Antidepressant
Antidepressants are medications used to treat major depressive disorder, some anxiety disorders, some chronic pain conditions, and to help manage some addictions.[1] Common side-effects of antidepressants include dry mouth, weight gain, dizziness, headaches, sexual dysfunction,[2][3][4][5][6] and emotional blunting.[7][8][9] Most types of antidepressants are typically safe to take, but may cause increased thoughts of suicide when taken by children, adolescents, and young adults.[10] A discontinuation syndrome can occur after stopping any antidepressant which resembles recurrent depression.[11][12]
| Antidepressant | |
|---|---|
| Drug class | |
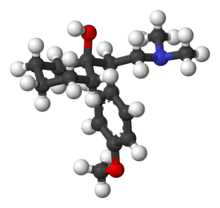
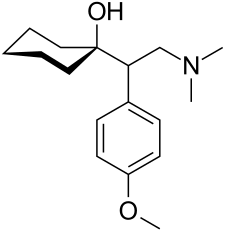 The skeleton structure of the SNRI venlafaxine, a typical example of an antidepressant. | |
| Class identifiers | |
| Use | Depressive disorders |
| ATC code | N06A |
| Clinical data | |
| Drugs.com | Drug Classes |
| Consumer Reports | Best Buy Drugs |
| WebMD | MedicineNet RxList |
| External links | |
| MeSH | D000928 |
| In Wikidata | |
Some reviews of antidepressants for depression in adults find benefit[13] while others do not.[14] Evidence of benefit in children and adolescents is unclear.[15] There is debate in the medical community about how much of the observed effects of antidepressants can be attributed to the placebo effect.[16][17] Most research on whether antidepressant drugs work is done on people with very severe symptoms,[18] so the results cannot be extrapolated to the general population.[19]
There are methods for managing depression which do not involve medications or may be used in conjunction with medications.
Medical uses
Antidepressants are used to treat major depressive disorder and of other conditions, including some anxiety disorders, some chronic pain conditions, and to help manage some addictions. Antidepressants are often used in combinations with one another.[1] The proponents of the monoamine hypothesis of depression recommend choosing the antidepressant with the mechanism of action impacting the most prominent symptoms—for example, they advocate that people with MDD who are also anxious or irritable should be treated with SSRIs or norepinephrine reuptake inhibitors, and the ones with the loss of energy and enjoyment of life—with norepinephrine and dopamine enhancing drugs.[20]
Major depressive disorder
The UK National Institute for Health and Care Excellence (NICE) 2009 guidelines indicate that antidepressants should not be routinely used for the initial treatment of mild depression, because the risk-benefit ratio is poor. The guidelines recommended that antidepressant treatment be considered for:
- People with a history of moderate or severe depression,
- Those with mild depression that has been present for a long period,
- As a second-line treatment for mild depression that persists after other interventions,
- As a first-line treatment for moderate or severe depression.
The guidelines further note that antidepressant treatment should be used in combination with psychosocial interventions in most cases, should be continued for at least six months to reduce the risk of relapse, and that SSRIs are typically better tolerated than other antidepressants.[21]
American Psychiatric Association treatment guidelines recommend that initial treatment should be individually tailored based on factors that include severity of symptoms, co-existing disorders, prior treatment experience, and the person's preference. Options may include pharmacotherapy, psychotherapy, electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS) or light therapy. They recommended antidepressant medication as an initial treatment choice in people with mild, moderate, or severe major depression, that should be given to all people with severe depression unless ECT is planned.[22]
Some reviews of antidepressants in adults with depression find benefits[19][13] while others do not.[14]
Anxiety disorders
Generalized anxiety disorder
Antidepressants are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of generalized anxiety disorder (GAD) that has failed to respond to conservative measures such as education and self-help activities. GAD is a common disorder of which the central feature is excessive worry about a number of different events. Key symptoms include excessive anxiety about multiple events and issues, and difficulty controlling worrisome thoughts that persists for at least 6 months.
Antidepressants provide a modest-to-moderate reduction in anxiety in GAD.[23] The efficacy of different antidepressants is similar.[23]
Social anxiety disorder
Some antidepressants are used as a treatment for social anxiety disorder, but their efficacy is not entirely convincing, as only a small proportion of antidepressants showed some efficacy for this condition. Paroxetine was the first drug to be FDA-approved for this disorder. Its efficacy is considered beneficial, although not everyone responds favorably to the drug. Sertraline and fluvoxamine extended release were later approved for it as well, while escitalopram is used off-label with acceptable efficacy. However, there isn't enough evidence to support citalopram for treating social phobia, and fluoxetine was no better than placebo in clinical trials. SSRIs are used as a first-line treatment for social anxiety, but they don't work for everyone. One alternative would be venlafaxine, which is a SNRI. It showed benefits for social phobia in five clinical trials against placebo, while the other SNRIs are not considered particularly useful for this disorder as many of them didn't undergo testing for it. As of now, it is unclear if duloxetine and desvenlafaxine can provide benefits for social anxiety sufferers. However, another class of antidepressants called MAOIs are considered effective for social anxiety, but they come with many unwanted side effects and are rarely used. Phenelzine was shown to be a good treatment option, but its use is limited by dietary restrictions. Moclobemide is a RIMA and showed mixed results but still got approval in some European countries for social anxiety disorder. TCA antidepressants, such as clomipramine and imipramine, are not considered effective for this anxiety disorder in particular. This leaves out SSRIs such as paroxetine, sertraline and fluvoxamine CR as acceptable and tolerated treatment options for this disorder.[24][25]
Obsessive–compulsive disorder
SSRIs are a second-line treatment of adult obsessive–compulsive disorder (OCD) with mild functional impairment and as first-line treatment for those with moderate or severe impairment. In children, SSRIs are considered as a second-line therapy in those with moderate-to-severe impairment, with close monitoring for psychiatric adverse effects.[26] SSRIs appear useful for OCD, at least in the short term.[27] Efficacy has been demonstrated both in short-term treatment trials of 6 to 24 weeks and in discontinuation trials of 28 to 52 weeks duration.[28][29][30] Clomipramine, a TCA drug, is considered effective and useful for OCD, however it is used as a second line treatment because it is less well tolerated than the SSRIs. Despite this, it has not shown superiority to fluvoxamine in trials. All SSRIs can be used effectively for OCD, and in some cases, SNRIs can also be tried even though none of them is approved specifically for OCD. However, even with all these treatment options, many people remain symptomatic after initiating the medication, and less than half of them do achieve remission.[31]
Post traumatic stress disorder
Antidepressants are one of the treatment options for PTSD, however their efficacy is not well established. Two antidepressants are FDA approved for it, paroxetine and sertraline, they belong to the serotonin reuptake inhibitors class. Paroxetine has slightly higher response and remission rates than sertraline for this condition, however both drugs are not considered very helpful for every person that takes them. Fluoxetine and venlafaxine are used off label, with fluoxetine producing unsatisfactory mixed results and venlafaxine, while having a response rates of 78%, which is significantly higher than what paroxetine and sertraline achieved, but it did not address all the symptoms of ptsd like the two drugs did, which is in part due to the fact the venlafaxine is an SNRI, this class of drugs inhibit the reuptake of norepinephrine too, this could cause some anxiety in some people. Fluvoxamine, escitalopram and citalopram were not well tested in this disorder. MAOIs, while some of them may be helpful, are not used much because of their unwanted side effects. This leaves paroxetine and sertraline as acceptable treatment options for some people, although more effective antidepressants are needed.[32]
Panic disorder
Panic disorder is relatively treated well with medications compared with other disorders, several classes of antidepressants have shown efficacy for this disorder, however SSRIs and SNRIs are used first-line. Paroxetine, sertraline, fluoxetine are FDA approved for panic disorder, although fluvoxamine, escitalopram and citalopram are considered effective for it. The SNRI venlafaxine is also approved for this condition. Unlike with social anxiety and PTSD, some TCAs antidepressants, like clomipramine and imipramine, have shown efficacy for panic disorder. Moreover, the MAOI phenelzine is considered useful too. Panic disorder has many drugs for its treatment, however, the starting dose must be lower than the one used for major depressive disorder because people, in the initiation of treatment, have reported an increase in anxiety as a result of starting the medication. In conclusion, while panic disorder's treatment options seem acceptable and useful for this condition, many people are still symptomatic after treatment with residual symptoms.[33][34][35]
