Up Global Malaria Control and Elimination. WHO Position Statement (PDF) (Report). World Health Organization. 2006. Archived (PDF) from the original on 2008-10-02.
- van den Berg H (2009). "Global status of DDT and its alternatives for use in vector control to prevent disease". Environmental Health Perspectives. 117 (11): 1656–63. doi:10.1289/ehp.0900785. PMC 2801202. PMID 20049114.
- Pates H, Curtis C (2005). "Mosquito behaviour and vector control". Annual Review of Entomology. 50: 53–70. doi:10.1146/annurev.ento.50.071803.130439. PMID 15355233.
- "Indoor residual spraying for preventing malaria in communities using insecticide-treated nets". Cochrane Database of Systematic Reviews. 2019-05-23. doi:10.1002/14651858.CD012688.pub2. PMC 6532761. PMID 31120132.
- Tusting LS, Thwing J, Sinclair D, Fillinger U, Gimnig J, Bonner KE, Bottomley C, Lindsay SW (2013). "Mosquito larval source management for controlling malaria". Cochrane Database of Systematic Reviews. 8 (8): CD008923. doi:10.1002/14651858.CD008923.pub2. PMC 4669681. PMID 23986463.
- Enayati AA, Hemingway J, Garner P (2007). Enayati A (ed.). "Electronic mosquito repellents for preventing mosquito bites and malaria infection". Cochrane Database of Systematic Reviews (2): CD005434. doi:10.1002/14651858.CD005434.pub2. PMC 6532582. PMID 17443590.
- Pryce J, Choi L, Richardson M, Malone D, et al. (Cochrane Infectious Diseases Group) (November 2018). "Insecticide space spraying for preventing malaria transmission". The Cochrane Database of Systematic Reviews. 11: CD012689. doi:10.1002/14651858.CD012689.pub2. PMC 6516806. PMID 30388303.
- Choi L, Majambere S, Wilson AL, et al. (Cochrane Infectious Diseases Group) (August 2019). "Larviciding to prevent malaria transmission". The Cochrane Database of Systematic Reviews. 8: CD012736. doi:10.1002/14651858.CD012736.pub2. PMC 6699674. PMID 31425624.
- Walshe DP, Garner P, Adeel AA, Pyke GH, Burkot TR, et al. (Cochrane Infectious Diseases Group) (December 2017). "Larvivorous fish for preventing malaria transmission". The Cochrane Database of Systematic Reviews. 12: CD008090. doi:10.1002/14651858.CD008090.pub3. PMC 5741835. PMID 29226959.
- Tickell-Painter M, Maayan N, Saunders R, Pace C, Sinclair D (October 2017). "Mefloquine for preventing malaria during travel to endemic areas". The Cochrane Database of Systematic Reviews. 10: CD006491. doi:10.1002/14651858.CD006491.pub4. PMC 5686653. PMID 29083100.
- "Malaria Worldwide – How Can Malaria Cases and Deaths Be Reduced? – Drug resistance in the Malaria Endemic World". www.cdc.gov. Retrieved 4 January 2018.
- Poirot E, Skarbinski J, Sinclair D, Kachur SP, Slutsker L, Hwang J, et al. (Cochrane Infectious Diseases Group) (December 2013). "Mass drug administration for malaria". The Cochrane Database of Systematic Reviews (12): CD008846. doi:10.1002/14651858.CD008846.pub2. PMC 4468927. PMID 24318836.
- Freedman DO (2008). "Clinical practice. Malaria prevention in short-term travelers". New England Journal of Medicine. 359 (6): 603–12. doi:10.1056/NEJMcp0803572. PMID 18687641.
- Fernando SD, Rodrigo C, Rajapakse S (2011). "Chemoprophylaxis in malaria: Drugs, evidence of efficacy and costs". Asian Pacific Journal of Tropical Medicine. 4 (4): 330–36. doi:10.1016/S1995-7645(11)60098-9. PMID 21771482.
- Radeva-Petrova D, Kayentao K, ter Kuile FO, Sinclair D, Garner P (October 2014). "Drugs for preventing malaria in pregnant women in endemic areas: any drug regimen versus placebo or no treatment". The Cochrane Database of Systematic Reviews. 10 (10): CD000169. doi:10.1002/14651858.CD000169.pub3. PMC 4498495. PMID 25300703.
- Turschner S, Efferth T (2009). "Drug resistance in Plasmodium: Natural products in the fight against malaria". Mini Reviews in Medicinal Chemistry. 9 (2): 206–14. doi:10.2174/138955709787316074. PMID 19200025.
- Esu EB, Oringanje C, Meremikwu MM, et al. (Cochrane Infectious Diseases Group) (December 2019). "Intermittent preventive treatment for malaria in infants". The Cochrane Database of Systematic Reviews. 12: CD011525. doi:10.1002/14651858.CD011525.pub2. PMC 6887842. PMID 31792925.
- González R, Pons-Duran C, Piqueras M, Aponte JJ, Ter Kuile FO, Menéndez C, et al. (Cochrane Infectious Diseases Group) (November 2018). "Mefloquine for preventing malaria in pregnant women". The Cochrane Database of Systematic Reviews. 11: CD011444. doi:10.1002/14651858.CD011444.pub3. PMC 6517148. PMID 30480761.
- Mathanga DP, Uthman OA, Chinkhumba J, et al. (Cochrane Infectious Diseases Group) (October 2011). "Intermittent preventive treatment regimens for malaria in HIV-positive pregnant women". The Cochrane Database of Systematic Reviews (10): CD006689. doi:10.1002/14651858.CD006689.pub2. PMC 6532702. PMID 21975756.
- Lalloo DG, Olukoya P, Olliaro P (2006). "Malaria in adolescence: Burden of disease, consequences, and opportunities for intervention". Lancet Infectious Diseases. 6 (12): 780–93. doi:10.1016/S1473-3099(06)70655-7. PMID 17123898.
