Klinefelter syndrome
Klinefelter syndrome (KS), also known as 47, XXY is the set of symptoms that result from two or more X chromosomes in males.[3] The primary features are infertility and small poorly functioning testicles.[3][9] Often, symptoms may be subtle and many people do not realize they are affected.[1] Sometimes, symptoms are more prominent and may include weaker muscles, greater height, poor coordination, less body hair, breast growth, and less interest in sex.[1] Often it is only at puberty that these symptoms are noticed.[5] Intelligence is usually normal; however, reading difficulties and problems with speech are more common.[1] Symptoms are typically more severe if three or more X chromosomes are present (48,XXXY syndrome or 49,XXXXY syndrome).[1]
| Klinefelter syndrome | |
|---|---|
| Other names | XXY syndrome, Klinefelter's syndrome, Klinefelter-Reifenstein-Albright syndrome |
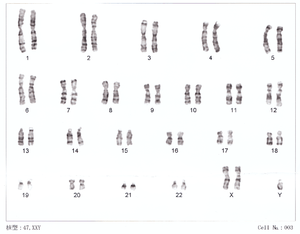 | |
| 47,XXY karyotype | |
| Pronunciation |
|
| Specialty | Medical genetics |
| Symptoms | Often few[1] |
| Usual onset | At fertilisation[2] |
| Duration | Long term |
| Causes | Two or more X chromosomes in males[3] |
| Risk factors | Older mother[4] |
| Diagnostic method | Genetic testing (karyotype)[5] |
| Prevention | None |
| Treatment | Physical therapy, speech and language therapy, counseling[6] |
| Prognosis | Nearly normal life expectancy[7] |
| Frequency | 1:500 to 1:1,000 males[4][8] |
Klinefelter syndrome occurs randomly.[4] The extra X chromosome comes from the father and mother nearly equally.[10] An older mother may have a slightly increased risk of a child with KS.[4] The condition is not typically inherited from one's parents.[4] The underlying mechanisms involves at least one extra X chromosome in addition to a Y chromosome such that the total chromosome number is 47 or more rather than the usual 46.[9] KS is diagnosed by the genetic test known as a karyotype.[5]
While no cure is known, a number of treatments may help.[7] Physical therapy, speech and language therapy, counselling, and adjustments of teaching methods may be useful.[6] Testosterone replacement may be used in those who have significantly lower levels.[6] Enlarged breasts may be removed by surgery.[6] About half of affected males have a chance of fathering children with the help of assisted reproductive technology, but this is expensive and not risk free.[6] XXY males appear to have a higher risk of breast cancer than typical, but still lower than that of females.[11] People with the condition have a nearly normal life expectancy.[7]
Klinefelter syndrome is one of the most common chromosomal disorders, occurring in one to two per 1,000 live male births.[4][8] It is named after American endocrinologist Harry Klinefelter, who identified the condition in the 1940s.[12] In 1956, identification of the extra X chromosome was first noticed.[13] Mice can also have the XXY syndrome, making them a useful research model.[14]
Signs and symptoms
The primary features are infertility and small poorly functioning testicles.[3][9] Often, symptoms may be subtle and many people do not realize they are affected.[1] Sometimes, symptoms are more prominent and may include weaker muscles, greater height, poor coordination, less body hair, breast growth, and less interest in sex.[1] Often it is only at puberty that these symptoms are noticed.[5]
Prenatal
It has been estimated that 60% of infants with Klinefelter syndrome result in miscarriage.[15]
Physical
As babies and children, XXY males may have weaker muscles and reduced strength. As they grow older, they tend to become taller than average. They may have less muscle control and coordination than other boys of their age.[16]
During puberty, the physical traits of the syndrome become more evident; because these boys do not produce as much testosterone as other boys, they have a less muscular body, less facial and body hair, and broader hips. As teens, XXY males may develop breast tissue[17] and also have weaker bones, and a lower energy level than other males.[16]
By adulthood, XXY males look similar to males without the condition, although they are often taller. In adults, possible characteristics vary widely and include little to no sign of affectedness, a lanky, youthful build and facial appearance, or a rounded body type with some degree of gynecomastia (increased breast tissue).[18] Gynecomastia is present to some extent in about a third of affected individuals, a slightly higher percentage than in the XY population. About 10% of XXY males have gynecomastia noticeable enough that they may choose to have cosmetic surgery.[19]
Affected males are often infertile, or may have reduced fertility. Advanced reproductive assistance is sometimes possible.[20] It has been estimated that 50% of males with Klinefelter syndrome can produce sperm.[21]
The term hypogonadism in XXY symptoms is often misinterpreted to mean "small testicles" when it means decreased testicular hormone/endocrine function. Because of this (primary) hypogonadism, individuals often have a low serum testosterone level, but high serum follicle-stimulating hormone and luteinizing hormone levels.[22] Despite this misunderstanding of the term, however, XXY men may also have microorchidism (i.e., small testicles).[22]
The testicle size of affected males are usually less than 2 cm in length (and always shorter than 3.5 cm[23]), 1 cm in width, and 4 ml in volume.[24][25]
XXY males are also more likely than other men to have certain health problems, such as autoimmune disorders, breast cancer, venous thromboembolic disease, and osteoporosis.[16][26] In contrast to these potentially increased risks, rare X-linked recessive conditions are thought to occur less frequently in XXY males than in normal XY males, since these conditions are transmitted by genes on the X chromosome, and people with two X chromosomes are typically only carriers rather than affected by these X-linked recessive conditions.
