Down syndrome
Down syndrome or Down's syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21.[2] It is usually associated with physical growth delays, mild to moderate intellectual disability, and characteristic facial features.[1] The average IQ of a young adult with Down syndrome is 50, but this can vary widely.[8]
| Down syndrome | |
|---|---|
| Other names | Down's syndrome, Down's, trisomy 21 |
 | |
| Illustration of the facial features of Down syndrome | |
| Specialty | Medical genetics, pediatrics |
| Symptoms | Delayed physical growth, characteristic facial features, mild to moderate intellectual disability[1] |
| Causes | Third copy of chromosome 21[2] |
| Risk factors | Older age of mother, prior affected child[3][4] |
| Diagnostic method | Prenatal screening, genetic testing[5] |
| Treatment | Educational support, sheltered work environment[6][7] |
| Prognosis | Life expectancy 50 to 60 years (developed world)[8][9] |
| Frequency | 5.4 million (0.1%)[1][10] |
| Deaths | 26,500 (2015)[11] |
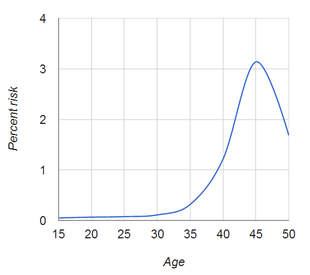
The parents of the affected individual are usually genetically normal.[12] The probability increases from less than 0.1% in 20-year-old mothers to 3% in those of age 45.[3] The extra chromosome is believed to occur by chance, with no known behavioral activity or environmental factor that changes the probability.[13] Down syndrome can be identified during pregnancy by prenatal screening followed by diagnostic testing or after birth by direct observation and genetic testing.[5] Since the introduction of screening, pregnancies with the diagnosis are often terminated.[14][15] Regular screening for health problems common in Down syndrome is recommended throughout the person's life.[8]
There is no cure for Down syndrome.[16] Education and proper care have been shown to improve quality of life.[6] Some children with Down syndrome are educated in typical school classes, while others require more specialized education.[7] Some individuals with Down syndrome graduate from high school, and a few attend post-secondary education.[17] In adulthood, about 20% in the United States do paid work in some capacity,[18] with many requiring a sheltered work environment.[7] Support in financial and legal matters is often needed.[9] Life expectancy is around 50 to 60 years in the developed world with proper health care.[8][9]
Down syndrome is one of the most common chromosome abnormalities in humans.[8] It occurs in about 1 in 1,000 babies born each year.[1] In 2015, Down syndrome was present in 5.4 million individuals globally and resulted in 27,000 deaths, down from 43,000 deaths in 1990.[10][11][19] It is named after British doctor John Langdon Down, who fully described the syndrome in 1866.[20] Some aspects of the condition were described earlier by French psychiatrist Jean-Étienne Dominique Esquirol in 1838 and French physician Édouard Séguin in 1844.[21] The genetic cause of Down syndrome was discovered in 1959.[20]
Signs and symptoms

Those with Down syndrome nearly always have physical and intellectual disabilities.[22] They also typically have poor immune function[12] and generally reach developmental milestones at a later age.[9] They have an increased risk of a number of other health problems, including congenital heart defect, epilepsy, leukemia, thyroid diseases, and mental disorders.[20]
| Characteristics | Percentage | Characteristics | Percentage |
|---|---|---|---|
| Mental impairment | 99%[23] | Abnormal teeth | 60%[24] |
| Stunted growth | 90%[25] | Slanted eyes | 60%[12] |
| Umbilical hernia | 90%[26] | Shortened hands | 60%[24] |
| Increased skin on back of neck | 80%[20] | Short neck | 60%[24] |
| Low muscle tone | 80%[27] | Obstructive sleep apnea | 60%[20] |
| Narrow roof of mouth | 76%[24] | Bent fifth finger tip | 57%[12] |
| Flat head | 75%[12] | Brushfield spots in the iris | 56%[12] |
| Flexible ligaments | 75%[12] | Single transverse palmar crease | 53%[12] |
| Proportionally large tongue[28] | 75%[27] | Protruding tongue | 47%[24] |
| Abnormal outer ears | 70%[20] | Congenital heart disease | 40%[24] |
| Flattened nose | 68%[12] | Strabismus | ~35%[1] |
| Separation of first and second toes | 68%[24] | Undescended testicles | 20%[29] |
Physical
People with Down syndrome may have some or all of these physical characteristics: a small chin, slanted eyes, poor muscle tone, a flat nasal bridge, a single crease of the palm, and a protruding tongue due to a small mouth and relatively large tongue.[27][28] These airway changes lead to obstructive sleep apnea in around half of those with Down syndrome.[20] Other common features include: a flat and wide face,[27] a short neck, excessive joint flexibility, extra space between big toe and second toe, abnormal patterns on the fingertips and short fingers.[24][27] Instability of the atlantoaxial joint occurs in about 20% and may lead to spinal cord injury in 1–2%.[8][9] Hip dislocations may occur without trauma in up to a third of people with Down syndrome.[20]
Growth in height is slower, resulting in adults who tend to have short stature—the average height for men is 154 cm (5 ft 1 in) and for women is 142 cm (4 ft 8 in).[30] Individuals with Down syndrome are at increased risk for obesity as they age.[20] Growth charts have been developed specifically for children with Down syndrome.[20]
Neurological
This syndrome causes about a third of cases of intellectual disability.[12] Many developmental milestones are delayed with the ability to crawl typically occurring around 8 months rather than 5 months and the ability to walk independently typically occurring around 21 months rather than 14 months.[31]
Most individuals with Down syndrome have mild (IQ: 50–69) or moderate (IQ: 35–50) intellectual disability with some cases having severe (IQ: 20–35) difficulties.[1][32] Those with mosaic Down syndrome typically have IQ scores 10–30 points higher.[33] As they age, people with Down syndrome typically perform worse than their same-age peers.[32][34]
Commonly, individuals with Down syndrome have better language understanding than ability to speak.[20][32] Between 10 and 45% have either a stutter or rapid and irregular speech, making it difficult to understand them.[35] After reaching 30 years of age, some may lose their ability to speak.[8]
They typically do fairly well with social skills.[20] Behavior problems are not generally as great an issue as in other syndromes associated with intellectual disability.[32] In children with Down syndrome, mental illness occurs in nearly 30% with autism occurring in 5–10%.[9] People with Down syndrome experience a wide range of emotions.[36] While people with Down syndrome are generally happy,[37] symptoms of depression and anxiety may develop in early adulthood.[8]
Children and adults with Down syndrome are at increased risk of epileptic seizures, which occur in 5–10% of children and up to 50% of adults.[8] This includes an increased risk of a specific type of seizure called infantile spasms.[20] Many (15%) who live 40 years or longer develop Alzheimer’s disease.[38] In those who reach 60 years of age, 50–70% have the disease.[8]
Senses

Hearing and vision disorders occur in more than half of people with Down syndrome.[20] Vision problems occur in 38 to 80%.[1] Between 20 and 50% have strabismus, in which the two eyes do not move together.[1] Cataracts (cloudiness of the lens of the eye) occur in 15%,[9] and may be present at birth.[1] Keratoconus (a thin, cone-shaped cornea)[8] and glaucoma (increased eye pressure) are also more common,[1] as are refractive errors requiring glasses or contacts.[8] Brushfield spots (small white or grayish/brown spots on the outer part of the iris) are present in 38 to 85% of individuals.[1]
Hearing problems are found in 50–90% of children with Down syndrome.[39] This is often the result of otitis media with effusion which occurs in 50–70%[9] and chronic ear infections which occur in 40 to 60%.[40] Ear infections often begin in the first year of life and are partly due to poor eustachian tube function.[41][42] Excessive ear wax can also cause hearing loss due to obstruction of the outer ear canal.[8] Even a mild degree of hearing loss can have negative consequences for speech, language understanding, and academics.[1][42] Additionally, it is important to rule out hearing loss as a factor in social and cognitive deterioration.[43] Age-related hearing loss of the sensorineural type occurs at a much earlier age and affects 10–70% of people with Down syndrome.[8]
Heart
The rate of congenital heart disease in newborns with Down syndrome is around 40%.[24] Of those with heart disease, about 80% have an atrioventricular septal defect or ventricular septal defect with the former being more common.[8] Mitral valve problems become common as people age, even in those without heart problems at birth.[8] Other problems that may occur include tetralogy of Fallot and patent ductus arteriosus.[41] People with Down syndrome have a lower risk of hardening of the arteries.[8]
Cancer
Although the overall risk of cancer in Down syndrome is not changed,[44] the risk of testicular cancer and certain blood cancers, including acute lymphoblastic leukemia (ALL) and acute megakaryoblastic leukemia (AMKL) is increased while the risk of other non-blood cancers is decreased.[8] People with Down syndrome are believed to have an increased risk of developing cancers derived from germ cells whether these cancers are blood or non-blood related.[45]
Blood cancers
Leukemia is 10 to 15 times more common in children with Down syndrome.[20] In particular, acute lymphoblastic leukemia is 20 times more common and the megakaryoblastic form of acute myeloid leukemia (acute megakaryoblastic leukemia), is 500 times more common.[46] Acute megakaryoblastic leukemia (AMKL) is a leukemia of megakaryoblasts, the precursors cells to megakaryocytes which form blood platelets.[46] Acute lymphoblastic leukemia in Down syndrome accounts for 1–3% of all childhood cases of ALL. It occurs most often in those older than nine years or having a white blood cell count greater than 50,000 per microliter and is rare in those younger than one year old. ALL in Down syndrome tends to have poorer outcomes than other cases of ALL in people without Down syndrome.[47][48]
In Down syndrome, AMKL is typically preceded by transient myeloproliferative disease (TMD), a disorder of blood cell production in which non-cancerous megakaryoblasts with a mutation in the GATA1 gene rapidly divide during the later period of pregnancy.[46][49] The condition affects 3–10% of babies with Down.[46] While it often spontaneously resolves within three months of birth, it can cause serious blood, liver, or other complications.[50] In about 10% of cases, TMD progresses to AMKL during the three months to five years following its resolution.[46][50][51]
