Osteoprotegerin
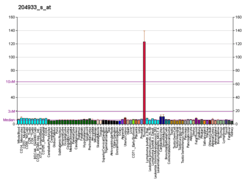
Osteoprotegerin (OPG), also known as osteoclastogenesis inhibitory factor (OCIF) or tumour necrosis factor receptor superfamily member 11B (TNFRSF11B), is a cytokine receptor of the tumour necrosis factor (TNF) receptor superfamily encoded by the TNFRSF11B gene.
OPG was first discovered as a novel secreted TNFR related protein that played a role in the regulation of bone density and later for its role as a decoy receptor for Receptor Activator of Nuclear Factor kappa-B ligand (RANKL).[5] OPG also binds to TNF-related apoptosis-inducing ligand (TRAIL) and inhibits TRAIL induced apoptosis of specific cells, including tumour cells.[6] Other OPG ligands include syndecan-1, glycosaminoglycans, von Willebrand Factor, and Factor VIII-von Willebrand Factor complex.[7]
OPG has been identified as having a role in tumour growth and metastasis,[6] heart disease,[8][9][10] immune system development and signalling,[7] mental health,[11] diabetes,[12] and the prevention of pre-eclampsia[13] and osteoporosis during pregnancy.[14]
Biochemistry
OPG is largely expressed by osteoblast lineage cells of bone, epithelial cells of the gastrointestinal tract, lung, breast and skin,[7][15] vascular endothelial cells,[16] as well as B-cells and dendritic cells in the immune system.[16]
OPG is a soluble glycoprotein which can be found as either a 60-kDa monomer or a 120-kDa dimer linked by disulfide bonds.[17] The dimerisation of OPG is necessary for RANK-RANKL inhibition as dimerisation increases the affinity of OPG for RANKL (from a KD of 3µM as a monomer to 10nM as a dimer).[17] As a monomer, OPG would have insufficient affinity for RANKL to compete with RANK and effectively suppress RANK-RANKL interactions.
OPG proteins are made up of 380 amino acids which form seven functional domains.[7] Domains 1-4 are cysteine-rich N-terminal domains that interact with RANKL during binding.[17] Domains 5-6 are death domains that contribute to the dimerisation of OPG.[17] Domain 7 is a C-terminal heparin-binding domain ending with a cysteine (Cys-400) which also plays an important role in the dimerisation of OPG.[17][7]
OPG expression can be upregulated by IL-1β,[18][19] 1α,25(OH)2D3,[18] Wnt/β-catenin signalling through Wnt16, Wnt4 and Wnt3a[20] TNFα[6] and estrogen.[21] OPG expression can also be upregulated transcriptionally through DNA binding sites for estrogen receptor α (ER-α)[21] and TCF[22] in the promoter region of the OPG gene. Downregulation of OPG can be effected by TGF-β1,[18] PTH[23] and DNA methylation of a CpG island in the OPG gene.[24]
Estrogen and OPG regulation
OPG expression in osteoblast lineage cells is highly regulated by estrogens such as estradiol (E2).[21][25] E2 transcriptionally regulates OPG expression through binding estrogen receptors (predominantly ER-α) on osteoblast lineage cell surfaces.[21] The E2-ERα complex then translocates into the cell nucleus where it binds an estrogen response element in the promoter region of the OPG gene to upregulate OPG mRNA transcription.[21]
Estrogens can also post-transcriptionally regulate OPG protein expression through the suppression of the microRNA (miRNA) miR-145.[26] miR-145 binds miRNA binding sites in the 3’UTR of OPG mRNA transcripts and suppresses the translation of OPG proteins.[26] Estrogen binds its ER-β receptor on the cell surface to suppress many miRNAs, including miR-145,[27] thus blocking inhibition of OPG mRNA translation.[28]
Estrogen suppresses osteoclastogenesis through the upregulation of OPG expression in osteoblast lineage cells.[25] Androgens such as testosterone and DHT also inhibit osteoclastogenesis, however androgens act directly through androgen receptors on osteoclast precursor cells without affecting OPG expression in osteoblasts.[25] Further, in the absence of aromatase enzymes converting testosterone into estrogen, testosterone and DHT downregulate OPG mRNA expression.[29][30]
