Healthcare in Canada
Healthcare in Canada is delivered through the provincial and territorial systems of publicly funded health care, informally called Medicare.[1][2] It is guided by the provisions of the Canada Health Act of 1984,[3] and is universal.[4] Universal access to publicly funded health services is often considered by Canadians as a "fundamental value that ensures national health care insurance for everyone wherever they live in the country."[5] Canadian Medicare provides coverage for approximately 70 percent of Canadians' healthcare needs, and the remaining 30 percent is paid for through the private sector.[6] The 30 percent typically relates to services not covered or only partially covered by Medicare, such as prescription drugs, dentistry and optometry.[6] Approximately 65 to 75 percent of Canadians have some form of supplementary health insurance related to the aforementioned reasons; many receive it through their employers or use secondary social service programs related to extended coverage for families receiving social assistance or vulnerable demographics, such as seniors, minors, and those with disabilities.[7][6]
| Part of series on |
| Healthcare in Canada |
|---|
 |
| Health Canada |
| History of medicine |
| Topics |
| Canada portal |
In common with many other developed countries, Canada is experiencing a cost increase due to a demographic shift towards an older population, with more retirees and fewer people of working age. In 2006, the average age was 39.5 years;[8] within twelve years it had risen to 42.4 years,[9] with a life expectancy of 81.1 years.[10] A 2016 report by the Chief Public Health Officer of Canada found that three in five Canadians, one of the highest proportions of the population among G7 countries, indicated that they "had good or very good health".[11] 80 percent of Canadian adults self-report having at least one major risk factor for chronic disease; smoking, physical inactivity, unhealthy eating or excessive alcohol use.[12] Canada has one of the highest rates of adult obesity among Organisation for Economic Co-operation and Development (OECD) countries attributing to approximately 2.7 million cases of diabetes (types 1 and 2 combined).[12] Four chronic diseases—cancer (leading cause of death), cardiovascular diseases, respiratory diseases and diabetes account for 65 percent of deaths in Canada.[12]
In 2017, the Canadian Institute for Health Information reported that healthcare spending was $242 billion, or 11.5 percent of Canada's gross domestic product (GDP) for that year.[13] In 2019, Canada' per-capita spending on health expenditures ranked 11th among health-care systems in the OECD.[14] Canada has performed close to, or above the average on the majority of OECD health indicators since the early 2000s.[15] In 2017 Canada ranked above the average on OECD indicators for wait-times and access to care, with average scores for quality of care and use of resources.[16] A comprehensive study from 2017 of the top 11 countries ranked Canada's health care system ninth.[17] Identified weaknesses of Canada's system were comparatively higher infant mortality rate, the prevalence of chronic conditions, long wait times, poor availability of after-hours care, and a lack of prescription drugs and dental coverage.[17]
Current status
The government guarantees the quality of care through federal standards. The government does not participate in day-to-day care or collect any information about an individual's health, which remains confidential between a person and their physician.[18] Canada's provincially-based Medicare systems are cost-effective because of their administrative simplicity. In each province, each doctor handles the insurance claim against the provincial insurer. There is no need for the person who accesses healthcare to be involved in billing and reclaim. Private health expenditure accounts for 30% of health care financing.[19]
The Canada Health Act does not cover prescription drugs, home care or long-term care or dental care.[18] Provinces provide partial coverage for children, those living in poverty and seniors.[18] Programs vary by province. In Ontario, for example, most prescriptions for youths under the age of 24 are covered by the Ontario health insurance plan if no private insurance plan is available.[20]
Competitive practices such as advertising are kept to a minimum, thus maximizing the percentage of revenues that go directly towards care. Costs are paid through funding from federal and provincial general tax revenues which include income taxes, sales taxes and corporate taxes. In British Columbia, taxation-based funding was (until January 1, 2020) supplemented by a fixed monthly premium which is waived or reduced for those on low incomes.[21] In Ontario, there is an income tax identified as a health premium on taxable income above $20,000.[22]
In addition to funding through the tax system, hospitals and medical research are funded in part by charitable contributions. For example, in 2018, Toronto's Hospital for Sick Children embarked on campaign to raise $1.3 billion to equip a new hospital.[23] Charities such as the Canadian Cancer Society provide assistance such as transportation for patients.[24] There are no deductibles on basic health care and co-pays are extremely low or non-existent (supplemental insurance such as Fair Pharmacare may have deductibles, depending on income). In general, user fees are not permitted by the Canada Health Act, but physicians may charge a small fee to the patient for reasons such as missed appointments, doctor's notes and prescription refills done over the phone. Some physicians charge "annual fees" as part of a comprehensive package of services they offer their patients and their families. Such charges are completely optional and can only be for non-essential health options.[18]
Benefits and features
Health cards are issued by provincial health ministries to individuals who enroll for the program in the province and everyone receives the same level of care.[25] There is no need for a variety of plans because virtually all essential basic care is covered, including maternity but excluding mental health and home care.[26] Infertility costs are not covered in any province other than Quebec, though they are now partially covered in some other provinces.[27] In some provinces, private supplemental plans are available for those who desire private rooms if they are hospitalized. Cosmetic surgery and some forms of elective surgery are not considered essential care and are generally not covered. For example, Canadian health insurance plans do not cover non-therapeutic circumcision.[28] These can be paid out-of-pocket or through private insurers.
Health coverage is not affected by loss or change of jobs, cannot be denied due to unpaid premiums, and there are no lifetime limits or exclusions for pre-existing conditions. The Canada Health Act deems that essential physician and hospital care be covered by the publicly funded system, but each province has reasons to determine what is considered essential, and where, how and who should provide the services. There are some provinces that are moving towards Private Health Care away from Public Health Care. The result is that there is a wide variance in what is covered across the country by the public health system, particularly in more controversial areas, such as in-vitro fertilization,[29] sex reassignment surgery,[30] midwifery or autism treatments.[18]
Canada (with the exception of the province of Quebec) is one of the few countries with a universal healthcare system that does not include coverage of prescription medication (other such countries are Russia and some of the former USSR republics[31]). Residents of Quebec who are covered by the province's public prescription drug plan pay an annual premium of $0 to $660 when they file their Quebec income tax return.[32][33]
Due to changes in the past two decades, at least some provinces have introduced some universal prescription drug insurance. Nova Scotia has Family Pharmacare, introduced in 2008 by Rodney MacDonald's Progressive Conservative government.[34] However, residents do not automatically receive it through their health care as they must register separately for it, and it covers a limited range of prescriptions. No premiums are charged. A deductible and out-of-pocket maximum for copayments are set as a percentage of taxable income of two years before.[35]
Pharmaceutical medications are covered by public funds in some provinces for the elderly or indigent,[36] or through employment-based private insurance or paid for out-of-pocket. In Ontario, eligible medications are provided at no cost for covered individuals aged 24 and under.[37] Most drug prices are negotiated with suppliers by each provincial government to control costs but more recently, the Council of the Federation announced an initiative for select provinces to work together to create a larger buying block for more leverage to control costs of pharmaceutical drugs.[38] More than 60 percent of prescription medications are paid for privately in Canada.[18] Family physicians ("General Practitioners") are chosen by individuals. If a patient wishes to see a specialist or is counseled to see a specialist by their GP, a referral is made by a GP in the local community. Preventive care and early detection are considered critical and yearly checkups are recommended for everyone.
Coverage
Mental health
The Canada Health Act covers the services of psychiatrists, medical doctors with additional training in psychiatry. In Canada, psychiatrists tend to focus on the treatment of mental illness with medication.[39] However, the Canada Health Act excludes care provided in a "hospital or institution primarily for the mentally disordered."[40] Some institutional care is provided by provinces. The Canada Health Act does not cover treatment by a psychologist[41][42] or psychotherapist unless the practitioner is also a medical doctor. Goods and Services Tax or Harmonized Sales Tax (depending on the province) applies to the services of psychotherapists.[43] Some coverage for mental health care and substance abuse treatment may be available under other government programs. For example, in Alberta, the province provides funding for mental health care through Alberta Health Services.[44] Most or all provinces and territories offer government-funded drug and alcohol addiction rehabilitation, although waiting lists may exist.[45] The cost of treatment by a psychologist or psychotherapist in Canada has been cited as a contributing factor in the high suicide rate among first responders such as police officers, EMTs and paramedics. According to a CBC report, some police forces "offer benefits plans that cover only a handful of sessions with community psychologists, forcing those seeking help to join lengthy waiting lists to seek free psychiatric assistance."[46]
Oral health
It is said that among the OECD countries, Canada ranks approximately second to last in the public funding of oral healthcare. Those who need dental care are usually responsible for the finances and some may benefit from the coverage available through employment, under provincial plans, or private dental care plans. "As opposed to its national system of public health insurance, dental care in Canada is almost wholly privately financed, with approximately 60% of dental care paid through employment-based insurance, and 35% through out-of-pocket expenditures [7,8]. Of the approximately 5% of publicly financed care that remains, most has focused on socially marginalized groups (e.g., low-income children and adults), and is supported by different levels of government depending on the group insured [9]."[47] It is true that compared to primary care checkups, dental care checkups are highly relied on the ability of people being able to pay those fees. While viewing studies done in the cities of Quebec as well as Ontario a few interesting facts were seen. For example, studies in Quebec showed that there was a strong relation among dental services and the socioeconomic factors of income and education whereas in Ontario older adults heavily relied on dental insurance with visits to the dentist. "According to the National Public Health Service in 1996/1997, it showed a whopping difference of people who were in different classes. About half of Canadians aged 15 or older (53%) reported having dental insurance (Table 1). Coverage tended to be highest among middle-aged people. At older ages, the rate dropped, and only one-fifth of the 65-or-older age group (21%) was covered."[48] Attributes that can contribute to these outcomes is household income, employment, as well as education. Those individuals who are in the middle class may be covered through the benefits of their employment whereas older individuals may not due to the fact of retirement.