Non-blood cancers
People with Down syndrome have a lower risk of all major solid cancers including those of lung, breast, cervix, with the lowest relative rates occurring in those aged 50 years or older.[45] This low risk is thought due to an increase in the expression of tumor suppressor genes present on chromosome 21.[52][45] One exception is testicular germ cell cancer which occurs at a higher rate in Down syndrome.[45]
Endocrine
Problems of the thyroid gland occur in 20–50% of individuals with Down syndrome.[8][20] Low thyroid is the most common form, occurring in almost half of all individuals.[8] Thyroid problems can be due to a poorly or nonfunctioning thyroid at birth (known as congenital hypothyroidism) which occurs in 1%[9] or can develop later due to an attack on the thyroid by the immune system resulting in Graves' disease or autoimmune hypothyroidism.[53] Type 1 diabetes mellitus is also more common.[8]
Gastrointestinal
Constipation occurs in nearly half of people with Down syndrome and may result in changes in behavior.[20] One potential cause is Hirschsprung's disease, occurring in 2–15%, which is due to a lack of nerve cells controlling the colon.[54] Other frequent congenital problems include duodenal atresia, pyloric stenosis, Meckel diverticulum, and imperforate anus.[41] Celiac disease affects about 7–20%[8][20] and gastroesophageal reflux disease is also more common.[41]
Teeth
Individuals with Down syndrome tend to be more susceptible to gingivitis as well as early, severe periodontal disease, necrotising ulcerative gingivitis, and early tooth loss, especially in the lower front teeth.[55][56] While plaque and poor oral hygiene are contributing factors, the severity of these periodontal diseases cannot be explained solely by external factors.[56] Research suggests that the severity is likely a result of a weakened immune system.[56][57] The weakened immune system also contributes to increased incidence of yeast infections in the mouth (from Candida albicans).[57]
Individuals with Down syndrome also tend to have a more alkaline saliva resulting in a greater resistance to tooth decay, despite decreased quantities of saliva,[58] less effective oral hygiene habits, and higher plaque indexes.[55][57][58][59]
Higher rates of tooth wear and bruxism are also common.[57] Other common oral manifestations of Down syndrome include enlarged hypotonic tongue, crusted and hypotonic lips, mouth breathing, narrow palate with crowded teeth, class III malocclusion with an underdeveloped maxilla and posterior crossbite, delayed exfoliation of baby teeth and delayed eruption of adult teeth, shorter roots on teeth, and often missing and malformed (usually smaller) teeth.[55][57][58][59] Less common manifestations include cleft lip and palate and enamel hypocalcification (20% prevalence).[59]
Fertility
Males with Down syndrome usually do not father children, while females have lower rates of fertility relative to those who are unaffected.[60] Fertility is estimated to be present in 30–50% of females.[61] Menopause usually occurs at an earlier age.[8] The poor fertility in males is thought to be due to problems with sperm development; however, it may also be related to not being sexually active.[60] As of 2006, three instances of males with Down syndrome fathering children and 26 cases of females having children have been reported.[60] Without assisted reproductive technologies, around half of the children of someone with Down syndrome will also have the syndrome.[60][62]
Cause
Down syndrome is caused by having three copies of the genes on chromosome 21, rather than the usual two.[2][63] The parents of the affected individual are typically genetically normal.[12] Those who have one child with Down syndrome have about a 1% risk of having a second child with the syndrome, if both parents are found to have normal karyotypes.[61]
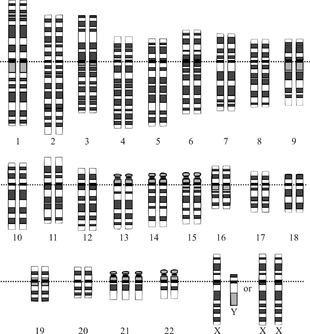
The extra chromosome content can arise through several different ways. The most common cause (about 92–95% of cases) is a complete extra copy of chromosome 21, resulting in trisomy 21.[62][64] In 1.0 to 2.5% of cases, some of the cells in the body are normal and others have trisomy 21, known as mosaic Down syndrome.[61][65] The other common mechanisms that can give rise to Down syndrome include: a Robertsonian translocation, isochromosome, or ring chromosome. These contain additional material from chromosome 21 and occur in about 2.5% of cases.[20][61] An isochromosome results when the two long arms of a chromosome separate together rather than the long and short arm separating together during egg or sperm development.[62]
Trisomy 21
Trisomy 21 (also known by the karyotype 47,XX,+21 for females and 47,XY,+21 for males)[66] is caused by a failure of the 21st chromosome to separate during egg or sperm development (nondisjunction).[62] As a result, a sperm or egg cell is produced with an extra copy of chromosome 21; this cell thus has 24 chromosomes. When combined with a normal cell from the other parent, the baby has 47 chromosomes, with three copies of chromosome 21.[2][62] About 88% of cases of trisomy 21 result from nonseparation of the chromosomes in the mother, 8% from nonseparation in the father, and 3% after the egg and sperm have merged.[67]
Translocation
The extra chromosome 21 material may also occur due to a Robertsonian translocation in 2–4% of cases.[61][68] In this situation, the long arm of chromosome 21 is attached to another chromosome, often chromosome 14.[69] In a male affected with Down syndrome, it results in a karyotype of 46XY,t(14q21q).[69][70] This may be a new mutation or previously present in one of the parents.[71] The parent with such a translocation is usually normal physically and mentally;[69] however, during production of egg or sperm cells, a higher chance of creating reproductive cells with extra chromosome 21 material exists.[68] This results in a 15% chance of having a child with Down syndrome when the mother is affected and a less than 5% probability if the father is affected.[71] The probability of this type of Down syndrome is not related to the mother's age.[69] Some children without Down syndrome may inherit the translocation and have a higher probability of having children of their own with Down syndrome.[69] In this case it is sometimes known as familial Down syndrome.[72]
Mechanism
The extra genetic material present in Down syndrome results in overexpression of a portion of the 310 genes located on chromosome 21.[63] This overexpression has been estimated at around 50%, due to the third copy of the chromosome present.[61] Some research has suggested the Down syndrome critical region is located at bands 21q22.1–q22.3,[73] with this area including genes for amyloid, superoxide dismutase, and likely the ETS2 proto oncogene.[74] Other research, however, has not confirmed these findings.[63] microRNAs are also proposed to be involved.[75]
The dementia that occurs in Down syndrome is due to an excess of amyloid beta peptide produced in the brain and is similar to Alzheimer's disease, which also involves amyloid beta build-up.[76] Amyloid beta is processed from amyloid precursor protein, the gene for which is located on chromosome 21.[76] Senile plaques and neurofibrillary tangles are present in nearly all by 35 years of age, though dementia may not be present.[12] Those with Down syndrome also lack a normal number of lymphocytes and produce less antibodies which contributes to their increased risk of infection.[20]
Epigenetics
Down syndrome is associated with an increased risk of many chronic diseases that are typically associated with older age such as Alzheimer's disease. The accelerated aging suggest that trisomy 21 increases the biological age of tissues, but molecular evidence for this hypothesis is sparse. According to a biomarker of tissue age known as epigenetic clock, trisomy 21 increases the age of blood and brain tissue (on average by 6.6 years).[77]
Diagnosis
Before birth
When screening tests predict a high risk of Down syndrome, a more invasive diagnostic test (amniocentesis or chorionic villus sampling) is needed to confirm the diagnosis.[78] The false-positive rate with screening is about 2–5% (see section Screening below).[79] Amniocentesis and chorionic villus sampling are more reliable tests, but they increase the risk of miscarriage between 0.5 and 1%.[80] The risk of limb problems may be increased in the offspring if chorionic villus sampling is performed before 10 weeks.[80] The risk from the procedure is greater the earlier it is performed, thus amniocentesis is not recommended before 15 weeks gestational age and chorionic villus sampling before 10 weeks gestational age.[80]
Abortion rates
About 92% of pregnancies in Europe with a diagnosis of Down syndrome are terminated.[15] As a result, there is almost no one with Down's in Iceland and Denmark, where screening is commonplace.[81] In the United States, the termination rate after diagnosis is around 75%,[81] but varies from 61% to 93% depending on the population surveyed.[14] Rates are lower among women who are younger and have decreased over time.[14] When asked if they would have a termination if their fetus tested positive, 23–33% said yes, when high-risk pregnant women were asked, 46–86% said yes, and when women who screened positive are asked, 89–97% say yes.[82]
After birth
The diagnosis can often be suspected based on the child's physical appearance at birth.[9] An analysis of the child's chromosomes is needed to confirm the diagnosis, and to determine if a translocation is present, as this may help determine the risk of the child's parents having further children with Down syndrome.[9] Parents generally wish to know the possible diagnosis once it is suspected and do not wish pity.[20]
Screening
Guidelines recommend screening for Down syndrome to be offered to all pregnant women, regardless of age.[78][83] A number of tests are used, with varying levels of accuracy. They are typically used in combination to increase the detection rate.[20] None can be definitive, thus if screening is positive, either amniocentesis or chorionic villus sampling is required to confirm the diagnosis.[78] Screening in both the first and second trimesters is better than just screening in the first trimester.[78] The different screening techniques in use are able to pick up 90–95% of cases, with a false-positive rate of 2–5%.[79] If Down syndrome occurs in one in 500 pregnancies and the test used has a 5% false-positive rate, this means, of 26 women who test positive on screening, only one will have Down syndrome confirmed.[79] If the screening test has a 2% false-positive rate, this means one of eleven who test positive on screening have a fetus with Down syndrome.[79]
