Hygiene
Hygiene is a series of practices performed to preserve health. According to the World Health Organization (WHO), "Hygiene refers to conditions and practices that help to maintain health and prevent the spread of diseases."[2] Personal hygiene refers to maintaining the body's cleanliness.
Many people equate hygiene with 'cleanliness,' but hygiene is a broad term. It includes such personal habit choices as how frequently to take a shower or bath, wash hands, trim fingernails, and wash clothes. It also includes attention to keeping surfaces in the home and workplace, including bathroom facilities, clean and pathogen-free.
Some regular hygiene practices may be considered good habits by the society, while the neglect of hygiene can be considered disgusting, disrespectful, or threatening.
Etymology
First attested in English in 1676, the word hygiene comes from the French hygiène, the latinisation of the Greek ὑγιεινή (τέχνη) hygieinē technē, meaning "(art) of health", from ὑγιεινός hygieinos, "good for the health, healthy",[3] in turn from ὑγιής (hygiēs), "healthful, sound, salutary, wholesome".[4] In ancient Greek religion, Hygeia (Ὑγίεια) was the personification of health, cleanliness, and hygiene.[5]
Background

.jpg)
Hygiene is a concept related to cleanliness, health and medicine. It is as well related to personal and professional care practices. In medicine and everyday life settings, hygiene practices are employed as preventive measures to reduce the incidence and spreading of disease.
Hygiene practices vary, and what is considered acceptable in one culture might not be acceptable in another.
In the manufacturing of food, pharmaceutical, cosmetic and other products, good hygiene is a critical component of quality assurance.
The terms cleanliness and hygiene are often used interchangeably, which can cause confusion. In general, hygiene refers to practices that prevent spread of disease-causing organisms. Cleaning processes (e.g., handwashing) remove infectious microbes as well as dirt and soil, and are thus often the means to achieve hygiene.
Other uses of the term appear in phrases including body hygiene, personal hygiene, sleep hygiene, mental hygiene, dental hygiene, and occupational hygiene, used in connection with public health. Hygiene is also the name of a branch of science that deals with the promotion and preservation of health.
Medical hygiene
Medical hygiene pertains to the hygiene practices related to the administration of medicine and medical care that prevents or minimizes the spread of disease.
Medical hygiene practices include:
- Isolation or quarantine of infectious persons or materials to prevent spread of infection.
- Sterilization of instruments used in surgical procedures.
- Use of protective clothing and barriers, such as masks, gowns, caps, eyewear and gloves.
- Proper bandaging and dressing of injuries.
- Safe disposal of medical waste.
- Disinfection of reusables (i.e., linen, pads, uniforms).
- Scrubbing up, hand-washing, especially in an operating room, but in more general health-care settings as well, where diseases can be transmitted.
- Ethanol-based sanitizers.
Most of these practices were developed in the 19th century and were well established by the mid-20th century. Some procedures (such as disposal of medical waste) were refined in response to late-20th century disease outbreaks, notably AIDS and Ebola.
Home and everyday hygiene
Home hygiene pertains to the hygiene practices that prevent or minimize the spread of disease at home and other everyday settings such as social settings, public transport, the workplace, public places, etc.
Hygiene in a variety of settings plays an important role in preventing the spread of infectious diseases.[6] It includes procedures used in a variety of domestic situations such as hand hygiene, respiratory hygiene, food and water hygiene, general home hygiene (hygiene of environmental sites and surfaces), care of domestic animals, and home health care (the care of those who are at greater risk of infection).
At present, these components of hygiene tend to be regarded as separate issues, although based on the same underlying microbiological principles. Preventing the spread of diseases means breaking the chain of infection transmission. Simply put, if the chain of infection is broken, infection cannot spread. In response to the need for effective codes of hygiene in home and everyday life settings the International Scientific Forum on Home Hygiene has developed a risk-based approach based on Hazard Analysis Critical Control Point (HACCP), also referred to as "targeted hygiene." Targeted hygiene is based on identifying the routes of pathogen spread in the home and introducing hygiene practices at critical times to break the chain of infection.
The main sources of infection in the home[7] are people (who are carriers or are infected), foods (particularly raw foods) and water, and domestic animals (in the U.S. more than 50% of homes have one or more pets[8]). Sites that accumulate stagnant water—such as sinks, toilets, waste pipes, cleaning tools, face cloths, etc. readily support microbial growth and can become secondary reservoirs of infection, though species are mostly those that threaten "at risk" groups. Pathogens (potentially infectious bacteria, viruses etc.—colloquially called "germs") are constantly shed from these sources via mucous membranes, feces, vomit, skin scales, etc. Thus, when circumstances combine, people are exposed, either directly or via food or water, and can develop an infection.
The main "highways" for the spread of pathogens in the home are the hands, hand and food contact surfaces, and cleaning cloths and utensils. Pathogens can also be spread via clothing and household linens, such as towels. Utilities such as toilets and wash basins, for example, were invented for dealing safely with human waste but still have risks associated with them. Safe disposal of human waste is a fundamental need; poor sanitation is a primary cause of diarrhea disease in low income communities. Respiratory viruses and fungal spores are spread via the air.
Good home hygiene means engaging in hygiene practices at critical points to break the chain of infection.[7] Because the "infectious dose" for some pathogens can be very small (10-100 viable units or even less for some viruses), and infection can result from direct transfer of pathogens from surfaces via hands or food to the mouth, nasal mucous or the eye, 'hygienic cleaning' procedures should be sufficient to eliminate pathogens from critical surfaces.
Hygienic cleaning can be done through:
- Mechanical removal (i.e., cleaning) using a soap or detergent. To be effective as a hygiene measure, this process must be followed by thorough rinsing under running water to remove pathogens from the surface.
- Using a process or product that inactivates the pathogens in situ. Pathogen kill is achieved using a "micro-biocidal" product, i.e., a disinfectant or antibacterial product; waterless hand sanitizer; or by application of heat.
- In some cases combined pathogen removal with kill is used, e.g., laundering of clothing and household linens such as towels and bed linen.
Hand washing
.jpg)
Hand hygiene is defined as hand washing or washing hands and nails with soap and water or using a water less hand sanitizer. Hand hygiene is central to preventing the spread of infectious diseases in home and everyday life settings.[9]
In situations where hand washing with soap is not an option (e.g., when in a public place with no access to wash facilities), a water less hand sanitizer such as an alcohol hand gel can be used. They can be used in addition to hand washing to minimize risks when caring for "at-risk" groups. To be effective, alcohol hand gels should contain not less than 60%v/v alcohol.