Physiotherapy, occupational therapy, and massage therapy
Coverage for services by physiotherapists, occupational therapists (also known as OTs) and Registered Massage Therapists (RMTs) varies by province. For example, in Ontario the provincial health plan, OHIP, does cover physiotherapy following hospital discharge and occupational therapy[49] but does not cover massage therapy. To be eligible for coverage for physiotherapy in Ontario, the insured individual has to have been discharged as an inpatient of a hospital after an overnight stay and require physiotherapy for the condition, illness or injury for which he or she was hospitalized, or be age 19 or younger or age 65 or older.[50]
Other coverage limitations
Coverage varies for care related to the feet. In Ontario, as of 2019, Medicare covers between $7–16 of each visit to a registered podiatrist up to $135 per patient per year, plus $30 for x-rays.[51] Although the elderly, as well as diabetic patients, may have needs that greatly exceed that limit, such costs would have to be covered by patients or private supplemental insurance.
As of 2014, most, but not all provinces and territories provide coverage for sex reassignment surgery (also known as gender confirming surgery) and other treatment for gender dysphoria.[52] In Ontario, sex reassignment surgery requires prior approval before being covered.[53]
There are wide discrepancies in coverage for various assistive devices such as wheelchairs and respiratory equipment in Canada. Ontario, which has one of the most generous programs, pays 75% of the cost for listed equipment and supplies for persons with a disability requiring such equipment or supplies for six months or longer.[54] The program does not have age or income restrictions. As with other health coverage, veterans and others covered by federal programs are not eligible under the provincial program. Only certain types of equipment and supplies are covered, and within categories only approved models of equipment from approved vendors are covered, and vendors may not charge more than specified prices established by the government.[55]
Coverage for seniors
As people grow older the need for care tends to grow stronger and the need for a well-rounded healthcare plan rises. Because Canada's public policies come from the federal government as well as the provincial governments, these two need to work together to create a beneficial healthcare plan. There are quite a few plans in which one, 65 years of age or older, can apply for to ensure they are covered. These include: Old Age Security (OAS), Guaranteed Income Supplement (GIS), Allowance and, Canada Pension Plan (CPP). The OAS is one in which citizens who have lived in Canada for 10 or more years and are age 65 or older can apply for. Those who have received the benefit of OAS and have a low income can then apply for the GIS. If a person has received the GIS, their spouse between the ages of 60–64 can apply for Allowance. Moving along, those who are in the workforce tend to put money aside for the Canada Pension Plan (CPP) by the time they reach age 65. The CPP is essentially a social insurance program preparing individuals for retirement. To those who obtain the CPP, they receive the benefit of the plan paying for things such as retirement, disability, children's benefits, and more. "You must apply for OAS, GIS, the Allowance, CPP and other federal programs. You will not receive them automatically."[56] Although there are these beneficial plans, the need for a better plan of action for seniors is in effect. Out of the approximately 39 million people in Canada, roughly 6 million of these people consist of seniors. "Given these challenges, it is not surprising that nine in ten (90%) Canadians agree that Canada requires a national seniors strategy to address needs along the full continuum of care."[57] In order to ensure maximum coverage of the elderly a few things need to be in order. For starters, having a shorter wait time for these seniors. As individuals grow older the more care is needed to ensure a healthy body and lifestyle and wait times can put a damper on this. Next, having specialized physicians who are knowledgeable in handling seniors in a gentle and well-equipped way. "Restrictions on government funding has limited access to care—wait-lists are routine, and Canadians are increasingly having difficulties accessing the services of family physicians. The system has not kept up with the demands and expectations of the patient."[58] This puts stress on those seniors and the need to ensure everyone is taken proper care of is essential having said that Canada is known to 'leave no Canadian behind'. And lastly, having continual care for these elders is essential in ensuring the finest health care available for those in need. It is stated that individuals ages 55–64, "Over half (55 percent) have savings that represent less than one year's worth of the resources they need to supplement government programs like OAS/GIS and CPP/QPP. And fewer than 20 percent have enough savings to support the supplemented resources required for at least five years."[59] With this being said, to ensure the coverage of all seniors, the expansion of public policies are in need. And to reiterate the federal government, as well as the provincial government, should work together to create enhanced opportunities for these individuals.
Nursing homes and home care
There appear to be some problems within the nursing home/home care subsection of health care in Canada, and scholars and advocates point to an increasingly complex care system, occupational hazards, and an overall shortage of workers willing to work in this field as the main causes. Authors Ruth Lowndes and James Struthers in their dissertation say that there has been an intensification of job precarity, inadequate staffing levels as well as increasingly complex needs including different types of routinized, assembly-lines types of work, and cost-cutting on equipment and supplies. They also point out that within increasing elder population, the supply of workers is not meeting the demand required to provide adequate care.[60] This idea couples with another study that as we enter the 2020s and 30s, the equipment and processes that nurses undergo will become progressively composite. This then leads to the need for higher training and instruction to the existing nurses including the reliance on them to think critically and execute real-time, evidence-based care decisions which all point to a need to re-conceptualize HCAs.[61] Besides, it has been discovered that there are myriad possible occupational hazards for workers in-home care. Researcher Matthew Wong uses chi-square analysis and posthoc pairwise tests with a Bonferroni correction to find out that occupational hazards home care nurses experience, although depending on the type of geographical setting (rural, town, suburban, urban areas), it is common to find that aggressive pets, environmental tobacco smoke, oxygen equipment, unsafe neighborhoods, and pests, hinder a quality performance by the nurse from occurring.[62]
Role of private sector
About 27.6% of Canadians' healthcare is paid for through the private sector. This mostly goes towards services not covered or partially covered by Medicare, such as prescription drugs, dentistry and optometry. Some 75% of Canadians have some form of supplementary private health insurance; many of them receive it through their employers.[63]
The Canadian system is for the most part publicly funded, yet most of the services are provided by private enterprises. Most doctors do not receive an annual salary, but receive a fee per visit or service.[64] According to Dr. Albert Schumacher, former president of the Canadian Medical Association, an estimated 75 percent of Canadian health care services are delivered privately but funded publicly.
"Front line practitioners whether they're GP's or specialists, by and large, are not salaried. They're small hardware stores. Same thing with labs and radiology clinics ... The situation we are seeing now are more services around not being funded publicly but people having to pay for them, or their insurance companies. We have sort of a passive privatization."[64]
Capitation based models are used in some provinces as in place of or in parallel with the traditional fee for service model.[65]
"Although there are laws prohibiting or curtailing private health care in some provinces, they can be changed", according to a report in the New England Journal of Medicine.[66][67] In June 2005, the Supreme Court of Canada ruled in Chaoulli v. Quebec (Attorney General) that Quebec's prohibition against private health insurance for medically necessary services laws violated the Quebec Charter of Human Rights and Freedoms, potentially opening the door to much more private sector participation in the health system. Justices Beverley McLachlin, Jack Major, Michel Bastarache and Marie Deschamps found for the majority. "Access to a waiting list is not access to health care", wrote Chief Justice McLachlin.[68]
Public opinion
Canadians strongly support the health system's public rather than for-profit private basis, and a 2009 poll by Nanos Research found 86.2% of Canadians surveyed supported or strongly supported "public solutions to make our public health care stronger."[69][70] A Strategic Counsel survey found 91% of Canadians prefer their healthcare system instead of a U.S. style system.[71][72]
A 2009 Harris-Decima poll found 82% of Canadians preferred their healthcare system to the one in the United States.[73]
A 2003 Gallup poll found 25% of Americans are either "very" or "somewhat" satisfied with "the availability of affordable healthcare in the nation", versus 50% of those in the UK and 57% of Canadians. Those "very dissatisfied" made up 44% of Americans, 25% of respondents of Britons, and 17% of Canadians. Regarding quality, 48% of Americans, 52% of Canadians, and 42% of Britons say they are satisfied.[74]
Economics

Canada has a publicly funded medicare system, with most services provided by the private sector. Each province may opt-out, though none currently does. Canada has what is known as a single payer system, where basic services are provided by private doctors (since 2002 they have been allowed to incorporate), with the entire fee paid for by the government at the same rate. Most government funding (94%) comes from the provincial level.[75] Most family doctors receive a fee per visit. These rates are negotiated between the provincial governments and the province's medical associations, usually on an annual basis. Pharmaceutical costs are set at a global median by the government price controls.
