Miscarriage
Miscarriage, also known as spontaneous abortion and pregnancy loss, is the natural death of an embryo or fetus before it is able to survive independently.[1][4] Some use the cutoff of 20 weeks of gestation, after which fetal death is known as a stillbirth.[13] The most common symptom of a miscarriage is vaginal bleeding with or without pain.[1] Sadness, anxiety and guilt may occur afterwards.[3][14] Tissue and clot-like material may leave the uterus and pass through and out of the vagina.[15] When a woman keeps having miscarriages, infertility is present.[16]
| Miscarriage | |
|---|---|
| Other names | spontaneous abortion, early pregnancy loss |
 | |
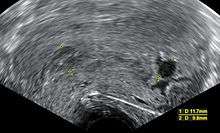
| An ultrasound showing a gestational sac containing a yolk sac but no embryo. | |
| Specialty | Obstetrics and gynecology |
| Symptoms | Vaginal bleeding with or without pain[1] |
| Complications | Infection, bleeding,[2] sadness, anxiety, guilt[3] |
| Usual onset | Before 20 weeks of pregnancy[4] |
| Causes | Chromosomal abnormalities,[1][5] uterine abnormalities [6] |
| Risk factors | Being an older parent, previous miscarriage, exposure to tobacco smoke, obesity, diabetes, autoimmune diseases, drug or alcohol use[7][8][9] |
| Diagnostic method | Physical examination, human chorionic gonadotropin, ultrasound[10] |
| Differential diagnosis | Ectopic pregnancy, implantation bleeding.[1] |
| Prevention | Prenatal care[11] |
| Treatment | Expectant management, vacuum aspiration, emotional support[8][12] |
| Medication | misoprostol |
| Frequency | 10–50% of pregnancies[1][7] |
Risk factors for miscarriage include being an older parent, previous miscarriage, exposure to tobacco smoke, obesity, diabetes, thyroid problems, and drug or alcohol use.[7][8] About 80% of miscarriages occur in the first 12 weeks of pregnancy (the first trimester).[1] The underlying cause in about half of cases involves chromosomal abnormalities.[5][1] Diagnosis of a miscarriage may involve checking to see if the cervix is open or closed, testing blood levels of human chorionic gonadotropin (hCG), and an ultrasound.[10] Other conditions that can produce similar symptoms include an ectopic pregnancy and implantation bleeding.[1]
Prevention is occasionally possible with good prenatal care.[11] Avoiding drugs, alcohol, infectious diseases, and radiation may decrease the risk of miscarriage.[11] No specific treatment is usually needed during the first 7 to 14 days.[8][12] Most miscarriages will complete without additional interventions.[8] Occasionally the medication misoprostol or a procedure such as vacuum aspiration is used to remove the remaining tissue.[12][17] Women who have a blood type of rhesus negative (Rh negative) may require Rho(D) immune globulin.[8] Pain medication may be beneficial.[12] Emotional support may help with processing the loss.[12]
Miscarriage is the most common complication of early pregnancy.[18] Among women who know they are pregnant, the miscarriage rate is roughly 10% to 20%, while rates among all fertilisation is around 30% to 50%.[1][7] In those under the age of 35 the risk is about 10% while it is about 45% in those over the age of 40.[1] Risk begins to increase around the age of 30.[7] About 5% of women have two miscarriages in a row.[19] Some recommend not using the term "abortion" in discussions with those experiencing a miscarriage in an effort to decrease distress.[20] In Britain the term miscarriage has replaced any use of the word abortion in relation to pregnancy loss in response to complaints of insensitivity towards women who had suffered such loss.[21]
Signs and symptoms
Signs of a miscarriage include vaginal spotting, abdominal pain, cramping, and fluid, blood clots, and tissue passing from the vagina.[22][23][24] Bleeding can be a symptom of miscarriage, but many women also have bleeding in early pregnancy and don't miscarry.[25] Bleeding during the first half of pregnancy may be referred to as a threatened miscarriage.[26] Of those who seek treatment for bleeding during pregnancy, about half will miscarry.[27] Miscarriage may be detected during an ultrasound exam, or through serial human chorionic gonadotropin (HCG) testing.
Risk factors
Miscarriage may occur for many reasons, not all of which can be identified. Risk factors are those things that increase the likelihood of having a miscarriage but don't necessarily cause a miscarriage. Up to 70 conditions,[1][5][28][29][30][31] infections,[32][33][34] medical procedures,[35][36][37] lifestyle factors,[7][8][38][39][40] occupational exposures,[11][41][42] chemical exposure,[42] and shift work are associated with increased risk for miscarriage.[43] Some of these risks include endocrine, genetic, uterine, or hormonal abnormalities, reproductive tract infections, and tissue rejection caused by an autoimmune disorder.[44]
Trimesters
First trimester
| Description | Proportion of total |
|---|---|
| Normal | 45–55% |
| Autosomal trisomy | 22–32% |
| Monosomy X (45, X) | 5–20% |
| Triploidy | 6–8% |
| Structural abnormality of the chromosome |
2% |
| Double or triple trisomy | 0.7–2.0%[45] |
| Translocation | Unknown[46] |
Most clinically apparent miscarriages (two-thirds to three-quarters in various studies) occur during the first trimester.[1][32][47][48] About 30% to 40% of all fertilized eggs miscarry, often before the pregnancy is known.[1] The embryo typically dies before the pregnancy is expelled; bleeding into the decidua basalis and tissue necrosis causes uterine contractions to expel the pregnancy.[48] Early miscarriages can be due to a developmental abnormality of the placenta or other embryonic tissues. In some instances an embryo does not form but other tissues do. This has been called a "blighted ovum".[49][50][45]
Successful implantation of the zygote into the uterus is most likely 8 to 10 days after fertilization. If the zygote has not implanted by day 10, implantation becomes increasingly unlikely in subsequent days.[51]
A chemical pregnancy is a pregnancy that was detected by testing but ends in miscarriage before or around the time of the next expected period.[52]
Chromosomal abnormalities are found in more than half of embryos miscarried in the first 13 weeks. Half of embryonic miscarriages (25% of all miscarriages) have an aneuploidy (abnormal number of chromosomes).[53] Common chromosome abnormalities found in miscarriages include an autosomal trisomy (22–32%), monosomy X (5–20%), triploidy (6–8%), tetraploidy (2–4%), or other structural chromosomal abnormalities (2%).[48] Genetic problems are more likely to occur with older parents; this may account for the higher rates observed in older women.[54]
Luteal phase progesterone deficiency may or may not be a contributing factor to miscarriage.[55]
Second and third trimesters
Second trimester losses may be due to maternal factors such as uterine malformation, growths in the uterus (fibroids), or cervical problems.[32] These conditions also may contribute to premature birth.[47] Unlike first-trimester miscarriages, second-trimester miscarriages are less likely to be caused by a genetic abnormality; chromosomal aberrations are found in a third of cases.[48] Infection during the third trimester can cause a miscarriage.[32]
Age
The age of the pregnant woman is a significant risk factor. Miscarriage rates increase steadily with age, with more substantial increases after age 35.[56] In those under the age of 35 the risk is about 10% while it is about 45% in those over the age of 40.[1] Risk begins to increase around the age of 30.[7] Paternal age is associated with increased risk.[57]
Obesity, eating disorders and caffeine
Not only is obesity associated with miscarriage; it can result in sub-fertility and other adverse pregnancy outcomes. Recurrent miscarriage is also related to obesity. Women with bulimia nervosa and anorexia nervosa may have a greater risk for miscarriage. Nutrient deficiencies have not been found to impact miscarriage rates but hyperemesis gravidarum sometimes precedes a miscarriage.[41]
Caffeine consumption also has been correlated to miscarriage rates, at least at higher levels of intake.[32] However, such higher rates have been found to be statistically significant only in certain circumstances.