Eating disorders
Antidepressants are recommended as an alternative or additional first step to self-help programs in the treatment of bulimia nervosa.[36] SSRIs (fluoxetine in particular) are preferred over other antidepressants due to their acceptability, tolerability, and superior reduction of symptoms in short-term trials. Long-term efficacy remains poorly characterized. Bupropion is not recommended for the treatment of eating disorders due to an increased risk of seizure.[37]
Similar recommendations apply to binge eating disorder.[36] SSRIs provide short-term reductions in binge eating behavior, but have not been associated with significant weight loss.[38]
Clinical trials have generated mostly negative results for the use of SSRIs in the treatment of anorexia nervosa.[39] Treatment guidelines from the National Institute of Health and Care Excellence[36] recommend against the use of SSRIs in this disorder. Those from the American Psychiatric Association note that SSRIs confer no advantage regarding weight gain, but that they may be used for the treatment of co-existing depressive, anxiety, or obsessive–compulsive disorders.[38]
Pain
Fibromyalgia
A 2012 meta-analysis concluded that antidepressants treatment favorably affects pain, health-related quality of life, depression, and sleep in fibromyalgia syndrome. Tricyclics appear to be the most effective class, with moderate effects on pain and sleep and small effects on fatigue and health-related quality of life. The fraction of people experiencing a 30% pain reduction on tricyclics was 48% versus 28% for placebo. For SSRIs and SNRIs the fraction of people experiencing a 30% pain reduction was 36% (20% in the placebo comparator arms) and 42% (32% in the corresponding placebo comparator arms). Discontinuation of treatment due to side effects was common.[40] Antidepressants including amitriptyline, fluoxetine, duloxetine, milnacipran, moclobemide, and pirlindole are recommended by the European League Against Rheumatism (EULAR) for the treatment of fibromyalgia based on "limited evidence".[41]
Neuropathic pain
A 2014 meta-analysis from the Cochrane Collaboration found the antidepressant duloxetine to be effective for the treatment of pain resulting from diabetic neuropathy.[42] The same group reviewed data for amitriptyline in the treatment of neuropathic pain and found limited useful randomized clinical trial data. They concluded that the long history of successful use in the community for the treatment of fibromyalgia and neuropathic pain justified its continued use.[43] The group was concerned about the potential for overestimating the amount of pain relief provided by amitriptyline, and highlighted that only a small number of people will experience significant pain relief by taking this medication.[43]
Other
Antidepressants may be modestly helpful for treating people who both have depression and alcohol dependence, however the evidence supporting this association is of low quality.[44] Buproprion is used to help people stop smoking. Antidepressants are also used to control some symptoms of narcolepsy.[45] Antidepressants may be used to relieve pain in people with active rheumatoid arthritis however, further research is required.[46] Antidepressants have been shown to be superior to placebo in treating depression in individuals with physical illness, although reporting bias may have exaggerated this finding.[47]
Limitations and strategies
Between 30% and 50% of individuals treated with a given antidepressant do not show a response.[48][49] Approximately one-third of people achieve a full remission, one-third experience a response and one-third are nonresponders. Partial remission is characterized by the presence of poorly defined residual symptoms. These symptoms typically include depressed mood, anxiety, sleep disturbance, fatigue and diminished interest or pleasure. It is currently unclear which factors predict partial remission. However, it is clear that residual symptoms are powerful predictors of relapse, with relapse rates 3–6 times higher in people with residual symptoms than in those who experience full remission.[50] In addition, antidepressant drugs tend to lose efficacy over the course of treatment.[51] According to data from the Centers for Disease Control and Prevention, less than one-third of Americans taking one antidepressant medication have seen a mental health professional in the previous year.[52] A number of strategies are used in clinical practice to try to overcome these limits and variations.[53] They include switching medication, augmentation, and combination.
Switching antidepressants
The American Psychiatric Association 2000 Practice Guideline advises that where no response is achieved following six to eight weeks of treatment with an antidepressant, to switch to an antidepressant in the same class, then to a different class of antidepressant. A 2006 meta-analysis review found wide variation in the findings of prior studies; for people who had failed to respond to an SSRI antidepressant, between 12% and 86% showed a response to a new drug. However, the more antidepressants an individual had already tried, the less likely they were to benefit from a new antidepressant trial.[49] However, a later meta-analysis found no difference between switching to a new drug and staying on the old medication; although 34% of treatment resistant people responded when switched to the new drug, 40% responded without being switched.[54]
Augmentation and combination
For a partial response, the American Psychiatric Association guidelines suggest augmentation, or adding a drug from a different class. These include lithium and thyroid augmentation, dopamine agonists, sex steroids, NRIs, glucocorticoid-specific agents, or the newer anticonvulsants.[55]
A combination strategy involves adding another antidepressant, usually from a different class so as to have effect on other mechanisms. Although this may be used in clinical practice, there is little evidence for the relative efficacy or adverse effects of this strategy.[56] Other tests conducted include the use of psychostimulants as an augmentation therapy. Several studies have shown the efficacy of combining modafinil for treatment-resistant people. It has been used to help combat SSRI-associated fatigue.[57]
Long-term use
The effects of antidepressants typically do not continue once the course of medication ends. This results in a high rate of relapse. A 2003 meta-analysis found that 18% of people who had responded to an antidepressant relapsed while still taking it, compared to 41% whose antidepressant was switched for a placebo.[58]
A gradual loss of therapeutic benefit occurs in a minority of people during the course of treatment.[59][60] A strategy involving the use of pharmacotherapy in the treatment of the acute episode, followed by psychotherapy in its residual phase, has been suggested by some studies.[61][62]
Adverse effects
Difficulty tolerating adverse effects is the most common reason for antidepressant discontinuation.[63]
Almost any medication involved with serotonin regulation has the potential to cause serotonin toxicity (also known as serotonin syndrome) — an excess of serotonin that can induce mania, restlessness, agitation, emotional lability, insomnia and confusion as its primary symptoms.[64][65] Although the condition is serious, it is not particularly common, generally only appearing at high doses or while on other medications. Assuming proper medical intervention has been taken (within about 24 hours) it is rarely fatal.[66][67] Antidepressants appear to increase the risk of diabetes by about 1.3 fold.[68]
MAOIs tend to have pronounced (sometimes fatal) interactions with a wide variety of medications and over-the-counter drugs. If taken with foods that contain very high levels of tyramine (e.g., mature cheese, cured meats, or yeast extracts), they may cause a potentially lethal hypertensive crisis. At lower doses, the person may only experience a headache due to an increase in blood pressure.[69]
In response to these adverse effects, a different type of MAOI has been developed: the reversible inhibitor of monoamine oxidase A (RIMA) class of drugs. Their primary advantage is that they do not require the person to follow a special diet, while being purportedly effective as SSRIs and tricyclics in treating depressive disorders.[70]
Tricyclics and SSRI can cause the so-called drug-induced QT prolongation, especially in older adults;[71] this condition can degenerate into a specific type of abnormal heart rhythm called torsades de points which can potentially lead to sudden cardiac arrest.[72]
Pregnancy
SSRI use in pregnancy has been associated with a variety of risks with varying degrees of proof of causation. As depression is independently associated with negative pregnancy outcomes, determining the extent to which observed associations between antidepressant use and specific adverse outcomes reflects a causative relationship has been difficult in some cases.[73] In other cases, the attribution of adverse outcomes to antidepressant exposure seems fairly clear.