Hospital care is delivered by publicly funded hospitals in Canada. Most of the public hospitals, each of which are independent institutions incorporated under provincial Corporations Acts, are required by law to operate within their budget.[77] Amalgamation of hospitals in the 1990s has reduced competition between hospitals. As the cost of patient care has increased, hospitals have been forced to cut costs or reduce services. Applying a pharmacoeconomic perspective to analyze cost reduction, it has been shown that savings made by individual hospitals result in actual cost increases to the provinces.[78]
In 2009, the government funded about 70% of Canadians' healthcare costs. This is slightly below the OECD average of public health spending.[79] This covered most hospital and physician costs while the dental and pharmaceutical costs were primarily paid for by individuals.[80] Half of private health expenditure comes from private insurance and the remaining half is supplied by out-of-pocket payments. Under the terms of the Canada Health Act, public funding is required to pay for medically necessary care, but only if it is delivered in hospitals or by physicians. There is considerable variation across the provinces/territories as to the extent to which such costs as out of hospital prescription medications, assistive devices, physical therapy, long-term care, dental care and ambulance services are covered.[81]
Healthcare spending in Canada (in 1997 dollars) has increased each year between 1975 and 2009, from $39.7 billion to $137.3 billion, or per capita spending from $1,715 to $4089.[82] In 2013 the total reached $211 billion, averaging $5,988 per person.[83] Figures in National Health Expenditure Trends, 1975 to 2012, show that the pace of growth is slowing. Modest economic growth and budgetary deficits are having a moderating effect. For the third straight year, growth in healthcare spending will be less than that in the overall economy. The proportion of Canada's gross domestic product will reach 11.6% in 2012 down from 11.7% in 2011 and the all-time high of 11.9% in 2010.[84] Total spending in 2007 was equivalent to 10.1% of the gross domestic product which was slightly above the average for OECD countries, and below the 16.0% of GDP spent in the United States.[85]
In 2009, the greatest proportion of this money went to hospitals ($51B), followed by pharmaceuticals ($30B), and physicians ($26B).[86] The proportion spent on hospitals and physicians has declined between 1975 and 2009 while the amount spent on pharmaceuticals has increased.[87] Of the three biggest health care expenses, the amount spent on pharmaceuticals has increased the most. In 1997, the total price of drugs surpassed that of doctors. In 1975, the three biggest health costs were hospitals ($5.5B/44.7%), physicians ($1.8B/15.1%), and medications ($1.1B/8.8%) while in 2007 the three biggest costs were hospitals ($45.4B/28.2% ), medications ($26.5B/16.5%), and physicians ($21.5B/13.4%).[88]
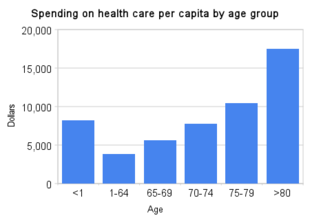
Healthcare costs per capita vary across Canada with Quebec ($4,891) and British Columbia ($5,254) at the lowest level and Alberta ($6,072) and Newfoundland ($5,970) at the highest.[75] It is also the greatest at the extremes of age at a cost of $17,469 per capita in those older than 80 and $8,239 for those less than 1 year old in comparison to $3,809 for those between 1 and 64 years old in 2007.[75]
In 2017, the Canadian Institute for Health Information reported that healthcare spending is expected to reach $242 billion, or 11.5% of Canada's gross domestic product for that year. Total health spending per resident varies from $7,378 in Newfoundland and Labrador to $6,321 in British Columbia. Public drug spending increased by 4.5% in 2016, driven largely by prescriptions for tumor necrosis factor alpha and hepatitis C drugs.[89]
According to a 2003 article by Lightman, "In-kind delivery in Canada is superior to the American market approach in its efficiency of delivery." In the US, 13.6 percent of GNP is used in medical care. By contrast, in Canada, only 9.5 percent of GNP is used on the Medicare system, "in part because there is no profit incentive for private insurers." Lightman also notes that the in-kind delivery system eliminates much of the advertising that is prominent in the US and the low overall administrative costs in the in-kind delivery system. Since there are no means tests and no bad-debt problems for doctors under the Canadian in-kind system, doctors billing and collection costs are reduced to almost zero.[90]
Efficiency of healthcare system
An OECD study in 2010 noted that there were variations in care across the different provinces in Canada. The study found that there was a difference in hospital admission rates depending on the number of people and what province they lived in. Typically, provinces with low population counts had higher hospital admission rates due to there being a lack of doctors and hospitals in the region.[91] A different study from the Canadian Institute for Health Information also concluded that there seem to be differences in the efficiency of care regionally. Regions that were similar in factors such as education levels and immigration numbers were found to have different efficiency levels in health care provision. The study concluded if increased efficiency of the current system was set as a goal, the death rate could be decreased by 18%-35%.[92] A separate study from the Canadian Institute for Health Information suggests multiple ways the efficiency of health care system could be improved. The study notes that supporting physician leadership and facilitating engagement of the care providers could reap great gains in efficiency. Additionally, the study suggested facilitating the exchange of information and interaction between health providers and government figures as well as flexible funding would also contribute to the improvement and solve the problem of differences in regional care by allowing regions to determine the needs of their general populace and meet those needs more efficiently by allowing target-specific allocation of funds.[93]
History
Government involvement
The various levels of government pay for about 70% of Canadians' healthcare, although this number has decreased somewhat in recent years.[94] The Constitution Act, 1867 (formerly called the British North America Act, 1867) did not give either the federal or provincial governments responsibility for healthcare, as it was then a minor concern. However, the Act did give the provinces responsibility for regulating hospitals, and the provinces claimed that their general responsibility for local and private matters encompassed healthcare. The federal government felt that the health of the population fell under the "Peace, order, and good government" part of its responsibilities. This led to several decades of debate over jurisdiction that were not resolved until the 1930s. Eventually, the Judicial Committee of the Privy Council decided that the administration and delivery of healthcare was a provincial concern, but that the federal government also had the responsibility of protecting the health and well-being of the population.
By far the largest government health program is Medicare, which is ten provincial programs, such as OHIP in Ontario, that are required to meet the general guidelines laid out in the federal Canada Health Act. Almost all government health spending goes through Medicare, but there are several smaller programs. The federal government directly administers health to groups such as the military, and inmates of federal prisons. They also provide some care to the Royal Canadian Mounted Police and veterans, but these groups mostly use the public system. Before 1966, Veterans Affairs Canada had a large healthcare network, but this was merged into the general system with the creation of Medicare. The largest group the federal government is directly responsible for is First Nations. Native peoples are a federal responsibility and the federal government guarantees complete coverage of their health needs. For the last twenty years and despite health care being a guaranteed right for First Nations due to the many treaties the government of Canada signed for access to First Nations lands and resources, the amount of coverage provided by the Federal government's Non-Insured Health Benefits program has diminished drastically for optometry, dentistry, and medicines. Status First Nations individuals qualify for a set number of visits to the optometrist and dentist, with a limited amount of coverage for glasses, eye exams, fillings, root canals, etc. For the most part, First Nations people use normal hospitals and the federal government then fully compensates the provincial government for the expense. The federal government also covers any user fees the province charges. The federal government maintains a network of clinics and health centers on Native Reserves. At the provincial level, there are also several much smaller health programs alongside Medicare. The largest of these is the health care costs paid by the workers' compensation system. Regardless of federal efforts, healthcare for First Nations has generally not been considered effective.[95][96][97]
Despite being a provincial responsibility, the large health costs have long been partially funded by the federal government. The cost-sharing agreement created by the Hospital Insurance and Diagnostic Services Act and extended by the Medical Care Act was discontinued in 1977 and replaced by Established Programs Financing. This gave a bloc transfer to the provinces, giving them more flexibility but also reducing the federal influence on the health system. In 1996, when faced with a large budget shortfall, the Liberal federal government merged the health transfers with the transfers for other social programs into the Canada Health and Social Transfer, and overall funding levels were cut. This placed considerable pressure on the provinces and combined with population aging and the generally high rate of inflation in health costs, has caused problems with the system.
Physicians and medical organization
Canada, like its North American neighbor the United States, has a ratio of practicing physicians to a population that is below the OECD average[98] but a level of practicing nurses that is higher than the OECD average, and below the US average in 2016.[99]
Family physicians in Canada make an average of $202,000 a year.[100] Alberta has the highest average salary of around $230,000, while Quebec has the lowest average annual salary at $165,000, arguably creating inter-provincial competition for doctors and contributing to local shortages.[100] In 2018, to draw attention to the low pay of nurses and the declining level of service provided to patients, more than 700 physicians, residents and medical students in Quebec signed an online petition asking for their pay raises to be canceled.[101]
In 1991, the Ontario Medical Association agreed to become a province-wide closed shop, making the OMA union a monopoly. Critics argue that this measure has restricted the supply of doctors to guarantee its members' incomes.[102] In 2008, the Ontario Medical Association and the Ontario government agreed to a four-year contract with a 12.25% doctors' pay raise, which was expected to cost Ontarians an extra $1 billion. Ontario's then-premier Dalton McGuinty said, "One of the things that we've got to do, of course, is ensure that we're competitive ... to attract and keep doctors here in Ontario ..."[103]
In December 2008, the Society of Obstetricians and Gynaecologists of Canada reported a critical shortage of obstetricians and gynecologists. The report stated that 1,370 obstetricians were practicing in Canada and that number is expected to fall by at least one-third within five years. The society is asking the government to increase the number of medical school spots for obstetrics and gynecologists by 30 percent a year for three years and also recommended rotating placements of doctors into smaller communities to encourage them to take up residence there.[104]
Each province regulates its medical profession through a self-governing College of Physicians and Surgeons, which is responsible for licensing physicians, setting practice standards, and investigating and disciplining its members.
The national doctors association is called the Canadian Medical Association (CMA);[105] it describes its mission as "To serve and unite the physicians of Canada and be the national advocate, in partnership with the people of Canada, for the highest standards of health and health care."[106] Because healthcare is deemed to be under provincial/territorial jurisdiction, negotiations on behalf of physicians are conducted by provincial associations such as the Ontario Medical Association. The views of Canadian doctors have been mixed, particularly in their support for allowing parallel private financing. The history of Canadian physicians in the development of Medicare has been described by C. David Naylor.[107] Since the passage of the 1984 Canada Health Act, the CMA itself has been a strong advocate of maintaining a strong publicly funded system, including lobbying the federal government to increase funding, and being a founding member of (and active participant in) the Health Action Lobby (HEAL).[108]
However, there are internal disputes. In particular, some provincial medical associations have argued for permitting a larger private role. To some extent, this has been a reaction to strong cost control; CIHI estimates that 99% of physician expenditures in Canada come from public sector sources, and physicians—particularly those providing elective procedures who have been squeezed for operating room time—have accordingly looked for alternative revenue sources. One indication came in August 2007 when the CMA elected as president Dr. Brian Day of B.C., who owns the largest private hospital in Canada and vocally supports increasing private healthcare in Canada. The CMA presidency rotates among the provinces, with the provincial association electing a candidate who is customarily ratified by the CMA general meeting. Day's selection was sufficiently controversial that he was challenged—albeit unsuccessfully—by another physician.[109]
A record number of doctors was reported in 2012 with 75,142 physicians. The gross average salary was $328,000. Out of the gross amount, doctors pay for taxes, rent, staff salaries and equipment.[110] Recent reports indicate that Canada may be heading toward an excess of doctors,[111] though communities in rural, remote and northern regions, however, may still experience a shortage.[112][113]
Criticisms
Wait times
Health Canada, a federal department, publishes a series of surveys of the healthcare system in Canada.[114] Although life-threatening cases are dealt with immediately, some services needed are non-urgent and patients are seen at the next-available appointment in their local chosen facility.