Cognitive and developmental
Some degree of language learning or reading impairment may be present,[27] and neuropsychological testing often reveals deficits in executive functions, although these deficits can often be overcome through early intervention.[28] Also, delays in motor development may occur, which can be addressed through occupational and physical therapies.[29] XXY males may sit up, crawl, and walk later than other infants; they may also struggle in school, both academically and with sports.[16] It’s estimated that 10% of men with Klinefelter syndrome are Autistic.[30]
Endocrine
Men with Klinefelter's syndrome have testosterone levels that are significantly lower (−260 ng/dL difference), estradiol levels that are slightly higher (+6.8 pg/mL) though not significantly different when restricted to high-accuracy assays (+5.5 pg/mL difference), and the ratio of estradiol to testosterone is significantly higher (+0.06).[31]
Cause
Maternal age is the only known risk factor.[10] Women at 40 years have a four times higher risk for a child with Klinefelter syndrome than women aged 24 years.[32][33]
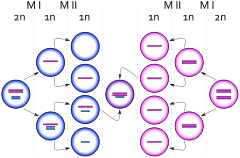
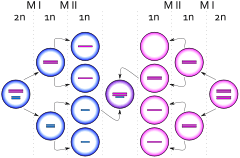
The extra chromosome is retained because of a nondisjunction event during paternal meiosis I, maternal meiosis I, or maternal meiosis II (gametogenesis). The relevant nondisjunction in meiosis I occurs when homologous chromosomes, in this case the X and Y or two X sex chromosomes, fail to separate, producing a sperm with an X and a Y chromosome or an egg with two X chromosomes. Fertilizing a normal (X) egg with this sperm produces an XXY offspring (Klinefelter). Fertilizing a double X egg with a normal sperm also produces an XXY offspring (Klinefelter).[34]
Another mechanism for retaining the extra chromosome is through a nondisjunction event during meiosis II in the egg. Nondisjunction occurs when sister chromatids on the sex chromosome, in this case an X and an X, fail to separate. An XX egg is produced, which when fertilized with a Y sperm, yields an XXY offspring. This XXY chromosome arrangement is one of the most common genetic variations from the XY karyotype, occurring in about one in 500 live male births.[16] See also Triple X syndrome.
In mammals with more than one X chromosome, the genes on all but one X chromosome are not expressed; this is known as X inactivation. This happens in XXY males, as well as normal XX females.[35] However, in XXY males, a few genes located in the pseudoautosomal regions of their X chromosomes have corresponding genes on their Y chromosome and are capable of being expressed.[36]
Variations
48,XXYY or 48,XXXY occurs in one in 18,000–50,000 male births. The incidence of 49,XXXXY is one in 85,000 to 100,000 male births.[37] These variations are extremely rare. Additional chromosomal material can contribute to cardiac, neurological, orthopedic, and other anomalies.