SSRI use in pregnancy is associated with an increased risk of spontaneous abortion of about 1.7-fold,[74][75] and is associated with preterm birth and low birth weight.[76]
A systematic review of the risk of major birth defects in antidepressant-exposed pregnancies found a small increase (3% to 24%) in the risk of major malformations and a risk of cardiovascular birth defects that did not differ from non-exposed pregnancies.[77] A study of fluoxetine-exposed pregnancies found a 12% increase in the risk of major malformations that just missed statistical significance.[78] Other studies have found an increased risk of cardiovascular birth defects among depressed mothers not undergoing SSRI treatment, suggesting the possibility of ascertainment bias, e.g. that worried mothers may pursue more aggressive testing of their infants.[79] Another study found no increase in cardiovascular birth defects and a 27% increased risk of major malformations in SSRI exposed pregnancies.[75] The FDA advises for the risk of birth defects with the use of paroxetine[80] and the MAOI should be avoided.
A 2013 systematic review and meta-analysis found that antidepressant use during pregnancy was statistically significantly associated with some pregnancy outcomes, such as gestational age and preterm birth, but not with other outcomes. The same review cautioned that because differences between the exposed and unexposed groups were small, it was doubtful whether they were clinically significant.[81]
A neonate (infant less than 28 days old) may experience a withdrawal syndrome from abrupt discontinuation of the antidepressant at birth. Antidepressants have been shown to be present in varying amounts in breast milk, but their effects on infants are currently unknown.[82]
Moreover, SSRIs inhibit nitric oxide synthesis, which plays an important role in setting vascular tone. Several studies have pointed to an increased risk of prematurity associated with SSRI use, and this association may be due to an increase risk of pre-eclampsia of pregnancy.[83]
Antidepressant-induced mania
Another possible problem with antidepressants is the chance of antidepressant-induced mania or hypomania in people with or without a diagnosis of bipolar disorder. Many cases of bipolar depression are very similar to those of unipolar depression. Therefore, the person can be misdiagnosed with unipolar depression and be given antidepressants. Studies have shown that antidepressant-induced mania can occur in 20–40% of people with bipolar disorder.[84] For bipolar depression, antidepressants (most frequently SSRIs) can exacerbate or trigger symptoms of hypomania and mania.[85]
Suicide
Studies have shown that the use of antidepressants is correlated with an increased risk of suicidal behavior and thinking (suicidality) in those aged under 25.[86] This problem has been serious enough to warrant government intervention by the US Food and Drug Administration (FDA) to warn of the increased risk of suicidality during antidepressant treatment.[87] According to the FDA, the heightened risk of suicidality occurs within the first one to two months of treatment.[88][89] The National Institute for Health and Care Excellence (NICE) places the excess risk in the "early stages of treatment".[90] A meta-analysis suggests that the relationship between antidepressant use and suicidal behavior or thoughts is age-dependent.[86] Compared with placebo, the use of antidepressants is associated with an increase in suicidal behavior or thoughts among those 25 or younger (OR=1.62). There is no effect or possibly a mild protective effect among those aged 25 to 64 (OR=0.79). Antidepressant treatment has a protective effect against suicidality among those aged 65 and over (OR=0.37).[86][91]
Sexual
Sexual side effects are also common with SSRIs, such as loss of sexual drive, failure to reach orgasm, and erectile dysfunction.[92] Although usually reversible, these sexual side-effects can, in rare cases, continue after the drug has been completely withdrawn.[93][94]
In a study of 1022 outpatients, overall sexual dysfunction with all antidepressants averaged 59.1%[95] with SSRI values between 57% and 73%, mirtazapine 24%, nefazodone 8%, amineptine 7% and moclobemide 4%. Moclobemide, a selective reversible MAO-A inhibitor, does not cause sexual dysfunction,[96] and can actually lead to an improvement in all aspects of sexual function.[97]
Biochemical mechanisms suggested as causative include increased serotonin, particularly affecting 5-HT2 and 5-HT3 receptors; decreased dopamine; decreased norepinephrine; blockade of cholinergic and α1adrenergic receptors; inhibition of nitric oxide synthetase; and elevation of prolactin levels.[98] Mirtazapine is reported to have fewer sexual side effects, most likely because it antagonizes 5-HT2 and 5-HT3 receptors and may, in some cases, reverse sexual dysfunction induced by SSRIs by the same mechanism.[99]
Bupropion, a weak NDRI and nicotinic antagonist, may be useful in treating reduced libido as a result of SSRI treatment.[100]
Changes in weight
Changes in appetite or weight are common among antidepressants, but are largely drug-dependent and related to which neurotransmitters they affect. Mirtazapine and paroxetine, for example, may be associated with weight gain and/or increased appetite,[101][102][103] while others (such as bupropion and venlafaxine) achieve the opposite effect.[104][105]
The antihistaminic properties of certain TCA- and TeCA-class antidepressants have been shown to contribute to the common side effects of increased appetite and weight gain associated with these classes of medication.
Discontinuation syndrome
Antidepressant discontinuation syndrome, also called antidepressant withdrawal syndrome, is a condition that can occur following the interruption, reduction, or discontinuation of antidepressant medication.[106] The symptoms may include flu-like symptoms, trouble sleeping, nausea, poor balance, sensory changes, and anxiety.[106][12][107] The problem usually begins within three days and may last for several months.[106][107] Rarely psychosis may occur.[106]
A discontinuation syndrome can occur after stopping any antidepressant including selective serotonin re-uptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs).[106][12] The risk is greater among those who have taken the medication for longer and when the medication in question has a short half-life.[106] The underlying reason for its occurrence is unclear.[106] The diagnosis is based on the symptoms.[106]
Methods of prevention include gradually decreasing the dose among those who wish to stop, though it is possible for symptoms to occur with tapering.[106][11][107] Treatment may include restarting the medication and slowly decreasing the dose.[106] People may also be switched to the long acting antidepressant fluoxetine which can then be gradually decreased.[11]
Approximately 20–50% of people who suddenly stop an antidepressant develop an antidepressant discontinuation syndrome.[106][12][107] The condition is generally not serious.[106] Though about half of people with symptoms describe them as severe.[107] Some restart antidepressants due to the severity of the symptoms.[107]
Emotional blunting
SSRIs appear to cause emotional blunting, or numbness in some people who take them. This is a reduction in extremes of emotion, both positive and negative. While the person may feel less depressed, they may also feel less happiness or empathy. This may be cause for a dose reduction or medication change. The mechanism is unknown.[108][109]
Pharmacology
The earliest and probably most widely accepted scientific theory of antidepressant action is the monoamine hypothesis (which can be traced back to the 1950s), which states that depression is due to an imbalance (most often a deficiency) of the monoamine neurotransmitters (namely serotonin, norepinephrine and dopamine).[110] It was originally proposed based on the observation that certain hydrazine anti-tuberculosis agents produce antidepressant effects, which was later linked to their inhibitory effects on monoamine oxidase, the enzyme that catalyses the breakdown of the monoamine neurotransmitters.[110] All currently marketed antidepressants have the monoamine hypothesis as their theoretical basis, with the possible exception of agomelatine which acts on a dual melatonergic-serotonergic pathway.[110] Despite the success of the monoamine hypothesis it has a number of limitations: for one, all monoaminergic antidepressants have a delayed onset of action of at least a week; and secondly, there are a sizeable portion (>40%) of depressed patients that do not adequately respond to monoaminergic antidepressants.[111][112] A number of alternative hypotheses have been proposed, including the glutamate, neurogenic, epigenetic, cortisol hypersecretion and inflammatory hypotheses.[111][112][113][114]
Types
Selective serotonin reuptake inhibitors

Selective serotonin reuptake inhibitors (SSRIs) are believed to increase the extracellular level of the neurotransmitter serotonin by limiting its reabsorption into the presynaptic cell, increasing the level of serotonin in the synaptic cleft available to bind to the postsynaptic receptor. They have varying degrees of selectivity for the other monoamine transporters, with pure SSRIs having only weak affinity for the norepinephrine and dopamine transporters.