The WHO (World Health Organization) recommends hand washing with ash if soap is not available in critical situations,[10] schools without access to soap[11] and other difficult situations like post-emergencies where use of (clean) sand is recommended, too.[12] Use of ash is common in rural areas of developing countries and has in experiments been shown at least as effective as soap for removing pathogens.[13]
Respiratory hygiene
Correct respiratory and hand hygiene when coughing and sneezing reduces the spread of pathogens particularly during the cold and flu season.[6]
- Carry tissues and use them to catch coughs and sneezes, or sneeze into your elbow
- Dispose of tissues as soon as possible
Food hygiene at home
Food hygiene is concerned with the hygiene practices that prevent food poisoning. The five key principles of food hygiene, according to WHO, are:[14]
- Prevent contaminating food with mixing chemicals, spreading from people, and animals.
- Separate raw and cooked foods to prevent contaminating the cooked foods.
- Cook foods for the appropriate length of time and at the appropriate temperature to kill pathogens.
- Store food at the proper temperature.
- Use safe water and raw materials.
Hygiene in the kitchen.
Routine cleaning of (hand, food, drinking water) sites and surfaces (such as toilet seats and flush handles, door and tap handles, work surfaces, bath and basin surfaces) in the kitchen, bathroom and toilet reduces the risk of spread of pathogens.[15] The infection risk from flush toilets is not high, provided they are properly maintained, although some splashing and aerosol formation can occur during flushing, particularly when someone has diarrhea. In case of using public toilets you can always use a Toilet Seat Sanitizer to spray on the seat before sitting on it. A toilet seat sanitizer helps to kill bacteria just as any other sanitizer which helps to protect from UTI. Pathogens can survive in the scum or scale left behind on baths, showers and wash basins after washing and bathing.
Water left stagnant in the pipes of showers can be contaminated with pathogens that become airborne when the shower is turned on. If a shower has not been used for some time, it should be left to run at a hot temperature for a few minutes before use.
Thorough cleaning is important in preventing the spread of fungal infections.[16] Molds can live on wall and floor tiles and on shower curtains. Mold can be responsible for infections, cause allergic responses, deteriorate/damage surfaces and cause unpleasant odors. Primary sites of fungal growth are inanimate surfaces, including carpets and soft furnishings.[17] Air-borne fungi are usually associated with damp conditions, poor ventilation or closed air systems.
Laundry hygiene
Laundry hygiene involves practices that prevent disease and its spread via soiled clothing and household linens such as towels.[18] Items most likely to be contaminated with pathogens are those that come into direct contact with the body, e.g., underwear, personal towels, facecloths, nappies. Cloths or other fabric items used during food preparation, or for cleaning the toilet or cleaning up material such as feces or vomit are a particular risk.[19]
Microbiological and epidemiological data indicates that clothing and household linens etc. are a risk factor for infection transmission in home and everyday life settings as well as institutional settings. The lack of quantitative data linking contaminated clothing to infection in the domestic setting makes it difficult to assess the extent of this risk.[18][19][20] It also indicates that risks from clothing and household linens are somewhat less than those associated with hands, hand contact and food contact surfaces, and cleaning cloths, but even so these risks needs to be managed through effective laundering practices. In the home, this routine should be carried out as part of a multibarrier approach to hygiene which includes hand, food, respiratory and other hygiene practices.[18][19][20]
Infectious diseases risks from contaminated clothing etc. can increase significantly under certain conditions, e.g., in healthcare situations in hospitals, care homes and the domestic setting where someone has diarrhoea, vomiting, or a skin or wound infection. It increases in circumstances where someone has reduced immunity to infection.
Hygiene measures, including laundry hygiene, are an important part of reducing spread of antibiotic resistant strains.[21][22] In the community, otherwise healthy people can become persistent skin carriers of MRSA, or faecal carriers of enterobacteria strains which can carry multi-antibiotic resistance factors (e.g. NDM-1 or ESBL-producing strains). The risks are not apparent until, for example, they are admitted to hospital, when they can become "self infected" with their own resistant organisms following a surgical procedure. As persistent nasal, skin or bowel carriage in the healthy population spreads "silently" across the world, the risks from resistant strains in both hospitals and the community increases.[22] In particular the data indicates that clothing and household linens are a risk factor for spread of S. aureus (including MRSA and PVL-producing MRSA strains), and that effectiveness of laundry processes may be an important factor in defining the rate of community spread of these strains.[18][23] Experience in the United States suggests that these strains are transmissible within families and in community settings such as prisons, schools and sport teams. Skin-to-skin contact (including unabraded skin) and indirect contact with contaminated objects such as towels, sheets and sports equipment seem to represent the mode of transmission.[18]
During laundering, temperature and detergent work to reduce microbial contamination levels on fabrics. Soil and microbes from fabrics are severed and suspended in the wash water. These are then "washed away" during the rinse and spin cycles. In addition to physical removal, micro-organisms can be killed by thermal inactivation which increases as the temperature is increased. Chemical inactivation of microbes by the surfactants and activated oxygen-based bleach used in detergents contributes to the hygiene effectiveness of laundering. Adding hypochlorite bleach in the washing process achieves inactivation of microbes. A number of other factors can contribute including drying and ironing.
Drying laundry on a line in direct sunlight is known to reduce pathogens.
Laundry detergents contain a mix of ingredients including surfactants, builders, optical brighteners, etc. Cleaning action arises primarily from the action of the surfactants and other ingredients, which are designed to maximise release and suspension of dirt and microbes into the wash liquid, together with enzymes and/or an activated oxygen-based bleach which digest and remove stains. Although activated oxygen bleach is included in many powder detergents to digest and remove stains, it produces some chemical inactivation of bacteria, fungi and viruses. As a rule of thumb, powders and tablets normally contain an activated oxygen bleach, but liquids and all products (liquid or powder) used for "coloureds" do not. Surfactants also exert some chemical inactivation action against certain species although the extent of their action is not known.