- Mehlhorn H, ed. (2008). "Disease Control, Methods". Encyclopedia of Parasitology (3rd ed.). Springer. pp. 362–66. ISBN 978-3-540-48997-9.
- Bardají A, Bassat Q, Alonso PL, Menéndez C (2012). "Intermittent preventive treatment of malaria in pregnant women and infants: making best use of the available evidence". Expert Opinion on Pharmacotherapy. 13 (12): 1719–36. doi:10.1517/14656566.2012.703651. PMID 22775553.
- Meremikwu MM, Donegan S, Sinclair D, Esu E, Oringanje C (2012). Meremikwu MM (ed.). "Intermittent preventive treatment for malaria in children living in areas with seasonal transmission". Cochrane Database of Systematic Reviews. 2 (2): CD003756. doi:10.1002/14651858.CD003756.pub4. PMC 6532713. PMID 22336792.
- Meremikwu MM, Odigwe CC, Akudo Nwagbara B, Udoh EE (2012). Meremikwu MM (ed.). "Antipyretic measures for treating fever in malaria". Cochrane Database of Systematic Reviews. 9 (9): CD002151. doi:10.1002/14651858.CD002151.pub2. PMC 6532580. PMID 22972057.
- Okwundu CI, Nagpal S, Musekiwa A, Sinclair D (31 May 2013). "Home- Or Community-Based Programmes for Treating Malaria". Cochrane Database of Systematic Reviews (5): CD009527. doi:10.1002/14651858.CD009527.pub2. PMC 6532579. PMID 23728693.
- McIntosh HM, Olliaro P, et al. (Cochrane Infectious Diseases Group) (1999-04-26). "Artemisinin derivatives for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (2): CD000256. doi:10.1002/14651858.CD000256. PMC 6532741. PMID 10796519.
- Kokwaro G (2009). "Ongoing challenges in the management of malaria". Malaria Journal. 8 (Suppl 1): S2. doi:10.1186/1475-2875-8-S1-S2. PMC 2760237. PMID 19818169.
- Omari AA, Gamble C, Garner P, et al. (Cochrane Infectious Diseases Group) (April 2006). "Artemether-lumefantrine (four-dose regimen) for treating uncomplicated falciparum malaria". The Cochrane Database of Systematic Reviews (2): CD005965. doi:10.1002/14651858.CD005965. PMC 6532603. PMID 16625646.
- Omari AA, Gamble C, Garner P, et al. (Cochrane Infectious Diseases Group) (October 2005). "Artemether-lumefantrine (six-dose regimen) for treating uncomplicated falciparum malaria". The Cochrane Database of Systematic Reviews (4): CD005564. doi:10.1002/14651858.CD005564. PMC 6532733. PMID 16235412.
- WHO 2010, p. 21
- Keating GM (2012). "Dihydroartemisinin/piperaquine: A review of its use in the treatment of uncomplicated Plasmodium falciparum malaria". Drugs. 72 (7): 937–61. doi:10.2165/11203910-000000000-00000. PMID 22515619.
- Sinclair D, Zani B, Donegan S, Olliaro P, Garner P, et al. (Cochrane Infectious Diseases Group) (July 2009). "Artemisinin-based combination therapy for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (3): CD007483. doi:10.1002/14651858.CD007483.pub2. PMC 6532584. PMID 19588433.
- Isba R, Zani B, Gathu M, Sinclair D, et al. (Cochrane Infectious Diseases Group) (February 2015). "Artemisinin-naphthoquine for treating uncomplicated Plasmodium falciparum malaria". The Cochrane Database of Systematic Reviews (2): CD011547. doi:10.1002/14651858.CD011547. PMC 4453860. PMID 25702785.
- Bukirwa H, Orton L, et al. (Cochrane Infectious Diseases Group) (October 2005). "Artesunate plus mefloquine versus mefloquine for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (4): CD004531. doi:10.1002/14651858.CD004531.pub2. PMC 6532646. PMID 16235367.
- Osei-Akoto A, Orton L, Owusu-Ofori SP, et al. (Cochrane Infectious Diseases Group) (October 2005). "Atovaquone-proguanil for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (4): CD004529. doi:10.1002/14651858.CD004529.pub2. PMC 6532621. PMID 16235366.
- van Eijk AM, Terlouw DJ, et al. (Cochrane Infectious Diseases Group) (February 2011). "Azithromycin for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (2): CD006688. doi:10.1002/14651858.CD006688.pub2. PMC 6532599. PMID 21328286.
- McIntosh HM, Jones KL, et al. (Cochrane Infectious Diseases Group) (October 2005). "Chloroquine or amodiaquine combined with sulfadoxine-pyrimethamine for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (4): CD000386. doi:10.1002/14651858.CD000386.pub2. PMC 6532604. PMID 16235276.
- Bukirwa H, Garner P, Critchley J, et al. (Cochrane Infectious Diseases Group) (October 2004). "Chlorproguanil-dapsone for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (4): CD004387. doi:10.1002/14651858.CD004387.pub2. PMC 6532720. PMID 15495106.
- Graves PM, Choi L, Gelband H, Garner P, et al. (Cochrane Infectious Diseases Group) (February 2018). "Primaquine or other 8-aminoquinolines for reducing Plasmodium falciparum transmission". The Cochrane Database of Systematic Reviews. 2: CD008152. doi:10.1002/14651858.CD008152.pub5. PMC 5815493. PMID 29393511.
- Bukirwa H, Critchley J, et al. (Cochrane Infectious Diseases Group) (January 2006). "Sulfadoxine-pyrimethamine plus artesunate versus sulfadoxine-pyrimethamine plus amodiaquine for treating uncomplicated malaria". The Cochrane Database of Systematic Reviews (1): CD004966. doi:10.1002/14651858.CD004966.pub2. PMC 6532706. PMID 16437507.
- Waters NC, Edstein MD (2012). "8-Aminoquinolines: Primaquine and tafenoquine". In Staines HM, Krishna S (eds.). Treatment and Prevention of Malaria: Antimalarial Drug Chemistry, Action and Use. Springer. pp. 69–93. ISBN 978-3-0346-0479-6. Archived from the original on 2016-06-17.
