Pentoxifylline
Pentoxifylline, also known as oxpentifylline, is a xanthine derivative used as a drug to treat muscle pain in people with peripheral artery disease.[4] It is generic and sold under many brand names worldwide.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌpɛntɒkˈsɪfɪliːn, -ɪn/ |
| Trade names | Many names worldwide[1] |
| Other names | oxpentifylline (former AAN)[2] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a685027 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 10–30%[3] |
| Metabolism | Hepatic and via erythrocytes |
| Elimination half-life | 0.4–0.8 hours (1–1.6 hours for active metabolite)[3] |
| Excretion | Urine (95%), faeces (<4%)[3] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.026.704 |
| Chemical and physical data | |
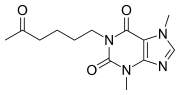
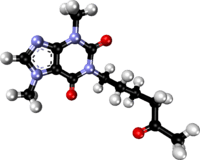
| Formula | C13H18N4O3 |
| Molar mass | 278.312 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Medical uses
Its primary use in medicine is to reduce pain, cramping, numbness, or weakness in the arms or legs which occurs due to intermittent claudication, a form of muscle pain resulting from peripheral artery diseases.[4] This is its only FDA, MHRA and TGA-labelled indication.[2][5][6] However, pentoxifylline is also recommended for off-label use as an adjunct to compression bandaging for the treatment of chronic venous leg ulcers by the Scottish Intercollegiate Guidelines Network) (SIGN) [7] as this has been shown to improve healing rates.[8]
Pentoxifylline has also been shown to be of benefit in alcoholic hepatitis, with some studies demonstrating a reduction in risk of hepatorenal syndrome.
Adverse effects
Common side effects are belching, bloating, stomach discomfort or upset, nausea, vomiting, indigestion, dizziness, and flushing. Uncommon and rare side effects include angina, palpitations, hypersensitivity, itchiness, rash, hives, bleeding, hallucinations, arrhythmias, and aseptic meningitis.[2][3][5][6]
Contraindications include intolerance to pentoxifylline or other xanthine derivatives, recent retinal or cerebral haemorrhage, and risk factors for haemorrhage.[3]
Mechanism
Like other methylated xanthine derivatives, pentoxifylline is a competitive nonselective phosphodiesterase inhibitor[9] which raises intracellular cAMP, activates PKA, inhibits TNF[10][11] and leukotriene[12] synthesis, and reduces inflammation and innate immunity.[12] In addition, pentoxifylline improves red blood cell deformability (known as a haemorrheologic effect), reduces blood viscosity and decreases the potential for platelet aggregation and blood clot formation.[13] Pentoxifylline is also an antagonist at adenosine 2 receptors.[14]
Research
There is some evidence that pentoxifylline can lower the levels of some biomarkers in non-alcoholic steatohepatitis but evidence is insufficient to determine if the drug is safe and effective for this use.[15] Animal studies have been conducted exploring the use of pentoxifylline for erectile dysfunction[16] and hearing loss.[17] Human studies have been conducted for Peyronie's disease.[18]
Pentoxifylline, in combination with tocopherol and clodronate, has been found to heal refractory osteoradionecrosis of the jaw,[19] and to be prophylactic against osteoradionecrosis.[20]
In a Cochrane systematic review on the use of pentoxifylline for intermittent claudication in 2015, the following was concluded "The quality of included studies was generally low, and very large variability between studies was noted in reported findings including duration of trials, doses of pentoxifylline and distances participants could walk at the start of trials. Most included studies did not report on randomisation techniques or how treatment allocation was concealed, did not provide adequate information to permit judgement of selective reporting and did not report blinding of outcome assessors. Given all these factors, the role of pentoxifylline in intermittent claudication remains uncertain, although this medication was generally well tolerated by participants".[21]
See also
- Lisofylline, an active metabolite of pentoxifylline
- Propentofylline
- Cilostazol, a PDE-3 inhibitor with better evidence for intermittent claudication on the Cochrane review cited above.
References
- Drugs.com drugs.com international listings for Pentoxifylline. Page accessed Feb 1, 206
- "PRODUCT INFORMATION TRENTAL® 400" (PDF). TGA eBusiness Services. sanofi-aventis australia pty limited. 25 March 2010. Retrieved 3 February 2014.
- "Trental, Pentoxil (pentoxifylline) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 3 February 2014.
- Salhiyyah K, Senanayake E, Abdel-Hadi M, Booth A, Michaels JA (September 2015). "Pentoxifylline for intermittent claudication". The Cochrane Database of Systematic Reviews. 9: CD005262. doi:10.1002/14651858.CD005262.pub3. PMC 6513423. PMID 26417854.