| Screen | Week of pregnancy when performed | Detection rate | False positive | Description |
|---|---|---|---|---|
| Combined test | 10–13.5 wks | 82–87% | 5% | Uses ultrasound to measure nuchal translucency in addition to blood tests for free or total beta-hCG and PAPP-A |
| Quad screen | 15–20 wks | 81% | 5% | Measures the maternal serum alpha-fetoprotein, unconjugated estriol, hCG, and inhibin-A |
| Integrated test | 15–20 wks | 94–96% | 5% | Is a combination of the quad screen, PAPP-A, and NT |
| Cell-free fetal DNA | From 10 wks[84] | 96–100%[85] | 0.3%[86] | A blood sample is taken from the mother by venipuncture and is sent for DNA analysis. |
Ultrasound
Ultrasound imaging can be used to screen for Down syndrome. Findings that indicate increased risk when seen at 14 to 24 weeks of gestation include a small or no nasal bone, large ventricles, nuchal fold thickness, and an abnormal right subclavian artery, among others.[87] The presence or absence of many markers is more accurate.[87] Increased fetal nuchal translucency (NT) indicates an increased risk of Down syndrome picking up 75–80% of cases and being falsely positive in 6%.[88]
- Ultrasound of fetus with Down syndrome showing a large bladder
 Enlarged NT and absent nasal bone in a fetus at 11 weeks with Down syndrome
Enlarged NT and absent nasal bone in a fetus at 11 weeks with Down syndrome
Blood tests
Several blood markers can be measured to predict the risk of Down syndrome during the first or second trimester.[79][89] Testing in both trimesters is sometimes recommended and test results are often combined with ultrasound results.[79] In the second trimester, often two or three tests are used in combination with two or three of: α-fetoprotein, unconjugated estriol, total hCG, and free βhCG detecting about 60–70% of cases.[89]
Testing of the mother's blood for fetal DNA is being studied and appears promising in the first trimester.[85][90] The International Society for Prenatal Diagnosis considers it a reasonable screening option for those women whose pregnancies are at a high risk for trisomy 21.[91] Accuracy has been reported at 98.6% in the first trimester of pregnancy.[20] Confirmatory testing by invasive techniques (amniocentesis, CVS) is still required to confirm the screening result.[91]
Management
Efforts such as early childhood intervention, screening for common problems, medical treatment where indicated, a good family environment, and work-related training can improve the development of children with Down syndrome. Education and proper care can improve quality of life.[6] Raising a child with Down syndrome is more work for parents than raising an unaffected child.[92] Typical childhood vaccinations are recommended.[20]
Health screening
| Testing | Children[93] | Adults[8] |
|---|---|---|
| Hearing | 6 months, 12 months, then yearly | 3–5 years |
| T4 and TSH | 6 months, then yearly | |
| Eyes | 6 months, then yearly | 3–5 years |
| Teeth | 2 years, then every 6 months | |
| Coeliac disease | Between 2 and 3 years of age, or earlier if symptoms occur | |
| Sleep study | 3 to 4 years, or earlier if symptoms of obstructive sleep apnea occur | |
| Neck X-rays | Between 3 and 5 years of age |
A number of health organizations have issued recommendations for screening those with Down syndrome for particular diseases.[93] This is recommended to be done systematically.[20]
At birth, all children should get an electrocardiogram and ultrasound of the heart.[20] Surgical repair of heart problems may be required as early as three months of age.[20] Heart valve problems may occur in young adults, and further ultrasound evaluation may be needed in adolescents and in early adulthood.[20] Due to the elevated risk of testicular cancer, some recommend checking the person's testicles yearly.[8]
Cognitive development
Hearing aids or other amplification devices can be useful for language learning in those with hearing loss.[20] Speech therapy may be useful and is recommended to be started around nine months of age.[20] As those with Down syndrome typically have good hand-eye coordination, learning sign language may be possible.[32] Augmentative and alternative communication methods, such as pointing, body language, objects, or pictures, are often used to help with communication.[94] Behavioral issues and mental illness are typically managed with counseling or medications.[9]
Education programs before reaching school age may be useful.[1] School-age children with Down syndrome may benefit from inclusive education (whereby students of differing abilities are placed in classes with their peers of the same age), provided some adjustments are made to the curriculum.[95] Evidence to support this, however, is not very strong.[96] In the United States, the Individuals with Disabilities Education Act of 1975 requires public schools generally to allow attendance by students with Down syndrome.[97]
Individuals with Down syndrome may learn better visually. Drawing may help with language, speech, and reading skills. Children with Down syndrome still often have difficulty with sentence structure and grammar, as well as developing the ability to speak clearly.[98] Several types of early intervention can help with cognitive development. Efforts to develop motor skills include physical therapy, speech and language therapy, and occupational therapy. Physical therapy focuses specifically on motor development and teaching children to interact with their environment. Speech and language therapy can help prepare for later language. Lastly, occupational therapy can help with skills needed for later independence.[99]
Other
Tympanostomy tubes are often needed[20] and often more than one set during the person's childhood.[39] Tonsillectomy is also often done to help with sleep apnea and throat infections.[20] Surgery, however, does not always address the sleep apnea and a continuous positive airway pressure (CPAP) machine may be useful.[39] Physical therapy and participation in physical education may improve motor skills.[100] Evidence to support this in adults, however, is not very good.[101]
Efforts to prevent respiratory syncytial virus (RSV) infection with human monoclonal antibodies should be considered, especially in those with heart problems.[1] In those who develop dementia there is no evidence for memantine,[102] donepezil,[103] rivastigmine,[104] or galantamine.[105]
Plastic surgery has been suggested as a method of improving the appearance and thus the acceptance of people with Down syndrome.[106] It has also been proposed as a way to improve speech.[106] Evidence, however, does not support a meaningful difference in either of these outcomes.[106] Plastic surgery on children with Down syndrome is uncommon,[107] and continues to be controversial.[106] The U.S. National Down Syndrome Society views the goal as one of mutual respect and acceptance, not appearance.[107]
Many alternative medical techniques are used in Down syndrome; however, they are poorly supported by evidence.[106] These include: dietary changes, massage, animal therapy, chiropractic and naturopathy, among others.[106] Some proposed treatments may also be harmful.[61]
Prognosis
Between 5 and 15% of children with Down syndrome in Sweden attend regular school.[108] Some graduate from high school; however, most do not.[17] Of those with intellectual disability in the United States who attended high school about 40% graduated.[109] Many learn to read and write and some are able to do paid work.[17] In adulthood about 20% in the United States do paid work in some capacity.[18][110] In Sweden, however, less than 1% have regular jobs.[108] Many are able to live semi-independently,[12] but they often require help with financial, medical, and legal matters.[9] Those with mosaic Down syndrome usually have better outcomes.[61]
Individuals with Down syndrome have a higher risk of early death than the general population.[20] This is most often from heart problems or infections.[1][8] Following improved medical care, particularly for heart and gastrointestinal problems, the life expectancy has increased.[1] This increase has been from 12 years in 1912,[111] to 25 years in the 1980s,[1] to 50 to 60 years in the developed world in the 2000s.[8][9] Currently between 4 and 12% die in the first year of life.[50] The probability of long-term survival is partly determined by the presence of heart problems. In those with congenital heart problems, 60% survive to 10 years and 50% survive to 30 years of age.[12] In those without heart problems, 85% survive to 10 years and 80% survive to 30 years of age.[12] About 10% live to 70 years of age.[62] The National Down Syndrome Society provide information regarding raising a child with Down syndrome.[112]
Epidemiology
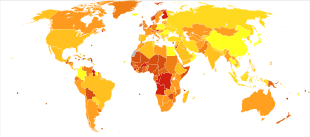
Down syndrome is the most common chromosomal abnormality in humans.[8] Globally, as of 2010, Down syndrome occurs in about 1 per 1,000 births[1] and results in about 17,000 deaths.[113] More children are born with Down syndrome in countries where abortion is not allowed and in countries where pregnancy more commonly occurs at a later age.[1] About 1.4 per 1,000 live births in the United States[114] and 1.1 per 1,000 live births in Norway are affected.[8] In the 1950s, in the United States, it occurred in 2 per 1000 live births with the decrease since then due to prenatal screening and abortions.[71] The number of pregnancies with Down syndrome is more than two times greater with many spontaneously aborting.[9] It is the cause of 8% of all congenital disorders.[1]
Maternal age affects the chances of having a pregnancy with Down syndrome.[3] At age 20, the chance is 1 in 1,441; at age 30, it is 1 in 959; at age 40, it is 1 in 84; and at age 50 it is 1 in 44.[3] Although the probability increases with maternal age, 70% of children with Down syndrome are born to women 35 years of age and younger, because younger people have more children.[3] The father's older age is also a risk factor in women older than 35, but not in women younger than 35, and may partly explain the increase in risk as women age.[115]
History

English physician John Langdon Down first described Down syndrome in 1862, recognizing it as a distinct type of mental disability, and again in a more widely published report in 1866.[20][117][118] Édouard Séguin described it as separate from cretinism in 1844.[21][119] By the 20th century, Down syndrome had become the most recognizable form of mental disability.
