Quartan fever
Quartan fever is one of the four types of malaria which can be contracted by humans.[1]
It is specifically caused by the Plasmodium malariae species, one of the six species of the protozoan genus Plasmodium. Quartan fever is a form of malaria where an onset of fever occurs in an interval of three-four days, hence the name "quartan."[2] It is transmitted by bites of infected female mosquitoes of the genus Anopheles. Symptoms include fevers which range from approximately 40–41°C and occur periodically in 72 hour intervals. Although cases of Malaria have occurred throughout the world, quartan fever typically occurs in sub-tropic regions. Quartan fever is considered to be a less severe form of malaria fever can be cured by anti-malarial treatments and prevention methods can be taken in order to avoid infection.[1]
| Quartan Fever | |
|---|---|
 | |
| P. malariae | |
| Specialty | Infectious disease |
| Symptoms | Fever, |
| Duration | Fever in 72 hour intervals |
| Causes | Plasmodium spread by mosquitos |
| Diagnostic method | Blood tests |
| Medication | Chloroquine |
Cause
The female Anopheles mosquito is a vector which transmits quartan fever to people. Mature mosquitoes carry uninucleate sporozoites in their salivary glands, these sporozoites enter a human's bloodstream when mosquitoes puncture human flesh during feeding. Sporozoites attack and inhabit liver parenchymal cells in order to develop. Once the uninucleate sporozoites have matured the sporozoites then develop into uninucleate merozoites. Uninucleated merozoites mature into an erythrocytic stage schizonts which contain merozoites. The schizonts then rupture to release these merozoites; leading to more infections in the red blood cells. Uninucleated merozoites can also mature into uninucleate gametocytes which can invade and infect other female Anopheles mosquitoes during feeding, thus spreading the disease onto a wider population of humans.[1]
Diagnosis
Fevers in intervals of 72 hours distinguish quartan fever from other forms of malaria where fevers range in 48 hour intervals or fever spikes happen sporadically.[1]
Early indications of catching quartan fever include having irritated spots, welts, hives, burning skin, however this is dependent on individual's tolerance to mosquito bites and may not show up on some people. With anopheles malaria mosquitoes the welts are most likely to not appear unless there are severe allergic reactions.[3]
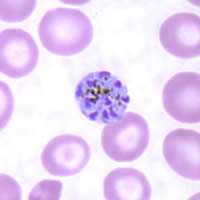
The prepatent period is the time interval for when parasites are detected on a thick blood film. For quartan fever, P. malariae has a prepatent period ranging from 16-59 days. Specifically in the case of quartan fever, the rupturing of liver stage schizonts releases merozoites. This stage of the P. malariae life cycle is known as the "ring stages" and are the first stages which can be detected in human blood for diagnosis.[4]
Medical procedures that diagnose a patient with quartan fever
- Blood smears can be used to detect the parasites within red blood cells, thick blood smears are typically used initially to detect the parasites, then it is followed by thin blood smears which can detect the parasites as the morphology of erythrocytes is maintained through the process.[5]
- Peripheral blood films stained with Giemsa strain are a method of blood examination used to diagnose the presence of Plasmodium malariae, and detect quartan fever.[4]
- Rapid diagnostic tests can detect antigens which cause malaria, a sample of blood is collected from the patient and placed on a test card. After 15-20 minutes bands show up on the test card which indicate the specific species of malaria the patient is infected with.[5]
- Serological tests are used in general to detect whether a patient has developed antibodies to specific microorganism,[6] therefore Serological tests are used to detect past encounters with Plasmodium virus rather than cases where a patient has newly come in contain/has been infected with P. malariae and has quartan fever.[5]
- Polymerase chain reactions (PCR) are used to diagnosis Plasmodium malariae (cause of quartan fever) as well to separate mixed infections.[4]
Treatment
- Chloroquine is administered in the form of a tablet for ingestion. [7]
- Chloroquine is a water-soluble drug which is used to treat quartan fever. Chloroquine a suppressive drug which is ingested in a compressed tablet form and is mainly absorbed by the gastrointestinal tract.[7]
- Hydrochloroquine is also a suppressive, anit-malarial agent used to treat quartan fever. Hydrochloroquine is also typically administered to patients suffering from lupus flares.
- Both hydrochloroquine and chloroquine have a side effect of retinal toxicity when administered to infected patients.[8]
- Adverse effects of the drug chloroquine include agitation, anxiety, confusion, Gastrointestinal discomfort,[8] blurring vision, and/or irreversible retinal damage.