- "PENTOXIFYLLINE tablet, extended release [Apotex Corp.]". DailyMed. Apotex Corp. February 2013. Retrieved 3 February 2014.
- "Trental 400 - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Sanofi. 10 October 2013. Retrieved 3 February 2014.
- SIGN (2010) Management of chronic venous leg ulcers. Clinical guideline No. 120. Scottish Intercollegiate Guidelines Network. www.sign.ac.uk ISBN 978-1-905813-66-7
- Jull, Andrew B; Arroll, Bruce; Parag, Varsha; Waters, Jill (2012). "Pentoxifylline for treating venous leg ulcers". Cochrane Database of Systematic Reviews. 12: CD001733. doi:10.1002/14651858.CD001733.pub3. ISSN 1465-1858. PMC 7061323. PMID 23235582.
- Essayan DM (2001). "Cyclic nucleotide phosphodiesterases". The Journal of Allergy and Clinical Immunology. 108 (5): 671–80. doi:10.1067/mai.2001.119555. PMID 11692087.
- Deree J, Martins JO, Melbostad H, Loomis WH, Coimbra R (2008). "Insights into the regulation of TNF-alpha production in human mononuclear cells: the effects of non-specific phosphodiesterase inhibition". Clinics. 63 (3): 321–8. doi:10.1590/S1807-59322008000300006. PMC 2664230. PMID 18568240.
- Marques LJ, Zheng L, Poulakis N, Guzman J, Costabel U (1999). "Pentoxifylline inhibits TNF-alpha production from human alveolar macrophages". American Journal of Respiratory and Critical Care Medicine. 159 (2): 508–11. doi:10.1164/ajrccm.159.2.9804085. PMID 9927365.
- Peters-Golden M, Canetti C, Mancuso P, Coffey MJ (2005). "Leukotrienes: underappreciated mediators of innate immune responses". Journal of Immunology. 174 (2): 589–94. doi:10.4049/jimmunol.174.2.589. PMID 15634873.
- Ward A, Clissold SP (1987). "Pentoxifylline. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy". Drugs. 34 (1): 50–97. doi:10.2165/00003495-198734010-00003. PMID 3308412.
- Rodríguez-Morán M, Guerrero-Romero F (2008). "Efficacy of pentoxifylline in the management of microalbuminuria in patients with diabetes". Current Diabetes Reviews. 4 (1): 55–62. doi:10.2174/157339908783502343. PMID 18220696.
- Li W, Zheng L, Sheng C, Cheng X, Qing L, Qu S (2011). "Systematic review on the treatment of pentoxifylline in patients with non-alcoholic fatty liver disease". Lipids in Health and Disease. 10: 49. doi:10.1186/1476-511X-10-49. PMC 3088890. PMID 21477300.
- Anele, U. A.; Morrison, B. F.; Burnett, A. L. (2015). "Molecular pathophysiology of priapism: Emerging targets". Current Drug Targets. 16 (5): 474–83. doi:10.2174/1389450115666141111111842. PMC 4430197. PMID 25392014.
- Latoni, J.; Shivapuja, B.; Seidman, M. D.; Quirk, W. S. (May 1996). "Pentoxifylline maintains cochlear microcirculation and attenuates temporary threshold shifts following acoustic overstimulation". Acta Oto-Laryngologica. 116 (3): 388–94. doi:10.3109/00016489609137862. PMID 8790737.
- El-Sakka, A. I. (2011). "Reversion of penile fibrosis: Current information and a new horizon". Arab Journal of Urology. 9 (1): 49–55. doi:10.1016/j.aju.2011.03.013. PMC 4149188. PMID 26579268.
- Delanian, S., Chatel, C., Porcher, R., Depondt, J. and Lefaix, J.L., 2011. Complete restoration of refractory mandibular osteoradionecrosis by prolonged treatment with a pentoxifylline-tocopherol-clodronate combination (PENTOCLO): a phase II trial. International Journal of Radiation Oncology* Biology* Physics, 80(3), pp.832-839.
- Patel, V., Gadiwalla, Y., Sassoon, I., Sproat, C., Kwok, J. and McGurk, M., 2016. Prophylactic use of pentoxifylline and tocopherol in patients who require dental extractions after radiotherapy for cancer of the head and neck. British Journal of Oral and Maxillofacial Surgery, 54(5), pp.547-550.
- Salhiyyah, Kareem; Forster, Rachel; Senanayake, Eshan; Abdel-Hadi, Mohammed; Booth, Andrew; Michaels, Jonathan A (2015-09-29). "Pentoxifylline for intermittent claudication". Cochrane Database of Systematic Reviews. 9 (9): CD005262. doi:10.1002/14651858.cd005262.pub3. ISSN 1465-1858. PMC 6513423. PMID 26417854.