In antiquity, many infants with disabilities were either killed or abandoned.[21] In June 2020, the earliest incidence of Down syndrome was found in genomic evidence from an infant that was buried before 3200 BC at Poulnabrone dolmen in Ireland.[120] Researchers believe that a number of historical pieces of art portray Down syndrome, including pottery from the pre-Columbian Tumaco-La Tolita culture in present-day Colombia and Ecuador,[121] and the 16th-century painting The Adoration of the Christ Child.[122][123]
In the 20th century, many individuals with Down syndrome were institutionalized, few of the associated medical problems were treated, and most people died in infancy or early adulthood. With the rise of the eugenics movement, 33 of the then 48 U.S. states and several countries began programs of forced sterilization of individuals with Down syndrome and comparable degrees of disability. Action T4 in Nazi Germany made public policy of a program of systematic involuntary euthanization.[124]
With the discovery of karyotype techniques in the 1950s it became possible to identify abnormalities of chromosomal number or shape.[119] In 1959 Jérôme Lejeune reported the discovery that Down syndrome resulted from an extra chromosome.[20] However, Lejeune's claim to the discovery has been disputed,[125] and in 2014 the Scientific Council of the French Federation of Human Genetics unanimously awarded its Grand Prize to his colleague Marthe Gautier for her role in this discovery.[126] The discovery took place in the laboratory of Raymond Turpin at the Hôpital Trousseau in Paris, France.[127] Jérôme Lejeune and Marthe Gautier were both his students.[128]
As a result of this discovery, the condition became known as trisomy 21.[129] Even before the discovery of its cause, the presence of the syndrome in all races, its association with older maternal age, and its rarity of recurrence had been noticed. Medical texts had assumed it was caused by a combination of inheritable factors that had not been identified. Other theories had focused on injuries sustained during birth.[130]
Society and culture
Name
Due to his perception that children with Down syndrome shared facial similarities with those of Blumenbach's Mongolian race, John Langdon Down used the term "mongoloid".[62][131] He felt that the existence of Down syndrome confirmed that all peoples were genetically related.[132] In the 1950s with discovery of the underlying cause as being related to chromosomes, concerns about the race-based nature of the name increased.[133]
In 1961, 19 scientists suggested that "mongolism" had "misleading connotations" and had become "an embarrassing term".[134][135] The World Health Organization (WHO) dropped the term in 1965 after a request by the delegation from the Mongolian People's Republic.[134] While the term mongoloid (also mongolism, Mongolian imbecility or idiocy) continued to be used until the early 1980s, it is now considered unacceptable and is no longer in common use.[134][136]
In 1975, the United States National Institutes of Health (NIH) convened a conference to standardize the naming and recommended replacing the possessive form, "Down's syndrome" with "Down syndrome".[137] However, both the possessive and nonpossessive forms remain in use by the general population.[138] The term "trisomy 21" is also commonly used.[135][139]
Ethics
Most obstetricians argue that not offering screening for Down syndrome is unethical.[140] As it is a medically reasonable procedure, per informed consent, people should at least be given information about it.[140] It will then be the woman's choice, based on her personal beliefs, how much or how little screening she wishes.[141][142] When results from testing become available, it is also considered unethical not to give the results to the person in question.[140][143]
Some bioethicists deem it reasonable for parents to select a child who would have the highest well-being.[144] One criticism of this reasoning is that it often values those with disabilities less.[145] Some parents argue that Down syndrome shouldn't be prevented or cured and that eliminating Down syndrome amounts to genocide.[146][147] The disability rights movement does not have a position on screening,[148] although some members consider testing and abortion discriminatory.[148] Some in the United States who are anti-abortion support abortion if the fetus is disabled, while others do not.[149] Of a group of 40 mothers in the United States who have had one child with Down syndrome, half agreed to screening in the next pregnancy.[149]
Within the US, some Protestant denominations see abortion as acceptable when a fetus has Down syndrome while Orthodox Christianity and Roman Catholicism do not.[150] Some of those against screening refer to it as a form of "eugenics".[150] Disagreement exists within Islam regarding the acceptability of abortion in those carrying a fetus with Down syndrome.[151] Some Islamic countries allow abortion, while others do not.[151] Women may face stigmatization whichever decision they make.[152]
Advocacy groups
Advocacy groups for individuals with Down syndrome began to be formed after the Second World War.[153] These were organizations advocating for the inclusion of people with Down syndrome into the general school system and for a greater understanding of the condition among the general population,[153] as well as groups providing support for families with children living with Down syndrome.[153] Before this individuals with Down syndrome were often placed in mental hospitals or asylums. Organizations included the Royal Society for Handicapped Children and Adults founded in the UK in 1946 by Judy Fryd,[153][154] Kobato Kai founded in Japan in 1964,[153] the National Down Syndrome Congress founded in the United States in 1973 by Kathryn McGee and others,[153][155] and the National Down Syndrome Society founded in 1979 in the United States.[153] The first Roman Catholic order of nuns for women with Down Syndrome, Little Sisters Disciples of the Lamb, was founded in 1985 in France.[156]
The first World Down Syndrome Day was held on 21 March 2006.[157] The day and month were chosen to correspond with 21 and trisomy, respectively.[158] It was recognized by the United Nations General Assembly in 2011.[157]
Research
Efforts are underway to determine how the extra chromosome 21 material causes Down syndrome, as currently this is unknown,[159] and to develop treatments to improve intelligence in those with the syndrome.[160] Two efforts being studied are the use stem cells[159] and gene therapy.[161][162] Other methods being studied include the use of antioxidants, gamma secretase inhibition, adrenergic agonists, and memantine.[163] Research is often carried out on an animal model, the Ts65Dn mouse.[164]
Other animals
Down syndrome may also occur in animals other than humans. In great apes chromosome 22 corresponds to the human chromosome 21 and thus trisomy 22 causes Down syndrome in apes. The condition was observed in a common chimpanzee in 1969 and a Bornean orangutan in 1979, but neither lived very long. The common chimpanzee Kanako (born around 1993, in Japan) has become the longest-lived known example of this condition. Kanako has some of the same symptoms that are common in human Down syndrome. It is unknown how common this condition is in chimps but it is plausible it could be roughly as common as Down syndrome is in humans.[165][166]
References
- Weijerman, ME; de Winter, JP (Dec 2010). "Clinical practice. The care of children with Down syndrome". European Journal of Pediatrics. 169 (12): 1445–52. doi:10.1007/s00431-010-1253-0. PMC 2962780. PMID 20632187.
- Patterson, D (Jul 2009). "Molecular genetic analysis of Down syndrome". Human Genetics. 126 (1): 195–214. doi:10.1007/s00439-009-0696-8. PMID 19526251.
- Morris, JK; Mutton, DE; Alberman, E (2002). "Revised estimates of the maternal age specific live birth prevalence of Down's syndrome". Journal of Medical Screening. 9 (1): 2–6. doi:10.1136/jms.9.1.2. PMID 11943789.
- "Down syndrome - Symptoms and causes". Mayo Clinic. Retrieved 17 March 2019.
- "How do health care providers diagnose Down syndrome?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2014-01-17. Archived from the original on 7 March 2016. Retrieved 4 March 2016.
- Roizen, NJ; Patterson, D (April 2003). "Down's syndrome". Lancet (Review). 361 (9365): 1281–89. doi:10.1016/S0140-6736(03)12987-X. PMID 12699967.
- "Facts About Down Syndrome". National Association for Down Syndrome. Archived from the original on 3 April 2012. Retrieved 20 March 2012.
- Malt, EA; Dahl, RC; Haugsand, TM; Ulvestad, IH; Emilsen, NM; Hansen, B; Cardenas, YE; Skøld, RO; Thorsen, AT; Davidsen, EM (Feb 5, 2013). "Health and disease in adults with Down syndrome". Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, NY Raekke. 133 (3): 290–94. doi:10.4045/tidsskr.12.0390. PMID 23381164.
- Kliegma, Robert M. (2011). "Down Syndrome and Other Abnormalities of Chromosome Number". Nelson textbook of pediatrics (19th ed.). Philadelphia: Saunders. pp. Chapter 76.2. ISBN 978-1-4377-0755-7.
- GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Hammer, edited by Stephen J. McPhee, Gary D. (2010). "Pathophysiology of Selected Genetic Diseases". Pathophysiology of disease : an introduction to clinical medicine (6th ed.). New York: McGraw-Hill Medical. pp. Chapter 2. ISBN 978-0-07-162167-0.CS1 maint: extra text: authors list (link)
- "What causes Down syndrome?". 2014-01-17. Archived from the original on 5 January 2016. Retrieved 6 January 2016.
