Ketorolac
Ketorolac, sold under the brand name Toradol among others, is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain.[1] Specifically it is recommended for moderate to severe pain.[2] Recommended duration of treatment is less than six days.[1] It is used by mouth, by nose, by injection into a vein or muscle, and as eye drops.[1][2] Effects begin within an hour and last for up to eight hours.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Toradol, Acular, Sprix, others |
| Other names | Ketorolac tromethamine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a693001 |
| License data | |
| Pregnancy category | |
| Routes of administration | By mouth, under the tongue, IM, IV, eye drops, nasal spray |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 80 - 100% (oral) 100% IV/IM |
| Metabolism | Liver |
| Elimination half-life | 3.5 h to 9.2 h, young adults; 4.7 h to 8.6 h, elderly (mean age 72) |
| Excretion | Kidney: 91.4% (mean) Biliary: 6.1% (mean) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.110.314 |
| Chemical and physical data | |
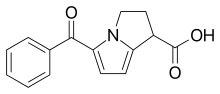
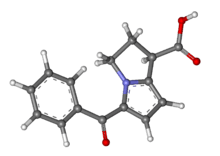
| Formula | C15H13NO3 |
| Molar mass | 255.273 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| | |
Common side effects include sleepiness, dizziness, abdominal pain, swelling, and nausea.[1] Serious side effects may include stomach bleeding, kidney failure, heart attacks, bronchospasm, heart failure, and anaphylaxis.[1] Use is not recommended during the last part of pregnancy or during breastfeeding.[1] Ketorolac works by blocking cyclooxygenase 1 and 2 (COX1 and COX2), thereby decreasing production of prostaglandins.[1][3]
Ketorolac was patented in 1976 and approved for medical use in 1989.[4][1] It is available as a generic medication.[2] In the United Kingdom it costs the NHS less than £1 per injectable dose as of 2019.[2] In the United States the wholesale cost of this amount is about US$1.50.[5] In 2017, it was the 271st most commonly prescribed medication in the United States, with more than one million prescriptions.[6][7]
Medical uses
.jpg)
Ketorolac is used for short-term management of moderate to severe pain.[8] It is usually not prescribed for longer than five days,[9][10][11][12] due to its potential to cause kidney damage.[13]
Ketorolac is effective when administered with paracetamol to control pain in newborns because it does not depress respiration as do opioids.[14] Ketorolac is also an adjuvant to opioid medications and improves pain relief. It is also used to treat dysmenorrhea.[12] Ketorolac is used to treat idiopathic pericarditis, where it reduces inflammation.[15]
For systemic use, ketorolac can be administered orally, under the tongue, by intramuscular injection, intravenously, and by nasal spray.[9] Usually, it is initially administered by intramuscular injection or intravenously,[8] with oral therapy used as a continuation after the initial IM or IV dose.[9][14]
Ketorolac is also used as an eye drop. It can be given during eye surgery to help with pain,[16] and is effective in treating ocular itching.[17] The eye drops are associated with decreased development of macular edema after cataract surgery, and is more effective alone than as an opioid/ketorolac combination treatment.[18][19] Ketorolac eye drops have also been used to manage pain from corneal abrasions.[20]
During treatment with ketorolac, clinicians monitor for the manifestation of adverse effects. Lab tests, such as liver function tests, bleeding time, BUN, serum creatinine and electrolyte levels are often used and help to identify potential complications.[9][10]
Contraindications
Ketorolac is contraindicated in those with hypersensitivity, allergies to the medication, cross-sensitivity to other NSAIDs, prior to surgery, history of peptic ulcer disease, gastrointestinal bleeding, alcohol intolerance, renal impairment, cerebrovascular bleeding, nasal polyps, angioedema, and asthma.[9][10] Recommendations exist for cautious use of ketorolac in those who have experienced cardiovascular disease, myocardial infarction, stroke, heart failure, coagulation disorders, renal impairment, and hepatic impairment.[9][10]
Adverse effects
A common (>10%) side effect is drowsiness. Infrequent (<1%) side effects include paresthesia, prolonged bleeding time, injection site pain, purpura, sweating, abnormal thinking, increased production of tears, edema, pallor, dry mouth, abnormal taste, urinary frequency, increased liver enzymes, itching and others. Platelet function can be decreased by use of ketorolac.[21]
Though uncommon, potentially fatal adverse effects include stroke, myocardial infarction, GI bleeding, Stevens–Johnson syndrome, toxic epidermal necrolysis and anaphylaxis. In terms of safety, ketorolac has been assessed to be a relatively higher-risk NSAID when compared to aceclofenac, celecoxib, and ibuprofen.[15]
Like all NSAIDs, ketorolac can cause premature constriction of the ductus arteriosus in the infant if taken by the mother during the third trimester of pregnancy.[9][10]
Interactions
