Erlotinib
Erlotinib, sold under the brand name Tarceva among others, is a medication used to treat non-small cell lung cancer (NSCLC) and pancreatic cancer.[2] Specifically it is used for NSCLC with mutations in the epidermal growth factor receptor (EGFR) — either an exon 19 deletion (del19) or exon 21 (L858R) substitution mutation — which has spread to other parts of the body.[2] It is taken by mouth.[2]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tarceva |
| Other names | Erlotinib hydrochloride |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605008 |
| License data | |
| Pregnancy category | |
| Routes of administration | By mouth tablets |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 59% |
| Protein binding | 95% |
| Metabolism | Liver (mainly CYP3A4, less CYP1A2) |
| Elimination half-life | 36.2 hrs (median) |
| Excretion | >98% as metabolites, of which >90% via feces, 9% via urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.216.020 |
| Chemical and physical data | |
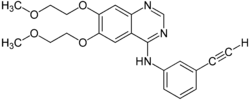
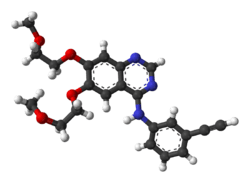
| Formula | C22H23N3O4 |
| Molar mass | 393.443 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Common side effects include rash, diarrhea, muscle pain, joint pain, and cough.[2][3] Serious side effects may include lung problems, kidney problems, liver failure, gastrointestinal perforation, stroke, and corneal ulceration.[2] Use in pregnancy may harm the baby.[2] It is a receptor tyrosine kinase inhibitor, which acts on the epidermal growth factor receptor (EGFR).[2]
Erlotinib was approved for medical use in the United States in 2004.[4][2][3] It is on the World Health Organization's List of Essential Medicines, which lists the safest and most effective medicines needed in a health system.[5] In the United States, as of 2019, it costs about US$8,832 per month.[6] In the United Kingdom this amount costs the NHS about £1,631.53 per month.[7]
Medical uses
Lung cancer
Erlotinib in unresectable non-small cell lung cancer when added to chemotherapy improves overall survival by 19%, and improved progression-free survival (PFS) by 29%, when compared to chemotherapy alone.[8][9] The U.S. Food and Drug Administration (FDA) approved erlotinib for the treatment of locally advanced or metastatic non-small cell lung cancer that has failed at least one prior chemotherapy regimen.[10]
In lung cancer, erlotinib has been shown to be effective in patients with or without EGFR mutations, but appears to be more effective in patients with EGFR mutations.[11][12] Overall survival, progression-free survival and one-year survival are similar to standard second-line therapy (docetaxel or pemetrexed). Overall response rate is about 50% better than standard second-line chemotherapy.[12] Patients who are non-smokers, and light former smokers, with adenocarcinoma or subtypes like BAC are more likely to have EGFR mutations, but mutations can occur in all types of patients. A test for the EGFR mutation has been developed by Genzyme.[13]
Pancreatic cancer
In November 2005, the FDA approved erlotinib in combination with gemcitabine for treatment of locally advanced, unresectable, or metastatic pancreatic cancer.[14]
Resistance to treatment
As with other ATP competitive small molecule tyrosine kinase inhibitors, such as imatinib in CML, patients rapidly develop resistance. In the case of erlotinib this typically occurs 8–12 months from the start of treatment. Over 50% of resistance is caused by a mutation in the ATP binding pocket of the EGFR kinase domain involving substitution of a small polar threonine residue with a large nonpolar methionine residue (T790M).[15]
Approximately 20% of drug resistance is caused by amplification of the hepatocyte growth factor receptor, which drives ERBB3 dependent activation of PI3K.[16][17]
Side effects
Common
- Rash occurs in the majority of patients. This resembles acne and primarily involves the face and neck. It is self-limited and resolves in the majority of cases, even with continued use. Some clinical studies have indicated a correlation between the severity of the skin reactions and increased survival though this has not been quantitatively assessed.[18] The Journal of Clinical Oncology reported in 2004 that "cutaneous [skin] rash seems to be a surrogate marker of clinical benefit, but this finding should be confirmed in ongoing and future studies."[19] The newsletter Lung Cancer Frontiers reported in its October 2003 issue, "Patients with moderate to severe cutaneous reactions [rashes] have a far better survival, than those with only mild reactions and much better than those with no cutaneous manifestations of drug effects."[20]
- Diarrhea
- Loss of appetite
- Fatigue
- Partial hair loss (by strands, not typically in clumps)
Rare
- interstitial pneumonitis, which is characterized by cough and increased dyspnea. This may be severe and must be considered among those patients whose breathing acutely worsens.