Function
OPG plays an important role in bone metabolism as a decoy receptor for RANKL in the RANK/RANKL/OPG axis, inhibiting osteoclastogenesis and bone resorption.[5] OPG has also been shown to bind and inhibit TNF-related apoptosis-inducing ligand (TRAIL) which is responsible for inducing apoptosis in tumour, infected and mutated cells.[10]
Bone metabolism
The RANK/RANKL/OPG axis is a critical pathway in maintaining the symbiosis between bone resorption by osteoclasts and bone formation by osteoblasts.[31] RANKL is released by osteoblast lineage cells and binds to receptor RANK on the surface of osteoclast progenitor cells[32] RANK-RANKL binding activates the nuclear factor kappa B (NF-κB) pathway resulting in the upregulation of the transcription factor nuclear factor of activated T-cells cytoplasmic 1 (NFATc1).[33] NFATc1 is a master regulator for the expression of essential cytokines during the differentiation of osteoclast precursor cells into mature osteoclasts, known as osteoclastogenesis.[34] Mature osteoclasts then bind to bone through tight junctions and release digestive enzymes to resorb the old bone.[32] As bone is resorbed, collagen and minerals are released into the local microenvironment creating both the space and minerals needed for osteoblasts to lay down new bone.[31] As a decoy receptor for RANKL, OPG inhibits RANK-RANKL interactions thus suppressing osteoclastogenesis and bone resorption.[32]
OPG is also a decoy receptor for TRAIL, another regulator of osteoclastogenesis in osteoclast precursor cells [35] and an autocrine signal for mature osteoclast cell death.[36] TRAIL induces osteoclastogenesis by binding to specific TRAIL receptors on osteoclast precursor cell surfaces, inducing TRAF6 signalling, activating NF-κB signalling and upregulating NFATc1 expression.[36] During osteoclastogenesis the different TRAIL receptors on the cell surface change resulting in an increase of apoptosis inducing TRAIL receptors expressed on mature osteoclasts.[37] As a decoy receptor for both RANKL and TRAIL, OPG simultaneously suppresses osteoclastogenesis while also inhibiting TRAIL induced cell death of mature osteoclast cells. OPG has an equally high affinity for RANKL and TRAIL[38] suggesting that it is equally effective at inducing osteoclastogenesis and inhibiting osteoclast apoptosis.
Disease
Atrophic nonunion shaft fractures
A normal steady state of bone metabolism seems to be present in patients with atrophic nonunion fractures, despite the high serum OPG. Only serum OPG was significantly higher in the patients compared to healed and healing controls. (49)
Osteoporosis
Osteoporosis is a bone-related disease caused by increased rates of bone resorption compared to bone formation.[39] A higher rate of resorption is often caused by increased osteoclastogenesis and results in symptoms of osteopenia such as excessive bone loss and low bone mineral density.[39]
Osteoporosis is often triggered in post-menopausal women due to reduced estrogen levels associated with the depletion of hormone-releasing ovarian follicles.[40] Decreasing estrogen levels result in the downregulation of OPG expression and reduced inhibition of RANKL. Therefore RANKL can more readily bind to RANK and cause the increased osteoclastogenesis and bone resorption seen in osteoporosis.[21][26] Decreased estrogen is a common cause of osteoporosis that can be seen in other conditions such as ovariectomy, ovarian failure, anorexia, and hyperprolactinaemia.[41]
Osteoblastic synthesis of bone does not increase to compensate for the accelerated bone resorption as the lower estrogen levels result in increased rates of osteoblast apoptosis.[42] The higher rate of bone resorption compared to bone formation leads to the increased porosity and low bone mineral density of individuals with osteoporosis.