- Gogtay N, Kannan S, Thatte UM, Olliaro PL, Sinclair D, et al. (Cochrane Infectious Diseases Group) (October 2013). "Artemisinin-based combination therapy for treating uncomplicated Plasmodium vivax malaria". The Cochrane Database of Systematic Reviews (10): CD008492. doi:10.1002/14651858.CD008492.pub3. PMC 6532731. PMID 24163021.
- Rajapakse S, Rodrigo C, Fernando SD (April 2015). "Tafenoquine for preventing relapse in people with Plasmodium vivax malaria". The Cochrane Database of Systematic Reviews. 4 (4): CD010458. doi:10.1002/14651858.cd010458.pub2. PMC 4468925. PMID 25921416.
- Galappaththy GN, Tharyan P, Kirubakaran R, et al. (Cochrane Infectious Diseases Group) (October 2013). "Primaquine for preventing relapse in people with Plasmodium vivax malaria treated with chloroquine". The Cochrane Database of Systematic Reviews (10): CD004389. doi:10.1002/14651858.CD004389.pub3. PMC 6532739. PMID 24163057.
- Milligan R, Daher A, Graves PM, et al. (Cochrane Infectious Diseases Group) (July 2019). "Primaquine at alternative dosing schedules for preventing relapse in people with Plasmodium vivax malaria". The Cochrane Database of Systematic Reviews. 7: CD012656. doi:10.1002/14651858.CD012656.pub2. PMC 6611223. PMID 31274189.
- Manyando C, Kayentao K, D'Alessandro U, Okafor HU, Juma E, Hamed K (2011). "A systematic review of the safety and efficacy of artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria during pregnancy". Malaria Journal. 11: 141. doi:10.1186/1475-2875-11-141. PMC 3405476. PMID 22548983.
- Orton LC, Omari AA, et al. (Cochrane Infectious Diseases Group) (October 2008). "Drugs for treating uncomplicated malaria in pregnant women". The Cochrane Database of Systematic Reviews (4): CD004912. doi:10.1002/14651858.CD004912.pub3. PMC 6532683. PMID 18843672.
- Kochar DK, Saxena V, Singh N, Kochar SK, Kumar SV, Das A (January 2005). "Plasmodium vivax malaria". Emerging Infectious Diseases. 11 (1): 132–4. doi:10.3201/eid1101.040519. PMC 3294370. PMID 15705338.
- Pasvol G (2005). "The treatment of complicated and severe malaria". British Medical Bulletin. 75-76: 29–47. doi:10.1093/bmb/ldh059. PMID 16495509.
- Sinclair D, Donegan S, Isba R, Lalloo DG (2012). Sinclair D (ed.). "Artesunate versus quinine for treating severe malaria". Cochrane Database of Systematic Reviews. 6 (6): CD005967. doi:10.1002/14651858.CD005967.pub4. PMC 6532684. PMID 22696354.
- Kyu HH, Fernández E (December 2009). "Artemisinin derivatives versus quinine for cerebral malaria in African children: a systematic review". Bulletin of the World Health Organization. 87 (12): 896–904. doi:10.2471/BLT.08.060327. PMC 2789363. PMID 20454480. Archived from the original on 2016-03-04.
- McIntosh HM, Olliaro P, et al. (Cochrane Infectious Diseases Group) (1998-07-27). "Artemisinin derivatives for treating severe malaria". The Cochrane Database of Systematic Reviews (2): CD000527. doi:10.1002/14651858.CD000527. PMC 6532607. PMID 10796551.
- Lesi A, Meremikwu M, et al. (Cochrane Infectious Diseases Group) (2004-07-19). "High first dose quinine regimen for treating severe malaria". The Cochrane Database of Systematic Reviews (3): CD003341. doi:10.1002/14651858.CD003341.pub2. PMC 6532696. PMID 15266481.
- Eisenhut M, Omari AA, et al. (Cochrane Infectious Diseases Group) (January 2009). "Intrarectal quinine versus intravenous or intramuscular quinine for treating Plasmodium falciparum malaria". The Cochrane Database of Systematic Reviews (1): CD004009. doi:10.1002/14651858.CD004009.pub3. PMC 6532585. PMID 19160229.
- Afolabi BB, Okoromah CN, et al. (Cochrane Infectious Diseases Group) (October 2004). "Intramuscular arteether for treating severe malaria". The Cochrane Database of Systematic Reviews (4): CD004391. doi:10.1002/14651858.CD004391.pub2. PMC 6532577. PMID 15495107.
- Okebe J, Eisenhut M, et al. (Cochrane Infectious Diseases Group) (May 2014). "Pre-referral rectal artesunate for severe malaria". The Cochrane Database of Systematic Reviews (5): CD009964. doi:10.1002/14651858.CD009964.pub2. PMC 4463986. PMID 24869943.
- Idro R, Marsh K, John CC, Newton CR (October 2010). "Cerebral malaria: mechanisms of brain injury and strategies for improved neurocognitive outcome". Pediatric Research. 68 (4): 267–74. doi:10.1203/pdr.0b013e3181eee738. PMC 3056312. PMID 20606600.
- Okoromah CA, Afolabi BB, Wall EC, et al. (Cochrane Infectious Diseases Group) (April 2011). "Mannitol and other osmotic diuretics as adjuncts for treating cerebral malaria". The Cochrane Database of Systematic Reviews (4): CD004615. doi:10.1002/14651858.CD004615.pub3. PMC 4018680. PMID 21491391.
- Meremikwu M, Marson AG, et al. (Cochrane Infectious Diseases Group) (2002-04-22). "Routine anticonvulsants for treating cerebral malaria". The Cochrane Database of Systematic Reviews (2): CD002152. doi:10.1002/14651858.CD002152. PMC 6532751. PMID 12076440.
