11β-Hydroxysteroid dehydrogenase
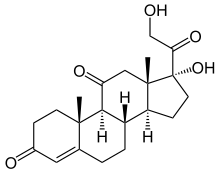
11β-Hydroxysteroid dehydrogenase (HSD-11β or 11β-HSD) is a family of enzymes that catalyze the conversion of inert 11 keto-products (cortisone) to active cortisol, or vice versa,[1] thus regulating the access of glucocorticoids to the steroid receptors:
- 11β-hydroxysteroid + NADP+ ⇌ an 11-oxosteroid + NADPH + H+
| 11-beta-hydroxysteroid dehydrogenase (NADP+) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
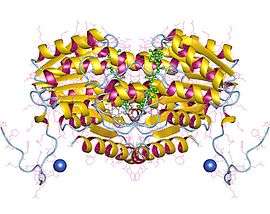 11-beta-hydroxysteroid dehydrogenase 1, dimer, Human | |||||||||
| Identifiers | |||||||||
| EC number | 1.1.1.146 | ||||||||
| CAS number | 9041-46-7 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| Gene Ontology | AmiGO / QuickGO | ||||||||
| |||||||||
Thus, the two substrates of this enzyme are 11beta-hydroxysteroid and NADP+, whereas its 3 products are 11-oxosteroid, NADPH, and H+.
This enzyme belongs to the family of oxidoreductases, specifically those acting on the CH-OH group of donor with NAD+ or NADP+ as acceptor. The systematic name of this enzyme class is 11beta-hydroxysteroid:NADP+ 11-oxidoreductase. Other names in common use include corticosteroid 11β-dehydrogenase, β-hydroxysteroid dehydrogenase, 11β-hydroxy steroid dehydrogenase, corticosteroid 11-reductase, and dehydrogenase, 11β-hydroxy steroid. This enzyme participates in c21-steroid hormone metabolism and androgen and estrogen metabolism.
Structural studies
As of late 2007, 8 structures have been solved for this class of enzymes, with PDB accession codes 1XSE, 1XU7, 1XU9, 1Y5M, 1Y5R, 2BEL, 2ILT, and 2IRW.
Function
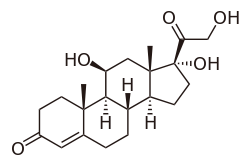
Cortisol, a glucocorticoid, binds the glucocorticoid receptor. However, because of its molecular similarity to aldosterone it also binds the mineralcorticoid receptor at higher concentrations. Both aldosterone and cortisol have a similar affinity for the mineralocorticoid receptor; however, there is vastly more cortisol in circulation than aldosterone. To prevent over-stimulation of the mineralocorticoid receptor by cortisol, 11β-HSD converts the biologically active cortisol to the inactive cortisone, which can no longer bind the mineralocorticoid receptor. 11β-HSD co-localizes with intracellular adrenal steroid receptors. Licorice, which contains glycyrrhizinic acid and enoxolone, can inhibit 11β-HSD and lead to a mineralocorticoid excess syndrome. Cortisol levels consequently rise, and cortisol binding to the mineralocorticoid receptor produces clinical signs and symptoms of hypokalemia, alkalosis and hypertension (i.e. mineralocorticoid excess).
Isoforms
In humans, there are two HSD11B isoforms:[2][3]
| HSD11B1 | NADPH-dependent | Highly expressed in key metabolic tissues including liver, adipose tissue, and the central nervous system. | In these tissues, HSD11B1 reduces cortisone to the active hormone cortisol that activates glucocorticoid receptors. |
| HSD11B2 | NAD+-dependent | Expressed in aldosterone-selective tissues, including kidneys, liver, lungs, colon, salivary glands, HSD2 neurons and placenta. | In these tissues, HSD11B2 oxidizes cortisol to cortisone and prevents illicit activation of the mineralocorticoid receptor. |
Inhibition of HSD11B1 has been suggested as a possible therapy for treatment of obesity and metabolic syndrome.[3]
Clinical Application
11-Beta Hydroxysteroid Dehydrogenase (HSD11B) is an enzyme that is involved in steroid hormone physiology. 11 beta- Hydroxysteroid Dehydrogenase enzyme exist in two isoforms, HSD11B-Type 1 and HSD11B- Type 2. The Type 1 isozyme is found in metabolic tissues targeted by glucocorticoids and converts cortisone to active cortisol.[4] HSD11B-Type 1 acts as a reductase producing active cortisol and the amplification of glucocorticoids. This enzyme is most abundant in the liver but can be found in most tissues in the body. The increased HSD11B is a common mechanism for visceral obesity.[5] HSD11B- Type 1 amplifies glucocorticoid concentrations in the liver and adipose tissue, glucocorticoid excess induces obesity with other features such as hypertension and diabetes mellitus.[6] The Type 2 isozyme is expressed by aldosterone-selective tissues and protects the mineralocorticoid receptor from the activation by cortisol by converting it to cortisone using the enzyme 11-Oxoreductase.Type 2 protects tissues from continuous activation by decreasing local cortisol levels and preventing 11- Oxoreductase from activating.[4] In tissues that do not express the mineralocorticoid receptor, such as the placenta and testis, it protects cells from the growth-inhibiting and/or pro-apoptotic effects of cortisol, particularly during embryonic development. Mutations in this gene cause the syndrome of apparent mineralocorticoid excess and hypertension.[7]
The 11-Beta Dehydrogenase enzyme has been researched and has been found to affect various tissues and body functions. The since the main functions of this enzyme are for the regulation of glucocorticoids, the enzyme is linked to various overstimulation or depletion of glucocorticosteroids that result in chemical imbalances in the human body. The clinical application of the 11-beta Dehydrogenase enzyme has made significant strides in research relating to obesity and studies in pregnancy. The effects of the enzyme as it relates to specific body functions and its associated disorders are listed below.