Vitamin supplementation has generally not shown to be effective in preventing miscarriage.[58] Chinese traditional medicine has not been found to prevent miscarriage.[24]
Endocrine disorders
Disorders of the thyroid may affect pregnancy outcomes. Related to this, iodine deficiency is strongly associated with an increased risk of miscarriage.[41] The risk of miscarriage is increased in those with poorly controlled insulin-dependent diabetes mellitus.[41] Women with well-controlled diabetes have the same risk of miscarriage as those without diabetes.[59][60]
Food poisoning
Ingesting food that has been contaminated with listeriosis, toxoplasmosis, and salmonella is associated with an increased risk of miscarriage.[32][16]
Amniocentesis and chorionic villus sampling
Amniocentesis and chorionic villus sampling (CVS) are procedures conducted to assess the fetus. A sample of amniotic fluid is obtained by the insertion of a needle through the abdomen and into the uterus. Chorionic villus sampling is a similar procedure with a sample of tissue removed rather than fluid. These procedures are not associated with pregnancy loss during the second trimester but they are associated with miscarriages and birth defects in the first trimester.[37] Miscarriage caused by invasive prenatal diagnosis (chorionic villus sampling (CVS) and amniocentesis) is rare (about 1%).[36]
Surgery
The effects of surgery on pregnancy are not well-known including the effects of bariatric surgery. Abdominal and pelvic surgery are not risk factors in miscarriage. Ovarian tumors and cysts that are removed have not been found to increase the risk of miscarriage. The exception to this is the removal of the corpus luteum from the ovary. This can cause fluctuations in the hormones necessary to maintain the pregnancy.[61]
Medications
There is no significant association between antidepressant medication exposure and spontaneous abortion.[62] The risk of miscarriage is not likely decreased by discontinuing SSRIs prior to pregnancy.[63] Some available data suggest that there is a small increased risk of miscarriage for women taking any antidepressant,[64][65] though this risk becomes less statistically significant when excluding studies of poor quality.[62][66]
Medicines that increase the risk of miscarriage include:
- retinoids
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- misoprostol
- methotrexate[32]
- statins[67]
Immunizations
Immunizations have not been found to cause miscarriage.[68] Live vaccinations, like the MMR vaccine, can theoretically cause damage to the fetus as the live virus can cross the placenta and potentially increase the risk for miscarriage.[69][70] Therefore, the Center for Disease Control (CDC) recommends against pregnant women receiving live vaccinations.[71] However, there is no clear evidence that has shown live vaccinations to increase the risk for miscarriage or fetal abnormalities.[70]
Some live vaccinations include: MMR, varicella, certain types of the influenza vaccine, and rotavirus.[72][73]
Treatments for cancer
Ionizing radiation levels given to a woman during cancer treatment cause miscarriage. Exposure can also impact fertility. The use of chemotherapeutic drugs used to treat childhood cancer increases the risk of miscarriage.[41]
Pre-existing diseases
Several pre-existing diseases in pregnancy can potentially increase the risk of miscarriage, including diabetes, polycystic ovary syndrome (PCOS), hypothyroidism, certain infectious diseases, and autoimmune diseases. PCOS may increase the risk of miscarriage.[32] Two studies suggested treatment with the drug metformin significantly lowers the rate of miscarriage in women with PCOS,[74][75] but the quality of these studies has been questioned.[76] Metformin treatment in pregnancy has not been shown to be safe.[77] In 2007 the Royal College of Obstetricians and Gynaecologists also recommended against use of the drug to prevent miscarriage.[76] Thrombophilias or defects in coagulation and bleeding were once thought to be a risk in miscarriage but have been subsequently questioned.[78] Severe cases of hypothyroidism increase the risk of miscarriage. The effect of milder cases of hypothyroidism on miscarriage rates has not been established. A condition called luteal phase defect (LPD) is a failure of the uterine lining to be fully prepared for pregnancy. This can keep a fertilized egg from implanting or result in miscarriage.[79]
Mycoplasma genitalium infection is associated with increased risk of preterm birth and miscarriage.[34]
Infections can increase the risk of a miscarriage: rubella (German measles), cytomegalovirus, bacterial vaginosis, HIV, chlamydia, gonorrhoea, syphilis, and malaria.[32]
Immune status
Autoimmunity is possible cause of recurrent or late-term miscarriages. In the case of an autoimmune-induced miscarriages the woman's body attacks the growing fetus or prevents normal pregnancy progression.[9][80] Autoimmune disease may cause genetic abnormalities in embryos which in turn may lead to miscarriage.[81] As an example, Celiac disease increases the risk of miscarriage by an odds ratio of approximately 1.4.[30][31] A disruption in normal immune function can lead to the formation of antiphospholipid antibody syndrome. This will affect the ability to continue the pregnancy, and if a woman has repeated miscarriages, she can be tested for it.[42] Approximately 15% of recurrent miscarriages are related to immunologic factors.[82] The presence of anti-thyroid autoantibodies is associated with an increased risk with an odds ratio of 3.73 and 95% confidence interval 1.8–7.6.[83] Having lupus also increases the risk for miscarriage.[84]
Anatomical defects and trauma
Fifteen percent of women who have experienced three or more recurring miscarriages have some anatomical defect that prevents the pregnancy from being carried for the entire term.[85] The structure of the uterus has an effect on the ability to carry a child to term. Anatomical differences are common and can be congenital.
| Type of uterine structure |
Miscarriage rate associated with defect |
References |
|---|---|---|
| Bicornate uterus | 40–79% | [28][29] |
| Septate or unicornate | 34–88% | [28] |
| Arcuate | Unknown | [28] |
| Didelphys | 40% | [28] |
| Fibroids | Unknown | [32] |
In some women, cervical incompetence or cervical insufficiency occurs with the inability of the cervix to stay closed during the entire pregnancy.[33][39] It does not cause first trimester miscarriages. In the second trimester it is associated with an increased risk of miscarriage. It is identified after a premature birth has occurred at about 16–18 weeks into the pregnancy.[85] During the second trimester, major trauma can result in a miscarriage.[31]
Smoking
Tobacco (cigarette) smokers have an increased risk of miscarriage.[38][39] There is an increased risk regardless of which parent smokes, though the risk is higher when the gestational mother smokes.[40]
Morning sickness
Nausea and vomiting of pregnancy (NVP, or morning sickness) are associated with a decreased risk. Several possible causes have been suggested for morning sickness but there is still no agreement.[86] NVP may represent a defense mechanism which discourages the mother's ingestion of foods that are harmful to the fetus; according to this model, a lower frequency of miscarriage would be an expected consequence of the different food choices made by women experiencing NVP.[87]
Chemicals and occupational exposure
Chemical and occupational exposures may have some effect in pregnancy outcomes.[88] A cause and effect relationship almost can never be established. Those chemicals that are implicated in increasing the risk for miscarriage are DDT, lead,[89] formaldehyde, arsenic, benzene and ethylene oxide. Video display terminals and ultrasound have not been found to have an effect on the rates of miscarriage. In dental offices where nitrous oxide is used with the absence of anesthetic gas scavenging equipment, there is a greater risk of miscarriage. For women who work with cytotoxic antineoplastic chemotherapeutic agents there is a small increased risk of miscarriage. No increased risk for cosmetologists has been found.[42]
Other
Alcohol increases the risk of miscarriage.[32] Cocaine use increases the rate of miscarriage.[38] Some infections have been associated with miscarriage. These include Ureaplasma urealyticum, Mycoplasma hominis, group B streptococci, HIV-1, and syphilis. Infections of Chlamydia trachomatis, Camphylobacter fetus, and Toxoplasma gondii have not been found to be linked to miscarriage.[48]
Diagnosis
In the case of blood loss, pain, or both, transvaginal ultrasound is performed. If a viable intrauterine pregnancy is not found with ultrasound, blood tests (serial βHCG tests) can be performed to rule out ectopic pregnancy, which is a life-threatening situation.[90][91]
If hypotension, tachycardia, and anemia are discovered, exclusion of an ectopic pregnancy is important.[91]
A miscarriage may be confirmed by an obstetric ultrasound and by the examination of the passed tissue. When looking for microscopic pathologic symptoms, one looks for the products of conception. Microscopically, these include villi, trophoblast, fetal parts, and background gestational changes in the endometrium. When chromosomal abnormalities are found in more than one miscarriage, genetic testing of both parents may be done.[92]
Ultrasound criteria
A review article in The New England Journal of Medicine based on a consensus meeting of the Society of Radiologists in Ultrasound in America (SRU) has suggested that miscarriage should be diagnosed only if any of the following criteria are met upon ultrasonography visualization:[93]
| Miscarriaged diagnosed | Miscarriage suspected | References |
|---|---|---|
| Crown-rump length of at least 7 mm and no heartbeat. | Crown–rump length of less than 7 mm and no heartbeat. | [93][94] |
| Mean gestational sac diameter of at least 25 mm and no embryo. | Mean gestational sac diameter of 16–24 mm and no embryo. | [93][94] |
| Absence of embryo with heartbeat at least 2 weeks after an ultrasound scan that showed a gestational sac without a yolk sac. | Absence of embryo with heartbeat 7–13 days after an ultrasound scan that showed a gestational sac without a yolk sac. | [93][94] |
| Absence of embryo with heartbeat at least 11 days after an ultrasound scan that showed a gestational sac with a yolk sac. | Absence of embryo with heartbeat 7–10 days after a scan that showed a gestational sac with a yolk sac. | [93][94] |
| Absence of embryo at least 6 weeks after last menstrual period. | [93][94] | |
| Amniotic sac seen adjacent to yolk sac, and with no visible embryo. | [93][94] | |
| Yolk sac of more than 7 mm. | [93][94] | |
| Small gestational sac compared to embryo size (less than 5 mm difference between mean sac diameter and crown–rump length). | [93][94] |
Classification
A threatened miscarriage is any bleeding during the first half of pregnancy.[95] At investigation it may be found that the fetus remains viable and the pregnancy continues without further problems.