- Prasad K, Garner P, et al. (Cochrane Infectious Diseases Group) (1999-07-26). "Steroids for treating cerebral malaria". The Cochrane Database of Systematic Reviews (2): CD000972. doi:10.1002/14651858.CD000972. PMC 6532619. PMID 10796562.
- Meremikwu M, Smith HJ, et al. (Cochrane Infectious Diseases Group) (1999-10-25). "Blood transfusion for treating malarial anaemia". The Cochrane Database of Systematic Reviews (2): CD001475. doi:10.1002/14651858.CD001475. PMC 6532690. PMID 10796646.
- Smith HJ, Meremikwu M, et al. (Cochrane Infectious Diseases Group) (2003-04-22). "Iron chelating agents for treating malaria". The Cochrane Database of Systematic Reviews (2): CD001474. doi:10.1002/14651858.CD001474. PMC 6532667. PMID 12804409.
- Sinha S, Medhi B, Sehgal R (2014). "Challenges of drug-resistant malaria". Parasite. 21: 61. doi:10.1051/parasite/2014059. PMC 4234044. PMID 25402734.
- O'Brien C, Henrich PP, Passi N, Fidock DA (2011). "Recent clinical and molecular insights into emerging artemisinin resistance in Plasmodium falciparum". Current Opinion in Infectious Diseases. 24 (6): 570–77. doi:10.1097/QCO.0b013e32834cd3ed. PMC 3268008. PMID 22001944.
- Fairhurst RM, Nayyar GM, Breman JG, Hallett R, Vennerstrom JL, Duong S, Ringwald P, Wellems TE, Plowe CV, Dondorp AM (2012). "Artemisinin-resistant malaria: research challenges, opportunities, and public health implications". American Journal of Tropical Medicine and Hygiene. 87 (2): 231–41. doi:10.4269/ajtmh.2012.12-0025. PMC 3414557. PMID 22855752.
- White NJ (2008). "Qinghaosu (artemisinin): The price of success". Science. 320 (5874): 330–34. Bibcode:2008Sci...320..330W. doi:10.1126/science.1155165. PMID 18420924.
- Wongsrichanalai C, Meshnick SR (2008). "Declining artesunate-mefloquine efficacy against falciparum malaria on the Cambodia–Thailand border". Emerging Infectious Diseases. 14 (5): 716–19. doi:10.3201/eid1405.071601. PMC 2600243. PMID 18439351.
- Dondorp AM, Yeung S, White L, Nguon C, Day NP, Socheat D, von Seidlein L (2010). "Artemisinin resistance: Current status and scenarios for containment". Nature Reviews Microbiology. 8 (4): 272–80. doi:10.1038/nrmicro2331. PMID 20208550.
- World Health Organization (2013). "Q&A on artemisinin resistance". WHO Malaria Publications. Archived from the original on 2016-07-20.
- Briggs, Helen (30 July 2014) Call for 'radical action' on drug-resistant malaria Archived 2014-07-31 at the Wayback Machine BBC News, health, Retrieved 30 July 2013
- Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. (July 2014). "Spread of artemisinin resistance in Plasmodium falciparum malaria". The New England Journal of Medicine. 371 (5): 411–23. doi:10.1056/NEJMoa1314981. PMC 4143591. PMID 25075834.
- Gallagher J (2019-07-23). "Resistant malaria spreading in South East Asia". Retrieved 2019-07-25.
- Orton L, Barnish G, et al. (Cochrane Infectious Diseases Group) (April 2005). "Unit-dose packaged drugs for treating malaria". The Cochrane Database of Systematic Reviews (2): CD004614. doi:10.1002/14651858.CD004614.pub2. PMC 6532754. PMID 15846723.
- "Frequently Asked Questions (FAQs): If I get malaria, will I have it for the rest of my life?". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on May 13, 2012. Retrieved 2012-05-14.
- Trampuz A, Jereb M, Muzlovic I, Prabhu R (2003). "Clinical review: Severe malaria". Critical Care. 7 (4): 315–23. doi:10.1186/cc2183. PMC 270697. PMID 12930555.
- Fernando SD, Rodrigo C, Rajapakse S (2010). "The 'hidden' burden of malaria: Cognitive impairment following infection". Malaria Journal. 9: 366. doi:10.1186/1475-2875-9-366. PMC 3018393. PMID 21171998.
- Riley EM, Stewart VA (2013). "Immune mechanisms in malaria: New insights in vaccine development". Nature Medicine. 19 (2): 168–78. doi:10.1038/nm.3083. PMID 23389617.
- Idro R, Marsh K, John CC, Newton CR (2010). "Cerebral malaria: Mechanisms of brain injury and strategies for improved neuro-cognitive outcome". Pediatric Research. 68 (4): 267–74. doi:10.1203/PDR.0b013e3181eee738. PMC 3056312. PMID 20606600.
- "Malaria". US Centers for Disease Control and Prevention. April 15, 2010. Archived from the original on April 16, 2012. Retrieved 2012-05-02.
- CDC-Centers for Disease Control and Prevention (28 January 2019). "CDC - Malaria - About Malaria - History - Elimination of Malaria in the United States (1947-1951)". www.cdc.gov. Retrieved 17 January 2020.
- Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. (October 2015). "The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015". Nature. 526 (7572): 207–211. Bibcode:2015Natur.526..207B. doi:10.1038/nature15535. PMC 4820050. PMID 26375008.
- Layne SP. "Principles of Infectious Disease Epidemiology" (PDF). EPI 220. UCLA Department of Epidemiology. Archived from the original (PDF) on 2006-02-20. Retrieved 2007-06-15.
- Provost C (April 25, 2011). "World Malaria Day: Which countries are the hardest hit? Get the full data". The Guardian. Archived from the original on August 1, 2013. Retrieved 2012-05-03.
- Murray CJ, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, Fullman N, Naghavi M, Lozano R, Lopez AD (2012). "Global malaria mortality between 1980 and 2010: A systematic analysis". Lancet. 379 (9814): 413–31. doi:10.1016/S0140-6736(12)60034-8. PMID 22305225.