In 2013 the International Scientific Forum on Home Hygiene (IFH) reviewed some 30 studies of the hygiene effectiveness of laundering at temperatures ranging from room temperature to 70 °C, under varying conditions.[24] A key finding was the lack of standardisation and control within studies, and the variability in test conditions between studies such as wash cycle time, number of rinses, etc. The consequent variability in the data (i.e., the reduction in contamination on fabrics) obtained, in turn makes it extremely difficult to propose guidelines for laundering with any confidence, based on currently available data. As a result, there is significant variability in the recommendations for hygienic laundering of clothing etc. given by different agencies.[25][26][27][28][29][30]
Of concern is recent data suggesting that, in reality, modern domestic washing machines do not reach the temperature specified on the machine controls.[31][32]
Medical hygiene at home
Medical hygiene pertains to the hygiene practices that prevents or minimizes disease and the spreading of disease in relation to administering medical care to those who are infected or who are more "at risk" of infection in the home. Across the world, governments are increasingly under pressure to fund the level of healthcare that people expect. Care of increasing numbers of patients in the community, including at home is one answer, but can be fatally undermined by inadequate infection control in the home. Increasingly, all of these "at-risk" groups are cared for at home by a carer who may be a household member who thus requires a good knowledge of hygiene. People with reduced immunity to infection, who are looked after at home, make up an increasing proportion of the population (currently up to 20%).[6] The largest proportion are the elderly who have co-morbidities, which reduce their immunity to infection. It also includes the very young, patients discharged from hospital, taking immuno-suppressive drugs or using invasive systems, etc. For patients discharged from hospital, or being treated at home special "medical hygiene" (see above) procedures may need to be performed for them e.g. catheter or dressing replacement, which puts them at higher risk of infection.
Antiseptics may be applied to cuts, wounds abrasions of the skin to prevent the entry of harmful bacteria that can cause sepsis. Day-to-day hygiene practices, other than special medical hygiene procedures[33] are no different for those at increased risk of infection than for other family members. The difference is that, if hygiene practices are not correctly carried out, the risk of infection is much greater.
Disinfectants and antibacterials in home hygiene
Chemical disinfectants are products that kill pathogens. If the product is a disinfectant, the label on the product should say "disinfectant" or "kills" pathogens. Some commercial products, e.g. bleaches, even though they are technically disinfectants, say that they "kill pathogens" but are not actually labelled as "disinfectants". Not all disinfectants kill all types of pathogens. All disinfectants kill bacteria (called bactericidal). Some also kill fungi (fungicidal), bacterial spores (sporicidal) or viruses (virucidal).
An antibacterial product is a product that acts against bacteria in some unspecified way. Some products labelled "antibacterial" kill bacteria while others may contain a concentration of active ingredient that only prevent them multiplying. It is, therefore, important to check whether the product label states that it "kills" bacteria." An antibacterial is not necessarily anti-fungal or anti-viral unless this is stated on the label.
The term sanitizer has been used to define substances that both clean and disinfect. More recently this term has been applied to alcohol-based products that disinfect the hands (alcohol hand sanitizers). Alcohol hand sanitizers however are not considered to be effective on soiled hands.
The term biocide is a broad term for a substance that kills, inactivates or otherwise controls living organisms. It includes antiseptics and disinfectants, which combat micro-organisms, and pesticides.
Home hygiene in developing countries
In developing countries, universal access to water and sanitation has been seen as the essential step in reducing the preventable infectious diseases burden, but it is now clear that this is best achieved by programs that integrate hygiene promotion with improvements in water quality and availability, and sanitation. This approach has been integrated into the Sustainable Development Goal Number 6 whose second target states: "By 2030, achieve access to adequate and equitable sanitation and hygiene for all and end open defecation, paying special attention to the needs of women and girls and those in vulnerable situations".[34] Due to their close linkages, water, sanitation, hygiene are together abbreviated and funded under the term WASH in development cooperation.
About 2 million people die every year due to diarrheal diseases, most of them are children less than 5 years of age.[35] The most affected are the populations in developing countries, living in extreme conditions of poverty, normally peri-urban dwellers or rural inhabitants. Providing access to sufficient quantities of safe water, the provision of facilities for a sanitary disposal of excreta, and introducing sound hygiene behaviors are of capital importance to reduce the burden of disease caused by these risk factors.
Research shows that, if widely practiced, hand washing with soap could reduce diarrhea by almost fifty percent[36][37][38] and respiratory infections by nearly twenty-five percent[39][40] Hand washing with soap also reduces the incidence of skin diseases,[41][42] eye infections like trachoma and intestinal worms, especially ascariasis and trichuriasis.[43]
Other hygiene practices, such as safe disposal of waste, surface hygiene, and care of domestic animals, are important in low income communities to break the chain of infection transmission.[44]
Cleaning of toilets and hand wash facilities is important to prevent odors and make them socially acceptable. Social acceptance is an important part of encouraging people to use toilets and wash their hands, in situations where open defecation is still seen as a possible alternative, e.g. in rural areas of some developing countries.
Household water treatment and safe storage
Household water treatment and safe storage ensure drinking water is safe for consumption. These interventions are part of the approach of self-supply of water for households. Drinking water quality remains a significant problem in developing[45] and in developed countries;[46] even in the European region it is estimated that 120 million people do not have access to safe drinking water. Point-of-use water quality interventions can reduce diarrheal disease in communities where water quality is poor or in emergency situations where there is a breakdown in water supply.[45][46][47][48] Since water can become contaminated during storage at home (e.g. by contact with contaminated hands or using dirty storage vessels), safe storage of water in the home is important.
Methods for treatment of drinking water,[15][48] include:
- Chemical disinfection using chlorine or iodine
- Boiling
- Filtration using ceramic filters
- Solar disinfection – Solar disinfection is an effective method, especially when no chemical disinfectants are available.[49]
- UV irradiation – community or household UV systems may be batch or flow-though. The lamps can be suspended above the water channel or submerged in the water flow.
- Combined flocculation/disinfection systems – available as sachets of powder that act by coagulating and flocculating sediments in water followed by release of chlorine.
- Multibarrier methods – Some systems use two or more of the above treatments in combination or in succession to optimize efficacy.
Personal hygiene
Regular activities

Personal hygiene involves those practices performed by an individual to care for one's bodily health and wellbeing through cleanliness. Motivations for personal hygiene practice include reduction of personal illness, healing from personal illness, optimal health and sense of wellbeing, social acceptance and prevention of spread of illness to others. What is considered proper personal hygiene can be cultural-specific and may change over time.
Practices that are generally considered proper hygiene include showering or bathing regularly, washing hands regularly and especially before handling food, washing scalp hair, keeping hair short or removing hair, wearing clean clothing, brushing teeth, cutting finger nails, besides other practices. Some practices are gender-specific, such as by a woman during her menstruation. Toiletry bags holds body hygiene and toiletry supplies.
Anal hygiene is the practice that a person performs on the anal area of themselves after defecation. The anus and buttocks may be either washed with liquids or wiped with toilet paper or adding gel wipe[50] to toilet tissue as an alternative to wet wipes or other solid materials in order to remove remnants of feces.
People tend to develop a routine for attending to their personal hygiene needs. Other personal hygienic practices would include covering one's mouth when coughing, disposal of soiled tissues appropriately, making sure toilets are clean, and making sure food handling areas are clean, besides other practices. Some cultures do not kiss or shake hands to reduce transmission of bacteria by contact.