Cancer
Tumour endothelial cells have been found to express higher levels of OPG when compared to normal endothelial cells.[6] When in contact with tumour cells, endothelial cells express higher levels of OPG in response to integrin αvβ3 ligation and the stimulation of NF-kB signalling.[6]
OPG expression has been found to promote tumour growth and survival through driving tumour vascularisation and inhibiting TRAIL-induced apoptosis.[6]
OPG has been identified as one of the many pro-angiogenic factors involved in the vascularisation of tumours.[6] Tumour angiogenesis is required for tumour growth and movement as it supplies the tumour with nutrients and allows metastatic cells to enter the bloodstream.[6] As a decoy receptor for TRAIL, OPG also promotes tumour cell survival by inhibiting TRAIL-induced apoptosis of tumour cells.[6]
Bone metastasis
Bone is a common site of metastasis in cancers such as breast, prostate and lung cancer.[43] In osteolytic bone metastases, tumour cells migrate to the bone and release cytokines such as parathyroid hormone-related protein (PTHrP), IL-8 and PGE2.[44] These cytokines act on osteoblasts to increase RANKL and decrease OPG expression resulting in excess bone resorption.[44] During resorption osteoclasts release nutrients such as growth factors and calcium from the mineralised bone matrix which cultivates a supportive environment for the proliferation and survival of tumour cells.[43]
Most bone metastases result in osteolytic lesions, however prostate cancer causes osteoblastic lesions characterised by excess bone formation and high bone density.[44] Prostate cancer releases cytokines such as insulin-like growth factor (IGF), endothelin-1, bone morphogenetic proteins (BMPs), sclerostin and Wnt proteins that act on local bone to increase osteoblast proliferation and activity.[44] Wnt proteins also act on osteoblasts to upregulate OPG expression through β-catenin signalling and suppress osteoclastic bone resorption.[44]
Multiple myeloma
Multiple myeloma is a type of cancer involving malignant plasma cells, called myeloma cells, within the bone marrow.[45] Multiple myeloma is associated with osteolytic bone lesions as the usually high levels of OPG in the bone marrow are diminished resulting in increased osteoclastic absorption.[16] The reduced OPG in multiple myeloma is caused by suppression of both constitutive OPG transcription and the OPG inducing cytokines TGF-β[16] and Wnt.[45] In addition, the efficacy of OPG in bone marrow is impeded with multiple myeloma by excessive binding to syndecan-1.[16] OPG binds to syndecan-1 on the surface of normal and multiple myeloma plasma cells to be internalised and degraded.[46][47] However the overabundance of proliferating myeloma cells results in the excessive binding and inhibition of OPG by syndecan-1.[47] Simultaneously, multiple myeloma is associated with unusually high levels of osteoclastogenesis-inducing factors.[16] The decreased OPG transcription and increased OPG protein degradation combined with increased osteoclastogenesis result in the osteolytic lesions that are characteristic of multiple myeloma.
Juvenile Paget's disease
This is a rare autosomal recessive disease that is associated with mutations in this gene.[48]
References
- GRCh38: Ensembl release 89: ENSG00000164761 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000063727 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Lüthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ (April 1997). "Osteoprotegerin: a novel secreted protein involved in the regulation of bone density". Cell. 89 (2): 309–19. doi:10.1016/s1525-0016(16)39531-4. PMID 9108485.
- Reid PE, Brown NJ, Holen I (July 2009). "Breast cancer cells stimulate osteoprotegerin (OPG) production by endothelial cells through direct cell contact". Molecular Cancer. 8 (1): 49. doi:10.1186/1476-4598-8-49. PMC 2719583. PMID 19604388.
- Baud'huin M, Duplomb L, Teletchea S, Lamoureux F, Ruiz-Velasco C, Maillasson M, Redini F, Heymann MF, Heymann D (October 2013). "Osteoprotegerin: multiple partners for multiple functions" (PDF). Cytokine & Growth Factor Reviews. 24 (5): 401–9. doi:10.1016/j.cytogfr.2013.06.001. PMID 23827649.
- Xi L, Cao H, Chen Y (2013). "OPG/RANK/RANKL axis in atrial fibrillation". Cardiology. 125 (3): 174–5. doi:10.1159/000351441. PMID 23752030.
- Hosbond SE, Poulsen TS, Diederichsen AC, Nybo M, Rasmussen LM, Mickley H (August 2012). "Osteoprotegerin as a marker of atherosclerosis: a systematic update". Scandinavian Cardiovascular Journal. 46 (4): 203–11. doi:10.3109/14017431.2012.685491. PMID 22506827.
- Bernardi S, Bossi F, Toffoli B, Fabris B (2016). "Roles and Clinical Applications of OPG and TRAIL as Biomarkers in Cardiovascular Disease". BioMed Research International. 2016: 1752854. doi:10.1155/2016/1752854. PMC 4856888. PMID 27200369.