- Guerra CA, Hay SI, Lucioparedes LS, Gikandi PW, Tatem AJ, Noor AM, Snow RW (2007). "Assembling a global database of malaria parasite prevalence for the Malaria Atlas Project". Malaria Journal. 6 (1): 17. doi:10.1186/1475-2875-6-17. PMC 1805762. PMID 17306022.
- Hay SI, Okiro EA, Gething PW, Patil AP, Tatem AJ, Guerra CA, Snow RW (2010). I (ed.). "Estimating the global clinical burden of Plasmodium falciparum malaria in 2007". PLOS Medicine. 7 (6): e1000290. doi:10.1371/journal.pmed.1000290. PMC 2885984. PMID 20563310.
- Gething PW, Patil AP, Smith DL, Guerra CA, Elyazar IR, Johnston GL, Tatem AJ, Hay SI (2011). "A new world malaria map: Plasmodium falciparum endemicity in 2010". Malaria Journal. 10 (1): 378. doi:10.1186/1475-2875-10-378. PMC 3274487. PMID 22185615.
- Weiss DJ, Lucas TC, Nguyen M, Nandi AK, Bisanzio D, Battle KE, et al. (July 2019). "Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000-17: a spatial and temporal modelling study". Lancet. 394 (10195): 322–331. doi:10.1016/S0140-6736(19)31097-9. PMC 6675740. PMID 31229234.
- Battle KE, Lucas TC, Nguyen M, Howes RE, Nandi AK, Twohig KA, et al. (July 2019). "Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000-17: a spatial and temporal modelling study". Lancet. 394 (10195): 332–343. doi:10.1016/S0140-6736(19)31096-7. PMC 6675736. PMID 31229233.
- World Malaria Report 2012 (PDF) (Report). World Health Organization. Archived (PDF) from the original on 2012-12-22.
- Feachem RG, Phillips AA, Hwang J, Cotter C, Wielgosz B, Greenwood BM, Sabot O, Rodriguez MH, Abeyasinghe RR, Ghebreyesus TA, Snow RW (2010). "Shrinking the malaria map: progress and prospects". Lancet. 376 (9752): 1566–78. doi:10.1016/S0140-6736(10)61270-6. PMC 3044848. PMID 21035842.
- Greenwood B, Mutabingwa T (2002). "Malaria in 2002". Nature. 415 (6872): 670–72. doi:10.1038/415670a. PMID 11832954.
- Jamieson A, Toovey S, Maurel M (2006). Malaria: A Traveller's Guide. Struik. p. 30. ISBN 978-1-77007-353-1. Archived from the original on 2016-05-11.
- Abeku TA (2007). "Response to malaria epidemics in Africa". Emerging Infectious Diseases. 13 (5): 681–86. doi:10.3201/eid1305.061333. PMC 2738452. PMID 17553244.
- Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, Fan Q, Fang Q, Jongwutiwes S, Parker D, Sirichaisinthop J, Kyaw MP, Su XZ, Yang H, Yang Z, Wang B, Xu J, Zheng B, Zhong D, Zhou G (2012). "Malaria in the Greater Mekong Subregion: Heterogeneity and complexity". Acta Tropica. 121 (3): 227–39. doi:10.1016/j.actatropica.2011.02.016. PMC 3132579. PMID 21382335.
- Machault V, Vignolles C, Borchi F, Vounatsou P, Pages F, Briolant S, Lacaux JP, Rogier C (2011). "The use of remotely sensed environmental data in the study of malaria" (PDF). Geospatial Health. 5 (2): 151–68. doi:10.4081/gh.2011.167. PMID 21590665. Archived from the original (PDF) on 2013-03-12.
- Harper K, Armelagos G (2011). "The changing disease-scape in the third epidemiological transition". International Journal of Environmental Research and Public Health. 7 (2): 675–97. doi:10.3390/ijerph7020675. PMC 2872288. PMID 20616997.
- Prugnolle F, Durand P, Ollomo B, Duval L, Ariey F, Arnathau C, Gonzalez JP, Leroy E, Renaud F (2011). Manchester M (ed.). "A fresh look at the origin of Plasmodium falciparum, the most malignant malaria agent". PLOS Pathogens. 7 (2): e1001283. doi:10.1371/journal.ppat.1001283. PMC 3044689. PMID 21383971.
- Cox F (2002). "History of human parasitology". Clinical Microbiology Reviews. 15 (4): 595–612. doi:10.1128/CMR.15.4.595-612.2002. PMC 126866. PMID 12364371.
- Strong RP (1944). Stitt's Diagnosis, Prevention and Treatment of Tropical Diseases (Seventh ed.). York, PA: The Blakiston Company. p. 3.
- "DNA clues to malaria in ancient Rome". BBC News. February 20, 2001. Archived from the original on November 2, 2010., in reference to Sallares R, Gomzi S (2001). "Biomolecular archaeology of malaria". Ancient Biomolecules. 3 (3): 195–213. OCLC 538284457.
- Sallares R (2002). Malaria and Rome: A History of Malaria in Ancient Italy. Oxford University Press. doi:10.1093/acprof:oso/9780199248506.001.0001. ISBN 978-0-19-924850-6.
- Hays JN (2005). Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, CA: ABC-CLIO. p. 11. ISBN 978-1-85109-658-9. Archived from the original on 2016-05-02.
- McKissack P, McKissack F (1995). The Royal Kingdoms of Ghana, Mali, and Songhay Life in Medieval Africa. Macmillan. p. 104. ISBN 978-0-8050-4259-7.
- Reiter P (1999). "From Shakespeare to Defoe: malaria in England in the Little Ice Age". Emerging Infectious Diseases. 6 (1): 1–11. doi:10.3201/eid0601.000101. PMC 2627969. PMID 10653562.
- Lindemann M (1999). Medicine and Society in Early Modern Europe. Cambridge University Press. p. 62. ISBN 978-0-521-42354-0. Archived from the original on 2016-04-26.