The median wait time for diagnostic services such as MRI and CAT scans[115] is two weeks with 86.4% waiting fewer than 90 days.[114] The median wait time for elective or non-urgent surgery is four weeks with 82.2% waiting fewer than 90 days.[114] Urgent cases requiring MRI and CT scans are prioritized, and the wait time for those patients is not included in the above statistics. In Ontario, urgent MRI and CT scans are performed almost immediately. [116]
Since 2002, the Canadian government has invested $5.5 billion to decrease wait times.[117] In April 2007, Prime Minister Stephen Harper announced that all ten provinces and three territories would establish wait-time guarantees by 2010. Canadians will be guaranteed timely access to healthcare in at least one of the following priority areas, prioritized by each province: cancer care, hip and knee replacement, cardiac care, diagnostic imaging, cataract surgeries or primary care.[118] The current cultural shift towards evidence-based medicine is burgeoning in Canada with the advent of organizations like Choosing Wisely Canada.[119] Organizations like this hope to encourage and facilitate doctor-patient communication, decreasing unnecessary care in Canada, and therefore hopefully decreasing wait times.[120]
Wait times for the same procedures can vary widely between hospitals and provinces. In Ontario, the average wait time for a knee replacement is 115 days (3 months and 4 weeks); however, average waiting times for individual hospitals vary from 45 days (1.5 months) to 397 days (about 1 year and 1 month).[121] This wait time was up by more than 50% from reported wait times in 5 Ontario hospitals from 1985 to 1990 (a median of 9.5 weeks, or about 2 months and 0.5 weeks), which was considered acceptable by most patients.[122] Wait times for knee replacements are much longer in Nova Scotia, ranging from 88 days (almost 3 months) to 350 days (about 11.5 months), with the hospitals in the middle range averaging 199 to 223 days (about 6 months 2.5 weeks to about 7 months 1.5 weeks).[123] Some patients wait significantly less, while the longest waits can be a good deal longer than the average. In contrast, Denmark has had a 2-month wait time guarantee for elective surgery (although this may not always have been met and does not itself show the rates of surgery performed), while in Germany, the Netherlands and Switzerland (all with near-universal coverage) the majority of patients contacted reported waiting less than 1 month for elective surgery (an average of 5 weeks for hip and knee replacements in the Netherlands).
Surveys on waiting times for elective surgery show that the percentage of patients who reported waiting a long time for elective surgery increased greatly in the 1990s, suggesting that waiting times were much shorter before then. Anecdotal (and therefore weak) evidence suggests that waiting times were not perceived as a major problem by the public before cutbacks in the 1990s at a time of greatly increased demand for health care. Another issue is the total waiting time. Ontario knee replacement recipients waited an average of 72 days to see an orthopedic surgeon (2 months 11 days), giving a total average waiting time of 177 days (about 5 months and 4 weeks) from referral to treatment.[121]
Sometimes, waiting times can be affected by temporary specialist shortages relative to demand rather than urgency, although patients waiting on the same list are often triaged; the author of this paragraph waited for only a little over 3 months to see a dermatologist because of a skin problem that itched slightly once a week and was not at all urgent (in the early 2000s) in Halifax, Nova Scotia, while cumulative waiting times (including referral to a medical test to appointment with a surgeon to radiation or cancer surgery) for cancer patients can be 2–3 months in areas with long waiting times. Waiting lists for cancer treatment are prioritized by level of urgency, but the triage process (while generally accurate) can occasionally assign a low priority to what turned out to be an urgent case.
A 2016 study by the Commonwealth Fund, based in the US, found that Canada's wait time for all categories of services ranked either at the bottom or second to the bottom of the 11 surveyed countries (Australia, Canada, France, Germany, Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States). Canada's wait time on emergency services was the longest of the 11 nations, with 29% of Canadians reporting that they waited for more than four hours the last time they went to an emergency department. Canada also had the longest wait time for specialist appointments, with 56% of all Canadians waiting for more than four weeks. Canada ranked last in all other wait time categories, including same- or next-day appointments, same-day answers from doctors, and elective surgeries, except for access to after-hour care, where Sweden ranks lower. The 2016 study also noted that despite government investment, Canada's wait-time improvements were negligible when compared to the 2010 survey.[124]
One Canadian doctor in 2006 quoted in the New York Times said, "This is a country in which dogs can get a hip replacement in under a week and in which humans can wait two to three years."[125] Day gave no source for his two to three years claim. The Canadian Health Coalition responded to Day's claims, pointing out that "access to veterinary care for animals is based on the ability to pay. Dogs are put down if their owners can't pay. Access to care should not be based on ability to pay."[126] Regional administrations of Medicare across Canada publish their own wait-time data on the web. The CHC is one of many groups across Canada calling for increased provincial and federal funding for Medicare and an end to provincial funding cuts as solutions to unacceptable wait times.[127] In a 2007 episode of ABC News's 20/20 titled "Sick in America", libertarian John Stossel cited numerous examples of Canadians who did not get the healthcare that they needed.[128] The conservative Fraser Institute found that treatment time from initial referral by a GP through consultation with a specialist to final treatment, across all specialties and all procedures (emergency, non-urgent, and elective), averaged 17.7 weeks in 2005,[129] contradicting the Canadian government's 2007 report regarding itself.[130]
Gender gap in healthcare
Disparities between men and women's access to healthcare in Canada have led to criticism, especially regarding healthcare privatization. While most healthcare expenses remain covered by Medicare, certain medical services previously paid for publicly have been shifted to individuals and employer-based supplemental insurance. While this shift has affected both genders, women have been more affected. Compared to men, women are generally less financially stable, and individual payments a greater burden.[131] Furthermore, many women work part-time or in fields that do not offer supplemental insurance, such as homemaking. As such, women are less likely to have private insurance to cover the costs of drugs and healthcare services.[132]
The shift from public to private financing has also meant additional labor for women due to families relying on them as caregivers. Less public financing has shifted care to women, leaving “them with more support to provide at home.”[133]
Women's additional healthcare requirements, such as pregnancy, further exacerbate the gender gap. Despite comprising approximately half of Canada's population, women receive the majority of Canadian healthcare.[131]
Men and women also experience different wait times for diagnostic tests; longer wait times have been associated with a higher risk of health complications. One Canadian study reports, "mean wait times are significantly lower for men than for women pertaining to overall diagnostic tests: for MRI, 70.3 days for women compared to 29.1 days for men."[134]
Inequality in the LGBT community
Canadians in the LGBT community, especially those in poverty, receive inadequate levels of treatment. A research study by Lori Ross and Margaret Gibson notes that of all demographics, LGBT members need mental health services the most due to systemic discrimination. According to the study, LGBT members often need to turn to mental health services that are mainly private and not covered by publicly-funded healthcare. Low-income LGBT members might be unable to afford these private programs; subsequently, their mental health issues may remain unaddressed or even worsen.[135]
Researcher Emily Colpitts states that LGBT members in Nova Scotia experience ambiguous or alienating language in their health policies. According to Colpitts, the "heteronormative and gender-binary language and structure of medical intake forms have the consequence of alienating LGBT populations." Colpitts adds that in the previous study of queer and transgender women in Nova Scotia, patients experienced significant discomfort in their meetings with healthcare providers and feared that because of the language of health policy, they would not be able to receive adequate healthcare based on their sexual identities.[136]
According to researcher Judith MacDonnell, LGBT members, especially childbearing lesbians, have trouble navigating through health policy. MacDonnell states that LBGT women encounter challenges at every point of the childbearing process in Canada and have to rely on personal and professional means to receive information that they can understand, such as in reproductive health clinics and postpartum or parenting support.[137]
Inequality in care for refugees
Refugees in Canada experience numerous barriers to healthcare, such as gaps in knowledge regarding healthcare needs, which may not be always considered by public health initiatives and policies.[138][139] Immigrants and refugees are among the groups most at risk for negative health effects resulting from persistent health disparities; differences in race, socioeconomic status, income, citizenship status, and other social factors further exacerbate healthcare inequalities. Compared to immigrants, refugees often require additional healthcare due to previous conditions in their countries of origin.[140]
The 2012 Protecting Canada's Immigration System Act formed a tiered system that classified refugees and separated care based on these classifications.[141][142] Differing levels of care were provided to refugees based on each refugee's home country and other factors.[142] The act also reduced healthcare coverage for refugees provided by the Interim Federal Health Program (IFHP).[143] The changes in refugee healthcare programs created in a rise in emergency room (ER) visits due to a lack of provisions of healthcare to refugees. This created concerns among Canadian citizens that the overall cost of healthcare will rise due. According to one study, the cuts to IFHP also made funding uncertain for programs that helped pay for ER costs.[144]
In July 2014, Canada's Federal Court ruled that denying health services to asylum seekers was "cruel and unusual treatment" and therefore unconstitutional.[141][145][146][142][147]
One study suggested open dialogue among policymakers, clinicians, and researchers and working with settlement programs to effectively respond to challenges encountered by the healthcare system regarding refugees.[148] The study notes that supporting primary care and focusing on social accountability training in medical schools will help ensure the sustainability of the healthcare system's response to refugees.[148]
Restrictions on privately funded healthcare
The Canada Health Act, which sets the conditions with which provincial/territorial health insurance plans must comply if they wish to receive their full transfer payments from the federal government, does not allow charges to insured persons for insured services (defined as medically necessary care provided in hospitals or by physicians). Most provinces have responded through various prohibitions on such payments. This does not constitute a ban on privately funded care; indeed, about 30% of Canadian health expenditures come from private sources, both insurance and out-of-pocket payments.[149] The Act does not address delivery. Private clinics are therefore permitted, albeit subject to provincial/territorial regulations, but they cannot charge above the agreed-upon fee schedule unless they are treating non-insured persons (which may include those eligible under automobile insurance or worker's compensation, in addition to those who are not Canadian residents), or providing non-insured services. This provision has been controversial among those seeking a greater role for private funding.
In 2006, the Government of British Columbia threatened to shut down one private clinic because it was planning to start accepting private payments from patients.[150] Since 2008, Dr. Brian Day has been suing the British Columbia government on the basis that the Canada Health Act is unconstitutional. In 2016, the Government of Quebec was sued for passing Bill 20, which allows and regulates add-on fees.[151][152]
Cross-border health care
The border between Canada and the United States represents a boundary line for medical tourism, in which a country's residents travel elsewhere to seek health care that is more available or affordable.