SSRIs are the most widely prescribed antidepressants in many countries.[115] The efficacy of SSRIs in mild or moderate cases of depression has been disputed.[116][117][118][119]
Serotonin–norepinephrine reuptake inhibitors
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are potent inhibitors of the reuptake of serotonin and norepinephrine. These neurotransmitters are known to play an important role in mood. SNRIs can be contrasted with the more widely used selective serotonin reuptake inhibitors (SSRIs), which act mostly upon serotonin alone.
The human serotonin transporter (SERT) and norepinephrine transporter (NET) are membrane proteins that are responsible for the reuptake of serotonin and norepinephrine. Balanced dual inhibition of monoamine reuptake can possibly offer advantages over other antidepressants drugs by treating a wider range of symptoms.[120]
SNRIs are sometimes also used to treat anxiety disorders, obsessive–compulsive disorder (OCD), attention deficit hyperactivity disorder (ADHD), chronic neuropathic pain, and fibromyalgia syndrome (FMS), and for the relief of menopausal symptoms.
Serotonin modulators and stimulators
Serotonin modulator and stimulators (SMSs), sometimes referred to more simply as "serotonin modulators", are a type of drug with a multimodal action specific to the serotonin neurotransmitter system. To be precise, SMSs simultaneously modulate one or more serotonin receptors and inhibit the reuptake of serotonin. The term was coined in reference to the mechanism of action of the serotonergic antidepressant vortioxetine, which acts as a serotonin reuptake inhibitor (SRI), partial agonist of the 5-HT1A receptor, and antagonist of the 5-HT3 and 5-HT7 receptors.[121][122][123] However, it can also technically be applied to vilazodone, which is an antidepressant as well and acts as an SRI and 5-HT1A receptor partial agonist.[124]
An alternative term is serotonin partial agonist/reuptake inhibitor (SPARI), which can be applied only to vilazodone.[125]
Serotonin antagonists and reuptake inhibitors
Serotonin antagonist and reuptake inhibitors (SARIs) while mainly used as antidepressants, are also anxiolytics and hypnotics. They act by antagonizing serotonin receptors such as 5-HT2A and inhibiting the reuptake of serotonin, norepinephrine, and/or dopamine. Additionally, most also act as α1-adrenergic receptor antagonists. The majority of the currently marketed SARIs belong to the phenylpiperazine class of compounds. They include trazodone and nefazodone.
Norepinephrine reuptake inhibitors
Norepinephrine reuptake inhibitors (NRIs or NERIs) are a type of drug that acts as a reuptake inhibitor for the neurotransmitter norepinephrine (noradrenaline) by blocking the action of the norepinephrine transporter (NET). This in turn leads to increased extracellular concentrations of norepinephrine.
NRIs are commonly used in the treatment of conditions like ADHD and narcolepsy due to their psychostimulant effects and in obesity due to their appetite suppressant effects. They are also frequently used as antidepressants for the treatment of major depressive disorder, anxiety and panic disorder. Additionally, many drugs of abuse such as cocaine and methylphenidate possess NRI activity, though it is important to mention that NRIs without combined dopamine reuptake inhibitor (DRI) properties are not significantly rewarding and hence are considered to have a negligible abuse potential.[126][127] However, norepinephrine has been implicated as acting synergistically with dopamine when actions on the two neurotransmitters are combined (e.g., in the case of NDRIs) to produce rewarding effects in psychostimulant drugs of abuse.[128]
Norepinephrine-dopamine reuptake inhibitors
The only drug used of this class for depression is bupropion.[100]
Tricyclic antidepressants
The majority of the tricyclic antidepressants (TCAs) act primarily as serotonin–norepinephrine reuptake inhibitors (SNRIs) by blocking the serotonin transporter (SERT) and the norepinephrine transporter (NET), respectively, which results in an elevation of the synaptic concentrations of these neurotransmitters, and therefore an enhancement of neurotransmission.[129][130] Notably, with the sole exception of amineptine, the TCAs have negligible affinity for the dopamine transporter (DAT), and therefore have no efficacy as dopamine reuptake inhibitors (DRIs).[129]
Although TCAs are sometimes prescribed for depressive disorders, they have been largely replaced in clinical use in most parts of the world by newer antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs) and norepinephrine reuptake inhibitors (NRIs). Adverse effects have been found to be of a similar level between TCAs and SSRIs.[131]
Tetracyclic antidepressants
Tetracyclic antidepressants (TeCAs) are a class of antidepressants that were first introduced in the 1970s. They are named after their chemical structure, which contains four rings of atoms, and are closely related to the tricyclic antidepressants (TCAs), which contain three rings of atoms.
Monoamine oxidase inhibitors
Monoamine oxidase inhibitors (MAOIs) are chemicals which inhibit the activity of the monoamine oxidase enzyme family. They have a long history of use as medications prescribed for the treatment of depression. They are particularly effective in treating atypical depression.[132] They are also used in the treatment of Parkinson's disease and several other disorders.
Because of potentially lethal dietary and drug interactions, monoamine oxidase inhibitors have historically been reserved as a last line of treatment, used only when other classes of antidepressant drugs (for example selective serotonin reuptake inhibitors and tricyclic antidepressants) have failed.
MAOIs have been found to be effective in the treatment of panic disorder with agoraphobia,[133] social phobia,[134][135][136] atypical depression[137][138] or mixed anxiety and depression, bulimia,[139][140][141][142] and post-traumatic stress disorder,[143] as well as borderline personality disorder.[144] MAOIs appear to be particularly effective in the management of bipolar depression according to a retrospective-analysis.[145] There are reports of MAOI efficacy in obsessive–compulsive disorder (OCD), trichotillomania, dysmorphophobia, and avoidant personality disorder, but these reports are from uncontrolled case reports.[146]
MAOIs can also be used in the treatment of Parkinson's disease by targeting MAO-B in particular (therefore affecting dopaminergic neurons), as well as providing an alternative for migraine prophylaxis. Inhibition of both MAO-A and MAO-B is used in the treatment of clinical depression and anxiety disorders.
NMDA receptor antagonists
NMDA receptor antagonists like ketamine and esketamine are rapid-acting antidepressants and seem to work via blockade of the ionotropic glutamate NMDA receptor.[147]
Others
See the list of antidepressants and management of depression for other drugs which are not specifically characterized.
Adjuncts
Adjunct medications are an umbrella category of substances that increase the potency or "enhance" antidepressants.[148] They work by affecting variables very close to the antidepressant, sometimes affecting a completely different mechanism of action. This may be attempted when depression treatments have not been successful in the past.