- Hope S, Melle I, Aukrust P, Agartz I, Lorentzen S, Steen NE, Djurovic S, Ueland T, Andreassen OA (September 2010). "Osteoprotegerin levels in patients with severe mental disorders". Journal of Psychiatry & Neuroscience. 35 (5): 304–10. doi:10.1503/jpn.090088. PMC 2928283. PMID 20569643.
- Nabipour I, Kalantarhormozi M, Larijani B, Assadi M, Sanjdideh Z (May 2010). "Osteoprotegerin in relation to type 2 diabetes mellitus and the metabolic syndrome in postmenopausal women". Metabolism. 59 (5): 742–7. doi:10.1016/j.metabol.2009.09.019. PMID 19922962.
- Shen P, Gong Y, Wang T, Chen Y, Jia J, Ni S, Zhou B, Song Y, Zhang L, Zhou R (2012). "Expression of osteoprotegerin in placenta and its association with preeclampsia". PLOS ONE. 7 (8): e44340. doi:10.1371/journal.pone.0044340. PMC 3431377. PMID 22952959.
- Yano K, Shibata O, Mizuno A, Kobayashi F, Higashio K, Morinaga T, Tsuda E (October 2001). "Immunological study on circulating murine osteoprotegerin/osteoclastogenesis inhibitory factor (OPG/OCIF): possible role of OPG/OCIF in the prevention of osteoporosis in pregnancy". Biochemical and Biophysical Research Communications. 288 (1): 217–24. doi:10.1006/bbrc.2001.5745. PMID 11594776.
- Fortner RT, Sarink D, Schock H, Johnson T, Tjønneland A, Olsen A, Overvad K, Affret A, His M, Boutron-Ruault MC, Boeing H, Trichopoulou A, Naska A, Orfanos P, Palli D, Sieri S, Mattiello A, Tumino R, Ricceri F, Bueno-de-Mesquita HB, Peeters PH, Van Gils CH, Weiderpass E, Lund E, Quirós JR, Agudo A, Sánchez MJ, Chirlaque MD, Ardanaz E, Dorronsoro M, Key T, Khaw KT, Rinaldi S, Dossus L, Gunter M, Merritt MA, Riboli E, Kaaks R (February 2017). "Osteoprotegerin and breast cancer risk by hormone receptor subtype: a nested case-control study in the EPIC cohort". BMC Medicine. 15 (1): 26. doi:10.1186/s12916-017-0786-8. PMC 5297136. PMID 28173834.
- Sordillo EM, Pearse RN (February 2003). "RANK-Fc: a therapeutic antagonist for RANK-L in myeloma". Cancer. 97 (3 Suppl): 802–12. doi:10.1002/cncr.11134. PMID 12548579.
- Schneeweis LA, Willard D, Milla ME (December 2005). "Functional dissection of osteoprotegerin and its interaction with receptor activator of NF-kappaB ligand". The Journal of Biological Chemistry. 280 (50): 41155–64. doi:10.1074/jbc.M506366200. PMID 16215261.
- Jurado S, Garcia-Giralt N, Díez-Pérez A, Esbrit P, Yoskovitz G, Agueda L, Urreizti R, Pérez-Edo L, Saló G, Mellibovsky L, Balcells S, Grinberg D, Nogués X (May 2010). "Effect of IL-1beta, PGE(2), and TGF-beta1 on the expression of OPG and RANKL in normal and osteoporotic primary human osteoblasts". Journal of Cellular Biochemistry. 110 (2): 304–10. doi:10.1002/jcb.22538. PMID 20225238.
- Chung ST, Geerts D, Roseman K, Renaud A, Connelly L (February 2017). "Osteoprotegerin mediates tumor-promoting effects of Interleukin-1beta in breast cancer cells". Molecular Cancer. 16 (1): 27. doi:10.1186/s12943-017-0606-y. PMC 5286681. PMID 28143606.
- Kobayashi Y, Thirukonda GJ, Nakamura Y, Koide M, Yamashita T, Uehara S, Kato H, Udagawa N, Takahashi N (August 2015). "Wnt16 regulates osteoclast differentiation in conjunction with Wnt5a". Biochemical and Biophysical Research Communications. 463 (4): 1278–83. doi:10.1016/j.bbrc.2015.06.102. PMID 26093292.