- Natoli, JL; Ackerman, DL; McDermott, S; Edwards, JG (Feb 2012). "Prenatal diagnosis of Down syndrome: a systematic review of termination rates (1995–2011)". Prenatal Diagnosis. 32 (2): 142–53. doi:10.1002/pd.2910. PMID 22418958.
- Mansfield, C; Hopfer, S; Marteau, TM (Sep 1999). "Termination rates after prenatal diagnosis of Down syndrome, spina bifida, anencephaly, and Turner and Klinefelter syndromes: a systematic literature review. European Concerted Action: DADA (Decision-making After the Diagnosis of a fetal Abnormality)". Prenatal Diagnosis. 19 (9): 808–12. doi:10.1002/(sici)1097-0223(199909)19:9<808::aid-pd637>3.0.co;2-b. PMID 10521836.
- "Down Syndrome: Other FAQs". 2014-01-17. Archived from the original on 6 January 2016. Retrieved 6 January 2016.
- Steinbock, Bonnie (2011). Life before birth the moral and legal status of embryos and fetuses (2nd ed.). Oxford: Oxford University Press. p. 222. ISBN 978-0-19-971207-6. Archived from the original on 2017-01-23.
- Szabo, Liz (May 9, 2013). "Life with Down syndrome is full of possibilities". USA Today. Archived from the original on 8 January 2014. Retrieved 7 February 2014.
- GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- Hickey, F; Hickey, E; Summar, KL (2012). "Medical update for children with Down syndrome for the pediatrician and family practitioner". Advances in Pediatrics. 59 (1): 137–57. doi:10.1016/j.yapd.2012.04.006. PMID 22789577.
- Evans-Martin, F. Fay (2009). Down syndrome. New York: Chelsea House. p. 12. ISBN 978-1-4381-1950-2.
- Faragher, edited by Rhonda; Clarke, Barbara (2013). Educating Learners with Down Syndrome Research, theory, and practice with children and adolescents. Hoboken: Taylor and Francis. p. 5. ISBN 978-1-134-67335-3. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Sankar, editors John M. Pellock, Blaise F.D. Bourgeois, W. Edwin Dodson; associate editors, Douglas R. Nordli, Jr., Raman (2008). Pediatric epilepsy diagnosis and therapy (3rd ed.). New York: Demos Medical Pub. p. Chapter 67. ISBN 978-1-934559-86-4. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Epstein, Charles J. (2007). The consequences of chromosome imbalance : principles, mechanisms, and models. Cambridge: Cambridge University Press. pp. 255–256. ISBN 978-0-521-03809-6. Archived from the original on 2017-01-23.
- Daniel Bernstein (2012). Pediatrics for medical students (3rd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 259. ISBN 978-0-7817-7030-9. Archived from the original on 2017-01-23.
- Tecklin, Jan S. (2008). Pediatric physical therapy (4th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 380. ISBN 978-0-7817-5399-9. Archived from the original on 2017-01-23.
- Domino, edited by Frank J. (2007). The 5-minute clinical consult 2007 (2007 ed.). Philadelphia: Lippincott Williams & Wilkins. p. 392. ISBN 978-0-7817-6334-9. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Perkins, JA (December 2009). "Overview of macroglossia and its treatment". Current Opinion in Otolaryngology & Head and Neck Surgery. 17 (6): 460–65. doi:10.1097/moo.0b013e3283317f89. PMID 19713845.
- Wilson, Golder N.; Cooley, W. Carl (2006). Preventive management of children with congenital anomalies and syndromes (2 ed.). Cambridge: Cambridge University Press. p. 190. ISBN 978-0-521-61734-5. Archived from the original on 2017-01-23.
- Williams Textbook of Endocrinology Expert Consult (12th ed.). London: Elsevier Health Sciences. 2011. ISBN 978-1-4377-3600-7. Archived from the original on 2017-01-23.
- Rondal, edited by Jean-Adolphe; Quartino, Alberto Rasore (2007). Therapies and rehabilitation in Down syndrome. Chichester, England: J. Wiley & Sons. p. 116. ISBN 978-0-470-31997-0. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Reilly, C (Oct 2012). "Behavioural phenotypes and special educational needs: is aetiology important in the classroom?". Journal of Intellectual Disability Research : JIDR. 56 (10): 929–46. doi:10.1111/j.1365-2788.2012.01542.x. PMID 22471356.
- Batshaw, Mark, ed. (2005). Children with disabilities (5th ed.). Baltimore [u.a.]: Paul H. Brookes. p. 308. ISBN 978-1-55766-581-2. Archived from the original on 2017-01-23.
- Patterson, T; Rapsey, CM; Glue, P (Apr 2013). "Systematic review of cognitive development across childhood in Down syndrome: implications for treatment interventions". Journal of Intellectual Disability Research : JIDR. 57 (4): 306–18. doi:10.1111/j.1365-2788.2012.01536.x. PMID 23506141.
- Kent, RD; Vorperian, HK (Feb 2013). "Speech impairment in Down syndrome: a review". Journal of Speech, Language, and Hearing Research. 56 (1): 178–210. doi:10.1044/1092-4388(2012/12-0148). PMC 3584188. PMID 23275397.
- McGuire, Dennis and Chicoine, Brian (2006). Mental Wellness in Adults with Down Syndrome. Bethesday, MD: Woodbine House, Inc. p. 49. ISBN 978-1-890627-65-2.
- Margulies, Phillip (2007). Down syndrome (1st ed.). New York: Rosen Pub. Group. p. 5. ISBN 978-1-4042-0695-3.
- M. William Schwartz, ed. (2012). The 5-minute pediatric consult (6th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 289. ISBN 978-1-4511-1656-4. Archived from the original on 2017-01-23.
- Rodman, R; Pine, HS (Jun 2012). "The otolaryngologist's approach to the patient with Down syndrome". Otolaryngologic Clinics of North America. 45 (3): 599–629, vii–viii. doi:10.1016/j.otc.2012.03.010. PMID 22588039.
- Evans-Martin, F. Fay (2009). Down syndrome. New York: Chelsea House. p. 71. ISBN 978-1-4381-1950-2.
- Tintinalli, Judith E. (2010). "The Child with Special Health Care Needs". Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. Chapter 138. ISBN 978-0-07-148480-0.
- Sam Goldstein, ed. (2011). Handbook of neurodevelopmental and genetic disorders in children (2nd ed.). New York: Guilford Press. p. 365. ISBN 978-1-60623-990-2. Archived from the original on 2017-01-23.
- editor, Vee P. Prasher (2009). Neuropsychological assessments of dementia in Down syndrome and intellectual disabilities. London: Springer. p. 56. ISBN 978-1-84800-249-4. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Richard Urbano (9 September 2010). Health Issues Among Persons With Down Syndrome. Academic Press. p. 129. ISBN 978-0-12-374477-7. Archived from the original on 12 May 2015.
- Nixon DW (March 2018). "Down Syndrome, Obesity, Alzheimer's Disease, and Cancer: A Brief Review and Hypothesis". Brain Sciences. 8 (4): 53. doi:10.3390/brainsci8040053. PMC 5924389. PMID 29587359.
- Seewald, L; Taub, JW; Maloney, KW; McCabe, ER (Sep 2012). "Acute leukemias in children with Down syndrome". Molecular Genetics and Metabolism. 107 (1–2): 25–30. doi:10.1016/j.ymgme.2012.07.011. PMID 22867885.
- Seewald L, Taub JW, Maloney KW, McCabe ER (September 2012). "Acute leukemias in children with Down syndrome". Molecular Genetics and Metabolism. 107 (1–2): 25–30. doi:10.1016/j.ymgme.2012.07.011. PMID 22867885.
- Lee P, Bhansali R, Izraeli S, Hijiya N, Crispino JD (September 2016). "The biology, pathogenesis and clinical aspects of acute lymphoblastic leukemia in children with Down syndrome". Leukemia. 30 (9): 1816–23. doi:10.1038/leu.2016.164. PMC 5434972. PMID 27285583.
- Tamblyn JA, Norton A, Spurgeon L, Donovan V, Bedford Russell A, Bonnici J, Perkins K, Vyas P, Roberts I, Kilby MD (January 2016). "Prenatal therapy in transient abnormal myelopoiesis: a systematic review". Archives of Disease in Childhood: Fetal and Neonatal Edition. 101 (1): F67–71. doi:10.1136/archdischild-2014-308004. PMID 25956670.
- Gamis, AS; Smith, FO (Nov 2012). "Transient myeloproliferative disorder in children with Down syndrome: clarity to this enigmatic disorder". British Journal of Haematology. 159 (3): 277–87. doi:10.1111/bjh.12041. PMID 22966823.
- Bhatnagar N, Nizery L, Tunstall O, Vyas P, Roberts I (October 2016). "Transient Abnormal Myelopoiesis and AML in Down Syndrome: an Update". Current Hematologic Malignancy Reports. 11 (5): 333–41. doi:10.1007/s11899-016-0338-x. PMC 5031718. PMID 27510823.
- Andrei Thomas-Tikhonenko, ed. (2010). Cancer genome and tumor microenvironment (Online-Ausg. ed.). New York: Springer. p. 203. ISBN 978-1-4419-0711-0. Archived from the original on 2015-07-04.