An anembryonic pregnancy (also called an "empty sac" or "blighted ovum") is a condition where the gestational sac develops normally, while the embryonic part of the pregnancy is either absent or stops growing very early. This accounts for approximately half of miscarriages. All other miscarriages are classified as embryonic miscarriages, meaning that there is an embryo present in the gestational sac. Half of embryonic miscarriages have aneuploidy (an abnormal number of chromosomes).[48]
An inevitable miscarriage occurs when the cervix has already dilated,[96] but the fetus has yet to be expelled. This usually will progress to a complete miscarriage. The fetus may or may not have cardiac activity.

A complete miscarriage is when all products of conception have been expelled; these may include the trophoblast, chorionic villi, gestational sac, yolk sac, and fetal pole (embryo); or later in pregnancy the fetus, umbilical cord, placenta, amniotic fluid, and amniotic membrane. The presence of a pregnancy test that is still positive as well as an empty uterus upon transvaginal ultrasonography does, however, fulfill the definition of pregnancy of unknown location. Therefore, there may be a need for follow-up pregnancy tests to ensure that there is no remaining pregnancy, including an ectopic pregnancy.
An incomplete miscarriage occurs when some products of conception have been passed, but some remains inside the uterus.[97] However, an increased distance between the uterine walls on transvaginal ultrasonography may also simply be an increased endometrial thickness and/or a polyp. The use of a Doppler ultrasound may be better in confirming the presence of significant retained products of conception in the uterine cavity.[98] In cases of uncertainty, ectopic pregnancy must be excluded using techniques like serial beta-hCG measurements.[98]
A missed miscarriage is when the embryo or fetus has died, but a miscarriage has not yet occurred. It is also referred to as delayed miscarriage, silent miscarriage, or missed abortion.[99][100]
A septic miscarriage occurs when the tissue from a missed or incomplete miscarriage becomes infected, which carries the risk of spreading infection (septicaemia) and can be fatal.[48]
Recurrent miscarriage ("recurrent pregnancy loss" (RPL) or "habitual abortion") is the occurrence of multiple consecutive miscarriages; the exact number used to diagnose recurrent miscarriage varies.[48] If the proportion of pregnancies ending in miscarriage is 15% and assuming that miscarriages are independent events,[101] then the probability of two consecutive miscarriages is 2.25% and the probability of three consecutive miscarriages is 0.34%. The occurrence of recurrent pregnancy loss is 1%.[101] A large majority (85%) of those who have had two miscarriages will conceive and carry normally afterward.[101]
The physical symptoms of a miscarriage vary according to the length of pregnancy, though most miscarriages cause pain or cramping. The size of blood clots and pregnancy tissue that are passed become larger with longer gestations. After 13 weeks' gestation, there is a higher risk of placenta retention.[102]
Prevention
Prevention of a miscarriage can sometimes be accomplished by decreasing risk factors.[11] This may include good prenatal care, avoiding drugs and alcohol, preventing infectious diseases, and avoiding x-rays.[11] Identifying the cause of the miscarriage may help prevent future pregnancy loss, especially in cases of recurrent miscarriage. Often there is little a person can do to prevent a miscarriage.[11] Vitamin supplementation before or during pregnancy has not been found to affect the risk of miscarriage.[103] Progesterone has been shown to prevent miscarriage in women with 1) vaginal bleeding early in their current pregnancy and 2) a previous history of miscarriage.[104]
Non-modifiable risk factors
Preventing a miscarriage in subsequent pregnancies may be enhanced with assessments of:
- Immune status[9][80]
- Chemical and occupational exposures[42]
- Anatomical defects[85][29]
- Pre-existing or acuired disease in pregnancy[78][34]
- Previous exposure to chemotherapy and radiation
- Medications[31][62][63][64][65][66]
- Surgical history[61]
- Endocrine disorders[41][109]
- Genetic abnormalities[28][29]
Modifiable risk factors
Maintaining a healthy weight and good pre-natal care can reduce the risk of miscarriage.[32] Some risk factors can be minimized by avoiding the following:
Management
Women who miscarry early in their pregnancy usually do not require any subsequent medical treatment but they can benefit from support and counseling.[25][110] Most early miscarriages will complete on their own; in other cases, medication treatment or aspiration of the products of conception can be used to remove remaining tissue.[111] While bed rest has been advocated to prevent miscarriage, this has not been found to be of benefit.[112][23] Those who are or who have experienced an abortion benefit from the use of careful medical language. Significant distress can often be managed by the ability of the clinician to clearly explain terms without suggesting that the woman or couple are somehow to blame.[113]
Evidence to support Rho(D) immune globulin after a spontaneous miscarriage is unclear.[114] In the UK, Rho(D) immune globulin is recommended in Rh-negative women after 12 weeks gestational age and before 12 weeks gestational age in those who need surgery or medication to complete the miscarriage.[115]
Methods
No treatment is necessary for a diagnosis of complete miscarriage (so long as ectopic pregnancy is ruled out). In cases of an incomplete miscarriage, empty sac, or missed abortion there are three treatment options: watchful waiting, medical management, and surgical treatment. With no treatment (watchful waiting), most miscarriages (65–80%) will pass naturally within two to six weeks.[116]This treatment avoids the possible side effects and complications of medications and surgery,[117]but increases the risk of mild bleeding, need for unplanned surgical treatment, and incomplete miscarriage. Medical treatment usually consists of using misoprostol (a prostaglandin) alone or in combination with mifepristone pre-treatment.[118]These medications help the uterus to contract and expel the remaining tissue out of the body. This works within a few days in 95% of cases.[116]Vacuum aspiration or sharp curettage can be used, though vacuum aspiration is lower-risk and more common.[116]
Delayed and incomplete miscarriage
In delayed or incomplete miscarriage, treatment depends on the amount of tissue remaining in the uterus. Treatment can include surgical removal of the tissue with vacuum aspiration or misoprostol.[119]Studies looking at the methods of anaesthesia for surgical management of incomplete miscarriage have not shown that any adaptation from normal practice is beneficial.[120]
Induced miscarriage
An induced abortion may be performed by a qualified healthcare provider for women who cannot continue the pregnancy.[121] Self-induced abortion performed by a woman or non-medical personnel can be dangerous and is still a cause of maternal mortality in some countries. In some locales it is illegal or carries heavy social stigma.[122] However, in the United States, many choose to self-induce or self-manage their abortion and have done so safely.[123]
Sex
Some organizations recommend delaying sex after a miscarriage until the bleeding has stopped to decrease the risk of infection.[124] However, there is not sufficient evidence for the routine use of antibiotic to try to avoid infection in incomplete abortion.[125] Others recommend delaying attempts at pregnancy until one period has occurred to make it easier to determine the dates of a subsequent pregnancy.[124] There is no evidence that getting pregnancy in that first cycle however affects outcomes and an early subsequent pregnancy may actually improve outcomes.[124][126]
Support
Organizations exist that provide information and counseling to help those who have had a miscarriage.[127] Family and friends often conduct a memorial or burial service. Hospitals also can provide support and help memorialize the event. Depending on locale others desire to have a private ceremony.[127] Providing appropriate support with frequent discussions and sympathetic counseling are part of evaluation and treatment. Those who experience unexplained miscarriage can be treated with emotional support.[110][113]
Outcomes
Psychological and emotional effects

Every woman's personal experience of miscarriage is different, and women who have more than one miscarriage may react differently to each event.[128]
In Western cultures since the 1980s,[128] medical providers assume that experiencing a miscarriage "is a major loss for all pregnant women".[110] A miscarriage can result in anxiety, depression or stress for those involved.[91][129][130] It can have an effect on the whole family.[131] Many of those experiencing a miscarriage go through a grieving process.[3][132][133] "Prenatal attachment" often exists that can be seen as parental sensitivity, love and preoccupation directed toward the unborn child.[134] Serious emotional impact is usually experienced immediately after the miscarriage.[3] Some may go through the same loss when an ectopic pregnancy is terminated.[32] In some, the realization of the loss can take weeks. Providing family support to those experiencing the loss can be challenging because some find comfort in talking about the miscarriage while others may find the event painful to discuss. The father can have the same sense of loss. Expressing feelings of grief and loss can sometimes be harder for men. Some women are able to begin planning their next pregnancy after a few weeks of having the miscarriage. For others, planning another pregnancy can be difficult.[127][124] Some facilities acknowledge the loss. Parents can name and hold their infant. They may be given mementos such as photos and footprints. Some conduct a funeral or memorial service. They may express the loss by planting a tree.[135]