Personal grooming extends personal hygiene as it pertains to the maintenance of a good personal and public appearance, which need not necessarily be hygienic. It may involve, for example, using deodorants or perfume, shaving, or combing, besides other practices.
Excessive body hygiene
Excessive body hygiene is one example of obsessive compulsive disorder.
Excessive body hygiene and allergies
The hygiene hypothesis was first formulated in 1989 by Strachan who observed that there was an inverse relationship between family size and development of atopic allergic disorders—the more children in a family, the less likely they were to develop these allergies.[51] From this, he hypothesized that a lack of exposure to "infections" in early childhood transmitted by contact with older siblings could be a cause of the rapid rise in atopic disorders over the last 30 to 40 years. Strachan further proposed that the reason why this exposure no longer occurs is not only because of the trend towards smaller families, but also "improved household amenities and higher standards of personal cleanliness".
Although there is substantial evidence that some microbial exposures in early childhood can in some way protect against allergies, there is no evidence that humans need exposure to harmful microbes (infection) or that it is necessary to suffer a clinical infection.[52][53][54][55] Nor is there evidence that hygiene measures such as hand washing, food hygiene etc. are linked to increased susceptibility to atopic disease.[43][44] If this is the case, there is no conflict between the goals of preventing infection and minimising allergies. A consensus is now developing among experts that the answer lies in more fundamental changes in lifestyle etc. that have led to decreased exposure to certain microbial or other species, such as helminths, that are important for development of immuno-regulatory mechanisms.[56] There is still much uncertainty as to which lifestyle factors are involved.
Although media coverage of the hygiene hypothesis has declined, a strong ‘collective mindset’ has become established that dirt is ‘healthy’ and hygiene somehow ‘unnatural’. This has caused concern among health professionals that everyday life hygiene behaviours, which are the foundation of public health, are being undermined. In response to the need for effective hygiene in home and everyday life settings, the International Scientific Forum on Home Hygiene has developed a "risk-based" or targeted approach to home hygiene that seeks to ensure that hygiene measures are focussed on the places, and at the times most critical for infection transmission.[7] Whilst targeted hygiene was originally developed as an effective approach to hygiene practice, it also seeks, as far as possible, to sustain "normal" levels of exposure to the microbial flora of our environment to the extent that is important to build a balanced immune system.
Excessive body hygiene of internal ear canals
Excessive cleaning of the ear canals can result in infection or irritation. The ear canals require less care than other parts of the body because they are sensitive and mostly self-cleaning; that is, there is a slow and orderly migration of the skin lining the ear canal from the eardrum to the outer opening of the ear. Old earwax is constantly being transported from the deeper areas of the ear canal out to the opening where it usually dries, flakes, and falls out.[57] Attempts to clean the ear canals through the removal of earwax can push debris and foreign material into the ear that the natural movement of ear wax out of the ear would have removed.
Oral hygiene
It is recommended that all healthy adults brush twice a day,[58] softly,[59] with the correct technique, replacing their toothbrush every few months (~3) or after a bout of illness.[60]
There are a number of common oral hygiene misconceptions. It is not correct to rinse the mouth with water after brushing.[61] It is also not recommended to brush immediately after drinking acidic substances, including sparkling water. It is also recommended to floss once a day,[62] with a different piece of floss at each flossing session. The Effectiveness of Tooth Mousse is in debate.[63] Visits to a dentist for a checkup every year at least are recommended.[64]
Culinary (food) hygiene
Culinary hygiene pertains to the practices related to food management and cooking to prevent food contamination, prevent food poisoning and minimize the transmission of disease to other foods, humans or animals. Culinary hygiene practices specify safe ways to handle, store, prepare, serve and eat food.
Culinary practices include:
- Cleaning and disinfection of food-preparation areas and equipment (for example using designated cutting boards for preparing raw meats and vegetables). Cleaning may involve use of chlorine bleach, ethanol, ultraviolet light, etc. for disinfection.
- Careful avoidance of meats contaminated by trichina worms, salmonella, and other pathogens; or thorough cooking of questionable meats.
- Extreme care in preparing raw foods, such as sushi and sashimi.
- Institutional dish sanitizing by washing with soap and clean water.
- Washing of hands thoroughly before touching any food.
- Washing of hands after touching uncooked food when preparing meals.
- Not using the same utensils to prepare different foods.
- Not sharing cutlery when eating.
- Not licking fingers or hands while or after eating.
- Not reusing serving utensils that have been licked.
- Proper storage of food so as to prevent contamination by vermin.
- Refrigeration of foods (and avoidance of specific foods in environments where refrigeration is or was not feasible).
- Labeling food to indicate when it was produced (or, as food manufacturers prefer, to indicate its "best before" date).
- Proper disposal of uneaten food and packaging.
Personal service hygiene
Personal service hygiene pertains to the practices related to the care and use of instruments used in the administration of personal care services to people:
Personal hygiene practices include:
- Sterilization of instruments used by service providers including hairdressers, aestheticians, and other service providers.
- Sterilization by autoclave of instruments used in body piercing and tattoo marking.
- Cleaning hands.
Sleep hygiene
Sleep hygiene is the recommended behavioral and environmental practice that is intended to promote better quality sleep.[65] This recommendation was developed in the late 1970s as a method to help people with mild to moderate insomnia, but, as of 2014, the evidence for effectiveness of individual recommendations is "limited and inconclusive".[65] Clinicians assess the sleep hygiene of people who present with insomnia and other conditions, such as depression, and offer recommendations based on the assessment. Sleep hygiene recommendations include establishing a regular sleep schedule, using naps with care, not exercising physically or mentally too close to bedtime, limiting worry, limiting exposure to light in the hours before sleep, getting out of bed if sleep does not come, not using bed for anything but sleep and avoiding alcohol as well as nicotine, caffeine, and other stimulants in the hours before bedtime, and having a peaceful, comfortable and dark sleep environment.
History

The earliest written account of Elaborate codes of hygiene can be found in several Hindu texts, such as the Manusmriti and the Vishnu Purana.[66] Bathing is one of the five Nitya karmas (daily duties) in Hinduism, and not performing it leads to sin, according to some scriptures.