- Sulfadoxine-pyrimethamine (SP) is administered to pregnant women during the gestation period. Two-three doses of SP has been proven to reduce the levels of placental malaria and had a reduced risk of moderate to severe anemia.[9]
Prevention
Ways to minimise exposure to the Anopheles mosquito include:
- Indoor residual sprays are one of the most utilised methods of malaria prevention by the Global Malaria Eradication Campaign. Spraying is a method in multiple regions and to control epidemics.[10]
- Nets treated with insecticide are effective in preventing mosquito contact for three years. The World Health Organisation (WHO) specifically targets younger children and pregnant women in order to reduce the risk of spreading Quartan fever within the population. [10]
- Sulfadoxine-pyrimethamine (SP) administration to pregnant women is also a source of prevention in order to reduce the risks of maternal anaemia, low birth rate, and perinatal mortality. SP reduces the impact Quartan fever may have on newborns and decrease the morality rate. This method of prevention is known as "chemoprevention." [9]
- House improvement is also a method of prevention. Traditional houses consisting of natural materials are susceptible to gaps which allow entry to infected Anopheles mosquitoes. House improvements including windows, installation and sealed doors reduce the risk of coming in contact with the infected mosquitoes. [10]
- Larval source management is the control and monitoring of aquatic environments in order to prevent fully Anopheles mosquitoes from fully developing.[10] Mosquitoes require aquatic environments in order to fully mature and develop. Once mosquito eggs hatch, the larva must live in the water and develop into pupa. The pupa stage then matures into a fully developed mosquito and emerges from its aquatic habitat. When removing any water-filled containers from the surrounding area the mosquito life cycle is halted and acts as a method to reduce mosquito population within the surrounding area.[11]
- Clothing can act as a physical barrier to prevent exposure of flesh for mosquitoes to feed on, treating beds and clothing with insecticides/repellents can further reduce chances of infected mosquitoes from biting and passing quartan fever to individuals.[10]
- Avoiding areas which have high mosquito populations, specifically for quartan fever the P. malariae strain.[10]
- Avoiding travelling to regions which have a sub-tropic climate to prevent infection and developing quartan fever.[10]
- Implementing the sugar baiting method aids in reducing the population of Anopheles mosquitoes, and ultimately reducing the likelihood of catching quartan fever. Both male and female mosquitoes feed on the Attractive toxic sugar bait (ATSB) and ingest low-risk oral toxins e.g. boric acid. This leads to mosquito death and reduces population.[12]
References
- Crutcher, James M. (1996). Medical Microbiology. 4th edition. Galveston: The University of Texas Medical Branch at Galveston.
- "quartan". English Oxford living Dictionaries. 2019. Retrieved 29 March 2019.
- "Insect Bite Prevention". IAMAT. 25 January 2019. Retrieved 13 May 2019.
- Collins, William E. (2007). "Plasmodium malariae: Parasite and Disease". Clinical Microbiology Reviews. 20 (4): 579–592. doi:10.1128/CMR.00027-07. PMC 2176047. PMID 17934075.
- "Rapid Diagnostic Tests: How They Work". CDC. 2018. Retrieved 9 May 2019.
- "AIDS info". HIV/AIDS Glossary. Retrieved 9 May 2019.
- "LABEL: CHLOROQUINE- chloroquine phosphate tablet". DAILY MED. 8 July 2010. Retrieved 10 May 2019.
- "Malaria". 2019. Retrieved 10 May 2019.
- Kayentao, K (23 February 2012). "Intermittent preventive therapy for malaria during pregnancy using 2 vs 3 or more doses of sulfadoxine-pyrimethamine and risk of low birth weight in Africa: systematic review and meta-analysis". JAMA. 309 (6): 594–604. doi:10.1001/jama.2012.216231. PMC 4669677. PMID 23403684.
- Tizifa, Tinashe A (8 February 2018). "Prevention Efforts for Malaria". Current Tropical Medicine Reports. 5 (1): 41–50. doi:10.1007/s40475-018-0133-y. PMC 5879044. PMID 29629252.
- "Mosquito Life Cycle". EPA. 13 March 2017. Retrieved 3 May 2019.
- C Beier, John (1 February 2012). "Attractive toxic sugar bait (ATSB) methods decimate populations of Anopheles malaria vectors in arid environments regardless of the local availability of favoured sugar-source blossoms". Malaria Journal. 11: 31. doi:10.1186/1475-2875-11-31. PMC 3293779. PMID 22297155.