- ingrown hairs, such as eyelashes
- gastrointestinal tract toxicity
- serious or fatal gastrointestinal tract perforations
- skin toxicity
- bullous, blistering, and exfoliative skin conditions (some fatal)
- Stevens–Johnson syndrome/toxic epidermal necrolysis [21]
- ocular disorders
- corneal lesions
- Pulmonary toxicity
- interstitial pneumonitis
- bronchiolitis obliterans with organizing pneumonia (BOOP)
- pulmonary fibrosis
- fatal asymmetric interstitial lung disease[22]
Interactions
Erlotinib is not a substrate for either of hepatic OATPs (OATP1B1 or OATP1B3).[23] Also, erlotinib is not an inhibitor of OATP-1B1 or OATP-1B3 transporter.[24]
Erlotinib is mainly metabolized by the liver enzyme CYP3A4. Compounds which induce this enzyme (i.e. stimulate its production), such as St John's wort, can lower erlotinib concentrations, while inhibitors can increase concentrations.[25]
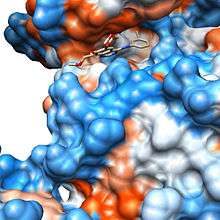
Mechanism
Erlotinib is an epidermal growth factor receptor inhibitor (EGFR inhibitor). The drug follows Iressa (gefitinib), which was the first drug of this type. Erlotinib specifically targets the epidermal growth factor receptor (EGFR) tyrosine kinase, which is highly expressed and occasionally mutated in various forms of cancer. It binds in a reversible fashion to the adenosine triphosphate (ATP) binding site of the receptor.[26] For the signal to be transmitted, two EGFR molecules need to come together to form a homodimer. These then use the molecule of ATP to trans-phosphorylate each other on tyrosine residues, which generates phosphotyrosine residues, recruiting the phosphotyrosine-binding proteins to EGFR to assemble protein complexes that transduce signal cascades to the nucleus or activate other cellular biochemical processes. When erlotinib binds to EGFR, formation of phosphotyrosine residues in EGFR is not possible and the signal cascades are not initiated.
Society and culture
It is marketed in the United States by Genentech[3] and OSI Pharmaceuticals[27] and elsewhere by Roche.[28]
The drug's U.S. patent will expire in 2020.[29] In May 2012, the US District Court of Delaware passed an order in favor of OSI Pharmaceutical LLC against Mylan Pharmaceuticals upholding the validity of the patent for Erlotinib. In India, generic pharmaceutical firm Cipla is battling with Roche against the Indian patent for this drug.[30][31]
Price
In the United States, as of 2019, it costs about US$8,832 per month.[6] In the United Kingdom this amount costs the NHS about £1,631.53 per month.[7]
References
- "Erlotinib (Tarceva) Use During Pregnancy". Drugs.com. 1 November 2019. Retrieved 23 December 2019.
- "Erlotinib Monograph for Professionals". Drugs.com. Retrieved 12 November 2019.
- "Tarceva- erlotinib hydrochloride tablet". DailyMed. 12 December 2018. Retrieved 23 December 2019.
- "Drug Approval Package: Tarceva (Erlotinib) NDA #021743". U.S. Food and Drug Administration (FDA). 28 March 2005. Retrieved 23 December 2019.
- Organization, World Health (2019). "World Health Organization model list of essential medicines: 21st list 2019". hdl:10665/325771. Cite journal requires
|journal=(help) - "Tarceva Prices, Coupons & Patient Assistance Programs". Drugs.com.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 950. ISBN 9780857113382.
- 2009 - SATURN: A double-blind, randomized, phase III study of maintenance erlotinib versus placebo following nonprogression with first-line platinum-based chemotherapy in patients with advanced NSCLC.
- April 2010 - Tarceva Indication Announcement Letter
- Cohen, Martin H.; Johnson, John R.; Chen, Yeh-Fong; Sridhara, Rajeshwari; Pazdur, Richard (August 2005). "FDA drug approval summary: erlotinib (Tarceva) tablets". The Oncologist. 10 (7): 461–466. doi:10.1634/theoncologist.10-7-461. ISSN 1083-7159. PMID 16079312.
- Kobayashi K, Hagiwara K (2013). "Epidermal growth factor receptor (EGFR) mutation and personalized therapy in advanced nonsmall cell lung cancer (NSCLC)". Targeted Oncology. 8 (1): 27–33. doi:10.1007/s11523-013-0258-9. PMC 3591525. PMID 23361373.
- Qi WX, Shen Z, Lin F, et al. (2012). "Comparison of the efficacy and safety of EFGR tyrosine kinase inhibitor monotherapy with standard second-line chemotherapy in previously treated advanced non-small-cell lung cancer: A systematic review and meta-analysis". Asian Pacific Journal of Cancer Prevention. 13 (10): 5177–5182. doi:10.7314/APJCP.2012.13.10.5177. PMID 23244131.