Regular bathing was a hallmark of Roman civilization.[67] Elaborate baths were constructed in urban areas to serve the public, who typically demanded the infrastructure to maintain personal cleanliness. The complexes usually consisted of large, swimming pool-like baths, smaller cold and hot pools, saunas, and spa-like facilities where individuals could be depilated, oiled, and massaged. Water was constantly changed by an aqueduct-fed flow. Bathing outside of urban centers involved smaller, less elaborate bathing facilities, or simply the use of clean bodies of water. Roman cities also had large sewers, such as Rome's Cloaca Maxima, into which public and private latrines drained. Romans didn't have demand-flush toilets but did have some toilets with a continuous flow of water under them. The Romans used scented oils (mostly from Egypt), among other alternatives.
Christianity places an emphasis on hygiene.[68] Despite the denunciation of the mixed bathing style of Roman pools by early Christian clergy, as well as the pagan custom of women naked bathing in front of men, this did not stop the Church from urging its followers to go to public baths for bathing,[69] which contributed to hygiene and good health according to the Church Father, Clement of Alexandria. The Church built public bathing facilities that were separate for both sexes near monasteries and pilgrimage sites; also, the popes situated baths within church basilicas and monasteries since the early Middle Ages.[70] Pope Gregory the Great urged his followers on value of bathing as a bodily need.[71] The use of water in many Christian countries is due in part to the Biblical toilet etiquette which encourages washing after all instances of defecation.[72] The bidet is common in predominantly Catholic countries where water is considered essential for anal cleansing.[73][74]
Islamic world
Islam stresses the importance of cleanliness and personal hygiene.[75] Islamic hygienical jurisprudence, which dates back to the 7th century, has a number of elaborate rules. Taharah (ritual purity) involves performing wudu (ablution) for the five daily salah (prayers), as well as regularly performing ghusl (bathing), which led to bathhouses being built across the Islamic world.[76][77] Islamic toilet hygiene also requires washing with water after using the toilet, for purity and to minimize germs.[78]
In the Abbasid Caliphate (8th-13th centuries), its capital city of Baghdad (Iraq) had 65,000 baths, along with a sewer system.[79] Cities of the medieval Islamic world had water supply systems powered by hydraulic technology that supplied drinking water along with much greater quantities of water for ritual washing, mainly in mosques and hammams (baths). Bathing establishments in various cities were rated by Arabic writers in travel guides. Medieval Islamic cities such as Baghdad, Córdoba (Islamic Spain), Fez (Morocco) and Fustat (Egypt) also had sophisticated waste disposal and sewage systems with interconnected networks of sewers. The city of Fustat also had multi-storey tenement buildings (with up to six floors) with flush toilets, which were connected to a water supply system, and flues on each floor carrying waste to underground channels.[80]
A basic form of contagion theory dates back to medicine in the medieval Islamic world, where it was proposed by Persian physician Ibn Sina (also known as Avicenna) in The Canon of Medicine (1025), the most authoritative medical textbook of the Middle Ages. He mentioned that people can transmit disease to others by breath, noted contagion with tuberculosis, and discussed the transmission of disease through water and dirt.[81] The concept of invisible contagion was eventually widely accepted by Islamic scholars. In the Ayyubid Sultanate, they referred to them as najasat ("impure substances"). The fiqh scholar Ibn al-Haj al-Abdari (c. 1250–1336), while discussing Islamic diet and hygiene, gave advice and warnings about how contagion can contaminate water, food, and garments, and could spread through the water supply.[82]
Hard toilet soap with a pleasant smell was invented in the Middle East during the Islamic Golden Age, when soap-making became an established industry. Recipes for soap-making are described by Muhammad ibn Zakariya al-Razi (854–925), who also gave a recipe for producing glycerine from olive oil. In the Middle East, soap was produced from the interaction of fatty oils and fats with alkali. In Syria, soap was produced using olive oil together with alkali and lime. Soap was exported from Syria to other parts of the Muslim world and to Europe.[83] Two key Islamic innovations in soapmaking was the invention of bar soap, described by al-Razi, and the addition of scents using perfume technology perfected in the Islamic world.[84] Soapmaking thus first became an established trade during the Islamic Golden Age, corresponding to the so-called "Dark Ages" in Europe.
In the 9th century, Ziryab invented a type of deodorant to get rid of bad odors.[85] He also promoted morning and evening baths, and emphasized the maintenance of personal hygiene. Ziryab is thought to have invented a type of toothpaste, which he popularized throughout Islamic Iberia.[86] The exact ingredients of this toothpaste are not currently known,[87] but it was reported to have been both "functional and pleasant to taste."[86]
Medieval Europe
Contrary to popular belief[88] and although the Early Christian leaders, such as Boniface I,[89] condemned bathing as unspiritual,[90] bathing and sanitation were not lost in Europe with the collapse of the Roman Empire.[91][92]
Northern Europeans were not in the habit of bathing: in the ninth century Notker the Stammerer, a Frankish monk of St Gall, related a disapproving anecdote that attributed ill results of personal hygiene to an Italian fashion:
There was a certain deacon who followed the habits of the Italians in that he was perpetually trying to resist nature. He used to take baths, he had his head very closely shaved, he polished his skin, he cleaned his nail, he had his hair cut as short as if it were turned on a lathe, and he wore linen underclothes and a snow-white shirt.
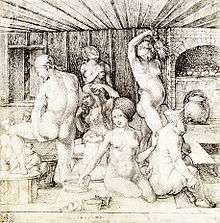
Secular medieval texts constantly refer to the washing of hands before and after meals, but Sone de Nansay, hero of a 13th-century romance, discovers to his chagrin that the Norwegians do not wash up after eating.[93] In the 11th and 12th centuries, bathing was essential to the Western European upper class: the Cluniac monasteries to which they resorted or retired were always provided with bathhouses, and even the monks were required to take full immersion baths twice a year, at the two Christian festivals of renewal, though exhorted not to uncover themselves from under their bathing sheets.[94] In 14th century Tuscany, the newlywed couple's bath together was such a firm convention one such couple, in a large coopered tub, is illustrated in fresco in the town hall of San Gimignano.[95]
Bathing had fallen out of fashion in Northern Europe long before the Renaissance, when the communal public baths of German cities were in their turn a wonder to Italian visitors. Bathing was replaced by the heavy use of sweat-bathing and perfume, as it was thought in Europe that water could carry disease into the body through the skin. Bathing encouraged an erotic atmosphere that was played upon by the writers of romances intended for the upper class;[96] in the tale of Melusine the bath was a crucial element of the plot. "Bathing and grooming were regarded with suspicion by moralists, however, because they unveiled the attractiveness of the body. Bathing was said to be a prelude to sin, and in the penitential of Burchard of Worms we find a full catalogue of the sins that ensued when men and women bathed together."[97] Medieval church authorities believed that public bathing created an environment open to immorality and disease; the 26 public baths of Paris in the late 13th century were strictly overseen by the civil authorities.[97] At a later date Roman Catholic Church officials even banned public bathing in an unsuccessful effort to halt syphilis epidemics from sweeping Europe.[98]
Until the late 19th century, only the elite in Western cities typically possessed indoor facilities for relieving bodily functions. The poorer majority used communal facilities built above cesspools in backyards and courtyards. This changed after Dr. John Snow discovered that cholera was transmitted by the fecal contamination of water. Though it took decades for his findings to gain wide acceptance, governments and sanitary reformers were eventually convinced of the health benefits of using sewers to keep human waste from contaminating water. This encouraged the widespread adoption of both the flush toilet and the moral imperative that bathrooms should be indoors and as private as possible.