Canadians visiting the US to receive healthcare
Some residents of Canada travel to the United States for care. A study by Barer, et al., indicates that the majority of Canadians who seek healthcare in the U.S. are already there for other reasons, including business travel or vacations. A smaller proportion seek care in the U.S. for reasons of confidentiality, including abortions, mental illness, substance abuse, and other problems that they may not wish to divulge to their local physician, family, or employer. Canadians offered free care in the US paid by the Canadian government have sometimes declined it.[153]
An analysis using data from the 1996–1997 National Population Health Survey (NPHS—a large survey representative of the Canadian noninstitutionalized population, including 17,276 Canadian residents) reported that 0.5% sought medical care in the US in the previous year. Of these, less than a quarter had travelled to the U.S. expressly to get that care.[154] This was supported by an additional analysis performed from the American side, using a structured telephone survey of all ambulatory care clinical facilities located in specific heavily populated U.S. urban corridors bordering Canada and discharge data for 1994–1998 from major border states, and contacted key informants at each of U.S. News & World Report's "America's Best Hospitals" to inquire about the number of Canadians seen in both inpatient and outpatient settings.[154] The authors characterized this rate of medical travel as "barely detectable relative to the use of care by Canadians at home" and that the results "do not support the widespread perception that Canadian residents seek care extensively in the United States."[154] A separate report issued privately rather than in a peer reviewed journal by the conservative Fraser Institute think tank found that the percentage of Canadian patients who travelled abroad to receive non-emergency medical care was 1.1% in 2014, and 0.9% in 2013, with British Columbia being the province with the highest proportion of its citizens making such trips.[155]
Some Canadian politicians have travelled to the United States for treatment, which is viewed variously as ironic or cynical. Prime Minister Jean Chrétien traveled to the Mayo Clinic twice in 1999 for medical care.[156] Chrétien allegedly kept the visits a secret, with one occurring during a publicly announced ski trip to Vancouver.[157] Canadian Liberal MP Belinda Stronach went to the United States for breast cancer surgery in June 2007. Stronach's spokesperson Greg MacEachern was quoted in the article saying that the US was the best place to have this type of surgery done. Stronach paid for the surgery out of her own pocket.[158] Prior to this incident, Stronach had stated in an interview that she was against two-tier health care.[159] When Robert Bourassa, the premier of Quebec, needed cancer treatment, he went to the US to get it.[160] In 2010, Newfoundland and Labrador Premier Danny Williams travelled to the US for heart surgery.[161]
In 2007, it was reported that Canada sent scores of pregnant women to the US to give birth.[162] In 2007 a woman from Calgary who was pregnant with quadruplets was sent to Great Falls, Montana to give birth. An article on this incident states there were no Canadian hospitals with enough neonatal intensive beds to accommodate the extremely rare quadruple birth.[163]
A January 19, 2008, article in The Globe and Mail states, "More than 150 critically ill Canadians—many with life-threatening cerebral hemorrhages—have been rushed to the United States since the spring of 2006 because they could not obtain intensive-care beds here. Before patients with bleeding in or outside the brain have been whisked through U.S. operating-room doors, some have languished for as long as eight hours in Canadian emergency wards while health-care workers scrambled to locate care."[164]
In 2005, Shona Holmes of Waterdown, Ontario, travelled to the Mayo Clinic after deciding she couldn't afford to wait for appointments with specialists through the Ontario health care system.[165][166] She has characterized her condition as an emergency, said she was losing her sight, and portrayed her condition as life-threatening brain cancer. OHIP did not reimburse her for her medical expenses. In 2007 she joined a lawsuit to force the Ontario government to reimburse patients who feel they had to travel outside of Canada for timely, life-saving medical treatment. In July 2009 Holmes agreed to appear in television ads broadcast in the United States warning Americans of the dangers of adopting a Canadian style health care system. After her ad appeared critics pointed out discrepancies in her story, including that Rathke's cleft cyst, the condition she was treated for, was not a form of cancer, and was not life-threatening.[167][168] In fact, the mortality rate for patients with a Rathke's cleft cyst is zero percent. [169]
Americans visiting Canada to receive healthcare
Some US citizens travel to Canada for healthcare-related reasons. These reasons frequently involve seeking lower costs.
Many US citizens purchase prescription drugs from Canada, either over the Internet or by travelling there to buy them in person, because prescription drug prices in Canada are substantially lower than prescription drug prices in the United States; this cross-border purchasing has been estimated at $1 billion annually.[170] Some states like Florida have signed bills to import prescription drugs from Canada but are awaiting federal approval.[171][172][173]
Because medical marijuana is legal in Canada but illegal in most of the US, many US citizens with cancer, AIDS, multiple sclerosis, and glaucoma have travelled to Canada for medical treatment. One of those is Steve Kubby, the Libertarian Party's 1998 candidate for governor of California, who has adrenal cancer.[174] Recent legal changes such as Proposition 215 may decrease this type of medical tourism from California only.
Portability and provincial residency requirements
The Canada Health Act covers residents of Canada, which are persons "lawfully entitled to be or to remain in Canada who makes his home and is ordinarily present in the province, but does not include a tourist, a transient or a visitor to the province."[175] When traveling within Canada, a Canadian's health card from his or her home province or territory is accepted for hospital and physician services.[175]
Each province has residency and physical presence requirements to qualify for health care coverage. For example, to qualify for coverage in Ontario, with certain exceptions, one must be physically present in Ontario for 153 days in any given 12-month period. Most provinces require 183 days of physical presence in any given 12-month period. Exceptions may be made for mobile workers, if the individual can provide documentation from his or her employer verifying that the individual's work requires frequent travel in and out of the province.[176] Transients, self-employed itinerant workers (e.g. farm workers) who move from province to province several times within a year, and peripatetic retired or unemployed individuals who move from province to province (e.g. staying with various relatives, or living in a recreational vehicle) may find themselves ineligible for health coverage in any province or territory, even though they are Canadian citizens or landed immigrants physically present in Canada 365 days a year. "Snowbirds" (Canadians who winter in warm climates) and other Canadians who are out their home province or territory for a total of more than 183 days in twelve months lose all coverage, which is reinstated after a three-month waiting period.[177] Students attending a university or college outside their home province are generally covered by the health insurance program of their home province, however, "Typically this coverage (while out-of-province but within Canada) is for physician and hospital services only."[176] The Ontario Ministry of Health and Long Term Care, for example, states, "Therefore, when travelling outside of Ontario but within Canada, the ministry recommends that you obtain private supplementary health insurance for non-physician/non-hospital services."[176] Such services might include prescription drugs, or ground and air ambulance services that might be covered in one's home province.[178]
Comparison to other countries
The Canadian health care system is often compared to the US system. The US system spends the most in the world per capita, and was ranked 37th in the world by the World Health Organization in 2000, while Canada's health system was ranked 30th. The relatively low Canadian WHO ranking has been criticized by some for its choice of ranking criteria and statistical methods, and the WHO is currently revising its methodology and withholding new rankings until the topics are addressed.[179][180]
Canada spent approximately 10.0% of GDP on health care in 2006, more than one percentage point higher than the average of 8.9% in OECD countries.[181] According to the Canadian Institute for Health Information, spending is expected to reach $160 billion, or 10.6% of GDP, in 2007.[182] This translates to $4,867 per person.
In a sample of 13 developed countries Canada was tenth in its population weighted usage of medication in 14 classes in 2009 and sixth in 2013. The drugs studied were selected on the basis that the conditions treated had a high incidence, prevalence and/or mortality, caused significant long-term morbidity and incurred high levels of expenditure and significant developments in prevention or treatment had been made in the last 10 years. The study noted considerable difficulties in cross border comparison of medication use.[183]
A 2017 cost-effectiveness analysis by the Fraser Institute showed that "although Canada ranks among the most expensive universal-access health-care systems in the OECD, its performance for availability and access to resources is generally below that of the average OECD country, while its performance for use of resources and quality and clinical performance is mixed."[184]
| Country | Life expectancy. 2015.[185] | Under-five mortality rate per 1000 live births. 2016.[186] | Maternal mortality rate per 100,000 live births. 2015.[187] | Physicians per 1000 people. 2013.[98][188] | Nurses per 1000 people. 2013.[99][189] | Per capita expenditure on health (USD - PPP). 2016.[14] | Healthcare costs as a percent of GDP. 2016.[14][190] | % of government revenue spent on health. 2014.[191] | % of health costs paid by government. 2016.[192][193] |
|---|---|---|---|---|---|---|---|---|---|
| 82.8 | 3.7 | 5.5 | 3.4 | 11.5 | 4,708 | 9.6 | 17.3 | 67.8 | |
| 82.2 | 4.9 | 7.3 | 2.6 | 9.5 | 4,753 | 10.1 | 18.8 | 70.3 | |
| 82.4 | 3.9 | 7.8 | 3.3 | 9.4 | 4,600 | 11.0 | 15.7 | 78.8 | |
| 81.0 | 3.8 | 9.0 | 4.0 | 13.0 | 5,551 | 11.3 | 19.7 | 84.6 | |
| 83.7 | 2.7 | 6.4 | 3.3 | 11.5 | 4,519 | 10.9 | 20.3 | 84.1 | |
| 82.4 | 2.9 | 4.4 | 4.1 | 11.2 | 5,488 | 11.0 | 19.0 | 83.9 | |
| 81.2 | 4.3 | 9.2 | 2.8 | 8.2 | 4,192 | 9.7 | 16.5 | 79.2 | |
| 79.3 | 6.5 | 26.4 | 2.6 | 11.1 | 9,892 | 17.2 | 21.3 | 49.1 |
See also
- Canada Health Transfer
- Canada Health and Social Transfer
- Canada's Health Care providers, 2007
- Comparison of the healthcare systems in Canada and the United States
- Health in Canada
- Health care compared - tabular comparisons of the US, Canada, and other countries not shown above.
- EvidenceNetwork.ca Evidence Network of Canadian Health Policy
- Indian Health Transfer Policy
- Royal Commission on the Future of Health Care in Canada
References
- Karina Aase; Justin Waring; Lene Schibevaag (2017). Researching Quality in Care Transitions: International Perspectives. Springer. pp. 128–129. ISBN 978-3-319-62346-7.
- "Public vs. private health care". CBC News. December 1, 2006.
- Monique Bégin (1988). Medicare: Canada's Right to Health. Optimum Pub. International. p. Intro. ISBN 978-0-88890-219-1.
- Peggy Leatt; Joseph Mapa (2003). Government Relations in the Health Care Industry. Greenwood Publishing Group. p. 81. ISBN 978-1-56720-513-8.