Effect of Hyperlipidemia on 11β-hydroxysteroid-dehydrogenase
Hyperlipidemia has a great effect on 11β-hydroxysteroid-dehydrogenase.[8] Glucocorticoid is dependent on Glucocorticoid plasma concentration, cellular glucocorticoid receptor expression and the pre-receptor hormone metabolism that is catalyzed by 11β-HSD.[8] There are two types of 11β-Hydroxysteroid dehydrogenases that control cortisol concentration: 11β-HSD1 and 11β-HSD2.[8] 11β-HSD1 is responsible for converting cortisone to cortisol by acting as an oxo-reductase because it is NADP(H) dependent, while 11β-HSD2 inactivates cortisol to cortisone via NAD.[8] 10-d hyperlipidemia increases the 11β-HSD1 expression in visceral and subcutaneous adipose tissues.[8] Hyperlipidemia decreases 11β-HSD2 expression in the liver and adipose tissue.[8] Hyperlipidemia has a great influence on 11β-HSD1 and 11β-HSD2.[8] This demonstrates that there is likely a relationship between hyperlipidemia and cortisol metabolism.[8]
Activity of 11β-HSD in organs
11β-hydroxysteroid dehydrogenase is active in organs and in the adrenal gland.[9] The isoforms of the enzyme take on various duties.[9] During an active state, the first isoform promotes the increase in glucocorticoids in the hepatocytes and also enhances gluconeogenesis.[9] The second isoform converts active glucocorticoid hormones to inactive metabolites in target tissues such as kidney, salivary glands, intestines, etc.[9] The activation of the two isoforms of 11β-HSD in the kidneys and liver triggers the extra-adrenal formation in alloxan diabetes, which affiliates with the reduction in the synthesis of glucocorticoid hormones in the adrenal glands.[9] The extra-adrenal formation leads to the increased local formation of corticosterone in the liver and has a high activity of reactions with gluconeogenesis.[9] These gluconeogenesis reactions add to the continued metabolic disorders similar to that of diabetes.[9] The first isoform of 11β-HSD can serve as a potential treatment agents for diabetes, obesity, and metabolic syndrome due to increasing local corticosterone.[9]
Involvement in the brain
11β-hydroxysteroid dehydrogenase is expressed in the central nervous system of aged individuals.[10] It is essential in Hypothalamo-Pituitary-Adrenal Axis function.[10] 11β-hydroxysteroid dehydrogenase also partakes involvement in the decline of conscious intellectual activity due to ageing.[10] The enzyme also contributes to central effects are also during the development stages.[10] For instance, the 11β-hydroxysteroid dehydrogenase type 2 shows frequently in fetal tissues such as a newborn's brain and placenta.[10] If there is an absence or decline in 11β-HSD2 in the fetus tissues, there are negative developmental consequences such as anxiety.[10]
11β-hydroxysteroid dehydrogenase are partly responsible for intracellular metabolism that determine the operation of glucocorticoids within cells.[10] Glucocorticoids impact the brain development and ultimately the function of the central nervous system.[10] So much so, that if there is a surplus or scant amounts of it, the consequences are deformities throughout one's entire life.[10] 11β-HSD1 is responsible for activating glucocorticoids while 11β-HSD2 is responsible for deactivating them.[10] The consequences for 11β-HSD1 activating glucocorticoids is that there is a decline in cognition especially as one ages.[10] Contrarily, the effects of 11β-HSD2 occur during development.[10] Some consequences of a high expression 11β-HSD2 are anxiety and cardiometabolic disorders, both of which are part of the early age glucocorticoid programming.[10]
Involvement in Preterm Births
Infants born underweight are susceptible to having metabolic disease throughout their lives.[11] The presence of glucocorticoids has contributed to the relatively low infant birth weight.[11] Glucocorticoid regulation is determined by 11β-hydroxysteroid dehydrogenase since they convert cortisone and cortisol and vice versa depending on the isoform (type 1 or type 2).[11] A decrease in 11β-HSD2 in the placenta can lead to infant restriction in growth, specifically during the first 12 months of an infant's life.[11] The reason for this is because the 11β-HSD2 is meant to be expressed in high quantities in the placenta, This is so because the enzymes secure the fetus from exposure to increased levels of glucocorticoids, which are linked to underweight newborns.[11]
See also
- Steroidogenic enzyme
- 11β-Hydroxysteroid dehydrogenase type 1
- 11β-Hydroxysteroid dehydrogenase type 2
- Cortisone reductase deficiency
References
- Seckl JR, Walker BR (April 2001). "Minireview: 11beta-hydroxysteroid dehydrogenase type 1- a tissue-specific amplifier of glucocorticoid action". Endocrinology. 142 (4): 1371–6. doi:10.1210/en.142.4.1371. PMID 11250914. Archived from the original on 2013-04-14.