Some health organizations recommend that sexual activity be delayed after the miscarriage. The menstrual cycle should resume after about three to four months.[127] Women report that they were dissatisfied with the care they received from physicians and nurses.[136]
Subsequent pregnancies
Some parents want to try to have a baby very soon after the miscarriage. The decision of trying to become pregnant again can be difficult. Reasons exist that may prompt parents to consider another pregnancy. For older mothers, there may be some sense of urgency. Other parents are optimistic that future pregnancies are likely to be successful. Many are hesitant and want to know about the risk of having another or more miscarriages. Some clinicians recommend that the women have one menstrual cycle before attempting another pregnancy. This is because the date of conception may be hard to determine. Also, the first menstrual cycle after a miscarriage can be much longer or shorter than expected. Parents may be advised to wait even longer if they have experienced late miscarriage or molar pregnancy, or are undergoing tests. Some parents wait for six months based upon recommendations from their health care provider.[124]
The risks of having another miscarriage vary according to the cause. The risk of having another miscarriage after a molar pregnancy is very low. The risk of another miscarriage is highest after the third miscarriage. Pre-conception care is available in some locales.[124]
Later cardiovascular disease
There is a significant association between miscarriage and later development of coronary artery disease, but not of cerebrovascular disease.[137][31]
Epidemiology
Among women who know they are pregnant, the miscarriage rate is roughly 10% to 20%, while rates among all fertilized zygotes are around 30% to 50%.[1][7][48][110] A 2012 review found the risk of miscarriage between 5 and 20 weeks from 11% to 22%.[138] Up to the 13th week of pregnancy, the risk of miscarriage each week was around 2%, dropping to 1% in week 14 and reducing slowly between 14 and 20 weeks.[138]
The precise rate is not known because a large number of miscarriages occur before pregnancies become established and before the woman is aware she is pregnant.[138] Additionally, those with bleeding in early pregnancy may seek medical care more often than those not experiencing bleeding.[138] Although some studies attempt to account for this by recruiting women who are planning pregnancies and testing for very early pregnancy, they still are not representative of the wider population.[138]
The prevalence of miscarriage increases with the age of both parents.[138][139][140] In a Danish register-based study where the prevalence of miscarriage was 11%, the prevalence rose from 9% at 22 years of age to 84% by 48 years of age.[141] Another, later study in 2013 found that when either parent was over the age of 40, the rate of known miscarriages doubled.[48]
In 2010, 50,000 inpatient admissions for miscarriage occurred in the UK.[14]
Terminology
Most affected women and family members refer to miscarriage as the loss of a baby, rather than an embryo or fetus, and healthcare providers are expected to respect and use the language that the person chooses.[113] Clinical terms can suggest blame, increase distress, and even cause anger. Terms that are known to cause distress in those experiencing miscarriage include:
- abortion (including spontaneous abortion) rather than miscarriage,
- habitual aborter rather than a woman experiencing recurrent pregnancy loss,
- products of conception rather than baby,
- blighted ovum rather than early pregnancy loss or delayed miscarriage,
- cervical incompetence rather than cervical weakness, and
- evacuation of retained products of conception (ERPC) rather than surgical management of miscarriage.[113]
Pregnancy loss is a broad term that is used for miscarriage, ectopic and molar pregnancies.[113] The term fetal death applies variably in different countries and contexts, sometimes incorporating weight, and gestational age from 16 weeks in Norway, 20 weeks in the US and Australia, 24 weeks in the UK to 26 weeks in Italy and Spain.[142][143][144] A fetus that died before birth after this gestational age may be referred to as a stillbirth.[142] Under UK law, all stillbirths should be registered,[145] although this does not apply to miscarriages.
History
The medical terminology applied to experiences during early pregnancy has changed over time.[146] Before the 1980s, health professionals used the phrase spontaneous abortion for a miscarriage and induced abortion for a termination of the pregnancy.[146][147] In the late 1980s and 1990s, doctors became more conscious of their language in relation to early pregnancy loss. Some medical authors advocated change to use of miscarriage instead of spontaneous abortion because they argued this would be more respectful and help ease a distressing experience.[148][149] The change was being recommended by some in the profession in Britain in the late 1990s.[150] In 2005 the European Society for Human Reproduction and Embryology (ESHRE) published a paper aiming to facilitate a revision of nomenclature used to describe early pregnancy events.[99]
Society and culture
Society's reactions to miscarriage has changed over time.[128] In the early 20th century, the focus was on the mother's physical health and the difficulties and disabilities that miscarriage could produce.[128] Other reactions, such as the expense of medical treatments and relief at ending an unwanted pregnancy, were also heard.[128] In the 1940s and 1950s, people were more likely to express relief, not because the miscarriage ended an unwanted or mistimed pregnancy, but because people believed that miscarriages were primarily caused by birth defects, and miscarrying meant that the family would not raise a child with disabilities.[128] The dominant attitude in the mid-century was that a miscarriage, although temporarily distressing, was a blessing in disguise for the family, and that another pregnancy and a healthier baby would soon follow, especially if women trusted physicians and reduced their anxieties.[128] Media articles were illustrated with pictures of babies, and magazine articles about miscarriage ended by introducing the healthy baby—usually a boy—that had shortly followed it.[128]
Beginning in the 1980s, miscarriage in the US was primarily framed in terms of the individual woman's personal emotional reaction, and especially her grief over a tragic outcome.[128] The subject was portrayed in the media with images of an empty crib or an isolated, grieving woman, and stories about miscarriage were published in general-interest media outlets, not just women's magazines or health magazines.[128] Family members were encouraged to grieve, to memorialize their losses through funerals and other rituals, and to think of themselves as being parents.[128] This shift to recognizing these emotional responses was partly due to medical and political successes, which created an expectation that pregnancies are typically planned and safe, and to women's demands that their emotional reactions no longer be dismissed by the medical establishments.[128] It also reinforces the pro-life movement's belief that human life begins at conception or early in pregnancy, and that motherhood is a desirable life goal.[128] The modern one-size-fits-all model of grief does not fit every woman's experience, and an expectation to perform grief creates unnecessary burdens for some women.[128] The reframing of miscarriage as a private emotional experience brought less awareness of miscarriage and a sense of silence around the subject, especially compared to the public discussion of miscarriage during campaigns for access to birth control during the early 20th century, or the public campaigns to prevent miscarriages, stillbirths, and infant deaths by reducing industrial pollution during the 1970s.[128][151]
In places where induced abortion is illegal or carries social stigma, suspicion may surround miscarriage, complicating an already sensitive issue.
In the 1960s, the use of the word miscarriage in Britain (instead of spontaneous abortion) occurred after changes in legislation.
Developments in ultrasound technology (in the early 1980s) allowed them to identify earlier miscarriages.[146]
According to French statutes, an infant born before the age of viability, determined to be 28 weeks, is not registered as a 'child'. If birth occurs after this, the infant is granted a certificate that allows women who have given birth to a stillborn child, to have a symbolic record of that child. This certificate can include a registered and given name with the purpose of allowing a funeral and acknowledgement of the event.[152][153][154]
Other animals
Miscarriage occurs in all animals that experience pregnancy, though in such contexts it is more commonly referred to as a "spontaneous abortion" (the two terms are synonymous). There are a variety of known risk factors in non-human animals. For example, in sheep, miscarriage may be caused by crowding through doors, or being chased by dogs.[155] In cows, spontaneous abortion may be caused by contagious disease, such as brucellosis or Campylobacter, but often can be controlled by vaccination.[156] In many species of sharks and rays, stress induced miscarriage occurs frequently on capture.[157]
Other diseases are also known to make animals susceptible to miscarriage. Spontaneous abortion occurs in pregnant prairie voles when their mate is removed and they are exposed to a new male,[158] an example of the Bruce effect, although this effect is seen less in wild populations than in the laboratory.[159] Female mice who had spontaneous abortions showed a sharp rise in the amount of time spent with unfamiliar males preceding the abortion than those who did not.[160]
References
- The Johns Hopkins Manual of Gynecology and Obstetrics (4 ed.). Lippincott Williams & Wilkins. 2012. pp. 438–439. ISBN 9781451148015. Archived from the original on September 10, 2017.