- "Roche obtains license for EGFR lung cancer assays and will develop Tarceva companion diagnostic test". www.roche.com. Retrieved 10 January 2020.
- Takimoto CH, Calvo E (15 April 2009), Principles of Oncologic Pharmacotherapy
- Balak MN, Gong Y, Riely GJ, et al. (2006). "Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors". Clin Cancer Res. 12 (1): 6494–501. doi:10.1158/1078-0432.CCR-06-1570. PMID 17085664.
- Engelman JA, Zejnullahu K, Mitsudomi T, et al. (2007). "MET Amplification Leads to Gefitinib Resistance in Lung Cancer by Activating ERBB3 Signaling". Science. 316 (5827): 1039–43. Bibcode:2007Sci...316.1039E. doi:10.1126/science.1141478. PMID 17463250.
- EBean J, Brennan C, Shih JY, et al. (2007). "MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib". PNAS. 104 (52): 20932–7. Bibcode:2007PNAS..10420932B. doi:10.1073/pnas.0710370104. PMC 2409244. PMID 18093943.
- Dudek AZ, Kmak KL, Koopmeiners J, et al. (2006). "Skin rash and bronchoalveolar histology correlates with clinical benefit in patients treated with gefitinib as a therapy for previously treated advanced or metastatic non-small cell lung cancer". Lung Cancer. 51 (1): 89–96. doi:10.1016/j.lungcan.2005.09.002. PMID 16290256.
- Pérez-Soler R, Chachoua A, Hammond LA, et al. (15 August 2004). "Determinants of tumor response and survival with erlotinib in patients with non--small-cell lung cancer". Journal of Clinical Oncology. 22 (16): 3238–3247. doi:10.1200/JCO.2004.11.057. ISSN 0732-183X. PMID 15310767.
- Thomas L. Petty, M.D. (2003). "Determinants of Tumor Response and Survival With Erlotinib in Patients With Non—Small-Cell Lung Cancer". Journal of Clinical Oncology. 1 (17): 3–4.
- Li X, Kamenecka TM, Cameron MD (2010). "Cytochrome P450-mediated bioactivation of the epidermal growth factor receptor inhibitor erlotinib to a reactive electrophile". Drug Metabolism and Disposition: The Biological Fate of Chemicals. 38 (7): 1238–45. doi:10.1124/dmd.109.030361. ISSN 0090-9556. PMC 3202369. PMID 20382753.
- Ren S, Li Y, Li W, et al. (2012). "Fatal asymmetric interstitial lung disease after erlotinib for lung cancer". Respiration. 84 (5): 431–5. doi:10.1159/000339508. PMID 22889962.
- Khurana V, Minocha M, Pal D, et al. (March 2014). "Role of OATP-1B1 and/or OATP-1B3 in hepatic disposition of tyrosine kinase inhibitors". Drug Metabol Drug Interact. 29 (3): 179–90. doi:10.1515/dmdi-2013-0062. PMC 4407685. PMID 24643910.
- Khurana V, Minocha M, Pal D, et al. (May 2014). "Inhibition of OATP-1B1 and OATP-1B3 by tyrosine kinase inhibitors". Drug Metabol Drug Interact. 29 (4): 249–59. doi:10.1515/dmdi-2014-0014. PMC 4407688. PMID 24807167.
- Haberfeld, H, ed. (2010). Austria-Codex (in German) (2010/2011 ed.). Vienna: Österreichischer Apothekerverlag.
- Raymond E, Faivre S, Armand JP (2000). "Epidermal growth factor receptor tyrosine kinase as a target for anticancer therapy". Drugs. 60 Suppl 1: 15–23, discussion 41–2. doi:10.2165/00003495-200060001-00002. PMID 11129168.
- Adis International Ltd (2003). "Erlotinib: CP 358774, NSC 718781, OSI 774, R 1415". Drugs in R&D. 4 (4): 243–248. doi:10.2165/00126839-200304040-00006. ISSN 1174-5886. PMID 12848590.
- "FDA Approves Roche Test as CDx for Tarceva for Treating Certain NSCLC Patients". GenomeWeb. Retrieved 10 January 2020.
- http://drugpatentwatch.com/p/ingredient/erlotinib, "Details for Generic Name: erlotinib", DrugPatentWatch.com
- "Roche and India's Glenmark reach truce over generic Tarceva". GaBI Online. 22 January 2016. Archived from the original on 24 December 2019. Retrieved 23 December 2019.
- "Cancer drug: Supreme Court allows Cipla to withdraw appeal against Roche". The Economic Times. 16 June 2017. Archived from the original on 24 December 2019. Retrieved 23 December 2019.
External links
- "Erlotinib". Drug Information Portal. U.S. National Library of Medicine.
- "Erlotinib". National Cancer Institute.