Approximately 15-20%[38] of males with KS may have a mosaic 47,XXY/46,XY constitutional karyotype and varying degrees of spermatogenic failure. Often symptoms are milder in mosaic cases, with regular male secondary sex characteristics and testicular volume even falling within typical adult ranges.[38] Another possible mosaicism is 47,XXY/46,XX with clinical features suggestive of KS and male phenotype, but this is very rare. Thus far, only about 10 cases of 47,XXY/46,XX have been described in literature.[39]
Analogous XXY syndromes are known to occur in cats—specifically, the presence of calico or tortoiseshell markings in male cats is an indicator of the relevant abnormal karyotype. As such, male cats with calico or tortoiseshell markings are a model organism for KS, because a color gene involved in cat tabby coloration is on the X chromosome.[40]
Diagnosis
The standard diagnostic method is the analysis of the chromosomes' karyotype on lymphocytes. A small blood sample is sufficient as test material. In the past, the observation of the Barr body was common practice, as well.[41] To investigate the presence of a possible mosaicism, analysis of the karyotype using cells from the oral mucosa is performed. Physical characteristics of a Klinefelter syndrome can be tall stature, low body hair and occasionally an enlargement of the breast. There is usually a small testicle volume of 1–5 ml per testicle (standard values: 12–30 ml).[42] During puberty and adulthood, low testosterone levels with increased levels of the pituitary hormones FSH and LH in the blood can indicate the presence of Klinefelter syndrome. A spermiogram can also be part of the further investigation. Often there is an azoospermia present, rarely an oligospermia.[10] Furthermore, Klinefelter syndrome can be diagnosed as a coincidental prenatal finding in the context of invasive prenatal diagnosis (amniocentesis, chorionic villus sampling). About 10% of KS cases are found by prenatal diagnosis.[43]
The symptoms of KS are often variable; therefore, a karyotype analysis should be ordered when small testes, infertility, gynecomastia, long arms/legs, developmental delay, speech/language deficits, learning disabilities/academic issues, and/or behavioral issues are present in an individual.[9]
Treatment
The genetic variation is irreversible, thus there is no causal therapy. From the onset of puberty, the existing testosterone deficiency can be compensated by appropriate hormone replacement therapy.[44] Testosterone preparations are available in the form of syringes, patches or gel. If gynecomastia is present, the surgical removal of the breast may be considered for both the psychological reasons and to reduce the risk of breast cancer.[45]
The use of behavioral therapy can mitigate any language disorders, difficulties at school, and socialization. An approach by occupational therapy is useful in children, especially those who have dyspraxia.[46]
Infertility treatment
Methods of reproductive medicine, such as intracytoplasmic sperm injection (ICSI) with previously conducted testicular sperm extraction (TESE), have led to men with Klinefelter's syndrome to produce biological offspring.[47] By 2010, over 100 successful pregnancies have been reported using IVF technology with surgically removed sperm material from males with KS.[48]
Prognosis
The lifespan of individuals with Klinefelter syndrome appears to be reduced by approximately 2.1 years compared to the general male population.[49] These results are still questioned data, are not absolute, and need further testing.[50]
Epidemiology
This syndrome, evenly distributed in all ethnic groups, has a prevalence of one to two subjects per every 1000 males in the general population.[32][51][52][53] However, it is estimated that only 25% of the individuals with Klinefelter syndrome are diagnosed throughout their lives.[44] 3.1% of infertile males have Klinefelter syndrome. The syndrome is also the main cause of male hypogonadism.[54]
History
The syndrome was named after American endocrinologist Harry Klinefelter, who in 1942 worked with Fuller Albright and E. C. Reifenstein at Massachusetts General Hospital in Boston, Massachusetts, and first described it in the same year.[18][55] The account given by Klinefelter came to be known as Klinefelter syndrome as his name appeared first on the published paper, and seminiferous tubule dysgenesis was no longer used. Considering the names of all three researchers, it is sometimes also called Klinefelter–Reifenstein–Albright syndrome.[56] In 1956 it was discovered that Klinefelter syndrome resulted from an extra chromosome.[13] Plunkett and Barr found the sex chromatin body in cell nuclei of the body.[57] This was further clarified as XXY in 1959 by Patricia Jacobs and John Anderson Strong.[58] The first published report of a man with a 47,XXY karyotype was by Patricia Jacobs and John Strong at Western General Hospital in Edinburgh, Scotland, in 1959.[58] This karyotype was found in a 24-year-old man who had signs of KS. Jacobs described her discovery of this first reported human or mammalian chromosome aneuploidy in her 1981 William Allan Memorial Award address.[59]
Other animals
Klinefelter syndrome can also occur in other animals. In cats it can result in a male tortoiseshell and calico cat (patches of different colored fur), a pattern that is usually only seen in female cats.[60] Not all cats with Klinefelter syndrome have tortoiseshell or calico patterns.
References
- "What are common symptoms of Klinefelter syndrome (KS)?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2013-10-25. Archived from the original on 2 April 2015. Retrieved 15 March 2015.