- "The Health of Canadians – The Federal Role". 17.2 Universality: Parliament of Canada. Retrieved January 5, 2017.CS1 maint: location (link)
- David J. Kroll (2012). Capitalism Revisited: How to Apply Capitalism in Your Life. Dorrance Publishing. p. 126. ISBN 978-1-4349-1768-3.
- Tsai-Jyh Chen (2018). An International Comparison of Financial Consumer Protection. Springer. p. 93. ISBN 978-981-10-8441-6.
- Martel, Laurent; Malenfant, Éric Caron (September 22, 2009). "2006 Census: Portrait of the Canadian Population in 2006, by Age and Sex". Statistics Canada.
- "The World FactBook – Canada", The World Factbook, July 12, 2018
- Thomas G. Weiss (2017). "Canadian Male and Female Life Expectancy Rates by Province and Territory". Disabled World.
- "Health Status of Canadians - How healthy are we? - Perceived health". Report of the Chief Public Health Officer - Public Health Agency of Canada. 2016.
- David Gregory; Tracey Stephens; Christy Raymond-Seniuk; Linda Patrick (2019). Fundamentals: Perspectives on the Art and Science of Canadian Nursing. Wolters Kluwer Health. p. 75. ISBN 978-1-4963-9850-5.
- "Total health spending in Canada reaches $242 billion". Canadian Institute for Health Information. 2017. Archived from the original on April 21, 2019. Retrieved November 8, 2017.
Spending on drugs is expected to outpace spending on hospitals and doctors.
- Health expenditure and financing. OECD (Organisation for Economic Co-operation and Development). Choose options from dropdown menus.
- "Health at a Glance 2017" (PDF). OECD Publishing. 2017.
- "Health at a Glance - OECD Indicators by country". OECD Publishing. 2017.
- "International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care". Commonwealth Fund. Retrieved March 6, 2020.
- "Five things Canadians get wrong about the health system". The Globe and Mail.
- "Exploring the 70/30 Split: How Canada's Health Care System Is Financed" (PDF). The Canadian Institute for Health Information. Retrieved April 11, 2013.
- https://www.ontario.ca/page/learn-about-ohip-plus
- "Ministry of Health - Redirect". gov.bc.ca.
- "Health Premium". Queen's Printer for Ontario. Retrieved February 19, 2019.
- "SickKids hospital rallying 'crews' around $1.3-billion fundraising drive | CTV News". www.ctvnews.ca. Retrieved February 19, 2019.
- "Travel and accommodation - Canadian Cancer Society". www.cancer.ca. Retrieved February 19, 2019.
- "Provincial/Territorial Role in Health". Hc-sc.gc.ca. August 23, 2016.
- "Philpott, provinces hit impasse over health funding". Theglobeandmail.com. Retrieved May 27, 2018 – via The Globe and Mail.
- Melissa Leong (September 28, 2013). "Does your province cover the cost of infertility treatments?". Financial Post.
- "PSHCP Bulletin 17" (PDF). The Public Service Health Care Plan Bulletin (17): 2. 2005.
- "Paying to treat infertility: Coverage varies widely across Canada - National | Globalnews.ca". globalnews.ca. November 15, 2016. Retrieved February 19, 2019.
- Harding, Gail. "P.E.I. to cover gender reconstructive surgeries". CBC. Retrieved February 19, 2019.
- "Russia may introduce free prescription drugs". May 5, 2017.
- "Canadian medicare needs an Rx". umanitoba.ca. Archived from the original on December 20, 2014. Retrieved September 19, 2014.
- "Why, in a sea of pink, are so many cancer patients in the red?". thestar.com. October 9, 2012.
- "New Nova Scotia Family Pharmacare Program Begins". novascotia.ca (Press release). Government of Nova Scotia. Retrieved June 17, 2019.
- "Family Pharmacare Program". novascotia.ca. Government of Nova Scotia. Retrieved June 17, 2019.
- CIHI p.91
- "OHIP+: Children and Youth Pharmacare". Queen's Printer for Ontario. Retrieved February 19, 2019.
- Cara. "Canada's Premiers - The pan-Canadian Pharmaceutical Alliance". conseildelafederation.ca. Archived from the original on December 20, 2014. Retrieved September 19, 2014.
- "Frequently Asked Questions: What is the difference between a psychologist and a psychiatrist?". The Ontario Psychological Association. Archived from the original on January 30, 2015. Retrieved January 30, 2015.
The practice of most psychiatrists in Ontario is focused on prescribing medications and consulting with family physicians, psychologists and other health professionals.
- "Canada Health Act Exclusion of Certain Psychiatric Services Draws Attention". Canadian Psychiatric Association. Retrieved January 30, 2015.
- "Myth: Medicare covers all necessary health services". Canadian Foundation for Healthcare Improvement. Retrieved January 30, 2015.
- "Frequently Asked Questions: Who pays for psychological treatment?". The Ontario Psychological Association. Archived from the original on January 30, 2015. Retrieved January 30, 2015.
- "HST Update" (PDF). Ontario Society of Psychotherapists. Archived from the original (PDF) on February 1, 2015. Retrieved January 30, 2015.
- "What is covered under the AHCIP". Alberta Health. Archived from the original on January 30, 2015. Retrieved January 30, 2015.
- "Directory [of drug rehab centers by province]". Drug Rehab Services (a nonprofit organization). Retrieved January 19, 2017.
- "Troubled cops need more government help, mental health experts say". CBC. October 5, 2014. Retrieved February 1, 2015.
- Quiñonez, Carlos; Grootendorst, Paul (2011). "Equity in dental care among Canadian households". International Journal for Equity in Health. 10: 14. doi:10.1186/1475-9276-10-14. PMC 3097153. PMID 21496297.
- "Dental Insurance and use of Dental Services" (PDF). Statcan.gc.ca. Retrieved May 27, 2018.
- "Occupational Therapy (OT)". pt Health. Retrieved January 19, 2017.
- "Get physiotherapy: Get government-funded physiotherapy". ontario.ca. Queen’s Printer for Ontario. Retrieved January 19, 2017.
- "What OHIP covers". www.ontario.ca. Retrieved February 19, 2019.
- Rose, Rebecca (July 24, 2014). "Sex-reassignment surgeries funded in all but two provinces - But gaps remain in which surgeries covered where for trans Canadians". Daily Xtra. Pink Triangle Press.
- "Sex Reassignment Surgery". health.gov.on.ca. Queen’s Printer for Ontario. Retrieved January 19, 2017.
- "Assistive Devices Program". ontario.ca. Queen’s Printer for Ontario. Retrieved January 19, 2017.
- "Mobility aids". ontario.ca. Queen’s Printer for Ontario. Retrieved January 19, 2017.
- "What every older Canadian should know about: Income and benefits from government programs - Canada.ca". Canada.ca. October 3, 2016. Retrieved May 4, 2018.
- "The State of Seniors Healthcare in Canada" (PDF). Archived from the original (PDF) on December 13, 2017.
- "Canadian healthcare: What works and what doesn't". Benefitscanada.com. Retrieved May 4, 2018.
- "We're facing a wave of seniors living in poverty — and we're not ready - iPolitics". iPolitics. February 17, 2016. Retrieved May 4, 2018.
- Lowndes, Ruth; Struthers, James (Spring 2016). "Changes and Continuities in the Workplace of Long-Term Residential Care in Canada, 1970–2015". Journal of Canadian Studies. 50 (2): 368–395. doi:10.3138/jcs.50.2.368.
- Berta, Whitney; Laporte, Audrey; Deber, Raisa; Baumann, Andrea; Gamble, Brenda (June 14, 2013). "The evolving role of health care aides in the long-term care and home and community care sectors in Canada". Human Resources for Health. 11 (1): 25. doi:10.1186/1478-4491-11-25. ISSN 1478-4491. PMC 3723545. PMID 23768158.
- Wong, Matthew; Saari, Margaret; Patterson, Erin; Puts, Martine; Tourangeau, Ann E. (May 2017). "Occupational hazards for home care nurses across the rural-to-urban gradient in Ontario, Canada". Health & Social Care in the Community. 25 (3): 1276–1286. doi:10.1111/hsc.12430. PMID 28215055.
- Private Health Insurance in OECD Countries OECD Health Project, 2004. Retrieved January 21, 2008.
- Public vs. private health care CBC, December 1, 2006.
- Government of Ontario, Ministry of Health and Long-Term Care. "Primary Care Payment Models in Ontario - Health Care Professionals - MOHLTC". www.health.gov.on.ca. Retrieved February 19, 2019.
- Robert Steinbrook (April 20, 2006). "Private Health Care in Canada". N Engl J Med. 354 (16): 1661–1664. doi:10.1056/nejmp068064. PMID 16625005.
- Kraus, Clifford (February 26, 2006). "As Canada's Slow-Motion Public Health System Falters, Private Medical Care Is Surging". New York Times. Retrieved July 16, 2007.
- "CBC News Indepth: Health Care". CBC News. August 22, 2006. Retrieved January 3, 2015.
- "Public health care scores big in poll as MDs study privatization". Healthzone.ca. August 12, 2009. Retrieved February 10, 2011.
- "Canada overwhelmingly supports public health care". Nupge.ca. August 13, 2009. Retrieved February 10, 2011.
- "Canadians prefer Obama over own leaders: poll - CTV News". CTV.ca. June 29, 2008. Archived from the original on September 23, 2009. Retrieved February 10, 2011.
- "Never mind the anecdotes: Do Canadians like their health-care system?". Chicago Tribune. August 6, 2009.
- "Never mind the anecdotes: Do Canadians like their health-care system?". Chicago Tribune. August 6, 2009. Retrieved February 10, 2011.
- "Healthcare System Ratings: U.S., Great Britain, Canada". Gallup.com. Retrieved February 10, 2011.
- CIHI p.xiv
- CIHI p.119
- "Ontario Ministry of Health and Long-Term Care - Public Information - Public - Hospitals - Questions and Answers - Details". July 26, 2010. Archived from the original on July 26, 2010.
- "MacInnes JK, McAlister VC. Myopia of healthcare reform using business models. Ann R Coll Physicians Surg Can 2001; 34: 20-2". Works.bepress.com. Retrieved May 27, 2018.