Modern sanitation was not widely adopted until the 19th and 20th centuries. According to medieval historian Lynn Thorndike, people in Medieval Europe probably bathed more than people did in the 19th century.[99] Some time after Louis Pasteur's experiments proved the germ theory of disease and Joseph Lister and others put them into practice in sanitation, hygienic practices came to be regarded as synonymous with health, as they are in modern times.
Society and culture
Religious hygienic customs
Many religions require or encourage ritual purification via bathing or immersing the hands in water. In Islam, washing oneself via wudu or ghusl is necessary for performing prayer. Islamic tradition also lists a variety of rules concerning proper hygiene after using the bathroom. The Bahá'í Faith mandates the washing of the hands and face prior to the obligatory Bahá'í prayers. Orthodox Judaism requires a mikveh bath following menstruation and childbirth, while washing the hands is performed upon waking up and before eating bread. The Ethiopian Orthodox Tewahedo Church prescribes several kinds of hand washing for example after leaving the latrine, lavatory or bathhouse, or before prayer, or after eating a meal.[100]
See also
References
- "Water, Sanitation and Hygiene Poster Set with Trainer Guide". Centre for Affordable Water and Sanitation Technology (CAWST). March 2013.
- "Hygiene: Overview". World Health Organization (WHO). Retrieved 29 January 2020.
- ὑγιεινός, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on Perseus
- ὑγιής, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on Perseus
- ὑγίεια, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on Perseus
- Bloomfield SF, Exner M, Fara GM, Nath KJ, Scott EA, Van der Voorden C (2009). "The global burden of hygiene-related diseases in relation to the home and community". International Scientific Forum on Home Hygiene.
- "The Chain of Infection Transmission in the Home and Everyday Life Settings, and the Role of Hygiene in Reducing the Risk of Infection". International Scientific Forum on Home Hygiene. 2012.
- U.S. Pet Ownership & Demographics Sourcebook. Schaumburg, IL: AMVA. 2012. ISBN 978-1-882691-28-9.
- Bloomfield, Sally F.; Aiello, Allison E.; Cookson, Barry; O'Boyle, Carol; Larson, Elaine L. (December 2007). "The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including hand washing and alcohol-based hand sanitizers". American Journal of Infection Control. 35 (10): S27–S64. doi:10.1016/j.ajic.2007.07.001. PMC 7115270.
- "Emergency treatment of drinking-water at the point of use" (PDF). World Health Organization. 2011.
- "Water, Sanitation and Hygiene Standards for Schools in Low-cost Settings" (PDF). World Health Organization. 2009.
- "How can personal hygiene be maintained in difficult circumstances?". World Health Organization. 2005.
- Baker, K.K.; Dil Farzana, F.; Ferdous, F.; Ahmed, S.; Kumar Das, S.; Faruque, A.S.G.; Nasrin, D.; Kotloff, K.L.; Nataro, J.P.; Kolappaswamy, K.; Levine, M.M. (28 April 2014). "Association between Moderate-to-Severe Diarrhea in Young Children in the Global Enteric Multi center Study (GEMS) and Types of Hand washing Materials Used by Caretakers in Mirzapur, Bangladesh". American Journal of Tropical Medicine and Hygiene. 91 (1): 181–89. doi:10.4269/ajtmh.13-0509. PMC 4080560. PMID 24778193.
- "The Five Keys to Safer Food Programme". World Health Organization. Retrieved 2012-11-14.
- Beumer R, Bloomfield SF, Exner M, Fara GM, Nath KJ, Scott EA (2008). "Hygiene procedures in the home and their effectiveness: a review of the scientific evidence base". International Scientific Forum on Home Hygiene.
- Scott E. Microbial Risk Reduction: The Benefits of Effective Cleaning. 2010 In preparation.
- Cole E. Allergen control through routine cleaning of pollutant reservoirs in the home environment. Proceedings of Healthy Building 2000;4:435-6.
- Bloomfield SF, Exner M, Signorelli C, Nath KJ, Scott EA (2011). "The infection risks associated with clothing and household linens in home and everyday life settings, and the role of laundry". International Scientific Forum on Home Hygiene.
- Bloomfield SF, Exner M, Signorelli C, Nath KJ, Scott EA (2012). "The chain of infection transmission in the home and everyday life settings, and the role of hygiene in reducing the risk of infection". International Scientific Forum on Home Hygiene.
- Larson EL, Lin SX, Gomez-Pichardo C (2004). "Predictors of infectious disease symptoms in inner city households". Nurs Res. 53 (3): 190–97. doi:10.1097/00006199-200405000-00006. PMID 15167507.
- "Recommendations for future collaboration between the U.S. and EU" (PDF). Transatlantic Taskforce on Antimicrobial Resistance. 2011. Archived from the original (PDF) on 2012-07-08.
- Bloomfield SF (2013). "Spread of Antibiotic Resistant Strains in the Home and Community". International Scientific Forum on Home Hygiene.
- Bloomfield SF, Cookson BD, Falkiner FR, Griffith C, Cleary V (2006). "Methicillin resistant Staphylococcus aureus (MRSA), Clostridium difficile and ESBL-producing Escherichia coli in the home and community: assessing the problem, controlling the spread". International Scientific Forum on Home Hygiene.
- Bloomfield SF, Exner M, Signorelli C, Scott EA (2013). "Effectiveness of laundering processes used in domestic (home) settings". International Scientific Forum on Home Hygiene.
- "Clothing, household linens, laundry and hygiene Factsheet". International Scientific Forum on Home Hygiene. 2013.
- "Laundry: Washing Infected Material". Centers for Disease Control and Prevention. Archived from the original on 2 March 2013. Retrieved 22 February 2017.
- "Guidelines for Environmental Infection Control in Health-Care Facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC)". CDC. 2003. Recommendations: Laundry and Bedding.
- "Health Technical Memorandum 01-04: Decontamination of linen for health and social care" (PDF). UK Department of Health. March 2016.