- Graber, E; Chacko, E; Regelmann, MO; Costin, G; Rapaport, R (Dec 2012). "Down syndrome and thyroid function". Endocrinology and Metabolism Clinics of North America. 41 (4): 735–45. doi:10.1016/j.ecl.2012.08.008. PMID 23099267.
- Moore, SW (Aug 2008). "Down syndrome and the enteric nervous system". Pediatric Surgery International. 24 (8): 873–83. doi:10.1007/s00383-008-2188-7. PMID 18633623.
- Cawson, R.A.; Odell, E.W. (2012). Cawson's essentials of oral pathology and oral medicine (8th ed.). Edinburgh: Churchill Livingstone. pp. 419–421. ISBN 978-0443-10125-0.
- Carranza, [edited by] Michael G. Newman, Henry H. Takei, Perry R. Klokkevold; editor emeritus Fermin A. (2006). Carranza's clinical periodontology (10th ed.). Philadelphia: W.B. Saunders Co. pp. 299, 397, 409, 623. ISBN 978-1-4160-2400-2.CS1 maint: extra text: authors list (link)
- Dean, Ralph E. McDonald; David R. Avery; Jeffrey A. (2004). Dentistry for the child and adolescent (8. ed.). St. Louis, Mo: Mosby. pp. 164–168, 190–194, 474. ISBN 978-0-323-02450-1.
- Wysocki, J. Philip Sapp; Lewis R. Eversole; George P. (2002). Contemporary oral and maxillofacial pathology (2nd ed.). St. Louis: Mosby. pp. 39–40. ISBN 978-0-323-01723-7.
- Regezi, Joseph A; Sciubba, James J; Jordan, Richard C K (2008). Oral Pathology: Clinical Pathologic Correlations (5th ed.). St Louis, Missouri: Saunders Elsevier. pp. 353–354. ISBN 978-1455702626.
- Pradhan, M; Dalal, A; Khan, F; Agrawal, S (2006). "Fertility in men with Down syndrome: a case report". Fertil Steril. 86 (6): 1765.e1–3. doi:10.1016/j.fertnstert.2006.03.071. PMID 17094988.
- Nelson, Maureen R. (2011). Pediatrics. New York: Demos Medical. p. 88. ISBN 978-1-61705-004-6. Archived from the original on 2017-01-23.
- Howard Reisner (2013). Essentials of Rubin's Pathology. Lippincott Williams & Wilkins. pp. 129–131. ISBN 978-1-4511-8132-6. Archived from the original on 2017-01-23.
- Lana-Elola, E; Watson-Scales, SD; Fisher, EM; Tybulewicz, VL (Sep 2011). "Down syndrome: searching for the genetic culprits". Disease Models & Mechanisms. 4 (5): 586–95. doi:10.1242/dmm.008078. PMC 3180222. PMID 21878459.
- "CDC—Birth Defects, Down Syndrome—NCBDDD". Cdc.gov. 2013-11-06. Archived from the original on 2017-07-28.
- Kausik Mandal (2013). Treatment & prognosis in pediatrics. Jaypee Brothers Medical P. p. 391. ISBN 978-93-5090-428-2. Archived from the original on 2017-01-23.
- Fletcher-Janzen, edited by Cecil R. Reynolds, Elaine (2007). Encyclopedia of special education a reference for the education of children, adolescents, and adults with disabilities and other exceptional individuals (3rd ed.). New York: John Wiley & Sons. p. 458. ISBN 978-0-470-17419-7. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- Zhang, edited by Liang Cheng, David Y. (2008). Molecular genetic pathology. Totowa, N.J.: Humana. p. 45. ISBN 978-1-59745-405-6. Archived from the original on 2017-01-23.CS1 maint: extra text: authors list (link)
- A.K. David (2013). Family Medicine Principles and Practice (Sixth ed.). New York, NY: Springer New York. p. 142. ISBN 978-0-387-21744-4. Archived from the original on 2017-01-23.
- Michael Cummings (2013). Human Heredity: Principles and Issues (10 ed.). Cengage Learning. p. 138. ISBN 978-1-285-52847-2. Archived from the original on 2017-01-23.
- Jerome Frank Strauss; Robert L. Barbieri (2009). Yen and Jaffe's reproductive endocrinology : physiology, pathophysiology, and clinical management (6th ed.). Philadelphia, PA: Saunders/Elsevier. p. 791. ISBN 978-1-4160-4907-4. Archived from the original on 2017-01-23.
- Menkes, John H.; Sarnat, Harvey B. (2005). Child neurology (7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. p. 228. ISBN 978-0-7817-5104-9. Archived from the original on 2017-01-23.
- Shaffer, R.J. McKinlay Gardner, Grant R. Sutherland, Lisa G. (2012). Chromosome abnormalities and genetic counseling (4th ed.). Oxford: Oxford University Press. p. 292. ISBN 978-0-19-974915-7. Archived from the original on 2017-01-23.
- "Genetics of Down syndrome". Archived from the original on 2011-05-27. Retrieved 2011-05-29.
- Michael H. Ebert, ed. (2008). "Psychiatric Genetics". Current diagnosis & treatment psychiatry (2nd ed.). New York: McGraw-Hill Medical. pp. Chapter 3. ISBN 978-0-07-142292-5.
- Patterson, D; Cabelof, DC (April 2012). "Down syndrome as a model of DNA polymerase beta haploinsufficiency and accelerated aging". Mechanisms of Ageing and Development. 133 (4): 133–37. doi:10.1016/j.mad.2011.10.001. PMID 22019846.
- Weksler, ME; Szabo, P; Relkin, NR; Reidenberg, MM; Weksler, BB; Coppus, AM (Apr 2013). "Alzheimer's disease and Down's syndrome: treating two paths to dementia". Autoimmunity Reviews. 12 (6): 670–73. doi:10.1016/j.autrev.2012.10.013. PMID 23201920.
- Horvath S, Garagnani P, Bacalini MG, Pirazzini C, Salvioli S, Gentilini D, Di Blasio AM, Giuliani C, Tung S, Vinters HV, Franceschi C (2015). "Accelerated epigenetic aging in Down syndrome". Aging Cell. 14 (3): 491–95. doi:10.1111/acel.12325. PMC 4406678. PMID 25678027.
- ACOG Committee on Practice, Bulletins (Jan 2007). "ACOG Practice Bulletin No. 77: screening for fetal chromosomal abnormalities". Obstetrics and Gynecology. 109 (1): 217–27. doi:10.1097/00006250-200701000-00054. PMID 17197615.
- Canick, J (Jun 2012). "Prenatal screening for trisomy 21: recent advances and guidelines". Clinical Chemistry and Laboratory Medicine. 50 (6): 1003–08. doi:10.1515/cclm.2011.671. PMID 21790505.
- Tabor, A; Alfirevic, Z (2010). "Update on procedure-related risks for prenatal diagnosis techniques". Fetal Diagnosis and Therapy. 27 (1): 1–7. doi:10.1159/000271995. PMID 20051662.
- Graham, Ruth (2018-05-31). "How Down Syndrome Is Redefining the Abortion Debate". Slate Magazine. Retrieved 2019-01-09.
- Choi, H; Van Riper, M; Thoyre, S (Mar–Apr 2012). "Decision making following a prenatal diagnosis of Down syndrome: an integrative review". Journal of Midwifery & Women's Health. 57 (2): 156–64. doi:10.1111/j.1542-2011.2011.00109.x. PMID 22432488.
- National Institute for Health and Clinical Excellence (2008). "CG62: Antenatal care". London: National Institute for Health and Clinical Excellence. Archived from the original on 26 January 2013. Retrieved 16 February 2013.
- "Noninvasive prenatal diagnosis of fetal aneuploidy using cell-free fetal nucleic acids in maternal blood" (PDF). United Healthcare Oxford. Archived (PDF) from the original on 7 March 2014. Retrieved 25 March 2014.
- Mersy E, Smits LJ, van Winden LA, de Die-Smulders CE, Paulussen AD, Macville MV, Coumans AB, Frints SG (Jul–Aug 2013). "Noninvasive detection of fetal trisomy 21: systematic review and report of quality and outcomes of diagnostic accuracy studies performed between 1997 and 2012". Human Reproduction Update. 19 (4): 318–29. doi:10.1093/humupd/dmt001. PMID 23396607.
- Bianchi DW, Parker RL, Wentworth J, Madankumar R, Saffer C, Das AF, Craig JA, Chudova DI, Devers PL, Jones KW, Oliver K, Rava RP, Sehnert AJ (Feb 27, 2014). "DNA sequencing versus standard prenatal aneuploidy screening". The New England Journal of Medicine. 370 (9): 799–808. doi:10.1056/nejmoa1311037. PMID 24571752.
- Agathokleous, M; Chaveeva, P; Poon, LC; Kosinski, P; Nicolaides, KH (Mar 2013). "Meta-analysis of second-trimester markers for trisomy 21". Ultrasound in Obstetrics & Gynecology. 41 (3): 247–61. doi:10.1002/uog.12364. PMID 23208748.
- Malone FD, D'Alton ME (Nov 2003). "First-trimester sonographic screening for Down syndrome". Obstetrics and Gynecology. 102 (5 Pt 1): 1066–79. doi:10.1016/j.obstetgynecol.2003.08.004. PMID 14672489.