- Gratz NG, World Health Organization (2006). The Vector- and Rodent-borne Diseases of Europe and North America: Their Distribution and Public Health Burden. Cambridge University Press. p. 33. ISBN 978-0-521-85447-4. Archived from the original on 2016-06-29.
- Webb Jr JL (2009). Humanity's Burden: A Global History of Malaria. Cambridge University Press. ISBN 978-0-521-67012-8. Archived from the original on 2016-04-27.
- "The Nobel Prize in Physiology or Medicine 1907: Alphonse Laveran". The Nobel Foundation. Archived from the original on 2012-06-23. Retrieved 2012-05-14.
- Tan SY, Sung H (2008). "Carlos Juan Finlay (1833–1915): Of mosquitoes and yellow fever" (PDF). Singapore Medical Journal. 49 (5): 370–71. PMID 18465043. Archived (PDF) from the original on 2008-07-23.
- Chernin E (1983). "Josiah Clark Nott, insects, and yellow fever". Bulletin of the New York Academy of Medicine. 59 (9): 790–802. PMC 1911699. PMID 6140039.
- Chernin E (1977). "Patrick Manson (1844–1922) and the transmission of filariasis". American Journal of Tropical Medicine and Hygiene. 26 (5 Pt 2 Suppl): 1065–70. doi:10.4269/ajtmh.1977.26.1065. PMID 20786.
- Cox FE (February 2010). "History of the discovery of the malaria parasites and their vectors". Parasites & Vectors. 3 (1): 5. doi:10.1186/1756-3305-3-5. PMC 2825508. PMID 20205846.
- "Ross and the Discovery that Mosquitoes Transmit Malaria Parasites". CDC Malaria website. Archived from the original on 2007-06-02. Retrieved 2012-06-14.
- Simmons JS (1979). Malaria in Panama. Ayer Publishing. ISBN 978-0-405-10628-6. Archived from the original on 2016-05-21.
- "Amico Bignami". www.whonamedit.com. Retrieved 30 July 2019.
- Kaufman TS, Rúveda EA (2005). "The quest for quinine: Those who won the battles and those who won the war". Angewandte Chemie International Edition in English. 44 (6): 854–85. doi:10.1002/anie.200400663. PMID 15669029.
- Pelletier PJ, Caventou JB (1820). "Des recherches chimiques sur les Quinquinas" [Chemical research on quinquinas]. Annales de Chimie et de Physique (in French). 15: 337–65. Archived from the original on 2016-05-04.
- Kyle R, Shampe M (1974). "Discoverers of quinine". Journal of the American Medical Association. 229 (4): 462. doi:10.1001/jama.229.4.462. PMID 4600403.
- Achan J, Talisuna AO, Erhart A, Yeka A, Tibenderana JK, Baliraine FN, Rosenthal PJ, D'Alessandro U (2011). "Quinine, an old anti-malarial drug in a modern world: Role in the treatment of malaria". Malaria Journal. 10 (1): 144. doi:10.1186/1475-2875-10-144. PMC 3121651. PMID 21609473.
- Hsu E (2006). "Reflections on the 'discovery' of the antimalarial qinghao". British Journal of Clinical Pharmacology. 61 (3): 666–70. doi:10.1111/j.1365-2125.2006.02673.x. PMC 1885105. PMID 16722826.
- Hao C (29 September 2011). "Lasker Award Rekindles Debate Over Artemisinin's Discovery". News: ScienceInsider. Science/AAAS. Archived from the original on 4 January 2014.
- "Nobel Prize announcement" (PDF). NobelPrize.org. Archived (PDF) from the original on 6 October 2015. Retrieved 5 October 2015.
- Vogel V (2013). "The Forgotten Malaria". Science. 342 (6159): 684–87. Bibcode:2013Sci...342..684V. doi:10.1126/science.342.6159.684. PMID 24202156.
- "Eradication of Malaria in the United States (1947–1951)". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on May 4, 2012. Retrieved 2012-05-02.
- Killeen G, Fillinger U, Kiche I, Gouagna L, Knols B (2002). "Eradication of Anopheles gambiae from Brazil: Lessons for malaria control in Africa?". Lancet Infectious Diseases. 2 (10): 618–27. doi:10.1016/S1473-3099(02)00397-3. PMID 12383612.
- Vanderberg JP (2009). "Reflections on early malaria vaccine studies, the first successful human malaria vaccination, and beyond". Vaccine. 27 (1): 2–9. doi:10.1016/j.vaccine.2008.10.028. PMC 2637529. PMID 18973784.
- Walsh F (24 July 2015). "Malaria vaccine gets 'green light'". BBC News Online. Archived from the original on 21 December 2016.
- Humphreys M (2001). Malaria: Poverty, Race, and Public Health in the United States. Johns Hopkins University Press. p. 256. ISBN 0-8018-6637-5.
- Sachs J, Malaney P (2002). "The economic and social burden of malaria". Nature. 415 (6872): 680–85. doi:10.1038/415680a. PMID 11832956.
- Roll Back Malaria WHO partnership (2003). "Economic costs of malaria" (PDF). WHO. Archived from the original (PDF) on 2009-12-29.
- Ricci F (2012). "Social implications of malaria and their relationships with poverty". Mediterranean Journal of Hematology and Infectious Diseases. 4 (1): e2012048. doi:10.4084/MJHID.2012.048. PMC 3435125. PMID 22973492.
- Lon CT, Tsuyuoka R, Phanouvong S, Nivanna N, Socheat D, Sokhan C, Blum N, Christophel EM, Smine A (2006). "Counterfeit and substandard antimalarial drugs in Cambodia". Transactions of the Royal Society of Tropical Medicine and Hygiene. 100 (11): 1019–24. doi:10.1016/j.trstmh.2006.01.003. PMID 16765399.
- Newton PN, Fernández FM, Plançon A, Mildenhall DC, Green MD, Ziyong L, Christophel EM, Phanouvong S, Howells S, McIntosh E, Laurin P, Blum N, Hampton CY, Faure K, Nyadong L, Soong CW, Santoso B, Zhiguang W, Newton J, Palmer K (2008). "A collaborative epidemiological investigation into the criminal fake artesunate trade in South East Asia". PLOS Medicine. 5 (2): e32. doi:10.1371/journal.pmed.0050032. PMC 2235893. PMID 18271620.