- "Spontaneous Abortion - Gynecology and Obstetrics". Merck Manuals Professional Edition. Retrieved May 5, 2018.
- Robinson GE (January 2014). "Pregnancy loss". Best Practice & Research. Clinical Obstetrics & Gynaecology. 28 (1): 169–78. doi:10.1016/j.bpobgyn.2013.08.012. PMID 24047642.
- "What is pregnancy loss/miscarriage?". www.nichd.nih.gov/. July 15, 2013. Archived from the original on April 2, 2015. Retrieved March 14, 2015.
- Vaiman D (2015). "Genetic regulation of recurrent spontaneous abortion in humans". Biomedical Journal. 38 (1): 11–24. doi:10.4103/2319-4170.133777. PMID 25179715.
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ (October 2011). "Reproductive outcomes in women with congenital uterine anomalies: a systematic review". Ultrasound in Obstetrics & Gynecology. 38 (4): 371–82. doi:10.1002/uog.10056. PMID 21830244.
- "How many people are affected by or at risk for pregnancy loss or miscarriage?". www.nichd.nih.gov. July 15, 2013. Archived from the original on April 2, 2015. Retrieved March 14, 2015.
- Oliver A, Overton C (May 2014). "Diagnosis and management of miscarriage". The Practitioner. 258 (1771): 25–8, 3. PMID 25055407.
- Carp HJ, Selmi C, Shoenfeld Y (May 2012). "The autoimmune bases of infertility and pregnancy loss". Journal of Autoimmunity (Review). 38 (2–3): J266-74. doi:10.1016/j.jaut.2011.11.016. PMID 22284905.
- "How do health care providers diagnose pregnancy loss or miscarriage?". www.nichd.nih.gov/. July 15, 2013. Retrieved March 14, 2015.
- "Is there a cure for pregnancy loss/miscarriage?". www.nichd.nih.gov/. October 21, 2013. Archived from the original on April 2, 2015. Retrieved March 14, 2015.
- "What are the treatments for pregnancy loss/miscarriage?". www.nichd.nih.gov. July 15, 2013. Archived from the original on April 2, 2015. Retrieved March 14, 2015.
- "Stillbirth: Overview". NICHD. September 23, 2014. Archived from the original on October 5, 2016. Retrieved October 4, 2016.
- Radford EJ, Hughes M (June 2015). "Women's experiences of early miscarriage: implications for nursing care". Journal of Clinical Nursing. 24 (11–12): 1457–65. doi:10.1111/jocn.12781. PMID 25662397.
- "What are the symptoms of pregnancy loss/miscarriage?". www.nichd.nih.gov/. July 15, 2013. Archived from the original on April 2, 2015. Retrieved March 14, 2015.
- "Glossary | womenshealth.gov". womenshealth.gov. January 10, 2017. Retrieved September 11, 2017.

- Tunçalp O, Gülmezoglu AM, Souza JP (September 2010). "Surgical procedures for evacuating incomplete miscarriage". The Cochrane Database of Systematic Reviews (9): CD001993. doi:10.1002/14651858.CD001993.pub2. PMC 7064046. PMID 20824830.
- National Coordinating Centre for Women's and Children's Health (UK) (December 2012). "Ectopic Pregnancy and Miscarriage: Diagnosis and Initial Management in Early Pregnancy of Ectopic Pregnancy and Miscarriage". NICE Clinical Guidelines, No. 154. Royal College of Obstetricians and Gynaecologists. Archived from the original on October 20, 2013. Retrieved July 4, 2013.
- Garrido-Gimenez C, Alijotas-Reig J (March 2015). "Recurrent miscarriage: causes, evaluation and management". Postgraduate Medical Journal. 91 (1073): 151–62. doi:10.1136/postgradmedj-2014-132672. PMID 25681385.
- Greaves I, Porter K, Hodgetts TJ, Woollard M (2005). Emergency Care: A Textbook for Paramedics. London: Elsevier Health Sciences. p. 506. ISBN 978-0-7020-2586-0. Archived from the original on April 26, 2016.
- Moscrop A (December 1, 2013). "'Miscarriage or abortion?' Understanding the medical language of pregnancy loss in Britain; a historical perspective". Medical humanities. 39 (2): 98–104. doi:10.1136/medhum-2012-010284. PMID 23429567.CS1 maint: extra punctuation (link)
- "How do health care providers diagnose pregnancy loss or miscarriage?". www.nichd.nih.gov. Retrieved November 7, 2017.
- Hoffman, p. 176.
- Li L, Dou L, Leung PC, Wang CC (May 2012). "Chinese herbal medicines for threatened miscarriage". The Cochrane Database of Systematic Reviews (5): CD008510. doi:10.1002/14651858.cd008510.pub2. PMID 22592730.
- "Miscarriage | Miscarriage Symptoms | MedlinePlus". Archived from the original on July 28, 2017. Retrieved September 9, 2017.

- Lee HJ, Norwitz E, Lee B (August 2018). "Relationship between threatened miscarriage and gestational diabetes mellitus". BMC Pregnancy and Childbirth. 18 (1): 318. doi:10.1186/s12884-018-1955-2. PMC 6080503. PMID 30081861.
- Everett C (July 1997). "Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice". BMJ. 315 (7099): 32–4. doi:10.1136/bmj.315.7099.32. PMC 2127042. PMID 9233324.
- Hoffman, p. 181–182.
- Ali O, Hakimi I, Chanana A, Habib MA, Guelzim K, Kouach J, et al. (2015). "[Term pegnancy on septate uterus: report of a case and review of the literature]". The Pan African Medical Journal. 22: 219. doi:10.11604/pamj.2015.22.219.7790. PMC 4760728. PMID 26955410.
- Tersigni C, Castellani R, de Waure C, Fattorossi A, De Spirito M, Gasbarrini A, et al. (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–93. doi:10.1093/humupd/dmu007. PMID 24619876.
- Hoffman, p. 172.
- Choices, NHS (December 7, 2017). "Miscarriage - Causes - NHS Choices". www.nhs.uk.
- American College of Obstetricians Gynecologists (February 2014). "ACOG Practice Bulletin No.142: Cerclage for the management of cervical insufficiency". Obstetrics and Gynecology. 123 (2 Pt 1): 372–9. doi:10.1097/01.AOG.0000443276.68274.cc. PMID 24451674.
- Lis R, Rowhani-Rahbar A, Manhart LE (August 2015). "Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis". Clinical Infectious Diseases. 61 (3): 418–26. doi:10.1093/cid/civ312. PMID 25900174.
- Tabor A, Alfirevic Z (2010). "Update on procedure-related risks for prenatal diagnosis techniques". Fetal Diagnosis and Therapy. 27 (1): 1–7. doi:10.1159/000271995. PMID 20051662.
- Agarwal K, Alfirevic Z (August 2012). "Pregnancy loss after chorionic villus sampling and genetic amniocentesis in twin pregnancies: a systematic review". Ultrasound in Obstetrics & Gynecology. 40 (2): 128–34. doi:10.1002/uog.10152. PMID 22125091.
- Alfirevic Z, Navaratnam K, Mujezinovic F (September 2017). "Amniocentesis and chorionic villus sampling for prenatal diagnosis". The Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd. 9: CD003252. doi:10.1002/14651858.cd003252.pub2. PMC 6483702. PMID 28869276.
- Ness RB, Grisso JA, Hirschinger N, Markovic N, Shaw LM, Day NL, Kline J (February 1999). "Cocaine and tobacco use and the risk of spontaneous abortion". The New England Journal of Medicine. 340 (5): 333–9. doi:10.1056/NEJM199902043400501. PMID 9929522.
- Choices, NHS. "Miscarriage - Causes - NHS Choices". www.nhs.uk. Retrieved September 10, 2017.
- Venners SA, Wang X, Chen C, Wang L, Chen D, Guang W, et al. (May 2004). "Paternal smoking and pregnancy loss: a prospective study using a biomarker of pregnancy". American Journal of Epidemiology. 159 (10): 993–1001. doi:10.1093/aje/kwh128. PMID 15128612.
- Hoffman, p. 173.
- Hoffman, p. 272.
- Chavarro JE, Rich-Edwards JW, Gaskins AJ, Farland LV, Terry KL, Zhang C, Missmer SA (September 2016). "Contributions of the Nurses' Health Studies to Reproductive Health Research". American Journal of Public Health. 106 (9): 1669–76. doi:10.2105/AJPH.2016.303350. PMC 4981818. PMID 27459445.(review)
- Acién P, Acién M (January 1, 2016). "The presentation and management of complex female genital malformations". Human Reproduction Update. 22 (1): 48–69. doi:10.1093/humupd/dmv048. PMID 26537987.