Common types of adjunct medication techniques generally fall into the following categories:
- Two or more antidepressants taken together
- From the same class (affecting the same area of the brain, often at a much higher level)
- From different classes (affecting multiple parts of the brain not covered simultaneously by either drug alone)
- An antipsychotic combined with an antidepressant, particularly atypical antipsychotics such as aripiprazole (Abilify), quetiapine (Seroquel), olanzapine (Zyprexa), and risperidone (Risperdal).[149]
It is unknown if undergoing psychological therapy at the same time as taking anti-depressants enhances the anti-depressive effect of the medication.[150]
Less common adjuncts
Lithium has been used to augment antidepressant therapy in those who have failed to respond to antidepressants alone.[151] Furthermore, lithium dramatically decreases the suicide risk in recurrent depression.[152] There is some evidence for the addition of a thyroid hormone, triiodothyronine, in patients with normal thyroid function.[153]
Psychopharmacologists have also tried adding a stimulant, in particular, d-amphetamine.[154] However, the use of stimulants in cases of treatment-resistant depression is relatively controversial.[155][156] A review article published in 2007 found psychostimulants may be effective in treatment-resistant depression with concomitant antidepressant therapy, but a more certain conclusion could not be drawn due to substantial deficiencies in the studies available for consideration, and the somewhat contradictory nature of their results.[156]
History
Before the 1950s, opioids and amphetamines were commonly used as antidepressants.[157][158] Their use was later restricted due to their addictive nature and side effects.[157] Extracts from the herb St John's wort have been used as a "nerve tonic" to alleviate depression.[159]
Isoniazid, iproniazid, and imipramine
In 1951, Irving Selikoff and Edward H. Robitzek, working out of Sea View Hospital on Staten Island, began clinical trials on two new anti-tuberculosis agents developed by Hoffman-LaRoche, isoniazid and iproniazid. Only patients with a poor prognosis were initially treated; nevertheless, their condition improved dramatically. Selikoff and Robitzek noted "a subtle general stimulation ... the patients exhibited renewed vigor and indeed this occasionally served to introduce disciplinary problems."[160] The promise of a cure for tuberculosis in the Sea View Hospital trials was excitedly discussed in the mainstream press.
In 1952, learning of the stimulating side effects of isoniazid, the Cincinnati psychiatrist Max Lurie tried it on his patients. In the following year, he and Harry Salzer reported that isoniazid improved depression in two-thirds of their patients and coined the term antidepressant to refer to its action.[161] A similar incident took place in Paris, where Jean Delay, head of psychiatry at Sainte-Anne Hospital, heard of this effect from his pulmonology colleagues at Cochin Hospital. In 1952 (before Lurie and Salzer), Delay, with the resident Jean-Francois Buisson, reported the positive effect of isoniazid on depressed patients.[162] The mode of antidepressant action of isoniazid is still unclear. It is speculated that its effect is due to the inhibition of diamine oxidase, coupled with a weak inhibition of monoamine oxidase A.[163]
Selikoff and Robitzek also experimented with another anti-tuberculosis drug, iproniazid; it showed a greater psychostimulant effect, but more pronounced toxicity.[164] Later, Jackson Smith, Gordon Kamman, George E. Crane, and Frank Ayd, described the psychiatric applications of iproniazid. Ernst Zeller found iproniazid to be a potent monoamine oxidase inhibitor.[165] Nevertheless, iproniazid remained relatively obscure until Nathan S. Kline, the influential head of research at Rockland State Hospital, began to popularize it in the medical and popular press as a "psychic energizer".[165][166] Roche put a significant marketing effort behind iproniazid.[165] Its sales grew until it was recalled in 1961, due to reports of lethal hepatotoxicity.[165]
The antidepressant effect of a tricyclic, a three ringed compound, was first discovered in 1957 by Roland Kuhn in a Swiss psychiatric hospital. Antihistamine derivatives were used to treat surgical shock and later as neuroleptics. Although in 1955 reserpine was shown to be more effective than placebo in alleviating anxious depression, neuroleptics were being developed as sedatives and antipsychotics.
Attempting to improve the effectiveness of chlorpromazine, Kuhn – in conjunction with the Geigy Pharmaceutical Company – discovered the compound "G 22355", later renamed imipramine. Imipramine had a beneficial effect in patients with depression who showed mental and motor retardation. Kuhn described his new compound as a "thymoleptic" "taking hold of the emotions," in contrast with neuroleptics, "taking hold of the nerves" in 1955–56. These gradually became established, resulting in the patent and manufacture in the US in 1951 by Häfliger and SchinderA.[167]
Second generation antidepressants
Antidepressants became prescription drugs in the 1950s. It was estimated that no more than 50 to 100 individuals per million suffered from the kind of depression that these new drugs would treat, and pharmaceutical companies were not enthusiastic in marketing for this small market. Sales through the 1960s remained poor compared to the sales of tranquilizers,[168] which were being marketed for different uses.[169] Imipramine remained in common use and numerous successors were introduced. The use of monoamine oxidase inhibitors (MAOI) increased after the development and introduction of "reversible" forms affecting only the MAO-A subtype of inhibitors, making this drug safer to use.[169][170]
By the 1960s, it was thought that the mode of action of tricyclics was to inhibit norepinephrine reuptake. However, norepinephrine reuptake became associated with stimulating effects. Later tricyclics were thought to affect serotonin as proposed in 1969 by Carlsson and Lindqvist as well as Lapin and Oxenkrug.
Researchers began a process of rational drug design to isolate antihistamine-derived compounds that would selectively target these systems. The first such compound to be patented was zimelidine in 1971, while the first released clinically was indalpine. Fluoxetine was approved for commercial use by the US Food and Drug Administration (FDA) in 1988, becoming the first blockbuster SSRI. Fluoxetine was developed at Eli Lilly and Company in the early 1970s by Bryan Molloy, Klaus Schmiegel, David T. Wong and others.[171][172] SSRIs became known as "novel antidepressants" along with other newer drugs such as SNRIs and NRIs with various selective effects.[173]
St John's wort fell out of favor in most countries through the 19th and 20th centuries, except in Germany, where Hypericum extracts were eventually licensed, packaged and prescribed. Small-scale efficacy trials were carried out in the 1970s and 1980s, and attention grew in the 1990s following a meta-analysis.[174] It remains an over-the-counter drug (OTC) supplement in most countries. Of concern are lead contaminant; on average, lead levels in women in the United States taking St. John's wort are elevated about 20%.[175] Research continues to investigate its active component hyperforin, and to further understand its mode of action.[176][177]
Rapid-acting antidepressants
Esketamine (brand name Spravato), the first rapid-acting antidepressant to be approved for clinical treatment of depression, was introduced for this indication in March 2019 in the United States.[147]
Research
A 2016 placebo randomized controlled trial evaluated the rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression with positive outcome.[178][179]
Society and culture
Prescription trends
In the United States, antidepressants were the most commonly prescribed medication in 2013.[180] Of the estimated 16 million "long term" (over 24 months) users, roughly 70 percent are female.[180] As of 2017, about 16.5% of white people in the United States took antidepressants compared with 5.6% of black people in the United States.[181]
In the UK, figures reported in 2010 indicated that the number of antidepressants prescribed by the National Health Service (NHS) almost doubled over a decade.[182] Further analysis published in 2014 showed that number of antidepressants dispensed annually in the community went up by 25 million in the 14 years between 1998 and 2012, rising from 15 million to 40 million. Nearly 50% of this rise occurred in the four years after the 2008 banking crash, during which time the annual increase in prescriptions rose from 6.7% to 8.5%.[183] These sources also suggest that aside from the recession, other factors that may influence changes in prescribing rates may include: improvements in diagnosis, a reduction of the stigma surrounding mental health, broader prescribing trends, GP characteristics, geographical location and housing status. Another factor that may contribute to increasing consumption of antidepressants is the fact that these medications now are used for other conditions including social anxiety and posttraumatic stress disorder.