- CIHI p.xiii
- Government of Ontario, Ministry of Health and Long-Term Care. "Ambulance Services Billing - Ontario Health Insurance (OHIP) - Publications - Public Information - MOHLTC". www.health.gov.on.ca.
- CIHI pg. 119
- "Health Spending in 2013" (PDF). Cihi.ca. Retrieved May 27, 2018.
- Canada's health care spending growth slows Archived June 15, 2013, at the Wayback Machine. Canadian Institute for Health Information (CIHI). Retrieved: May 28, 2013.
- CIHI p.55
- "Canadian health-care spending to top $180B". CBC News. November 19, 2009. Retrieved January 3, 2015.
- CIHI p.20
- CIHI p.112-113
- "Total health spending in Canada reaches $242 billion". Canadian Institute for Health Information. November 7, 2017. Archived from the original on April 21, 2019. Retrieved November 8, 2017.
Spending on drugs is expected to outpace spending on hospitals and doctors.
- Ernie Lightman, 2003 Social policy in Canada Toronto: Oxford University Press pg 130-131
- Alari, A., G. Lafortune and D. Srivastava (2014), "Canada: Geographic variations in health care", in Geographic Variations in Health Care: What Do We Know and What Can Be Done to Improve Health System Performance?, OECD Publishing, Paris, https://doi.org/10.1787/9789264216594-7-en.
- "Health System Efficiency in Canada: Why Does Efficiency Vary Among Regions?" (PDF). www.cihi.ca. Canadian Institute for Health Information. Retrieved December 13, 2018.
- "Improving Health System Efficiency in Canada Perspectives of Decision-Makers" (PDF). secure.cihi.ca. Canadian Institute for Health Information. Retrieved December 13, 2018.
- CIHI
- Silversides, Ann (October 23, 2007). "The North "like Darfur"". Canadian Medical Association Journal. 177 (9): 1013–4. doi:10.1503/cmaj.071359. PMC 2025628. PMID 17954876.
- Gao, Song; et al. (November 4, 2008). "Access to health care among status Aboriginal people with chronic kidney disease". Canadian Medical Association Journal. 179 (10): 1007–12. doi:10.1503/cmaj.080063. PMC 2572655. PMID 18981441.
- Peiris, David; Alex Brown; BMed MPH; Alan Cass; MBBS PhD (November 4, 2008). "Addressing inequities in access to quality health care for indigenous people". Canadian Medical Association Journal. 179 (10): 985–6. doi:10.1503/cmaj.081445. PMC 2572646. PMID 18981431.
- Health resources - Doctors. OECD Data.
- Health resources - Nurses. OECD Data.
- "Que. doctors lagging in fee-for-service payments". Ctv.ca. December 21, 2006. Archived from the original on June 10, 2009. Retrieved February 10, 2011.
- Wang, Amy (March 7, 2018). "Hundreds of Canadian doctors demand lower salaries. (Yes, lower.)". washingtonpost.com.
- Terence Corcoran (November 9, 2004). "ONTARIO DOCTORS SOLD OUT AGAIN" (PDF). National Post. Archived from the original (PDF) on May 31, 2006. Retrieved February 10, 2011.
- "Ont. doctors get 12.25 per cent wage hike". Archived from the original on September 30, 2008. Retrieved September 15, 2008.
- "Obstetrician shortage endangers moms, babies: report says". CTV.ca. December 5, 2008. Archived from the original on December 6, 2008.
- "Canadian Medical Association". Cma.ca. Archived from the original on July 8, 2009. Retrieved February 10, 2011.
- "About CMA". Cma.ca. March 24, 2010. Archived from the original on May 2, 2006. Retrieved February 10, 2011.
- Naylor, C David (1986). Private Practice, Public Payment: Canadian Medicine and the Politics of Health Insurance 1911-1966. Kingston, Ontario: McGill-Queen's University Press.
- "HEAL home page". Physiotherapy.ca. Archived from the original on March 10, 2011. Retrieved February 10, 2011.
- "CBC Private health-care advocate wins CMA presidency". CBC.ca. August 22, 2006. Retrieved February 10, 2011.
- "Canadian doctor total at record high". CBC.ca. Retrieved September 28, 2013.
- "Barer & Evans: What doctor shortage?". Nationalpost.com. October 8, 2013. Retrieved May 27, 2018.
- "More health specialists not the answer to health system woes". Umanitoba.ca. Archived from the original on December 20, 2014. Retrieved September 19, 2014.
- "Maria Mathews: Calling all country doctors". Nationalpost.ca. February 22, 2013.
- "Healthy Canadians: Canadian government report on comparable health care indicators" (PDF).
- Diagnostic tests defined as the following: non-emergency magnetic resonance imaging (MRI) devices; computed tomography (CT or CAT) scans; and angiographies that use X-rays to examine the inner opening of blood-filled structures such as veins and arteries.
- "MRI and CT Scan Wait Times Diagnostic Imaging – Health Quality Ontario (HQO)". www.hqontario.ca. Retrieved February 5, 2020.
- Waiting for access, CBC News: In-Depth: Health Care, November 29, 2006. Retrieved November 19, 2007.
- Media release Canada's New Government announces Patient Wait Times Guarantees Archived December 11, 2007, at the Wayback Machine, Office of the Prime Minister, April 4, 2007. Retrieved November 19, 2007.
- , CMAJ: More Hospitals Choosing Wisely, June 8, 2015. Retrieved July 15, 2015.
- Huffington Post: How to Reduce Wait Times in Canadian Health Care, May 16, 2015. Retrieved July 15, 2015.
- "Time to Patient's First Orthopedic Surgical Appointment – Health Quality Ontario". www.hqontario.ca. Retrieved June 15, 2019.
- Ho, E.; Coyte, P. C.; Bombardier, C.; Hawker, G.; Wright, J. G. (November 1994). "Ontario patients' acceptance of waiting times for knee replacements". The Journal of Rheumatology. 21 (11): 2101–2105. ISSN 0315-162X. PMID 7869317.
- Scotia, Communications Nova (October 20, 2014). "Government of Nova Scotia". waittimes.novascotia.ca. Retrieved June 15, 2019.
- "Commonwealth Fund Survey 2016". Canadian Institute for Health Information. The Commonwealth Fund. Retrieved August 11, 2017.
- Krauss, Clifford (February 28, 2006). "Canada's Private Clinics Surge as Public System Falters". The New York Times. Retrieved May 4, 2010.
- "Fact Check" (PDF). Retrieved February 17, 2009.
- "Ontario Health Coalition - Home". Web.net. Archived from the original on November 14, 2001. Retrieved February 10, 2011.
- 20/20, "Sick in America", ABC News, 2007
- "Hidden costs of Canada's Health Care System". Independent.org. April 23, 2004. Retrieved February 10, 2011.
- "Wait Times Tables: A Comparison by Province 2007" (PDF). Retrieved February 10, 2011.
- "Women and Private Health Insurance" (PDF). Womenandhealthcarereform.ca. Retrieved May 27, 2018.
- Canada, Health; Canada, Health (April 22, 2005). "Women's Health Strategy". aem. Retrieved May 4, 2018.
- "Health Care Privatization: Women Are Paying the Price | Canadian Women's Health Network". Cwhn.ca. Retrieved May 4, 2018.
- Kazanjian, Arminée; Morettin, Denise; Cho, Robert (August 25, 2004). "Health Care Utilization by Canadian Women". BMC Women's Health. 4 (Suppl 1): S33. doi:10.1186/1472-6874-4-S1-S33. PMC 2096683. PMID 15345096.
- Ross, Lori E.; Gibson, Margaret F.; Daley, Andrea; Steele, Leah S.; Williams, Charmaine C. (August 14, 2018). "In spite of the system: A qualitatively-driven mixed-methods analysis of the mental health services experiences of LGBTQ people living in poverty in Ontario, Canada". PLOS ONE. 13 (8): e0201437. Bibcode:2018PLoSO..1301437R. doi:10.1371/journal.pone.0201437. PMC 6093609. PMID 30110350.
- Colpitts, Emily; Gahagan, Jacqueline (September 22, 2016). ""I feel like I am surviving the health care system": understanding LGBTQ health in Nova Scotia, Canada". BMC Public Health. 16 (1): 1005. doi:10.1186/s12889-016-3675-8. PMC 5034675. PMID 27658489.
- MacDonnell, Judith A. (January 2014). "LGBT Health Care Access: Considering the Contributions of an Invitational Approach". Journal of Invitational Theory & Practice. 20: 38–60.
- McKeary, Marie (2010). "Barriers to Care: The Challenges for Canadian Refugees and their Health Care Providers". Journal of Refugee Studies [0951-6328]. 23 (4): 523–545. doi:10.1093/jrs/feq038.
- Lane, Ginny; Farag, Marwa; White, Judy; Nisbet, Christine; Vatanparast, Hassan (October 2018). "Chronic health disparities among refugee and immigrant children in Canada". Applied Physiology, Nutrition, and Metabolism. 43 (10): 1043–1058. doi:10.1139/apnm-2017-0407. ISSN 1715-5320. PMID 29726691.
- "Promoting the health of refugees and migrants" (PDF). World Health Organization. January 2017.
- "Federal Court rules against government's cuts to refugee health program". Toronto Sun. July 4, 2014. Retrieved March 10, 2019.
- Levitz, Stephanie (January 26, 2015). "Current refugee health care system still violates court decision: advocates". CTV News. Retrieved March 10, 2019.
- Harris, Helen (2015). "Harming Refugee and Canadian Health: the Negative Consequences of Recent Reforms to Canada's Interim Federal Health Program". Journal of International Migration and Integration. 16 (4): 1041–1055. doi:10.1007/s12134-014-0385-x.
- Evans, A.; Caudarella, A.; Ratnapalan, S.; Chan, K. (May 2014). "The Cost and Impact of the Interim Federal Health Program Cuts on Child Refugees in Canada" (PDF). PLOS ONE. 9 (5): e96902. doi:10.1371/journal.pone.0096902. PMC 4014561. PMID 24809676.
- "World Report 2016: Rights Trends in Canada". Human Rights Watch. January 6, 2016. Retrieved March 10, 2019.