- Alldred, SK; Deeks, JJ; Guo, B; Neilson, JP; Alfirevic, Z (Jun 13, 2012). "Second trimester serum tests for Down's Syndrome screening" (PDF). The Cochrane Database of Systematic Reviews. 6 (6): CD009925. doi:10.1002/14651858.CD009925. PMC 7086392. PMID 22696388.
- Verweij EJ, van den Oever JM, de Boer MA, Boon EM, Oepkes D (2012). "Diagnostic accuracy of noninvasive detection of fetal trisomy 21 in maternal blood: a systematic review". Fetal Diagnosis and Therapy. 31 (2): 81–86. doi:10.1159/000333060. PMID 22094923.
- Benn, P; Borrell, A; Cuckle, H; Dugoff, L; Gross, S; Johnson, JA; Maymon, R; Odibo, A; Schielen, P; Spencer, K; Wright, D; Yaron, Y (Jan 2012). "Prenatal Detection of Down Syndrome using Massively Parallel Sequencing (MPS): a rapid response statement from a committee on behalf of the Board of the International Society for Prenatal Diagnosis, 24 October 2011" (PDF). Prenatal Diagnosis. 32 (1): 1–2. doi:10.1002/pd.2919. PMID 22275335. Archived from the original (PDF) on 2012-03-19.
- Sheets KB, Crissman BG, Feist CD, et al. (October 2011). "Practice guidelines for communicating a prenatal or postnatal diagnosis of Down syndrome: recommendations of the national society of genetic counselors". J Genet Couns. 20 (5): 432–41. doi:10.1007/s10897-011-9375-8. PMID 21618060.
- Bull, MJ; Committee on, Genetics (Aug 2011). "Health supervision for children with Down syndrome". Pediatrics. 128 (2): 393–406. doi:10.1542/peds.2011-1605. PMID 21788214.
- Roberts, JE; Price, J; Malkin, C (2007). "Language and communication development in Down syndrome". Ment Retard Dev Disabil Res Rev. 13 (1): 26–35. doi:10.1002/mrdd.20136. PMID 17326116.
- "Inclusion: Educating Students with Down Syndrome with Their Non-Disabled Peers" (PDF). National Down Syndrome Society. Archived (PDF) from the original on 27 November 2014. Retrieved 5 February 2014.
- Lindsay, G (Mar 2007). "Educational psychology and the effectiveness of inclusive education/mainstreaming". The British Journal of Educational Psychology. 77 (Pt 1): 1–24. doi:10.1348/000709906x156881. PMID 17411485. S2CID 28040160.
- New, Rebecca S.; Cochran, Moncrieff (2007). Early childhood education an international encyclopedia. Westport, Conn.: Praeger Publishers. p. 305. ISBN 978-0-313-01448-2. Archived from the original on 2017-01-23.
- "Development and learning for people with Down syndrome". Archived from the original on 2016-11-19. Retrieved 2016-11-18.
- "Early Intervention – National Down Syndrome Society". www.ndss.org. Archived from the original on 2016-11-19. Retrieved 2016-11-18.
- Wearmouth, Janice (2012). Special educational needs, the basics. Milton Park, Abingdon, Oxon: Routledge. p. 66. ISBN 978-1-136-57989-9. Archived from the original on 2015-05-12.
- Andriolo RB, El Dib RP, Ramos L, Atallah AN, da Silva EM (May 12, 2010). "Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome". The Cochrane Database of Systematic Reviews (5): CD005176. doi:10.1002/14651858.CD005176.pub4. PMID 20464738.
- Mohan, M; Bennett, C; Carpenter, PK (Jan 21, 2009). "Memantine for dementia in people with Down syndrome". The Cochrane Database of Systematic Reviews (1): CD007657. doi:10.1002/14651858.CD007657. PMC 7197456. PMID 19160343.
- Mohan, M; Carpenter, PK; Bennett, C (Jan 21, 2009). "Donepezil for dementia in people with Down syndrome". The Cochrane Database of Systematic Reviews (1): CD007178. doi:10.1002/14651858.CD007178.pub2. PMC 7208846. PMID 19160328.
- Mohan, M; Bennett, C; Carpenter, PK (Jan 21, 2009). "Rivastigmine for dementia in people with Down syndrome". The Cochrane Database of Systematic Reviews (1): CD007658. doi:10.1002/14651858.CD007658. PMC 7197503. PMID 19160344.
- Mohan, M; Bennett, C; Carpenter, PK (Jan 21, 2009). "Galantamine for dementia in people with Down syndrome". The Cochrane Database of Systematic Reviews (1): CD007656. doi:10.1002/14651858.CD007656. PMC 7197502. PMID 19160342.
- Roizen, NJ (2005). "Complementary and alternative therapies for Down syndrome". Mental Retardation and Developmental Disabilities Research Reviews. 11 (2): 149–55. doi:10.1002/mrdd.20063. PMID 15977315.
- National Down Syndrome Society. "Position Statement on Cosmetic Surgery for Children with Down Syndrome". Archived from the original on 2006-09-06. Retrieved 2006-06-02.
- "European Down Syndrome Association news" (PDF). European Down Syndrome Association. 2006. Archived from the original (PDF) on 22 February 2014. Retrieved 7 February 2014.
- "Number of 14- through 21-year-old students served under Individuals with Disabilities Education Act, Part B, who exited school, by exit reason, age, and type of disability: 2007–08 and 2008–09". National Center for Education Statistics. Archived from the original on 22 February 2014. Retrieved 7 February 2014.
- "Down's Syndrome: Employment Barriers". Rehab Care International. Archived from the original on 22 February 2014. Retrieved 7 February 2014.
- Richard Urbano (9 September 2010). Health Issues Among Persons With Down Syndrome. Academic Press. p. 108. ISBN 978-0-12-374477-7. Archived from the original on 12 May 2015.
- "Where Should I Go From Here?". Archived from the original on 22 December 2015. Retrieved 19 December 2015.
- Lozano, R; Naghavi, M; Foreman, K; Lim, S; Shibuya, K; Aboyans, V; Abraham, J; Adair, T; Aggarwal, R; Ahn, S. Y.; Alvarado, M; Anderson, H. R.; Anderson, L. M.; Andrews, K. G.; Atkinson, C; Baddour, L. M.; Barker-Collo, S; Bartels, D. H.; Bell, M. L.; Benjamin, E. J.; Bennett, D; Bhalla, K; Bikbov, B; Bin Abdulhak, A; Birbeck, G; Blyth, F; Bolliger, I; Boufous, S; Bucello, C; et al. (Dec 15, 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604.
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, Correa A (Dec 2010). "Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006". Birth Defects Research. Part A, Clinical and Molecular Teratology. 88 (12): 1008–16. doi:10.1002/bdra.20735. PMID 20878909.
- Douglas T. Carrell, ed. (2013). Paternal influences on human reproductive success. Cambridge University Press. p. 65. ISBN 978-1-107-02448-9. Archived from the original on 2017-01-23.
- Levitas, AS; Reid, CS (Feb 1, 2003). "An angel with Down syndrome in a sixteenth century Flemish Nativity painting". American Journal of Medical Genetics Part A. 116A (4): 399–405. doi:10.1002/ajmg.a.10043. PMID 12522800.
We have identified a 16th-century Flemish Nativity painting in which one angelic figure appears distinctly different from other individuals in the painting with an appearance of Down syndrome.
- Down, JLH (1866). "Observations on an ethnic classification of idiots". Clinical Lecture Reports, London Hospital. 3: 259–62. Archived from the original on 2006-06-15. Retrieved 2006-07-14.
- Conor, WO (1998). John Langdon Down, 1828–1896. Royal Society of Medicine Press. ISBN 978-1-85315-374-7.
- Neri, G; Opitz, JM (Dec 2009). "Down syndrome: comments and reflections on the 50th anniversary of Lejeune's discovery". American Journal of Medical Genetics Part A. 149A (12): 2647–54. doi:10.1002/ajmg.a.33138. PMID 19921741.
- "Genetics study shines light on early periods of Ireland's human history". www.rte.ie. Raidió Teilifís Éireann. 17 June 2020. Retrieved 17 June 2020.
- Bernal, J.E.; Briceno, I. (September 2006). "Genetic and other diseases in the pottery of Tumaco-La Tolita culture in Colombia-Ecuador". Clinical Genetics. 70 (3): 188–91. doi:10.1111/j.1399-0004.2006.00670.x. PMID 16922718.
- Evans-Martin, F. Fay (2009). Down Syndrome. Genes & Disease. New York: Infobase Publishing. p. 13. ISBN 9781438119502. Retrieved 20 March 2020.
There is also very little representation of Down syndrome in art over the centuries. Only a few paintings, such as the sixteenth century Flemish painting The Adoration of the Christ Child, have been identified in which characters appear appear to have facial features and other characteristics typical of Down syndrome.
- Evans-Martin, F. Fay (2009). Down Syndrome. New York: Chelsea House. pp. 13–14. ISBN 978-1-4381-1950-2.
- David Wright (25 August 2011). Downs:The history of a disability: The history of a disability. Oxford University Press. pp. 104–108. ISBN 978-0-19-956793-5. Archived from the original on 28 May 2013. Retrieved 25 August 2012.
- David Wright (25 August 2011). Downs:The history of a disability: The history of a disability. Oxford University Press. p. 145. ISBN 978-0-19-956793-5. Archived from the original on 28 May 2013. Retrieved 25 August 2012.