United States: The most commonly prescribed antidepressants in the US retail market in 2010 were:[184]
| Drug name | Drug class | Total prescriptions |
|---|---|---|
| Sertraline | SSRI | 33,409,838 |
| Citalopram | SSRI | 27,993,635 |
| Fluoxetine | SSRI | 24,473,994 |
| Escitalopram | SSRI | 23,000,456 |
| Trazodone | SARI | 18,786,495 |
| Venlafaxine (all formulations) | SNRI | 16,110,606 |
| Bupropion (all formulations) | NDRI | 15,792,653 |
| Duloxetine | SNRI | 14,591,949 |
| Paroxetine | SSRI | 12,979,366 |
| Amitriptyline | TCA | 12,611,254 |
| Venlafaxine XR | SNRI | 7,603,949 |
| Bupropion XL | NDRI | 7,317,814 |
| Mirtazapine | TeCA | 6,308,288 |
| Venlafaxine ER | SNRI | 5,526,132 |
| Bupropion SR | NDRI | 4,588,996 |
| Desvenlafaxine | SNRI | 3,412,354 |
| Nortriptyline | TCA | 3,210,476 |
| Bupropion ER | NDRI | 3,132,327 |
| Venlafaxine | SNRI | 2,980,525 |
| Bupropion | NDRI | 753,516 |
Netherlands: In the Netherlands, paroxetine is the most prescribed antidepressant, followed by amitriptyline, citalopram and venlafaxine.[185]
Adherence
As of 2003, worldwide, 30 to 60% of people didn't follow their practitioner's instructions about taking their antidepressants,[186] and as of 2013 in the US, it appeared that around 50% of people did not take their antidepressants as directed by their practitioner.[187]
When people fail to take their antidepressants, there is a greater risk that the drug won't help, that symptoms get worse, that they miss work or are less productive at work, and that the person may be hospitalized.[188] This also increases costs for caring for them.[188]
Social science perspective
Some academics have highlighted the need to examine the use of antidepressants and other medical treatments in cross-cultural terms, due to the fact that various cultures prescribe and observe different manifestations, symptoms, meanings and associations of depression and other medical conditions within their populations.[189][190] These cross-cultural discrepancies, it has been argued, then have implications on the perceived efficacy and use of antidepressants and other strategies in the treatment of depression in these different cultures.[189][190] In India, antidepressants are largely seen as tools to combat marginality, promising the individual the ability to reintegrate into society through their use—a view and association not observed in the West.[189]
Environmental impacts
Because most antidepressants function by inhibiting the reuptake of neurotransmitters serotonin, dopamine, and norepinepherine[191] these drugs can interfere with natural neurotransmitter levels in other organisms impacted by indirect exposure.[192] Antidepressants fluoxetine and sertraline have been detected in aquatic organisms residing in effluent dominated streams.[193] The presence of antidepressants in surface waters and aquatic organisms has caused concern because ecotoxicological effects to aquatic organisms due to fluoxetine exposure have been demonstrated.[194]
Coral reef fish have been demonstrated to modulate aggressive behavior through serotonin.[195] Artificially increasing serotonin levels in crustaceans can temporarily reverse social status and turn subordinates into aggressive and territorial dominant males.[196]
Exposure to fluoxetine has been demonstrated to increase serotonergic activity in fish, subsequently reducing aggressive behavior.[197] Perinatal exposure to fluoxetine at relevant environmental concentrations has been shown to lead to significant modifications of memory processing in 1-month-old cuttlefish.[198] This impairment may disadvantage cuttlefish and decrease their survival. Somewhat less than 10% of orally administered fluoxetine is excreted from humans unchanged or as glucuronide.[199][200]
See also
| Wikimedia Commons has media related to Antidepressants. |
- Management of depression
- Antidepressants in Japan
- Atypical antidepressant
- Depression and natural therapies
- Listening to Prozac by Peter Kramer
- Anatomy of an Epidemic by Robert Whittaker
- List of investigational antidepressants
References
- Jennings, Leigh (2018). "Chapter 4: Antidepressants". In Grossberg, George T.; Kinsella, Laurence J. (eds.). Clinical psychopharmacology for neurologists: a practical guide. Springer. pp. 45–71. doi:10.1007/978-3-319-74604-3_4. ISBN 978-3-319-74602-9.
- Healy D, Noury LJ, Manginb D (May 2018). "Enduring sexual dysfunction after treatment with antidepressants, 5α-reductase inhibitors and isotretinoin: 300 cases". International Journal of Risk & Safety in Medicine. 29 (3): 125–134. doi:10.3233/JRS-180744. PMC 6004900. PMID 29733030.
- Bahrick AS (2008). "Persistence of Sexual Dysfunction Side Effects after Discontinuation of Antidepressant Medications: Emerging Evidence". The Open Psychology Journal. 1: 42–50. doi:10.2174/1874350100801010042.
- Taylor MJ, Rudkin L, Bullemor-Day P, Lubin J, Chukwujekwu C, Hawton K (May 2013). "Strategies for managing sexual dysfunction induced by antidepressant medication". The Cochrane Database of Systematic Reviews. 5 (5): CD003382. doi:10.1002/14651858.CD003382.pub3. PMID 23728643.
- Kennedy SH, Rizvi S (April 2009). "Sexual dysfunction, depression, and the impact of antidepressants". Journal of Clinical Psychopharmacology. 29 (2): 157–64. doi:10.1097/jcp.0b013e31819c76e9. PMID 19512977.
- Serotonin and noradrenaline reuptake inhibitors (SNRI); selective serotonin reuptake inhibitors (SSRI) – Persistent sexual dysfunction after drug withdrawal (EPITT no 19277), 11 June 20191, EMA/PRAC/265221/2019, Pharmacovigilance Risk Assessment Committee (PRAC)
- Sansone, Randy A.; Sansone, Lori A. (October 2010). "SSRI-Induced Indifference". Psychiatry. 7 (10): 14–18. PMC 2989833. PMID 21103140.
- https://www.health.harvard.edu/depression/is-your-antidepressant-making-life-a-little-too-blah
- https://www.hcplive.com/view/half-of-patients-on-antidepressants-experience-emotional-blunting
- "Revisions to Product Labeling" (PDF). FDA. Retrieved 10 November 2018.
- Wilson, E; Lader, M (December 2015). "A review of the management of antidepressant discontinuation symptoms". Therapeutic Advances in Psychopharmacology. 5 (6): 357–68. doi:10.1177/2045125315612334. PMC 4722507. PMID 26834969.
- Gabriel, M; Sharma, V (29 May 2017). "Antidepressant discontinuation syndrome". Canadian Medical Association Journal. 189 (21): E747. doi:10.1503/cmaj.160991. PMC 5449237. PMID 28554948.
- Barth, Michael; Kriston, Levente; Klostermann, Swaantje; Barbui, Corrado; Cipriani, Andrea; Linde, Klaus (2 January 2018). "Efficacy of selective serotonin reuptake inhibitors and adverse events: Meta-regression and mediation analysis of placebo-controlled trials". British Journal of Psychiatry. 208 (2): 114–119. doi:10.1192/bjp.bp.114.150136. PMID 26834168.
- Jakobsen, JC; Gluud, C; Kirsch, I (25 September 2019). "Should antidepressants be used for major depressive disorder?". BMJ Evidence-based Medicine: bmjebm–2019–111238. doi:10.1136/bmjebm-2019-111238. PMID 31554608.