- Ranalli, Audra (August 18, 2014). "Cuts to Refugee Health Care Found Unconstitutional: Canadian Doctors for Refugee Care v Canada". TheCourt.ca. Retrieved March 10, 2019.
- Fine, Sean (July 4, 2014). "Ottawa's refugee health-care cuts 'cruel and unusual,' court rules". The Globe and Mail. Retrieved March 10, 2019.
- Pottie, Kevin; Gruner, Doug; Magwood, Olivia (March 15, 2018). "Canada's response to refugees at the primary health care level". Public Health Research & Practice. 28 (1). doi:10.17061/phrp2811803. PMID 29582036.
- Canadian Institute for Health Information (September 27, 2005). CIHI exploring the 70-30 split. Ottawa, Ont.: Canadian Institute for Health Information. ISBN 978-1-55392-655-9. Archived from the original on March 19, 2006. Retrieved December 21, 2007.
- Cernetig, Miro (December 1, 2006). "B.C. gov't gets tough with private clinic". Vancouver Sun. CanWest News Service. Archived from the original on August 7, 2009. Retrieved January 9, 2008."B.C. gov't gets tough with private clinic". Archived from the original on August 7, 2009. Retrieved January 9, 2008.
- "Quebec groups worried about overbilling take legal action". CBC News. Retrieved December 29, 2017.
- "Inside the nearly eight-year long fight of Brian Day, the doctor who would free Canadians from medicare". National Post. September 1, 2016. Retrieved December 29, 2017.
- Schmitz, Anthony (January–February 1991). "Health Assurance" (PDF). In Health. 5 (1). pp. 39–47.
- Katz, S. J.; Cardiff, K.; Pascali, M.; Barer, M. L.; Evans, R. G. (2002). "Phantoms in the Snow: Canadians' Use of Health Care Services in the United States". Health Affairs. 21 (3): 19–31. doi:10.1377/hlthaff.21.3.19. PMID 12025983.
- Barua, Bacchus; Ren, Feixue. "Leaving Canada for Medical Care, 2015" (PDF). Fraser Institute Bulletin. Retrieved May 2, 2017.
- "The ultimate in two-tier health care". Montreal Gazette (editorial). February 3, 2010. Archived from the original on February 4, 2010. Retrieved May 29, 2016.
- Levant, Ezra (January 15, 2002). "PM proves health care not equal for all Canadians". Calgary Herald (column). Archived from the original on June 24, 2016. Retrieved May 29, 2016.
- "Stronach went to U.S. for cancer treatment: report". CTV.ca. September 14, 2007. Archived from the original on October 11, 2007. Retrieved February 10, 2011.
- "CBC News: Sunday - Belinda Stronach Interview". April 7, 2005. Archived from the original on April 14, 2004. Retrieved January 3, 2015.
- Rationing Health Care: Price Controls Are Hazardous to Our Health The Independent Institute, February 1, 1994
- Heart surgery to sideline N.L. premier for weeks, CBC News, February 2, 2010
- "Some Canadian mothers forced to give birth in U.S. | KOMO-TV - Seattle, Washington | News". Komo-Tv. April 1, 2010. Archived from the original on July 5, 2008. Retrieved February 10, 2011.
- Calgary, The (August 17, 2007). "Calgary's quads: Born in the U.S.A". Canada.com. Archived from the original on July 11, 2011. Retrieved February 10, 2011.
- Canada (January 19, 2008). "Health". Globe and Mail. Toronto.
- Tanya Talaga (September 6, 2007). "Patients suing province over wait times: Man, woman who couldn't get quick treatment travelled to U.S. to get brain tumours removed". Toronto Star. Archived from the original on March 1, 2009. Retrieved July 27, 2009.
Lindsay McCreith, 66, of Newmarket and Shona Holmes, 43, of Waterdown filed a joint statement of claim yesterday against the province of Ontario. Both say their health suffered because they are denied the right to access care outside of Ontario's "government-run monopolistic" health-care system. They want to be able to buy private health insurance.
- Sam Solomon (September 30, 2007). "New lawsuit threatens Ontario private care ban: "Ontario Chaoulli" case seeks to catalyze healthcare reform". National Review of Medicine. 4 (16). Archived from the original on August 2, 2009. Retrieved July 27, 2009.
- "Anti-medicare ad an exaggeration: experts". CBC News. July 31, 2009. Archived from the original on August 3, 2009. Retrieved August 7, 2009.
- Ian Welsh (July 21, 2009). "Americans Lives vs. Insurance Company Profits: The Real Battle in Health Care Reform". Huffington Post. Archived from the original on July 25, 2009. Retrieved July 21, 2009.
- Omar Islam MD FRCP(C) (March 27, 2008). "Rathke Cleft Cyst". Medscape. Retrieved November 22, 2009.
- Morgan, Steven; Hurley, Jeremiah (March 16, 2004). "Internet pharmacy: prices on the up-and-up". CMAJ. 170 (6): 945–946. doi:10.1503/cmaj.104001. PMC 359422. PMID 15023915.
- Koh, Elizabeth. "Gov. DeSantis signs bill that would allow Florida to pursue importing prescription drugs". Tampa Bay Times.
- Writer, Kevin MillerStaff (June 24, 2019). "Gov. Mills signs 4 bills to reduce medication prices, including buying from Canada".
- "Colorado wants to import prescription drugs from Canada. How it could work, and why it may not". The Colorado Sun.
- US cannabis refugees cross border The Guardian July 20, 2002
- "Canada Health Act - Frequently Asked Questions". Government of Canada. May 16, 2005. Retrieved February 1, 2015.
- "Studying, Working or Travelling to Another Province or Territory Within Canada". Queen's Printer for Ontario. Retrieved February 1, 2015.
- "How do I resume my health care coverage when returning to Canada following a lengthy absence?". Government of Canada. May 16, 2005. Retrieved February 1, 2015.
- "Do I need private health care coverage when travelling within Canada?". Government of Canada. May 16, 2005. Retrieved February 1, 2015.
- Phyllida Brown (January 26, 2002). "WHO to revise its method for ranking health systems". BMJ. 324 (7331): 190b–190. doi:10.1136/bmj.324.7331.190b. PMC 1172006. Retrieved February 10, 2011.
- Deber, Raisa (March 15, 2004). "Why Did the World Health Organization Rate Canada's Health System as 30th? Some Thoughts on League Tables". Longwoods Review. 2 (1). Retrieved January 9, 2008.
The measure of "overall health system performance" derives from adjusting "goal attainment" for educational attainment. Although goal attainment is in theory based on five measures (level and distribution of health, level and distribution of "responsiveness" and "fairness of financial contribution"), the actual values assigned to most countries, including Canada, were never directly measured. The scores do not incorporate any information about the actual workings of the system, other than as reflected in life expectancy. The primary reason for Canada's low standing rests on the high educational level of its population, particularly as compared to France, rather than on any features of its health system.
- OECD Health Data 2007: How Does Canada Compare Archived June 28, 2013, at the Wayback Machine, OECD, July 2007. Retrieved February 2, 2009.
- Media release, Health care spending to reach $160 billion this year Archived December 23, 2007, at the Wayback Machine, Canadian Institute for Health Information, November 13, 2007. Retrieved November 19, 2007.
- Office of health Economics. "International Comparison of Medicines Usage: Quantitative Analysis" (PDF). Association of the British Pharmaceutical Industry. Archived from the original (PDF) on November 11, 2015. Retrieved July 2, 2015.
- Barua, Bacchus; Hasan, Sazid; Timmermans, Ingrid (September 21, 2017), Comparing Performance of Universal Health Care Countries, 2017, Fraser Institute, ISBN 978-0-88975-464-5, retrieved November 26, 2017
- Life expectancy at birth. World Health Organization (WHO).
- Mortality rate, under-5 (per 1,000 live births). World Bank Data. World Development Indicators. World DataBank.
- Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. October 8, 2016. The Lancet. Volume 388. 1775–1812. See table of countries on page 1784 of the PDF.
- Health workforce. Density of physicians. World Health Organization (WHO) Archived September 22, 2017, at the Wayback Machine.
- Health workforce. Density of nursing and midwifery personnel. World Health Organization (WHO).
- Health expenditure, total (% of GDP). World Bank Data. World Health Organization Global Health Expenditure database.
- Health Financing. General government expenditure on health as a percentage of total government expenditure. World Health Organization (WHO).
- OECD Data. Health resources - Health spending. doi:10.1787/8643de7e-en.
- Health expenditure, public (% of total health expenditure). World Bank Data. World Health Organization Global Health Expenditure database.
Further reading
- Caulfield, Timothy A; Von Tigerstrom, Barbara (2002). Health care reform & the law in Canada: meeting the challenge. University of Alberta Press. p. 37. ISBN 978-0-88864-366-7.
Canada Health Act.
- Fierlbeck, Katherine (2011). Health Care in Canada: A Citizen's Guide to Policy and Politics. University of Toronto Press. ISBN 978-1-4426-0983-9.
- Jacobs, Philip; Jonsson, Egon; Rapoport, John (2008). Cost Containment and Efficiency in National Health Systems : A Global Comparison. Wiley-VCH. ISBN 978-3-527-32110-0.
- Institute, John Deutsch (2006). Study of Economic Policy Health Services Restructuring in Canada Conference. Economic Policy, Queen's University. ISBN 978-1-55339-075-6.
- Marchildon, Gregory P (2006). Health systems in transition : Canada. University of Toronto Press. ISBN 978-0-8020-9400-1.
Health care in Canada.
- Raphael, Dennis (2007). Poverty and Policy in Canada: Implications for Health and Quality of Life. Canadian Scholars' Press. ISBN 978-1-55130-323-9.
- Mullner, Ross M (2009). Encyclopedia of health services research. SAGE. pp. 559–562. ISBN 978-1-4129-7194-2.
External links
| Wikiquote has quotations related to: Healthcare in Canada |
- Canadian Federalism and Public Health Care: The Evolution of Federal-Provincial Relations | Mapleleafweb.com
- CBC Digital Archives — The Birth of Medicare
- Canadian Health Services Research Foundation
- Data from the Canadian Institute for Health Information