- "Klinefelter syndrome". rarediseases.info.nih.gov. Retrieved 15 April 2019.
- "Klinefelter Syndrome (KS): Overview". nichd.nih.gov. Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2013-11-15. Archived from the original on 18 March 2015. Retrieved 15 March 2015.
- "How many people are affected by or at risk for Klinefelter syndrome (KS)?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2012-11-30. Archived from the original on 17 March 2015. Retrieved 15 March 2015.
- "How do health care providers diagnose Klinefelter syndrome (KS)?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2012-11-30. Archived from the original on 17 March 2015. Retrieved 15 March 2015.
- "What are the treatments for symptoms in Klinefelter syndrome (KS)?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2013-10-25. Archived from the original on 15 March 2015. Retrieved 15 March 2015.
- "Is there a cure for Klinefelter syndrome (KS)?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2012-11-30. Archived from the original on 17 March 2015. Retrieved 16 March 2015.
- "Klinefelter syndrome". Genetics Home Reference. National Library of Medicine. 2012-10-30. Archived from the original on 2012-11-15. Retrieved 2012-11-02.
- Visootsak J, Graham JM (October 2006). "Klinefelter syndrome and other sex chromosomal aneuploidies". Orphanet Journal of Rare Diseases. 1: 42. doi:10.1186/1750-1172-1-42. PMC 1634840. PMID 17062147.
- Kanakis GA, Nieschlag E (September 2018). "Klinefelter syndrome: more than hypogonadism". Metabolism. 86: 135–144. doi:10.1016/j.metabol.2017.09.017. PMID 29382506.
- Brinton LA (June 2011). "Breast cancer risk among patients with Klinefelter syndrome". Acta Paediatrica. 100 (6): 814–8. doi:10.1111/j.1651-2227.2010.02131.x. PMC 4024394. PMID 21241366.
- "Klinefelter Syndrome (KS): Condition Information". nichd.nih.gov. 2013-11-15. Archived from the original on 18 March 2015. Retrieved 15 March 2015.
- Odom, Samuel L. (2009). Handbook of developmental disabilities (Pbk. ed.). New York: Guilford. p. 113. ISBN 9781606232484.
- Conn, P. Michael (2013). Animal models for the study of human disease (First ed.). San Diego: Elsevier Science & Technology Books. p. 780. ISBN 9780124159129.
- "Klinefelter Syndrome | Encyclopedia.com". encyclopedia.com. Retrieved 2020-07-14.
- "Klinefelter Syndrome". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2007-05-24. Archived from the original on November 27, 2012.
- "47, XXY (Klinefelter syndrome)". University of Utah. Archived from the original on 30 July 2014. Retrieved 15 June 2014.
- Klinefelter HF (September 1986). "Klinefelter's syndrome: historical background and development". Southern Medical Journal. 79 (9): 1089–93. doi:10.1097/00007611-198609000-00012. PMID 3529433.
- Bock, Robert (August 1993). "Understanding Klinefelter Syndrome: A Guide for XXY Males and their Families". NIH Pub. No. 93-3202. Eunice Kennedy Shriver National Institute of Child Health and Human Development. Retrieved 2007-04-07.
- Denschlag D, Tempfer C, Kunze M, Wolff G, Keck C (October 2004). "Assisted reproductive techniques in patients with Klinefelter syndrome: a critical review". Fertility and Sterility. 82 (4): 775–9. doi:10.1016/j.fertnstert.2003.09.085. PMID 15482743.
- "What are the treatments for symptoms in Klinefelter syndrome (KS)?". https://www.nichd.nih.gov/. Retrieved 2020-07-14. External link in
|website=(help) - Leask, Kathryn (October 2005). "Klinefelter syndrome". National Library for Health, Specialist Libraries, Clinical Genetics. National Library for Health. Archived from the original on 2007-09-27. Retrieved 2007-04-07.
- Astwood, E. B. (2013-10-22). Recent Progress in Hormone Research: Proceedings of the 1967 Laurentian Hormone Conference. Academic Press. ISBN 9781483223308.
- "Klinefelter's Syndrome: XXY Males". Archived from the original on 2017-08-24. Retrieved 2017-07-01.
- Smyth CM, Bremner WJ (June 1998). "Klinefelter syndrome". Archives of Internal Medicine. 158 (12): 1309–14. doi:10.1001/archinte.158.12.1309. PMID 9645824.