- Millán MM (2015). "The Role of Estrogen Receptor in Bone Cells". Clinical Reviews in Bone and Mineral Metabolism. 13 (2): 105–112. doi:10.1007/s12018-015-9188-7.
- Bilezikian JP, Raisz LG, Martin TJ (2008). Principles of Bone Biology (3rd ed.). San Diego, CA: Academic Press. ISBN 9780123738844.
- Szulc P, Hofbauer LC, Heufelder AE, Roth S, Delmas PD (July 2001). "Osteoprotegerin serum levels in men: correlation with age, estrogen, and testosterone status". The Journal of Clinical Endocrinology and Metabolism. 86 (7): 3162–5. doi:10.1210/jcem.86.7.7657. PMID 11443182.
- Delgado-Calle J, Sañudo C, Fernández AF, García-Renedo R, Fraga MF, Riancho JA (January 2012). "Role of DNA methylation in the regulation of the RANKL-OPG system in human bone". Epigenetics. 7 (1): 83–91. doi:10.4161/epi.7.1.18753. PMC 3337833. PMID 22207352.
- Michael H, Härkönen PL, Väänänen HK, Hentunen TA (December 2005). "Estrogen and testosterone use different cellular pathways to inhibit osteoclastogenesis and bone resorption". Journal of Bone and Mineral Research. 20 (12): 2224–32. doi:10.1359/JBMR.050803. PMID 16294275.
- Jia J, Zhou H, Zeng X, Feng S (April 2017). "Estrogen stimulates osteoprotegerin expression via the suppression of miR-145 expression in MG-63 cells". Molecular Medicine Reports. 15 (4): 1539–1546. doi:10.3892/mmr.2017.6168. PMC 5364970. PMID 28260003.
- Piperigkou Z, Franchi M, Götte M, Karamanos NK (December 2017). "Estrogen receptor beta as epigenetic mediator of miR-10b and miR-145 in mammary cancer". Matrix Biology. 64: 94–111. doi:10.1016/j.matbio.2017.08.002. PMID 28797712.
- Cohen A, Burgos-Aceves MA, Kahan T, Smith Y (August 2017). "Estrogen Repression of MicroRNAs Is Associated with High Guanine Content in the Terminal Loop Sequences of Their Precursors". Biomedicines. 5 (3): 47–57. doi:10.3390/biomedicines5030047. PMC 5618305. PMID 28805722.
- Hofbauer LC, Hicok KC, Chen D, Khosla S (August 2002). "Regulation of osteoprotegerin production by androgens and anti-androgens in human osteoblastic lineage cells". European Journal of Endocrinology. 147 (2): 269–73. doi:10.1530/eje.0.1470269. PMID 12153751.
- Khosla S, Atkinson EJ, Dunstan CR, O'Fallon WM (April 2002). "Effect of estrogen versus testosterone on circulating osteoprotegerin and other cytokine levels in normal elderly men". The Journal of Clinical Endocrinology and Metabolism. 87 (4): 1550–4. doi:10.1210/jcem.87.4.8397. PMID 11932280.
- Boyce BF, Xing L (May 2008). "Functions of RANKL/RANK/OPG in bone modeling and remodeling". Archives of Biochemistry and Biophysics. 473 (2): 139–46. doi:10.1016/j.abb.2008.03.018. PMC 2413418. PMID 18395508.
- Boyle WJ, Simonet WS, Lacey DL (May 2003). "Osteoclast differentiation and activation". Nature. 423 (6937): 337–42. doi:10.1038/nature01658. PMID 12748652.
- Boyce BF, Xiu Y, Li J, Xing L, Yao Z (March 2015). "NF-κB-Mediated Regulation of Osteoclastogenesis". Endocrinology and Metabolism. 30 (1): 35–44. doi:10.3803/EnM.2015.30.1.35. PMC 4384681. PMID 25827455.
- Kim JH, Kim N (November 2014). "Regulation of NFATc1 in Osteoclast Differentiation". Journal of Bone Metabolism. 21 (4): 233–41. doi:10.11005/jbm.2014.21.4.233. PMC 4255043. PMID 25489571.
- Yen ML, Hsu PN, Liao HJ, Lee BH, Tsai HF (2012). "TRAF-6 dependent signaling pathway is essential for TNF-related apoptosis-inducing ligand (TRAIL) induces osteoclast differentiation". PLOS ONE. 7 (6): e38048. doi:10.1371/journal.pone.0038048. PMC 3375273. PMID 22719861.