- Seckl JR (January 1997). "11beta-Hydroxysteroid dehydrogenase in the brain: a novel regulator of glucocorticoid action?". Front Neuroendocrinol. 18 (1): 49–99. doi:10.1006/frne.1996.0143. PMID 9000459.
- Anagnostis P, Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP (2009). "Clinical review: The pathogenetic role of cortisol in the metabolic syndrome: a hypothesis". The Journal of Clinical Endocrinology and Metabolism. 94 (8): 2692–2701. doi:10.1210/jc.2009-0370. PMID 19470627. Archived from the original on 2010-07-12. Retrieved 2011-03-13.
- Lindsay, Kaitlin. "Kaitlin Lindsay: Medical & Scientific Illustration". kaitlinlindsay.com. Archived from the original on 2019-04-22.
- Ellis, Wendy L. "11-Beta-Hydroxysteroid Dehydrogenase" (PDF). semanticscholar.org. Retrieved November 23, 2018.
- Hughes, Katherine A; Webster, Scott P; Walker, Brian R (2008-03-25). "11-Beta-hydroxysteroid dehydrogenase type 1 (11β-HSD1) inhibitors in Type 2 diabetes mellitus and obesity". Expert Opinion on Investigational Drugs. 17 (4): 481–496. doi:10.1517/13543784.17.4.481. ISSN 1354-3784. PMID 18363514.
- "HSD11B2 Gene". www.greencards.org.
- Sieber-Ruckstuhl, Nadja S.; Zini, Eric; Osto, Melanie; Franchini, Marco; Boretti, Felicitas S.; Meli, Marina L.; Sigrist, Brigitte; Lutz, Thomas A.; Reusch, Claudia E. (November 2010). "Effect of hyperlipidemia on 11β-hydroxysteroid-dehydrogenase, glucocorticoid receptor, and leptin expression in insulin-sensitive tissues of cats" (PDF). Domestic Animal Endocrinology. 39 (4): 222–230. doi:10.1016/j.domaniend.2010.06.003. ISSN 0739-7240. PMID 20688460.
- Cherkasova, O. P.; Selyatitskaya, V. G.; Pal’chikova, N. A.; Kuznetsova, N. V. (2014-11-29). "Activity of 11β-Hydroxysteroid Dehydrogenase in the Adrenal Glands, Liver, and Kidneys of Rats with Experimental Diabetes". Bulletin of Experimental Biology and Medicine. 158 (2): 185–187. doi:10.1007/s10517-014-2718-3. ISSN 0007-4888. PMID 25430643.
- Wyrwoll, Caitlin S.; Holmes, Megan C.; Seckl, Jonathan R. (August 2011). "11β-Hydroxysteroid dehydrogenases and the brain: From zero to hero, a decade of progress". Frontiers in Neuroendocrinology. 32 (3): 265–286. doi:10.1016/j.yfrne.2010.12.001. ISSN 0091-3022. PMC 3149101. PMID 21144857.
- Rogers, Samantha L.; Hughes, Beverly A.; Jones, Christopher A.; Freedman, Lauren; Smart, Katherine; Taylor, Norman; Stewart, Paul M.; Shackleton, Cedric H. L.; Krone, Nils P. (May 2014). "Diminished 11β-Hydroxysteroid Dehydrogenase Type 2 Activity Is Associated With Decreased Weight and Weight Gain Across the First Year of Life". The Journal of Clinical Endocrinology & Metabolism. 99 (5): E821–E831. doi:10.1210/jc.2013-3254. ISSN 0021-972X. PMID 24517145.
- Agarwal AK, Monder C, Eckstein B, White PC (1989). "Cloning and expression of rat cDNA encoding corticosteroid 11 beta-dehydrogenase". J. Biol. Chem. 264 (32): 18939–43. PMID 2808402.
- Bush IE, Hunter SA, Meigs RA (1968). "Metabolism of 11-oxygenated steroids. Metabolism in vitro by preparations of liver". Biochem. J. 107 (2): 239–58. doi:10.1042/bj1070239. PMC 1198650. PMID 4384445.
- Lakshmi V, Monder C (1988). "Purification and characterization of the corticosteroid 11 beta-dehydrogenase component of the rat liver 11 beta-hydroxysteroid dehydrogenase complex". Endocrinology. 123 (5): 2390–8. doi:10.1210/endo-123-5-2390. PMID 3139396.
- Phillips DM, Lakshmi V, Monder C (1989). "Corticosteroid 11 beta-dehydrogenase in rat testis". Endocrinology. 125 (1): 209–16. doi:10.1210/endo-125-1-209. PMID 2661206.
External links
- 11-beta-Hydroxysteroid+Dehydrogenases at the US National Library of Medicine Medical Subject Headings (MeSH)