- Newton PN, Green MD, Fernández FM, Day NP, White NJ (2006). "Counterfeit anti-infective drugs". Lancet Infectious Diseases. 6 (9): 602–13. doi:10.1016/S1473-3099(06)70581-3. PMID 16931411.}
- Parry J (2005). "WHO combats counterfeit malaria drugs in Asia". British Medical Journal. 330 (7499): 1044. doi:10.1136/bmj.330.7499.1044-d. PMC 557259. PMID 15879383.
- Gautam CS, Utreja A, Singal GL (2009). "Spurious and counterfeit drugs: A growing industry in the developing world". Postgraduate Medical Journal. 85 (1003): 251–56. doi:10.1136/pgmj.2008.073213. PMID 19520877.
- Caudron JM, Ford N, Henkens M, Macé, Kidle-Monroe R, Pinel J (2008). "Substandard medicines in resource-poor settings: A problem that can no longer be ignored" (PDF). Tropical Medicine & International Health. 13 (8): 1062–72. doi:10.1111/j.1365-3156.2008.02106.x. hdl:10144/37334. PMID 18631318.
- Nayyar GM, Breman JG, Newton PN, Herrington J (2012). "Poor-quality antimalarial drugs in southeast Asia and sub-Saharan Africa". Lancet Infectious Diseases. 12 (6): 488–96. doi:10.1016/S1473-3099(12)70064-6. PMID 22632187.
- Russell PF (2009). "Communicable diseases Malaria". Medical Department of the United States Army in World War II. U.S. Army Medical Department. Office of Medical History. Archived from the original on October 9, 2012. Retrieved 2012-09-24.
- Melville CH (1910). "The prevention of malaria in war". In Ross R (ed.). The Prevention of Malaria. New York: E.P. Dutton. p. 577. Archived from the original on 2016-03-12.
- Bryant BJ, Knights KM (2011). Pharmacology for Health Professionals. Elsevier Australia. p. 895. ISBN 9780729539296.
- Bray RS (2004). Armies of Pestilence: The Effects of Pandemics on History. James Clarke. p. 102. ISBN 978-0-227-17240-7. Archived from the original on 2016-08-21.
- Byrne JP (2008). Encyclopedia of Pestilence, Pandemics, and Plagues: A-M. ABC-CLIO. p. 383. ISBN 978-0-313-34102-1. Archived from the original on 2013-12-03.
- Kakkilaya BS (April 14, 2006). "History of Malaria During Wars". Malariasite.com. Archived from the original on April 3, 2012. Retrieved 2012-05-03.
- "History | CDC Malaria". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on August 28, 2010. Retrieved 2012-05-15.
- Strom S (April 1, 2011). "Mission Accomplished, Nonprofits Go Out of Business". The New York Times. nytimes.com. OCLC 292231852. Archived from the original on December 25, 2011. Retrieved 2012-05-09.
- "Fighting AIDS, Tuberculosis and Malaria". The Global Fund. Archived from the original on 2012-05-05. Retrieved 2012-05-09.
- Schoofs M (July 17, 2008). "Clinton foundation sets up malaria-drug price plan". Wall Street Journal. Archived from the original on January 19, 2016. Retrieved 2012-05-14.
- "Executive summary and key points" (PDF). World Malaria Report 2013. World Health Organization. Archived (PDF) from the original on 4 March 2016. Retrieved 13 February 2014.
- "World Malaria Report 2013" (PDF). World Health Organization. Retrieved 13 February 2014.
- Meade MS, Emch M (2010). Medical Geography (3rd ed.). Guilford Press. pp. 120–23. ISBN 978-1-60623-016-9. Archived from the original on 2016-04-23.
- Williams LL (1963). "Malaria eradication in the United States". American Journal of Public Health and the Nation's Health. 53 (1): 17–21. doi:10.2105/AJPH.53.1.17. PMC 1253858. PMID 14000898.
- Fletcher M (2018-08-11). "Mutant mosquitoes: Can gene editing kill off malaria?". The Telegraph. ISSN 0307-1235. Retrieved 2018-08-12.
- Radwick D (October 5, 2016). "Can Malaria Be Eradicated?". Council on Foreign Relations. Archived from the original on October 5, 2016.
- "WHO certifies Paraguay malaria-free". World Health Organization. 11 June 2018. Retrieved 17 June 2018.
- "Malaria eradication: benefits, future scenarios and feasibility. Executive summary of the report of the WHO Strategic Advisory Group on Malaria Eradication". www.who.int. Retrieved 2019-08-25.
- Mendis K (September 2019). "Eliminating malaria should not be the end of vigilance". Nature. 573 (7772): 7. doi:10.1038/d41586-019-02598-1. PMID 31485061.
- Hall BF, Fauci AS (December 2009). "Malaria control, elimination, and eradication: the role of the evolving biomedical research agenda". The Journal of Infectious Diseases. 200 (11): 1639–43. doi:10.1086/646611. PMID 19877843.
- "WHO | A research agenda for malaria eradication". www.who.int. Archived from the original on 2016-03-07. Retrieved 2016-03-07.
- World Health Organization (March 2020). "Q&A on the malaria vaccine implementation programme (MVIP)". WHO. Retrieved 6 May 2020.
- Hill AV (2011). "Vaccines against malaria". Philosophical Transactions of the Royal Society B. 366 (1579): 2806–14. doi:10.1098/rstb.2011.0091. PMC 3146776. PMID 21893544.
- Crompton PD, Pierce SK, Miller LH (2010). "Advances and challenges in malaria vaccine development". Journal of Clinical Investigation. 120 (12): 4168–78. doi:10.1172/JCI44423. PMC 2994342. PMID 21123952.