- Hultborn R, Hanson C, Köpf I, Verbiené I, Warnhammar E, Weimarck A (November–December 1997). "Prevalence of Klinefelter's syndrome in male breast cancer patients". Anticancer Research. 17 (6D): 4293–7. PMID 9494523.
- Graham JM, Bashir AS, Stark RE, Silbert A, Walzer S (June 1988). "Oral and written language abilities of XXY boys: implications for anticipatory guidance". Pediatrics. 81 (6): 795–806. PMID 3368277.
- Boone KB, Swerdloff RS, Miller BL, Geschwind DH, Razani J, Lee A, et al. (May 2001). "Neuropsychological profiles of adults with Klinefelter syndrome". Journal of the International Neuropsychological Society. 7 (4): 446–56. doi:10.1017/S1355617701744013. PMID 11396547.
- Samango-Sprouse C (December 2010). "Expansion of the phenotypic profile of the young child with XXY". Pediatric Endocrinology Reviews. 8 Suppl 1: 160–8. PMID 21217608.
- Reference, Genetics Home. "Klinefelter syndrome". Genetics Home Reference. Retrieved 2020-07-14.
- Santi D, De Vincentis S, Scaltriti S, Rochira V (May 2019). "Relative hyperestrogenism in Klinefelter Syndrome: results from a meta-analysis". Endocrine. 64 (2): 209–219. doi:10.1007/s12020-019-01850-y. PMID 30701446.
- Bojesen A, Juul S, Gravholt CH (February 2003). "Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study". The Journal of Clinical Endocrinology and Metabolism. 88 (2): 622–6. doi:10.1210/jc.2002-021491. PMID 12574191.
- Tüttelmann F, Gromoll J (June 2010). "Novel genetic aspects of Klinefelter's syndrome". Molecular Human Reproduction. 16 (6): 386–95. doi:10.1093/molehr/gaq019. PMID 20228051.
- "Klinefelter Syndrome - Inheritence Pattern". NIH - Genetics Home Reference. NIH. Archived from the original on 30 January 2017. Retrieved 27 January 2017.
- Chow JC, Yen Z, Ziesche SM, Brown CJ (2005). "Silencing of the mammalian X chromosome". Annual Review of Genomics and Human Genetics. 6: 69–92. doi:10.1146/annurev.genom.6.080604.162350. PMID 16124854.
- Blaschke RJ, Rappold G (June 2006). "The pseudoautosomal regions, SHOX and disease". Current Opinion in Genetics & Development. 16 (3): 233–9. doi:10.1016/j.gde.2006.04.004. PMID 16650979.
- Linden MG, Bender BG, Robinson A (October 1995). "Sex chromosome tetrasomy and pentasomy". Pediatrics. 96 (4 Pt 1): 672–82. PMID 7567329.
- Samplaski, Mary K.; et al. (April 2014). "Phenotypic differences in mosaic Klinefelter patients as compared with non-mosaic Klinefelter patients". Fertility and Sterility. 101 (4): 950–955. Retrieved 13 June 2020.
- Velissariou V, Christopoulou S, Karadimas C, Pihos I, Kanaka-Gantenbein C, Kapranos N, et al. (2006). "Rare XXY/XX mosaicism in a phenotypic male with Klinefelter syndrome: case report". European Journal of Medical Genetics. 49 (4): 331–7. doi:10.1016/j.ejmg.2005.09.001. PMID 16829354.
- Centerwall WR, Benirschke K (September 1975). "An animal model for the XXY Klinefelter's syndrome in man: tortoiseshell and calico male cats". American Journal of Veterinary Research. 36 (9): 1275–80. PMID 1163864.
- Kamischke A, Baumgardt A, Horst J, Nieschlag E (Jan–Feb 2003). "Clinical and diagnostic features of patients with suspected Klinefelter syndrome". Journal of Andrology. 24 (1): 41–8. PMID 12514081.
- Nieschlag E (May 2013). "Klinefelter syndrome: the commonest form of hypogonadism, but often overlooked or untreated". Deutsches Ärzteblatt International. 110 (20): 347–53. doi:10.3238/arztebl.2013.0347. PMC 3674537. PMID 23825486.
- Abramsky L, Chapple J (April 1997). "47,XXY (Klinefelter syndrome) and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling". Prenatal Diagnosis. 17 (4): 363–8. doi:10.1002/(SICI)1097-0223(199704)17:4<363::AID-PD79>3.0.CO;2-O. PMID 9160389.