Ketorolac can interact with other medications. Probenecid can increase the probability of having an adverse reaction when taken with ketorolac. Pentoxifylline can increase the risk of bleeding. When aspirin is taken at the same time as ketorolac, the effectiveness is decreased. Problematic GI effects are additive and become more likely if potassium supplements, aspirin, other NSAIDs, corticosteroids, or alcohol is taken at the same time. The effectiveness of antihypertensives and diuretics can be lowered. The use of ketorolac can increase serum lithium levels to the point of toxicity. Toxicity to methotrexate is more likely if ketorolac is taken at the same time. The risk of bleeding increases with the concurrent medications clopidogrel, cefoperazone, valproic acid, cefotetan, eptifibatide, tirofiban, and ticlopidine. Anticoagulants and thrombolytic medications also increase the likelihood of bleeding. Medications used to treat cancer can interact with ketorolac along with radiation therapy. The risk of toxicity to the kidneys increases when ketorolac is taken with cyclosporine.[9][10]
Interactions with ketorolac also exist with some herbal supplements. The use of Panax ginseng, clove, ginger, arnica, feverfew, dong quai, chamomile, and Ginkgo biloba increases the risk of bleeding.[9][10]
Mechanism of action
Chemically ketorolac functions as a carboxylic acid derivative serving non-selectively to block the prostaglandin synthesis by inhibition of prostaglandin G/H synthesis one and two. Prostaglandin functions in the body as a messenger for contraction/relaxation of smooth muscle and modulation of inflammation. Resultant, inhibition of prostaglandin synthesis prevents inflammation.[22] The primary mechanism of action responsible for ketorolac's anti-inflammatory, antipyretic and analgesic effects is the inhibition of prostaglandin synthesis by competitive blocking of the enzyme cyclooxygenase (COX). Ketorolac is a non-selective COX inhibitor.[23] It is considered a first-generation NSAID.[21]
History
In the US, ketorolac is the only widely available intravenous NSAID. An IV form of paracetamol, which is not an NSAID, became available in Europe in 2009 and then in the US.[14]
The Syntex company, of Palo Alto, California developed the ophthalmic solution Acular around 2006.
In 2007, there were concerns about the high incidence of reported side effects. This led to restriction in its dosage and maximum duration of use. In the UK, treatment was initiated only in a hospital, although this was not designed to exclude its use in prehospital care and mountain rescue settings.[8] Dosing guidelines were published at that time.[24]
Concerns over the high incidence of reported side effects with ketorolac trometamol led to its withdrawal (apart from the ophthalmic formulation) in several countries, while in others its permitted dosage and maximum duration of treatment have been reduced. From 1990 to 1993, 97 reactions with a fatal outcome were reported worldwide.[25]
The eye-drop formulation was approved by the FDA in 1992.[26]
An intranasal formulation (Sprix) was approved by the FDA in 2010[27] for short-term management of moderate to moderately severe pain requiring analgesia at the opioid level.
Ketorolac has also been used in collegiate and professional sports, and is reported to be routinely used in the National Football League and National Hockey League. Competitive sports athletes, particularly in contact sports, are often required to play through injuries.[28] In the late 1990s opioids and their associated pharmaceutical companies came under fire.[29] Then sporting leagues began to push back against team physicians giving them to players attempting to play through injuries as it was clear that numbing the pain during practice/competition only furthered injuries.[30] Resultantly teams moved to using ketorolac as the drug is certainly powerful enough to numb players pain, but ketorolac is not a commonly abused drug with a bad reputation. Furthermore, ketorolac is a NSAID which are generally considered safe by those without a background in pharmacology as they are associated with more mild drugs such as aspirin/ibuprofen.[31] Only recently has this issue been addressed, with researchers speaking out and making recommendations[32] and a lawsuit against the National Football League in 2017.[33]
References
- "Ketorolac Tromethamine Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 13 April 2019.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 1144, 1302–1303. ISBN 9780857113382.
- "DailyMed - ketorolac tromethamine tablet, film coated". dailymed.nlm.nih.gov. Retrieved 14 April 2019.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 521. ISBN 9783527607495.
- "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Retrieved 3 March 2019.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Ketorolac Tromethamine - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Mallinson, Tom (2017). "A review of ketorolac as a prehospital analgesic". Journal of Paramedic Practice. 9 (12): 522–526. doi:10.12968/jpar.2017.9.12.522. Retrieved 2 June 2018.
- Vallerand AH (2017). Davis's Drug Guide for Nurses. Philadelphia: F.A. Davis Company. p. 730. ISBN 9780803657052.
- Physician's Desk Reference 2017. Montvale, New Jersey: PDR, LLC. 2017. pp. S–474–5. ISBN 9781563638381.
- "Ketorolac-tromethamine". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- Henry 2016, p. 291.
- Henry 2016, p. 280.
- Martin LD, Jimenez N, Lynn AM (2017). "A review of perioperative anesthesia and analgesia for infants: updates and trends to watch". F1000Research. 6: 120. doi:10.12688/f1000research.10272.1. PMC 5302152. PMID 28232869.