- Hoffman, p. 171.
- "Archived copy" (PDF). Archived from the original (PDF) on September 14, 2017. Retrieved September 14, 2017.CS1 maint: archived copy as title (link)
- Rosenthal, M. Sara (1999). "The Second Trimester". The Gynecological Sourcebook. WebMD. Archived from the original on December 1, 2006. Retrieved December 18, 2006.
- Cunningham F, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, Sheffield JS (2013). "Abortion". Williams Obstetrics. McGraw-Hill. p. 5.
- "Blighted Ovum: Symptoms, Causes and Prevention". American Pregnancy Association. April 26, 2012. Archived from the original on July 25, 2017. Retrieved September 9, 2017.
- "Blighted ovum: What causes it?". Mayo Clinic. Archived from the original on July 20, 2017. Retrieved September 9, 2017.
- Wilcox AJ, Baird DD, Weinberg CR (June 1999). "Time of implantation of the conceptus and loss of pregnancy". The New England Journal of Medicine. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- Condous, edited by Tom Bourne, George (2006). Handbook of early pregnancy care. London: Informa Healthcare. pp. 28–29. ISBN 9780203016213. Archived from the original on September 10, 2017.CS1 maint: extra text: authors list (link)
- Kajii T, Ferrier A, Niikawa N, Takahara H, Ohama K, Avirachan S (1980). "Anatomic and chromosomal anomalies in 639 spontaneous abortuses". Human Genetics. 55 (1): 87–98. doi:10.1007/BF00329132. PMID 7450760.
- "Pregnancy Over Age 30". MUSC Children's Hospital. Archived from the original on November 13, 2006. Retrieved December 18, 2006.
- Bukulmez O, Arici A (December 2004). "Luteal phase defect: myth or reality". Obstetrics and Gynecology Clinics of North America. 31 (4): 727–44, ix. doi:10.1016/j.ogc.2004.08.007. PMID 15550332.
- Bray I, Gunnell D, Davey Smith G (October 2006). "Advanced paternal age: how old is too old?". Journal of Epidemiology and Community Health. 60 (10): 851–3. doi:10.1136/jech.2005.045179. PMC 2566050. PMID 16973530.
- Hoffman, p. 175.
- Balogun OO, da Silva Lopes K, Ota E, Takemoto Y, Rumbold A, Takegata M, Mori R (May 2016). "Vitamin supplementation for preventing miscarriage". The Cochrane Database of Systematic Reviews (5): CD004073. doi:10.1002/14651858.cd004073.pub4. PMC 7104220. PMID 27150280.
- Fred F. Ferri (2017). Ferri's Clinical Advisor 2017. Elsevier. p. 1198. ISBN 978-0-323-28048-8.
- Sumita Mehta; Bindiya Gupta (2018). Recurrent Pregnancy Loss. Springer. p. 185. ISBN 978-981-10-7337-3.
- Hoffman, pp. 172–173.
- Ross LE, Grigoriadis S, Mamisashvili L, Vonderporten EH, Roerecke M, Rehm J, et al. (April 2013). "Selected pregnancy and delivery outcomes after exposure to antidepressant medication: a systematic review and meta-analysis". JAMA Psychiatry. 70 (4): 436–43. doi:10.1001/jamapsychiatry.2013.684. PMID 23446732.
- Dalke KB, Wenzel A, Kim DR (June 2016). "Depression and Anxiety During Pregnancy: Evaluating the Literature in Support of Clinical Risk-Benefit Decision-Making". Current Psychiatry Reports. 18 (6): 59. doi:10.1007/s11920-016-0698-x. PMID 27091646.
- Broy P, Bérard A (January 2010). "Gestational exposure to antidepressants and the risk of spontaneous abortion: a review". Current Drug Delivery. 7 (1): 76–92. doi:10.2174/156720110790396508. PMID 19863482.
- Nakhai-Pour HR, Broy P, Bérard A (July 2010). "Use of antidepressants during pregnancy and the risk of spontaneous abortion". CMAJ. 182 (10): 1031–7. doi:10.1503/cmaj.091208. PMC 2900326. PMID 20513781.
- Yonkers KA, Blackwell KA, Glover J, Forray A (January 1, 2014). "Antidepressant use in pregnant and postpartum women". Annual Review of Clinical Psychology. 10 (1): 369–92. doi:10.1146/annurev-clinpsy-032813-153626. PMC 4138492. PMID 24313569.
- Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. (June 2019). "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 73 (24): 3168–3209. doi:10.1016/j.jacc.2018.11.002. PMID 30423391.
- Hoffman, p. 72.
- Racicot K, Mor G (May 2017). "Risks associated with viral infections during pregnancy". The Journal of Clinical Investigation. 127 (5): 1591–1599. doi:10.1172/JCI87490. PMC 5409792. PMID 28459427.
- Bozzo P, Narducci A, Einarson A (May 2011). "Vaccination during pregnancy". Canadian Family Physician. 57 (5): 555–7. PMC 3093587. PMID 21571717.
- "Pregnancy Guidelines and Recommendations by Vaccine | CDC". www.cdc.gov. April 19, 2019. Retrieved August 1, 2019.
- "List of Vaccines | CDC". www.cdc.gov. April 15, 2019. Retrieved August 6, 2019.
- "Vaccine Types | Vaccines". www.vaccines.gov. Retrieved August 6, 2019.
- Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE (February 2002). "Effects of metformin on early pregnancy loss in the polycystic ovary syndrome". The Journal of Clinical Endocrinology and Metabolism. 87 (2): 524–9. doi:10.1210/jc.87.2.524. PMID 11836280.
- Khattab S, Mohsen IA, Foutouh IA, Ramadan A, Moaz M, Al-Inany H (December 2006). "Metformin reduces abortion in pregnant women with polycystic ovary syndrome". Gynecological Endocrinology. 22 (12): 680–4. doi:10.1080/09513590601010508. PMID 17162710.
- Royal College of Obstetricians and Gynaecologists (December 2007). "Long-term consequences of polycystic ovarian syndrome" (PDF). Green-top Guideline No. 27. Royal College of Obstetricians and Gynaecologists. Archived from the original (PDF) on July 10, 2010. Retrieved July 2, 2013.
- Lilja AE, Mathiesen ER (2006). "Polycystic ovary syndrome and metformin in pregnancy". Acta Obstetricia et Gynecologica Scandinavica. 85 (7): 861–8. doi:10.1080/00016340600780441. PMID 16817087.
- Hoffman, p. 174.
- "Trying to conceive | womenshealth.gov". womenshealth.gov. December 13, 2016. Retrieved September 11, 2017.

- Gleicher N, Weghofer A, Barad D (2007). "Female infertility due to abnormal autoimmunity: Frequently overlooked and greatly underappreciated. Part II". Expert Review of Obstetrics & Gynecology. 2 (4): 465–75. doi:10.1586/17474108.2.4.465.
- Gleicher N, Weghofer A, Barad DH (April 2011). "Do chromosomally abnormal pregnancies really preclude autoimmune etiologies of spontaneous miscarriages?". Autoimmunity Reviews. 10 (6): 361–3. doi:10.1016/j.autrev.2010.12.004. PMID 21195806.
- Hoffman, p. 182.
- van den Boogaard E, Vissenberg R, Land JA, van Wely M, van der Post JA, Goddijn M, Bisschop PH (2011). "Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: a systematic review". Human Reproduction Update. 17 (5): 605–19. doi:10.1093/humupd/dmr024. PMID 21622978.
- "Pregnancy and lupus". womenshealth.gov. April 20, 2017. Retrieved September 11, 2017.
- Hoffman, p. 181.
- Koren G (December 2014). "Treating morning sickness in the United States--changes in prescribing are needed". American Journal of Obstetrics and Gynecology. 211 (6): 602–6. doi:10.1016/j.ajog.2014.08.017. PMID 25151184.
- Haviland WA, Prins HE, Walrath, McBride B (2016). "12. Human Adaptation to Changing World". Anthropology: The Human Challenge. Cengage Learning. p. 31. ISBN 9781305863354.
- Snijder CA, Roeleveld N, Te Velde E, Steegers EA, Raat H, Hofman A, et al. (March 2012). "Occupational exposure to chemicals and fetal growth: the Generation R Study". Human Reproduction. 27 (3): 910–20. doi:10.1093/humrep/der437. PMC 3279127. PMID 22215632.