- "Trisomie : une pionnière intimidée". Le Monde. Feb 3, 2014. Retrieved 25 March 2014.
- Gautier, Marthe and Peter S. Harper (2009). "Fiftieth anniversary of trisomy 21: returning to a discovery" (PDF). Human Genetics. 126 (2): 317–324. doi:10.1007/s00439-009-0690-1. Archived (PDF) from the original on 2017-02-02.
- Pain, Elisabeth (2014). "After More Than 50 Years, a Dispute Over Down Syndrome Discovery". Science. 343 (6172): 720–721. doi:10.1126/science.343.6172.720. PMID 24531949.
- David Wright (25 August 2011). Downs:The history of a disability: The history of a disability. Oxford University Press. pp. 9–10. ISBN 978-0-19-956793-5. Archived from the original on 28 May 2013. Retrieved 25 August 2012.
- Warkany, J (1971). Congenital Malformations. Chicago: Year Book Medical Publishers, Inc. pp. 313–14. ISBN 978-0-8151-9098-1.
- Ward, OC (Aug 1999). "John Langdon Down: the man and the message". Down Syndrome Research and Practice. 6 (1): 19–24. doi:10.3104/perspectives.94. PMID 10890244.
- Gould, Stephen (2010). The Panda's Thumb: More Reflections in Natural History. W. W. Norton & Company. p. 166. ISBN 9780393340839. Archived from the original on 2017-09-11.
- Keevak, Michael (2011). Becoming Yellow: A Short History of Racial Thinking. Princeton University Press. p. 120. ISBN 978-1400838608. Archived from the original on 2017-09-11.
- Howard-Jones, Norman (1979). "On the diagnostic term "Down's disease"". Medical History. 23 (1): 102–04. doi:10.1017/s0025727300051048. PMC 1082401. PMID 153994.
- Rodríguez-Hernández, ML; Montoya, E (Jul 30, 2011). "Fifty years of evolution of the term Down's syndrome". Lancet. 378 (9789): 402. doi:10.1016/s0140-6736(11)61212-9. PMID 21803206.
- Rodríguez-Hernández, ML; Montoya, E (30 July 2011). "Fifty years of evolution of the term Down's syndrome". Lancet. 378 (9789): 402. doi:10.1016/s0140-6736(11)61212-9. PMID 21803206.
- "Classification and nomenclature of morphological defects (Discussion)". The Lancet. 305 (7905): 513. 1975. doi:10.1016/S0140-6736(75)92847-0. PMID 46972. S2CID 37636187.
- Smith, Kieron (2011). The politics of Down syndrome. [New Alresford, Hampshire]: Zero. p. 3. ISBN 978-1-84694-613-4. Archived from the original on 2017-01-23.
- Westman, Judith A. (2005). Medical genetics for the modern clinician. Philadelphia, PA: Lippincott Williams & Wilkins. p. 136. ISBN 978-0-7817-5760-7.
- Chervenak, FA; McCullough, LB (Apr 2010). "Ethical considerations in first-trimester Down syndrome risk assessment". Current Opinion in Obstetrics and Gynecology. 22 (2): 135–38. doi:10.1097/gco.0b013e3283374a9f. PMID 20125014.
- Chervenak, FA; McCullough, LB; Sharma, G; Davis, J; Gross, S (Jul 2008). "Enhancing patient autonomy with risk assessment and invasive diagnosis: an ethical solution to a clinical challenge". American Journal of Obstetrics and Gynecology. 199 (1): 19.e1–4. doi:10.1016/j.ajog.2008.02.021. PMID 18355783.
- Zindler, L (Apr–Jun 2005). "Ethical decision making in first trimester pregnancy screening". The Journal of Perinatal & Neonatal Nursing. 19 (2): 122–31, quiz 132–33. doi:10.1097/00005237-200504000-00008. PMID 15923961. S2CID 45181967.
- Sharma, G; McCullough, LB; Chervenak, FA (Feb 15, 2007). "Ethical considerations of early (first vs. second trimester) risk assessment disclosure for trisomy 21 and patient choice in screening versus diagnostic testing". American Journal of Medical Genetics Part C. 145C (1): 99–104. doi:10.1002/ajmg.c.30118. PMID 17299736.
- Savulescu, J; Kahane, G (Jun 2009). "The moral obligation to create children with the best chance of the best life". Bioethics. 23 (5): 274–90. doi:10.1111/j.1467-8519.2008.00687.x. PMID 19076124.
- Bennett, R (Jun 2009). "The fallacy of the Principle of Procreative Beneficence". Bioethics. 23 (5): 265–73. doi:10.1111/j.1467-8519.2008.00655.x. PMID 18477055.
- "Halifax mom questions Down syndrome suppression". Archived from the original on 2015-11-05. Retrieved 2015-09-26.
- Belkin, Lisa (2010-01-11). "Should Down Syndrome Be Cured?". Archived from the original on 2015-04-25. Retrieved 2015-09-26.
- Parens, E; Asch, A (2003). "Disability rights critique of prenatal genetic testing: reflections and recommendations". Mental Retardation and Developmental Disabilities Research Reviews. 9 (1): 40–47. doi:10.1002/mrdd.10056. PMID 12587137.
- Green, RM (Spring 1997). "Parental autonomy and the obligation not to harm one's child genetically". The Journal of Law, Medicine & Ethics. 25 (1): 5–15, 2. doi:10.1111/j.1748-720x.1997.tb01389.x. PMID 11066476.
- Bill J. Leonard; Jill Y. Crainshaw (2013). Encyclopedia of religious controversies in the United States (2nd ed.). Santa Barbara, Calif.: ABC-CLIO. p. 278. ISBN 978-1-59884-867-0. Archived from the original on 2017-01-23.
- Al-Alaiyan, S; Alfaleh, KM (Jan 2012). "Aborting a Malformed Fetus: A Debatable Issue in Saudi Arabia". Journal of Clinical Neonatology. 1 (1): 6–11. doi:10.4103/2249-4847.92231. PMC 3761984. PMID 24027674.
- Sara Grace Shields; Lucy M. Candib (2010). Woman-centered care in pregnancy and childbirth. Oxford: Radcliffe Pub. p. 140. ISBN 978-1-84619-161-9. Archived from the original on 2017-01-23.
- David Wright (2011). Downs: The history of a disability. Oxford University Press. p. 147. ISBN 978-0-19-161978-6. Archived from the original on 2017-01-23.
- "Timeline". MENCAP. Archived from the original on 17 June 2011. Retrieved 2 February 2014.
- "National Down Syndrome Organizations in the U.S." Global Down Syndrome Foundation. 2012-02-21. Archived from the original on 18 January 2014. Retrieved 2 February 2014.
- Vet, Cyprien (July 24, 2019). "Religious Sisters with Down syndrome: the joy of shared contemplative life". Vatican News. Retrieved July 31, 2019.
- "World Down Syndrome Day". Down Syndrome International. Down Syndrome International. Archived from the original on 14 March 2014. Retrieved 2 February 2014.
- Pratt, Geraldine; Rosner, Victoria (2012). The global and the intimate feminism in our time. New York: Columbia University Press. p. 113. ISBN 978-0-231-52084-3. Archived from the original on 2017-01-23.
- Briggs, JA; Mason, EA; Ovchinnikov, DA; Wells, CA; Wolvetang, EJ (Mar 2013). "Concise review: new paradigms for Down syndrome research using induced pluripotent stem cells: tackling complex human genetic disease". Stem Cells Translational Medicine. 2 (3): 175–84. doi:10.5966/sctm.2012-0117. PMC 3659762. PMID 23413375.
- Goodman, MJ; Brixner, DI (Apr 2013). "New therapies for treating Down syndrome require quality of life measurement". American Journal of Medical Genetics Part A. 161A (4): 639–41. doi:10.1002/ajmg.a.35705. PMID 23495233.
- Mole, Beth (2013). "Researchers turn off Down's syndrome genes". Nature News. doi:10.1038/nature.2013.13406. Retrieved 25 December 2018.
- Fillat, C; Altafaj, X (2012). Gene therapy for Down syndrome. Progress in Brain Research. 197. pp. 237–47. doi:10.1016/B978-0-444-54299-1.00012-1. ISBN 9780444542991. PMID 22541296.
- Costa, AC; Scott-McKean, JJ (Sep 2013). "Prospects for improving brain function in individuals with Down syndrome". CNS Drugs. 27 (9): 679–702. doi:10.1007/s40263-013-0089-3. PMID 23821040.
- Costa, AC (2011). "On the promise of pharmacotherapies targeted at cognitive and neurodegenerative components of Down syndrome". Developmental Neuroscience. 33 (5): 414–27. doi:10.1159/000330861. PMC 3254040. PMID 21893967.
- Hirata, S; Hirai, H; Nogami, E; Morimura, N; Udono, T (April 2017). "Chimpanzee Down syndrome: a case study of trisomy 22 in a captive chimpanzee". Primates; Journal of Primatology. 58 (2): 267–273. doi:10.1007/s10329-017-0597-8. hdl:2433/228259. PMID 28220267.
- "Second case of 'Down syndrome' in chimpanzees identified in Japan". UPI. Retrieved 11 May 2019.
External links
| Wikimedia Commons has media related to Down syndrome. |
| Classification | |
|---|---|
| External resources |