- "Uniform and workwear: Guidance on uniform and workwear policies for NHS employers" (PDF). UK Department of Health. March 2010. Archived from the original (PDF) on 2012-09-07. Retrieved 2013-10-29.
- "Laundry treatments at high and low temperatures". UK health and Safety Executive. 2013.
- Vossebein L. Wäschehygiene im Haushalt / Linen Hygiene in Households SOFW-Journal, 139, 3-2013, 51–58
- Lucassen, Ralf; Merettig, Nadine; Bockmühl, Dirk P. (15 July 2013). "Antimicrobial Efficacy of Hygiene Rinsers under Consumer-Related Conditions". Tenside Surfactants Detergents. 50 (4): 259–62. doi:10.3139/113.110257.
- "Home hygiene – prevention of infection at home: a training resource for carers and their trainers". International Scientific Forum on Home Hygiene. 2003.
- "Goal 6: Clean water and sanitation". UNDP. Retrieved 18 April 2017.
- "The global burden of disease: 2004 update". World Health Organization.
- Curtis V, Cairncross S (2003). "Effect of washing hands with soap on diarrhea risk in the community: a systematic review". Lancet Infectious Diseases. 3 (5): 275–81. doi:10.1016/S1473-3099(03)00606-6. PMID 12726975.
- Aiello, AE; Coulborn, RM; Perez, V; Larson, EL (August 2008). "Effect of Hand Hygiene on Infectious Disease Risk in the Community Setting: A Meta-Analysis". American Journal of Public Health. 98 (8): 1372–81. doi:10.2105/AJPH.2007.124610. PMC 2446461. PMID 18556606.
- Fewtrell L, Kauffman RB, Kay D, Enanoria W, Haller L, Colford JM (2005). "Water, sanitation, and hygiene interventions to reduce diarrhea in less developed countries: a systematic review and meta-analysis". Lancet Infectious Diseases. 5 (1): 42–52. doi:10.1016/S1473-3099(04)01253-8. PMID 15620560.
- Jeroen Ensink (2006). "Health impact of handwashing with soap". WELL. Archived from the original on 2010-06-19.
- Jefferson T, Foxlee R, Del Mar C, et al. (2007). "Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review". British Medical Journal. 336 (7635): 77–80. doi:10.1136/BMJ.39393.510347.BE. PMC 2190272. PMID 18042961.
- Luby S, Agboatalla M, Feikin DR, Painter J, Billhimmer W, Atref A, Hoekstra RM (2005). "Effect of hand-washing on child health: a randomized control trial". Lancet. 366 (9481): 225–33. doi:10.1016/S0140-6736(05)66912-7. PMID 16023513.
- Luby S, Agboatwalla M, Schnell BM, Hoekstra RM, Rahbar MH, Keswick BH (2002). "The effect of antibacterial soap on impetigo incidence, Karachi, Pakistan". American Journal of Tropical Medicine and Hygiene. 67 (4): 430–35. doi:10.4269/ajtmh.2002.67.430. PMID 12452499.
- Bloomfield SF, Nath KJ (2009). "Use of ash and mud for hand-washing in low income communities". International Scientific Forum on Home Hygiene.
- "Guidelines for the prevention of infection and cross-infection in the domestic environment: focus on home hygiene issues in developing countries". International Scientific Forum on Home Hygiene. 2002.
- "Combating waterborne disease at the household level" (PDF). World Health Organization. 2007.
- "Household water storage, handling and point-of-use treatment". International Scientific Forum on Home Hygiene. 2006.
- "Water quality interventions to prevent diarrhoea: Cost and cost-effectiveness". World Health Organization. 2008.
- "Household Water Treatment and Safe Storage Following Emergencies and Disasters" (PDF). World Health Organisation. 2005.
- "Managing water in the home". World Health Organization. 2002.
- "Toilet Paper Gel Cleans Up No. 2 In More Ways Than One".
- Strachan, DP (August 2000). "Family size, infection and atopy: the first decade of the 'hygiene hypothesis'". Thorax. 55 (1): S2–S10. doi:10.1136/thorax.55.suppl_1.s2. PMC 1765943. PMID 10943631.
- Stanwell Smith R, Bloomfield SF, Rook GA (2012). "The Hygiene Hypothesis and its Implications for Home Hygiene, Lifestyle and Public Health". International Scientific Forum on Home Hygiene.
- "The Hygiene Hypothesis and its implications for home hygiene, lifestyle and public health: Summary". International Scientific Forum on Home Hygiene. 2012.
- Bloomfield, S. F.; Stanwell-Smith, R.; Crevel, R.W.R.; Pickup, J. (April 2006). "Too clean, or not too clean: the Hygiene Hypothesis and home hygiene" (PDF). Clinical and Experimental Allergy. 36 (4): 402–25. doi:10.1111/j.1365-2222.2006.02463.x. PMC 1448690. PMID 16630145.
- Bremner, SA; Carey, IM; DeWilde, S; Richards, N; Maier, WC; Hilton, SR; Strachan, DP; Cook, DG (March 2008). "Infections presenting for clinical care in early life and later risk of hay fever in two UK birth cohorts". Allergy. 63 (3): 274–83. doi:10.1111/j.1398-9995.2007.01599.x. PMID 18269673.
- Rook, G. A. W. (11 March 2010). "99th Dahlem Conference on Infection, Inflammation and Chronic Inflammatory Disorders: Darwinian medicine and the 'hygiene' or 'old friends' hypothesis". Clinical & Experimental Immunology. 160 (1): 70–79. doi:10.1111/j.1365-2249.2010.04133.x. PMC 2841838. PMID 20415854.
- "Ear Wax Symptoms, Treatment, Causes – When should ear wax be removed?". medicinenet.com.
- "Brushing & Flossing: Technique & Choosing Dental Products". www.colgate.com.
- Corporation, Australian Broadcasting. "Can you brush your teeth too hard? – Health & Wellbeing". www.abc.net.au.
- "Brush Teeth". www.mouthhealthy.org. American Dental Association.
- Choices, NHS. "Teeth cleaning guide – Live Well". www.nhs.uk.
- "The Medical Benefit of Daily Flossing Called Into Question". www.ada.org.
- Raphael, Sarah; Blinkhorn, Anthony (25 September 2015). "Is there a place for Tooth Mousse® in the prevention and treatment of early dental caries? A systematic review". BMC Oral Health. 15 (1): 113. doi:10.1186/s12903-015-0095-6. PMC 4583988. PMID 26408042.
- Hammond, Claudia. "How often do you need to see a dentist?".