- Graves P, Gelband H (2006). Graves PM (ed.). "Vaccines for preventing malaria (blood-stage)". Cochrane Database of Systematic Reviews (4): CD006199. doi:10.1002/14651858.CD006199. PMC 6532641. PMID 17054281.
- Graves P, Gelband H (2006). Graves PM (ed.). "Vaccines for preventing malaria (SPf66)". Cochrane Database of Systematic Reviews (2): CD005966. doi:10.1002/14651858.CD005966. PMC 6532709. PMID 16625647.
- Kalanon M, McFadden GI (2010). "Malaria, Plasmodium falciparum and its apicoplast". Biochemical Society Transactions. 38 (3): 775–82. doi:10.1042/BST0380775. PMID 20491664.
- Müller IB, Hyde JE, Wrenger C (2010). "Vitamin B metabolism in Plasmodium falciparum as a source of drug targets". Trends in Parasitology. 26 (1): 35–43. doi:10.1016/j.pt.2009.10.006. PMID 19939733.
- Du Q, Wang H, Xie J (2011). "Thiamin (vitamin B1) biosynthesis and regulation: A rich source of antimicrobial drug targets?". International Journal of Biological Sciences. 7 (1): 41–52. doi:10.7150/ijbs.7.41. PMC 3020362. PMID 21234302.
- Biot C, Castro W, Botté CY, Navarro M (2012). "The therapeutic potential of metal-based antimalarial agents: Implications for the mechanism of action". Dalton Transactions. 41 (21): 6335–49. doi:10.1039/C2DT12247B. PMID 22362072.
- Roux C, Biot C (2012). "Ferrocene-based antimalarials". Future Medicinal Chemistry. 4 (6): 783–97. doi:10.4155/fmc.12.26. PMID 22530641.
- John C (8 December 2014). "New malaria drug unleashes an immune system assault on infected cells". fiercebiotechresearch.com. Archived from the original on 4 April 2016. Retrieved 16 December 2014.
- Aultman KS, Gottlieb M, Giovanni MY, Fauci AS (2002). "Anopheles gambiae genome: completing the malaria triad". Science. 298 (5591): 13. doi:10.1126/science.298.5591.13. PMID 12364752.
- Ito J, Ghosh A, Moreira LA, Wimmer EA, Jacobs-Lorena M (2002). "Transgenic anopheline mosquitoes impaired in transmission of a malaria parasite". Nature. 417 (6887): 452–55. Bibcode:2002Natur.417..452I. doi:10.1038/417452a. PMID 12024215.
- Gantz VM, Jasinskiene N, Tatarenkova O, Fazekas A, Macias VM, Bier E, James AA (December 2015). "Highly efficient Cas9-mediated gene drive for population modification of the malaria vector mosquito Anopheles stephensi". Proceedings of the National Academy of Sciences of the United States of America. 112 (49): E6736-43. doi:10.1073/pnas.1521077112. PMC 4679060. PMID 26598698.
- Flam F (4 February 2016). "Fighting Zika Virus With Genetic Engineering". Bloomberg. Archived from the original on 6 June 2016.
- Rich SM, Ayala FJ (2006). "Evolutionary origins of human malaria parasites". In Dronamraju KR, Arese P (eds.). Malaria: Genetic and Evolutionary Aspects. New York: Springer. pp. 125–46. ISBN 978-0-387-28294-7.
- Baird JK (2009). "Malaria zoonoses". Travel Medicine and Infectious Disease. 7 (5): 269–77. doi:10.1016/j.tmaid.2009.06.004. PMID 19747661.
- Ameri M (2010). "Laboratory diagnosis of malaria in nonhuman primates". Veterinary Clinical Pathology. 39 (1): 5–19. doi:10.1111/j.1939-165X.2010.00217.x. PMID 20456124.
- Mlambo G, Kumar N (2008). "Transgenic rodent Plasmodium berghei parasites as tools for assessment of functional immunogenicity and optimization of human malaria vaccines". Eukaryotic Cell. 7 (11): 1875–79. doi:10.1128/EC.00242-08. PMC 2583535. PMID 18806208.
- Lapointe DA, Atkinson CT, Samuel MD (2012). "Ecology and conservation biology of avian malaria". Annals of the New York Academy of Sciences. 1249 (1): 211–26. Bibcode:2012NYASA1249..211L. doi:10.1111/j.1749-6632.2011.06431.x. PMID 22320256.
- Cited literature
- WHO (2010). Guidelines for the Treatment of Malaria (PDF) (Report) (2nd ed.). World Health Organization. ISBN 978-92-4-154792-5.CS1 maint: ref=harv (link)
- Schlagenhauf-Lawlor P (2008). Travelers' Malaria. PMPH-USA. ISBN 978-1-55009-336-0.CS1 maint: ref=harv (link)
Further reading
- Bynum WF, Overy C, eds. (1998). The Beast in the Mosquito: The Correspondence of Ronald Ross and Patrick Manson. Wellcome Institute Series in The History of Medicine. Rodopi. ISBN 978-90-420-0721-5.
- Guidelines for the treatment of malaria (3rd ed.). World Health Organization. 2015. ISBN 978-92-4-154912-7.
- Jarvis B (29 July 2019). "How Mosquitoes Changed Everything". Retrieved 8 August 2019.
- "Tightening the handle on malaria". Nature Methods (Editorial). 16 (4): 271. 28 March 2019. doi:10.1038/s41592-019-0390-2. PMID 30923375.
A day dedicated to raising awareness of the disease is a good opportunity to ask how far malaria research has come and which methods are needed for further breakthroughs.
External links
| Classification | |
|---|---|
| External resources |
| Wikiquote has quotations related to: Malaria |
- Malaria at Curlie
- WHO site on malaria
- UNHCO site on malaria
- Global Malaria Action Plan (2008)
- Doctors Without Borders/Médecins Sans Frontières – Malaria information pages
- WHO/TDR Malaria Database via the Wayback Machine
- Anti-malaria and sustainable development
- Worldwide Antimalarial Resistance Network (WWARN)