- Cipriani, Andrea; Zhou, Xinyu; Del Giovane, Cinzia; Hetrick, Sarah E; Qin, Bin; Whittington, Craig; Coghill, David; Zhang, Yuqing; Hazell, Philip; Leucht, Stefan; Cuijpers, Pim; Pu, Juncai; Cohen, David; Ravindran, Arun V; Liu, Yiyun; Michael, Kurt D; Yang, Lining; Liu, Lanxiang; Xie, Peng (August 2016). "Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis". The Lancet. 388 (10047): 881–890. doi:10.1016/S0140-6736(16)30385-3. PMID 27289172.
When considering the risk-benefit profile of antidepressants in the acute treatment of major depressive disorder, these drugs do not seem to offer a clear advantage for children and adolescents.
- Kirsch, Irving (January 2014). "Antidepressants and the Placebo Effect". Zeitschrift für Psychologie. 222 (3): 128–134. doi:10.1027/2151-2604/a000176. PMC 4172306. PMID 25279271.
- Turner, Erick H; Rosenthal, Robert (8 March 2008). "Efficacy of antidepressants". BMJ. 336 (7643): 516–517. doi:10.1136/bmj.39510.531597.80. PMC 2265347. PMID 18319297.
- Depression: The Treatment and Management of Depression in Adults (Updated Edition). British Psychological Society. 2010. ISBN 978-1-904671-85-5.
- Cipriani, Andrea; Furukawa, Toshi A; Salanti, Georgia; Chaimani, Anna; Atkinson, Lauren Z; Ogawa, Yusuke; Leucht, Stefan; Ruhe, Henricus G; Turner, Erick H; Higgins, Julian P T; Egger, Matthias; Takeshima, Nozomi; Hayasaka, Yu; Imai, Hissei; Shinohara, Kiyomi; Tajika, Aran; Ioannidis, John P A; Geddes, John R (April 2018). "Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis". The Lancet. 391 (10128): 1357–1366. doi:10.1016/S0140-6736(17)32802-7. PMC 5889788. PMID 29477251.
- Nutt, David J. (30 April 2008). "Relationship of Neurotransmitters to the Symptoms of Major Depressive Disorder". The Journal of Clinical Psychiatry. 69 (suppl E1): 4–7. PMID 18494537.
- "Depression in adults: The treatment and management of depression in adults". NICE guidelines [CG90]. National Institute for Health and Care Excellence (UK). October 2009. Archived from the original on 23 September 2015. Retrieved 23 September 2015.
- "Practice Guideline for the Treatment of Patients With Major Depressive Disorder" (PDF). PsychiatryOnline (Third ed.).
- "www.nice.org.uk" (PDF). Archived from the original (PDF) on 21 October 2012. Retrieved 20 February 2013.
- Glue, Paul; Scott, KM; Glue, P (May 2012). "Optimal treatment of social phobia: systematic review and meta-analysis". Neuropsychiatric Disease and Treatment: 203. doi:10.2147/NDT.S23317. PMC 3363138. PMID 22665997.
- Hansen, Richard A.; Gaynes, Bradley N.; Gartlehner, Gerald; Moore, Charity G.; Tiwari, Ruchi; Lohr, Kathleen N. (May 2008). "Efficacy and tolerability of second-generation antidepressants in social anxiety disorder". International Clinical Psychopharmacology. 23 (3): 170–179. doi:10.1097/YIC.0b013e3282f4224a. PMC 2657552. PMID 18408531.
- "www.nice.org.uk" (PDF). Archived from the original (PDF) on 6 December 2008.
- Soomro, GM; Altman, D; Rajagopal, S; Oakley-Browne, M (23 January 2008). "Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD)". The Cochrane Database of Systematic Reviews (1): CD001765. doi:10.1002/14651858.CD001765.pub3. PMC 7025764. PMID 18253995.
- Fineberg, N. A.; Brown, A; Reghunandanan, S; Pampaloni, I (2012). "Evidence-based pharmacotherapy of obsessive-compulsive disorder". The International Journal of Neuropsychopharmacology. 15 (8): 1173–91. doi:10.1017/S1461145711001829. hdl:2299/216. PMID 22226028.
- "Paroxetine prescribing information" (PDF). Archived from the original (PDF) on 19 February 2015. Retrieved 30 January 2015.
- "Sertraline prescribing information" (PDF). Archived (PDF) from the original on 16 June 2015. Retrieved 30 January 2015.
- Kellner, Michael (June 2010). "Drug treatment of obsessive-compulsive disorder". Dialogues in Clinical Neuroscience. 12 (2): 187–197. PMC 3181958. PMID 20623923.
- Alexander, Walter (January 2012). "Pharmacotherapy for Post-traumatic Stress Disorder in Combat Veterans". Pharmacy and Therapeutics. 37 (1): 32–38. PMC 3278188. PMID 22346334.
- Bighelli, Irene; Castellazzi, Mariasole; Cipriani, Andrea; Girlanda, Francesca; Guaiana, Giuseppe; Koesters, Markus; Turrini, Giulia; Furukawa, Toshi A; Barbui, Corrado (5 April 2018). "Antidepressants versus placebo for panic disorder in adults". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD010676.pub2. PMC 6494573. PMID 29620793.
- Bighelli, Irene; Trespidi, Carlotta; Castellazzi, Mariasole; Cipriani, Andrea; Furukawa, Toshi A; Girlanda, Francesca; Guaiana, Giuseppe; Koesters, Markus; Barbui, Corrado (12 September 2016). "Antidepressants and benzodiazepines for panic disorder in adults". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD011567.pub2. PMC 6457579. PMID 27618521.
- Andrisano, Costanza; Chiesa, Alberto; Serretti, Alessandro (January 2013). "Newer antidepressants and panic disorder". International Clinical Psychopharmacology. 28 (1): 33–45. doi:10.1097/YIC.0b013e32835a5d2e. PMID 23111544.
- "www.nice.org.uk" (PDF). Archived (PDF) from the original on 27 March 2014.
- "Bupropion: MedlinePlus Drug Information". Archived from the original on 8 May 2016. Retrieved 24 May 2016.
- "National Guideline Clearinghouse | Practice guideline for the treatment of patients with eating disorders". 5 July 2018. Archived from the original on 25 May 2013.
- Flament MF, Bissada H, Spettigue W (March 2012). "Evidence-based pharmacotherapy of eating disorders". Int. J. Neuropsychopharmacol. 15 (2): 189–207. doi:10.1017/S1461145711000381. PMID 21414249.
- Häuser W, Wolfe F, Tölle T, Uçeyler N, Sommer C (April 2012). "The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis". CNS Drugs. 26 (4): 297–307. doi:10.2165/11598970-000000000-00000. PMID 22452526. S2CID 207301478.
- "www.enfa-europe.eu" (PDF). Archived from the original (PDF) on 23 May 2014.
- Lunn MP, Hughes RA, Wiffen PJ (2014). "Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia". Cochrane Database Syst Rev. 1 (1): CD007115. doi:10.1002/14651858.CD007115.pub3. PMID 24385423.
- Moore, R. Andrew; Derry, Sheena; Aldington, Dominic; Cole, Peter; Wiffen, Philip J. (6 July 2015). "Amitriptyline for neuropathic pain in adults". The Cochrane Database of Systematic Reviews (7): CD008242. doi:10.1002/14651858.CD008242.pub3. PMC 6447238. PMID 26146793.
- Agabio, Roberta; Trogu, Emanuela; Pani, Pier Paolo (24 April 2018). "Antidepressants for the treatment of people with co-occurring depression and alcohol dependence". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD008581.pub2. PMC 6494437. PMID 29688573.