- Groth KA, Skakkebæk A, Høst C, Gravholt CH, Bojesen A (January 2013). "Clinical review: Klinefelter syndrome--a clinical update". The Journal of Clinical Endocrinology and Metabolism. 98 (1): 20–30. doi:10.1210/jc.2012-2382. PMID 23118429.
- Gabriele R, Borghese M, Conte M, Egidi F (2002). "[Clinical-therapeutic features of gynecomastia]". Il Giornale di Chirurgia (in Italian). 23 (6–7): 250–2. PMID 12422780.
- Harold Chen. "Klinefelter Syndrome - Treatment". medscape.com. Archived from the original on 2 July 2012. Retrieved 4 September 2012.
- Corona G, Pizzocaro A, Lanfranco F, Garolla A, Pelliccione F, Vignozzi L, et al. (May 2017). "Sperm recovery and ICSI outcomes in Klinefelter syndrome: a systematic review and meta-analysis". Human Reproduction Update. 23 (3): 265–275. doi:10.1093/humupd/dmx008. PMID 28379559.
- Fullerton G, Hamilton M, Maheshwari A (March 2010). "Should non-mosaic Klinefelter syndrome men be labelled as infertile in 2009?". Human Reproduction. 25 (3): 588–97. doi:10.1093/humrep/dep431. PMID 20085911.
- Bojesen A, Juul S, Birkebaek N, Gravholt CH (August 2004). "Increased mortality in Klinefelter syndrome". The Journal of Clinical Endocrinology and Metabolism. 89 (8): 3830–4. doi:10.1210/jc.2004-0777. PMID 15292313. Archived from the original on 2013-04-14.
- Swerdlow AJ, Higgins CD, Schoemaker MJ, Wright AF, Jacobs PA (December 2005). "Mortality in patients with Klinefelter syndrome in Britain: a cohort study". The Journal of Clinical Endocrinology and Metabolism. 90 (12): 6516–22. doi:10.1210/jc.2005-1077. PMID 16204366. Archived from the original on 2013-12-16. Retrieved 2012-10-24.
- Jacobs PA (1979). "Recurrence risks for chromosome abnormalities". Birth Defects Original Article Series. 15 (5C): 71–80. PMID 526617.
- Maclean N, Harnden DG, Court Brown WM (August 1961). "Abnormalities of sex chromosome constitution in newborn babies". Lancet. 2 (7199): 406–8. doi:10.1016/S0140-6736(61)92486-2. PMID 13764957.
- Visootsak J, Aylstock M, Graham JM (December 2001). "Klinefelter syndrome and its variants: an update and review for the primary pediatrician". Clinical Pediatrics. 40 (12): 639–51. doi:10.1177/000992280104001201. PMID 11771918.
- Matlach J, Grehn F, Klink T (Jan 2012). "Klinefelter syndrome associated with goniodysgenesis". Journal of Glaucoma. 22 (5): e7-8. doi:10.1097/IJG.0b013e31824477ef. PMID 22274665.
- Klinefelter HF Jr; Reifenstein EC Jr; Albright F. (1942). "Syndrome characterized by gynecomastia, aspermatogenesis without a-Leydigism and increased excretion of follicle-stimulating hormone". The Journal of Clinical Endocrinology & Metabolism. 2 (11): 615–624. doi:10.1210/jcem-2-11-615.
- The Klinefelter-Reifenstein-Albright syndrome. on biomedsearch.com, retrieved 26 August 2017
- "Klinefelter Syndrome - an overview | ScienceDirect Topics". ScienceDirect Topics.
- Jacobs PA, Strong JA (January 1959). "A case of human intersexuality having a possible XXY sex-determining mechanism". Nature. 183 (4657): 302–3. Bibcode:1959Natur.183..302J. doi:10.1038/183302a0. PMID 13632697.
- Jacobs PA (September 1982). "The William Allan Memorial Award address: human population cytogenetics: the first twenty-five years". American Journal of Human Genetics. 34 (5): 689–98. PMC 1685430. PMID 6751075.
- Spadafori, Gina. "The Pet Connection: Feline Fallacies". VeterinaryPartner.com. Archived from the original on 2008-06-12. Retrieved 2008-07-03.
Further reading
- Virginia Isaacs Cover (2012). Living with Klinefelter Syndrome, Trisomy X and 47,XYY: A Guide for Families and Individuals Affected by Extra X and Y Chromosomes. ISBN 978-0-615-57400-4.
External links
| Classification | |
|---|---|
| External resources |