- Schwier N, Tran N (March 2016). "Non-Steroidal Anti-Inflammatory Drugs and Aspirin Therapy for the Treatment of Acute and Recurrent Idiopathic Pericarditis". Pharmaceuticals. 9 (2): 17. doi:10.3390/ph9020017. PMC 4932535. PMID 27023565.
- Gonzalez-Salinas R, Guarnieri A, Guirao Navarro MC, Saenz-de-Viteri M (2016). "Patient considerations in cataract surgery - the role of combined therapy using phenylephrine and ketorolac". Patient Preference and Adherence. 10: 1795–1801. doi:10.2147/PPA.S90468. PMC 5029911. PMID 27695298.
- Karch A (2017). Focus on nursing pharmacology. Philadelphia: Wolters Kluwer. p. 272. ISBN 9781496318213.
- Lim BX, Lim CH, Lim DK, Evans JR, Bunce C, Wormald R (November 2016). "Prophylactic non-steroidal anti-inflammatory drugs for the prevention of macular oedema after cataract surgery". The Cochrane Database of Systematic Reviews. 11: CD006683. doi:10.1002/14651858.CD006683.pub3. PMC 6464900. PMID 27801522.
- Sivaprasad S, Bunce C, Crosby-Nwaobi R (February 2012). "Non-steroidal anti-inflammatory agents for treating cystoid macular oedema following cataract surgery". The Cochrane Database of Systematic Reviews (2): CD004239. doi:10.1002/14651858.CD004239.pub3. PMID 22336801.
- Wakai A, Lawrenson JG, Lawrenson AL, Wang Y, Brown MD, Quirke M, et al. (May 2017). "Topical non-steroidal anti-inflammatory drugs for analgesia in traumatic corneal abrasions". The Cochrane Database of Systematic Reviews. 5: CD009781. doi:10.1002/14651858.CD009781.pub2. PMC 6481688. PMID 28516471.
- Henry 2016, p. 279.
- PubChem. "Ketorolac". pubchem.ncbi.nlm.nih.gov. Retrieved 2020-04-18.
- Lee IO, Seo Y (March 2008). "The effects of intrathecal cyclooxygenase-1, cyclooxygenase-2, or nonselective inhibitors on pain behavior and spinal Fos-like immunoreactivity". Anesthesia and Analgesia. 106 (3): 972–7, table of contents. doi:10.1213/ane.0b013e318163f602. PMID 18292448.
- MHRA Drug Safety Update October 2007, Volume 1, Issue 3, pp 3-4.
- Committee on the Safety of Medicines, Medicines Control Agency: Ketorolac: new restrictions on dose and duration of treatment. Current Problems in Pharmacovigilance: June 1993; Volume 19 (pages 5-8).
- "Ketorolac ophthalmic medical facts from". Drugs.com. Retrieved 2013-10-06.
- "Sprix Information from". Drugs.com. Retrieved 2013-10-06.
- "Masking the pain: The trouble with Toradol in college sports". FOX31 Denver. 2015-05-14. Retrieved 2020-04-18.
- Affairs (ASPA), Assistant Secretary of Public (2017-12-04). "What is the U.S. Opioid Epidemic?". HHS.gov. Retrieved 2020-04-18.
- Klemko, Robert. "Toradol Lawsuit: NFL Can't Outrun Legacy of Abuse". Sports Illustrated. Retrieved 2020-04-18.
- "Hopkins NSAID" (PDF). Johns Hopkins. 2020.
- Matava, Matthew; Brater, D. Craig; Gritter, Nancy; Heyer, Robert; Rollins, Douglas; Schlegel, Theodore; Toto, Robert; Yates, Anthony (September 2012). "Recommendations of the National Football League Physician Society Task Force on the Use of Toradol® Ketorolac in the National Football League". Sports Health. 4 (5): 377–383. doi:10.1177/1941738112457154. ISSN 1941-7381. PMC 3435943. PMID 23016110.
- Maese, Rick (2017-03-09). "NFL abuse of painkillers and other drugs described in court filings". Washington Post. ISSN 0190-8286. Retrieved 2020-04-18.
Bibliography
- AHFS drug information. Bethesda, MD: American Society of Health-System Pharmacists. 2011. ISBN 9781585282609.
- Hamilton R (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 9. ISBN 9781284057560.
- Handley DA, Cervoni P, McCray JE, McCullough JR (February 1998). "Preclinical enantioselective pharmacology of (R)- and (S)- ketorolac". Journal of Clinical Pharmacology. 38 (2S): 25S–35S. doi:10.1002/j.1552-4604.1998.tb04414.x. PMID 9549656.
- Henry N (2016). RN pharmacology for nursing : review module. Overland Park, KS: Assessment Technologies Institute. ISBN 9781565335738.
- Kizior R (2017). Saunders nursing drug handbook 2017. St. Louis, MO: Elsevier. ISBN 9780323442916.
External links
- "Ketorolac". Drug Information Portal. U.S. National Library of Medicine.