- Krieg SA, Shahine LK, Lathi RB (September 2016). "Environmental exposure to endocrine-disrupting chemicals and miscarriage". Fertility and Sterility. 106 (4): 941–7. doi:10.1016/j.fertnstert.2016.06.043. PMID 27473347.
- Condous G, Okaro E, Khalid A, Bourne T (June 2005). "Do we need to follow up complete miscarriages with serum human chorionic gonadotrophin levels?". BJOG. 112 (6): 827–9. doi:10.1111/j.1471-0528.2004.00542.x. PMID 15924545.
- BMJ Best Practice. "Miscarriage". us.bestpractice.bmj.com. Ida Muslim, Jothi Doraiswamy, Acknowledgements. Retrieved October 8, 2017.
- Royal College of Obstetricians and Gynaecologists (RCOG) (April 2011). "The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage" (PDF). Green-top Guideline No. 17. Royal College of Obstetricians and Gynaecologists (RCOG). Archived from the original (PDF) on July 5, 2013. Retrieved July 2, 2013.
- Doubilet PM, Benson CB, Bourne T, Blaivas M, Barnhart KT, Benacerraf BR, et al. (October 2013). "Diagnostic criteria for nonviable pregnancy early in the first trimester". The New England Journal of Medicine. 369 (15): 1443–51. doi:10.1056/NEJMra1302417. PMID 24106937.
- Hoffman, pp. 173–4.
- Lee HJ, Norwitz E, Lee B (August 2018). "Relationship between threatened miscarriage and gestational diabetes mellitus". BMC Pregnancy and Childbirth. 18 (1): 318. doi:10.1186/s12884-018-1955-2. PMC 6080503. PMID 30081861.
- Stead L, Stead SM, Kaufman M, Suarez L (2006). First Aid for The Obstetrics and Gynecology Clerkship. New York: McGraw-Hill. p. 138. ISBN 978-0-07-144874-1.
- MedlinePlus (October 25, 2004). "Abortion – incomplete". Medical Encyclopedia. Archived from the original on April 25, 2006. Retrieved May 24, 2006.
- Kirk E, Bottomley C, Bourne T (2013). "Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location". Human Reproduction Update. 20 (2): 250–61. doi:10.1093/humupd/dmt047. PMID 24101604.
- Farquharson RG, Jauniaux E, Exalto N (November 2005). "Updated and revised nomenclature for description of early pregnancy events". Human Reproduction. 20 (11): 3008–11. doi:10.1093/humrep/dei167. PMID 16006453.
- Hutchon DJ (June 1997). "Missed abortion versus delayed miscarriage". British Journal of Obstetrics and Gynaecology. 104 (6): 753. doi:10.1111/j.1471-0528.1997.tb11994.x. PMID 9197887.
- Royal College of Obstetricians and Gynaecologists (May 2003). "The investigation and treatment of couples with recurrent miscarriage". Green-top Guideline No. 17. Archived from the original on January 4, 2011. Retrieved October 20, 2010.
- Home page at www.birth.com.au (October 2004). "miscarriage". Archived from the original on December 1, 2008. Retrieved January 3, 2014.
- Balogun OO, da Silva Lopes K, Ota E, Takemoto Y, Rumbold A, Takegata M, Mori R (May 2016). "Vitamin supplementation for preventing miscarriage". The Cochrane Database of Systematic Reviews. 5 (5): CD004073. doi:10.1002/14651858.CD004073.pub4. PMC 7104220. PMID 27150280.
- https://www.journalslibrary.nihr.ac.uk/hta/hta24330/#/full-report
- Boomsma CM, Fauser BC, Macklon NS (January 2008). "Pregnancy complications in women with polycystic ovary syndrome". Seminars in Reproductive Medicine. 26 (1): 72–84. doi:10.1055/s-2007-992927. PMID 18181085.
- Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE (February 2002). "Effects of metformin on early pregnancy loss in the polycystic ovary syndrome". The Journal of Clinical Endocrinology and Metabolism. 87 (2): 524–9. doi:10.1210/jc.87.2.524. PMID 11836280.
- Khattab S, Mohsen IA, Foutouh IA, Ramadan A, Moaz M, Al-Inany H (December 2006). "Metformin reduces abortion in pregnant women with polycystic ovary syndrome". Gynecological Endocrinology. 22 (12): 680–4. doi:10.1080/09513590601010508. PMID 17162710.
- Lilja AE, Mathiesen ER (2006). "Polycystic ovary syndrome and metformin in pregnancy". Acta Obstetricia et Gynecologica Scandinavica. 85 (7): 861–8. doi:10.1080/00016340600780441. PMID 16817087.
- Mills JL, Simpson JL, Driscoll SG, Jovanovic-Peterson L, Van Allen M, Aarons JH, et al. (December 1988). "Incidence of spontaneous abortion among normal women and insulin-dependent diabetic women whose pregnancies were identified within 21 days of conception". The New England Journal of Medicine. 319 (25): 1617–23. doi:10.1056/NEJM198812223192501. PMID 3200277.
- Jeve YB, Davies W (July 2014). "Evidence-based management of recurrent miscarriages". Journal of Human Reproductive Sciences. 7 (3): 159–69. doi:10.4103/0974-1208.142475. PMC 4229790. PMID 25395740.
- "Understanding early miscarriage". BabyCenter, L.L.C. January 2017. Archived from the original on September 5, 2017. Retrieved June 4, 2017.
- McCall CA, Grimes DA, Lyerly AD (June 2013). ""Therapeutic" bed rest in pregnancy: unethical and unsupported by data". Obstetrics and Gynecology. 121 (6): 1305–8. doi:10.1097/AOG.0b013e318293f12f. PMID 23812466.
- Christiansen O (2014). Recurrent pregnancy loss. Chichester, West Sussex, UK: John Wiley & Sons. pp. 98–99. ISBN 9780470672945.
It is important to bear in mind that some clinical terms can cause great distress and even anger. It is not acceptable to use the term "abortion" for miscarriage, despite its historical clinical prevalence. To the lay person, "abortion" means the elective termination of pregnancy and while they may have no theoretical objections to that procedure, they are likely to be distressed and even angered at its use in their situation. "Miscarriage" (qualified by adjectives such as recurrent, delayed, early, late, etc.) is easily understood and well accepted.
- Karanth L, Jaafar SH, Kanagasabai S, Nair NS, Barua A (March 2013). "Anti-D administration after spontaneous miscarriage for preventing Rhesus alloimmunisation". The Cochrane Database of Systematic Reviews. 3 (3): CD009617. doi:10.1002/14651858.CD009617.pub2. PMID 23543581.
- Royal College of Obstetric and Gynecologists (March 2011). "The Use of Anti-D Immunoglobulin for Rhesus D Prophylaxis" (PDF). p. 5. Archived from the original (PDF) on November 28, 2014. Retrieved September 25, 2014.
- Kripke C (October 2006). "Expectant management vs. surgical treatment for miscarriage". American Family Physician. 74 (7): 1125–6. PMID 17039747. Archived from the original on May 25, 2014.
- Tang OS, Ho PC (December 2006). "The use of misoprostol for early pregnancy failure". Current Opinion in Obstetrics & Gynecology. 18 (6): 581–6. doi:10.1097/GCO.0b013e32800feedb. PMID 17099326.
- Schreiber CA, Creinin MD, Atrio J, Sonalkar S, Ratcliffe SJ, Barnhart KT (June 2018). "Mifepristone Pretreatment for the Medical Management of Early Pregnancy Loss". The New England Journal of Medicine. 378 (23): 2161–2170. doi:10.1056/NEJMoa1715726. PMC 6437668. PMID 29874535.
- Babigumira JB, Vlassoff M, Ahimbisibwe A, Stergachis A (January 1, 2015). Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds.). Surgery for Family Planning, Abortion, and Postabortion Care. Washington (DC): The International Bank for Reconstruction and Development / The World Bank. doi:10.1596/978-1-4648-0346-8_ch7. ISBN 9781464803468. PMID 26741012. Archived from the original on September 10, 2017.
- Calvache JA, Delgado-Noguera MF, Lesaffre E, Stolker RJ (April 2012). "Anaesthesia for evacuation of incomplete miscarriage". The Cochrane Database of Systematic Reviews (4): CD008681. doi:10.1002/14651858.CD008681.pub2. PMID 22513963.
- Borgatta, L (December 2014). "Labor Induction Termination of Pregnancy". Global Library of Women's Medicine. GLOWM.10444. doi:10.3843/GLOWM.10444. Archived from the original on September 24, 2015. Retrieved September 25, 2015.