- Irish, Leah A.; Kline, Christopher E; Gunn, Heather E; Buysse, Daniel J; Hall, Martica H (October 2014). "The role of sleep hygiene in promoting public health: A review of empirical evidence". Sleep Medicine Reviews. 22: 23–36. doi:10.1016/j.smrv.2014.10.001. PMC 4400203. PMID 25454674.
- "Aryan Code of Toilets (2nd Century AD)". Sulabh International Museum of Toilets.
- "Roman bath houses". Time Team. Channel Four Television Corporation. Archived from the original on 4 February 2007.
- Warsh, Cheryl Krasnick (2006). Children's Health Issues in Historical Perspective. Veronica Strong-Boag. Wilfrid Laurier Univ. Press. p. 315. ISBN 978-0-88920-912-1.
... From Fleming's perspective, the transition to Christianity required a good dose of personal and public hygiene ...
- Warsh, Cheryl Krasnick (2006). Children's Health Issues in Historical Perspective. Veronica Strong-Boag. Wilfrid Laurier Univ. Press. p. 315. ISBN 978-0-88920-912-1.
... Thus bathing also was considered a part of good health practice. For example, Tertullian attended the baths and believed them hygienic. Clement of Alexandria, while condemning excesses, had given guidelines for Christian] who wished to attend the baths ...
- Thurlkill, Mary (2016). Sacred Scents in Early Christianity and Islam: Studies in Body and Religion. Rowman & Littlefield. pp. 6–11. ISBN 978-0-7391-7453-1.
... Clement of Alexandria (d. c. 215 CE) allowed that bathing contributed to good health and hygiene ... Christian skeptics could not easily dissuade the baths' practical popularity, however; popes continued to build baths situated within church basilicas and monasteries throughout the early medieval period ...
- Squatriti, Paolo (2002). Water and Society in Early Medieval Italy, AD 400-1000, Parti 400-1000. Cambridge University Press. p. 54. ISBN 978-0-521-52206-9.
... but baths were normally considered therapeutic until the days of Gregory the Great, who understood virtuous bathing to be bathing "on account of the needs of body" ...
- E. Clark, Mary (2006). Contemporary Biology: Concepts and Implications. University of Michigan Press. ISBN 9780721625973.
- E. Clark, Mary (2006). Contemporary Biology: Concepts and Implications. University of Michigan Press. p. 613. ISBN 9780721625973.
Douching is commonly practiced in Catholic countries. The bidet ... is still commonly found in France and other Catholic countries.
- Made in Naples. Come Napoli ha civilizzato l'Europa (e come continua a farlo) [Made in Naples. How Naples civilised Europe (And still does it)] (in Italian). Addictions-Magenes Editoriale. 2013. ISBN 978-8866490395.
- Majeed, Azeem (22 December 2005). "How Islam changed medicine". BMJ. 331 (7531): 1486–1487. doi:10.1136/bmj.331.7531.1486. ISSN 0959-8138. PMC 1322233. PMID 16373721.
- https://www.britannica.com/topic/tahara-Islam
- "Ṭahāra". Encyclopedia Britannica.
- Israr Hasan (2006), Muslims in America, p. 144, ISBN 978-1-4259-4243-4
- Judith Kidd, Rosemary Rees, Ruth Tudor (2000). Life in Medieval Times. Heinemann. p. 165. ISBN 0435325949.CS1 maint: multiple names: authors list (link)
- Colin Chant, David Goodman (2005). Pre-Industrial Cities and Technology. Routledge. pp. 136–8. ISBN 1134636202.
- Byrne, Joseph Patrick (2012). Encyclopedia of the Black Death. ABC-CLIO. p. 29. ISBN 9781598842531.
- Reid, Megan H. (2013). Law and Piety in Medieval Islam. Cambridge University Press. pp. 106, 114, 189–190. ISBN 9781107067110.
- Ahmad Y. al-Hassan (2001), Science and Technology in Islam: Technology and applied sciences, pages 73–74 Archived 2017-12-09 at the Wayback Machine, UNESCO
- Kalın, İbrahim (2014). The Oxford Encyclopedia of Philosophy, Science, and Technology in Islam. Oxford University Press. p. 137. ISBN 9780199812578.
- Menocal, María Rosa; Raymond P. Scheindlin; Michael Anthony Sells, eds. (2000), The Literature of Al-Andalus, Cambridge University Press
- van Sertima, Ivan (1992), The Golden Age of the Moor, Transaction Publishers, p. 267, ISBN 978-1-56000-581-0
- Lebling Jr., Robert W. (July–August 2003), "Flight of the Blackbird", Saudi Aramco World: 24–33, retrieved 28 January 2008
- "Did Medieval Brides Really Smell Bad?". about.com.
- [Dogma Evolution & Papal Fallacies (Google eBook); by Imma Penn; AuthorHouse, May 30, 2007; p. 223]
- "Ablutions or Bathing, Historical Perspectives + (Latin: abluere, to wash away)". Word Information. Retrieved 22 February 2017.
- "The Great Famine and the Black Death – 1315–1317, 1346–1351 – Lectures in Medieval History – Dr. Lynn H. Nelson, Emeritus Professor, Medieval History, KU". vlib.us.
- "Middle Ages Hygiene". middle-ages.org.uk.
- Noted in Danielle Régnier-Bohler, "Imagining the self" in Duby 1988:363f.
- Philippe Braunstein "Solitude: eleventh to thirteenth century", in Georges Duby, ed. A History of Private Life: II. Revelations of the Medieval World 1988:525
- Fresco of c. 1320 illustrated in Charles de la Roncière, "Tuscan notables on the eve of the Renaissance" in Duby 1988:232.
- Régnier-Bohler 1988:363ff.
- Braunstein 1988:525.
- Paige, John C; Laura Woulliere Harrison (1987). Out of the Vapors: A Social and Architectural History of Bathhouse Row, Hot Springs National Park (PDF). U.S. Department of the Interior.
- "Thorndike, Tales of the Middle Ages – Daily Life". Gode Cookery. Retrieved 22 February 2017.
- IS THE CHURCH OF ETHIOPIA A JUDAIC CHURCH ?
Further reading
External links
| Look up hygiene in Wiktionary, the free dictionary. |
| Wikisource has the text of the 1905 New International Encyclopedia article Sanitary Science. |
- US Centre for Disease Control and Prevention
- European Centre for Disease Control and Prevention
- Water Sanitation and Hygiene
- The International Scientific Forum on Home Hygiene
- Hygiene Centre, London School of Hygiene and Tropical Medicine
- Centers for Disease Control on hand hygiene in healthcare settings