- Chamoux E, Houde N, L'Eriger K, Roux S (August 2008). "Osteoprotegerin decreases human osteoclast apoptosis by inhibiting the TRAIL pathway". Journal of Cellular Physiology. 216 (2): 536–42. doi:10.1002/jcp.21430. PMID 18338379.
- Colucci S, Brunetti G, Cantatore FP, Oranger A, Mori G, Pignataro P, Tamma R, Grassi FR, Zallone A, Grano M (September 2007). "The death receptor DR5 is involved in TRAIL-mediated human osteoclast apoptosis". Apoptosis. 12 (9): 1623–32. doi:10.1007/s10495-007-0095-3. PMID 17558561.
- Vitovski S, Phillips JS, Sayers J, Croucher PI (October 2007). "Investigating the interaction between osteoprotegerin and receptor activator of NF-kappaB or tumor necrosis factor-related apoptosis-inducing ligand: evidence for a pivotal role for osteoprotegerin in regulating two distinct pathways". The Journal of Biological Chemistry. 282 (43): 31601–9. doi:10.1074/jbc.M706078200. PMID 17702740.
- Snyman, L (2014). "Menopause-related osteoporosis". South African Family Practice. 56 (3): 174–177. doi:10.1080/20786204.2014.932549. hdl:2263/41558.
- Nelson HD (March 2008). "Menopause". Lancet. 371 (9614): 760–70. doi:10.1016/S0140-6736(08)60346-3. PMID 18313505.
- Meczekalski B, Podfigurna-Stopa A, Genazzani AR (September 2010). "Hypoestrogenism in young women and its influence on bone mass density". Gynecological Endocrinology. 26 (9): 652–7. doi:10.3109/09513590.2010.486452. PMID 20504098.
- Bradford PG, Gerace KV, Roland RL, Chrzan BG (February 2010). "Estrogen regulation of apoptosis in osteoblasts". Physiology & Behavior. 99 (2): 181–5. doi:10.1016/j.physbeh.2009.04.025. PMC 2825744. PMID 19426747.
- Dougall WC (January 2012). "Molecular pathways: osteoclast-dependent and osteoclast-independent roles of the RANKL/RANK/OPG pathway in tumorigenesis and metastasis". Clinical Cancer Research. 18 (2): 326–35. doi:10.1158/1078-0432.CCR-10-2507. PMID 22031096.
- Bertoldo F (2017). "Biology and Pathophysiology of Bone Metastasis in Prostate Cancer". In Bertoldo F, Boccardo F, Bombardieri E, Evangelista L, Valdagni R (eds.). Bone Metastases from Prostate Cancer: Biology, Diagnosis and Management. Cham, Switzerland: Springer International Publishing. ISBN 978-3-319-42326-5.
- Palumbo A, Anderson K (March 2011). "Multiple myeloma". The New England Journal of Medicine. 364 (11): 1046–60. doi:10.1056/NEJMra1011442. PMID 21410373.
- Renema N, Navet B, Heymann MF, Lezot F, Heymann D (August 2016). "RANK-RANKL signalling in cancer". Bioscience Reports. 36 (4): e00366. doi:10.1042/BSR20160150. PMC 4974605. PMID 27279652.
- Standal T, Seidel C, Hjertner Ø, Plesner T, Sanderson RD, Waage A, Borset M, Sundan A (October 2002). "Osteoprotegerin is bound, internalized, and degraded by multiple myeloma cells". Blood. 100 (8): 3002–7. doi:10.1182/blood-2002-04-1190. PMID 12351414.
- Naot D, Wilson LC, Allgrove J, Adviento E, Piec I, Musson DS, Cundy T, Calder AD (2019). "Juvenile Paget's disease with compound heterozygous mutations in TNFRSF11B presenting with recurrent clavicular fractures and a mild skeletal phenotype". Bone. 130: 115098. doi:10.1016/j.bone.2019.115098.
External links
- Osteoprotegerin at the US National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: O00300 (Human Tumor necrosis factor receptor superfamily member 11B) at the PDBe-KB.
- Overview of all the structural information available in the PDB for UniProt: O08712 (Mouse Tumor necrosis factor receptor superfamily member 11B) at the PDBe-KB.