- Haddad LB, Nour NM (2009). "Unsafe abortion: unnecessary maternal mortality". Reviews in Obstetrics & Gynecology. 2 (2): 122–6. PMC 2709326. PMID 19609407.
- "Decriminalization of Self-Induced Abortion - ACOG". www.acog.org. Retrieved September 12, 2019.
- "Thinking About Another Pregnancy" (PDF). Miscarriage Association. 2013. Archived (PDF) from the original on September 5, 2017. Retrieved September 4, 2017.
- May W, Gülmezoglu AM, Ba-Thike K (October 2007). "Antibiotics for incomplete abortion". The Cochrane Database of Systematic Reviews (4): CD001779. doi:10.1002/14651858.CD001779.pub2. PMID 17943756.
- "Trying to conceive soon after a pregnancy loss may increase chances of live birth". National Institutes of Health (NIH). January 12, 2016. Retrieved September 1, 2019.
- Choices, NHS. "Miscarriage - Afterwards - NHS Choices". www.nhs.uk. Archived from the original on September 5, 2017. Retrieved September 5, 2017.
- Reagan LJ (2003). "From Hazard to Blessing to Tragedy: Representations of Miscarriage in Twentieth-Century America". Feminist Studies. 29 (2): 357–378. JSTOR 3178514.
- Hunter A, Tussis L, MacBeth A (December 2017). "The presence of anxiety, depression and stress in women and their partners during pregnancies following perinatal loss: A meta-analysis" (PDF). Journal of Affective Disorders. 223: 153–164. doi:10.1016/j.jad.2017.07.004. PMID 28755623.
- Vismara L (2017). "Perspectives on perinatal stressful and traumatic experiences (review)". European Journal of Trauma & Dissociation. 1 (2): 111–120. doi:10.1016/j.ejtd.2017.03.006.
- Garrido-Gimenez C, Alijotas-Reig J (March 2015). "Recurrent miscarriage: causes, evaluation and management". Postgraduate Medical Journal. 91 (1073): 151–62. doi:10.1136/postgradmedj-2014-132672. PMID 25681385. Archived from the original on September 10, 2017.
- "13 Things To Know About Grief After Miscarriage or Loss". Postpartum Progress. May 16, 2013. Archived from the original on September 9, 2017. Retrieved September 9, 2017.
- "Grief Issues Special to Miscarriage – the broken bond". www.miscarriagesupport.org.nz. Archived from the original on July 4, 2017. Retrieved September 9, 2017.
- Christiansen DM (February 2017). "Posttraumatic stress disorder in parents following infant death: A systematic review". Clinical Psychology Review. 51: 60–74. doi:10.1016/j.cpr.2016.10.007. PMID 27838460.
- Emanuela Q (2013). Becoming Parents and Overcoming Obstacles : Understanding the Experience of Miscarriage, Premature Births, Infertility, and Postnatal Depression. Karnac Books. p. 63. ISBN 9781782200185. OCLC 858653965.
- Robinson J (March 1, 2014). "Provision of information and support to women who have suffered an early miscarriage (review)". British Journal of Midwifery. 22 (3): 175–180. doi:10.12968/bjom.2014.22.3.175. ISSN 0969-4900.
- Oliver-Williams CT, Heydon EE, Smith GC, Wood AM (November 2013). "Miscarriage and future maternal cardiovascular disease: a systematic review and meta-analysis". Heart. 99 (22): 1636–44. doi:10.1136/heartjnl-2012-303237. PMC 3812894. PMID 23539554.
- Ammon Avalos L, Galindo C, Li DK (June 2012). "A systematic review to calculate background miscarriage rates using life table analysis". Birth Defects Research. Part A, Clinical and Molecular Teratology. 94 (6): 417–23. doi:10.1002/bdra.23014. PMID 22511535.
- Kleinhaus K, Perrin M, Friedlander Y, Paltiel O, Malaspina D, Harlap S (August 2006). "Paternal age and spontaneous abortion". Obstetrics and Gynecology. 108 (2): 369–77. doi:10.1097/01.AOG.0000224606.26514.3a. PMID 16880308.
- Slama R, Bouyer J, Windham G, Fenster L, Werwatz A, Swan SH (May 2005). "Influence of paternal age on the risk of spontaneous abortion". American Journal of Epidemiology. 161 (9): 816–23. doi:10.1093/aje/kwi097. PMID 15840613.
- Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M (June 2000). "Maternal age and fetal loss: population based register linkage study". BMJ. 320 (7251): 1708–12. doi:10.1136/bmj.320.7251.1708. PMC 27416. PMID 10864550.
- Mohangoo AD, Blondel B, Gissler M, Velebil P, Macfarlane A, Zeitlin J (2013). "International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age?". PLOS ONE. 8 (5): e64869. Bibcode:2013PLoSO...864869M. doi:10.1371/journal.pone.0064869. PMC 3658983. PMID 23700489.
- Li Z, Zeki R, Hilder L, Sullivan EA (2012). "Australia's Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government. Archived from the original on July 18, 2013. Retrieved July 4, 2013.
- Royal College of Obstetricians & Gynaecologists UK (April 2001). "Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists UK. Archived from the original on November 5, 2013. Retrieved July 4, 2013.
- "Register a stillbirth - GOV.UK". www.gov.uk. Archived from the original on September 5, 2017. Retrieved September 5, 2017.
- Moscrop A (December 2013). "'Miscarriage or abortion?' Understanding the medical language of pregnancy loss in Britain; a historical perspective". Medical Humanities. 39 (2): 98–104. doi:10.1136/medhum-2012-010284. PMC 3841747. PMID 23429567.
- "Standard terminology for reporting of reproductive health statistics in the United States". Public Health Reports. 103 (5): 464–71. 1988. PMC 1478116. PMID 3140271.
- Beard RW, Mowbray JF, Pinker GD (November 1985). "Miscarriage or abortion". Lancet. 2 (8464): 1122–3. doi:10.1016/S0140-6736(85)90709-3. PMID 2865589.
- Hutchon DJ, Cooper S (October 1998). "Terminology for early pregnancy loss must be changed". BMJ. 317 (7165): 1081. doi:10.1136/bmj.317.7165.1081. PMC 1114078. PMID 9774309.
- Hutchon DJ, Cooper S (October 1998). "Terminology for early pregnancy loss must be changed". BMJ. 317 (7165): 1081. doi:10.1136/bmj.317.7165.1081. PMC 1114078. PMID 9774309.
- Blei D. "The History of Talking About Miscarriage". The Cut. Retrieved April 26, 2018.
- Communiqué de presse de Rachida Dati, Garde des Sceaux, ministre de la Justice et de Roselyne Bachelot-Narquin, ministre de la Santé, de la Jeunesse, des Sports et de la Vie associative, « Possibilité de demande d’un acte d’enfant sans vie », 22 août 2008, lire en ligne Archived April 19, 2012, at the Wayback Machine
- "Accueil Particuliers | service-public.fr". www.service-public.fr (in French). Retrieved November 4, 2017.
- Décret n°74-449 du 15 mai 1974 relatif au livret de famille et à l'information des futurs époux sur le droit de la famille - Article 9, May 15, 1974, retrieved November 4, 2017
- Spencer, James. Sheep Husbandry in Canada Archived September 24, 2015, at the Wayback Machine, page 124 (1911).
- "Beef cattle and Beef production: Management and Husbandry of Beef Cattle" Archived January 1, 2009, at the Wayback Machine, Encyclopaedia of New Zealand (1966).
- Adams KR, Fetterplace LC, Davis AR, Taylor MD, Knott NA (January 2018). "Sharks, rays and abortion: The prevalence of capture-induced parturition in elasmobranchs". Biological Conservation. 217: 11–27. doi:10.1016/j.biocon.2017.10.010.
- Fraser-Smith AC (March 1975). "Male-induced pregnancy termination in the prairie vole, Microtus ochrogaster". Science. 187 (4182): 1211–3. Bibcode:1975Sci...187.1211S. doi:10.1126/science.1114340. PMID 1114340.
- Mahady S, Wolff J (2002). "A field test of the Bruce effect in the monogamous prairie vole (Microtus ochrogaster)". Behavioral Ecology and Sociobiology. 52 (1): 31–7. doi:10.1007/s00265-002-0484-0. JSTOR 4602102.
- Becker SD, Hurst JL (May 2009). "Female behaviour plays a critical role in controlling murine pregnancy block". Proceedings. Biological Sciences. 276 (1662): 1723–9. doi:10.1098/rspb.2008.1780. JSTOR 30245000. PMC 2660991. PMID 19324836.
Bibliography
- Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
External links
| Classification | |
|---|---|
| External resources |