- "Narcolepsy Information Page". National Institute of Neurological Disorders and Stroke. 27 March 2019. Retrieved 11 April 2020.
- Richards, Bethan L; Whittle, Samuel L; Buchbinder, Rachelle (9 November 2011). "Antidepressants for pain management in rheumatoid arthritis". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD008920.pub2. PMID 22071859.
- Rayner, Lauren; Price, Annabel; Evans, Alison; Valsraj, Koravangattu; Higginson, Irene J; Hotopf, Matthew (17 March 2010). "Antidepressants for depression in physically ill people". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD007503.pub2. PMID 20238354.
- Baghai TC, Möller HJ, Rupprecht R (2006). "Recent Progress in Pharmacological and Non-Pharmacological Treatment Options of Major Depression". Current Pharmaceutical Design. 12 (4): 503–15. doi:10.2174/138161206775474422. PMID 16472142.
- Ruhé HG, Huyser J, Swinkels JA, Schene AH (2006). "Switching Antidepressants After a First Selective Serotonin Reuptake Inhibitor in Major Depressive Disorder" (PDF). The Journal of Clinical Psychiatry. 67 (12): 1836–55. doi:10.4088/JCP.v67n1203. PMID 17194261. S2CID 9758110.
- Tranter R, O'Donovan C, Chandarana P, Kennedy S (2002). "Prevalence and outcome of partial remission in depression". Journal of Psychiatry & Neuroscience. 27 (4): 241–7. PMC 161658. PMID 12174733.
- Byrne SE, Rothschild AJ (1998). "Loss of Antidepressant Efficacy During Maintenance Therapy". The Journal of Clinical Psychiatry. 59 (6): 279–88. doi:10.4088/JCP.v59n0602. PMID 9671339.
- "Antidepressant Use in Persons Aged 12 and Over: United States, 2005–2008". cdc.gov. Products – Data Briefs – Number 76 – October 2011. Centers for Disease Control and Prevention. Archived from the original on 4 February 2016. Retrieved 4 February 2016.
- Mischoulon D, Nierenberg AA, Kizilbash L, Rosenbaum JF, Fava M (2000). "Strategies for managing depression refractory to selective serotonin reuptake inhibitor treatment: A survey of clinicians". Canadian Journal of Psychiatry. 45 (5): 476–81. doi:10.1177/070674370004500509. PMID 10900529.
- Bschor T, Baethge C (2010). "No evidence for switching the antidepressant: Systematic review and meta-analysis of RCTs of a common therapeutic strategy". Acta Psychiatrica Scandinavica. 121 (3): 174–9. doi:10.1111/j.1600-0447.2009.01458.x. PMID 19703121.
- DeBattista C, Lembke A (2005). "Update on augmentation of antidepressant response in resistant depression". Current Psychiatry Reports. 7 (6): 435–40. doi:10.1007/s11920-005-0064-x. PMID 16318821. S2CID 25499899.
- Lam RW, Wan DD, Cohen NL, Kennedy SH (2002). "Combining Antidepressants for Treatment-Resistant Depression". The Journal of Clinical Psychiatry. 63 (8): 685–93. doi:10.4088/JCP.v63n0805. PMID 12197448.
- Goss AJ, Kaser M, Costafreda SG, Sahakian BJ, Fu CH (2013). "Modafinil augmentation therapy in unipolar and bipolar depression: a systematic review and meta-analysis of randomized controlled trials" (PDF). The Journal of Clinical Psychiatry. 74 (11): 1101–7. doi:10.4088/JCP.13r08560. PMID 24330897. S2CID 13911763.
- Geddes JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, Frank E, Goodwin GM (2003). "Relapse prevention with antidepressant drug treatment in depressive disorders: A systematic review". The Lancet. 361 (9358): 653–61. doi:10.1016/S0140-6736(03)12599-8. PMID 12606176. S2CID 20198748.
- Targum SD (March 2014). "Identification and treatment of antidepressant tachyphylaxis". Innov Clin Neurosci. 11 (3–4): 24–8. PMC 4008298. PMID 24800130.
- Fava GA, Offidani E (2011). "The mechanisms of tolerance in antidepressant action". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 35 (7): 1593–602. doi:10.1016/j.pnpbp.2010.07.026. PMID 20728491. S2CID 207409469.
- Fava GA, Park SK, Sonino N (2006). "Treatment of recurrent depression". Expert Review of Neurotherapeutics. 6 (11): 1735–40. doi:10.1586/14737175.6.11.1735. PMID 17144786. S2CID 22808803.
- Petersen TJ (2006). "Enhancing the efficacy of antidepressants with psychotherapy". Journal of Psychopharmacology. 20 (3 suppl): 19–28. doi:10.1177/1359786806064314. PMID 16644768. S2CID 23649861.
- Allen, Arthur. "Coping With Side Effects of Depression Treatment". WebMD. Retrieved 4 February 2019.
- Birmes P, Coppin D, Schmitt L, Lauque D (2003). "Serotonin syndrome: a brief review". CMAJ. 168 (11): 1439–42. PMC 155963. PMID 12771076.
- Boyer EW, Shannon M (2005). "The serotonin syndrome" (PDF). N. Engl. J. Med. 352 (11): 1112–20. doi:10.1056/NEJMra041867. PMID 15784664. Archived from the original (PDF) on 18 June 2013.
- Mason PJ, Morris VA, Balcezak TJ (2000). "Serotonin syndrome. Presentation of 2 cases and review of the literature". Medicine. 79 (4): 201–9. doi:10.1097/00005792-200007000-00001. PMID 10941349.
- Sampson E, Warner JP (1999). "Serotonin syndrome: potentially fatal but difficult to recognize". Br J Gen Pract. 49 (448): 867–8. PMC 1313553. PMID 10818648.
- Salvi, Virginio; Grua, Ilaria; Cerveri, Giancarlo; Mencacci, Claudio; Barone-Adesi, Francesco; Meyre, David (31 July 2017). "The risk of new-onset diabetes in antidepressant users – A systematic review and meta-analysis". PLOS ONE. 12 (7): e0182088. Bibcode:2017PLoSO..1282088S. doi:10.1371/journal.pone.0182088. PMC 5536271. PMID 28759599.
In our meta-analysis we found an association between exposure to ADs and new-onset diabetes, with a relative risk of 1.27. When we restricted the analysis to the studies to high NOS score the association between ADs and diabetes was even stronger. The results are in line with those from two previous meta-analyses that reported a 1.5-fold increase of diabetes among AD users.
- Sathyanarayana Rao TS, Yeragani VK (2009). "Hypertensive crisis and cheese". Indian J Psychiatry. 51 (1): 65–6. doi:10.4103/0019-5545.44910. PMC 2738414. PMID 19742203.
- Paykel ES (1995). "Clinical efficacy of reversible and selective inhibitors of monoamine oxidase A in major depression". Acta Psychiatr Scand Suppl. 386: 22–7. doi:10.1111/j.1600-0447.1995.tb05920.x. PMID 7717091.
- Rochester, Matthew P.; Kane, Allison M.; Linnebur, Sunny Anne; Fixen, Danielle R. (4 May 2018). "Evaluating the risk of QTc prolongation associated with antidepressant use in older adults: a review of the evidence". Therapeutic Advances in Drug Safety. 9 (6): 297–308. doi:10.1177/2042098618772979. PMC 5971403. PMID 29854391.
- Ayad, Ramy F.; Assar, Manish D.; Simpson, Leo; Garner, John B.; Schussler, Jeffrey M. (11 December 2017). "Causes and Management of Drug-Induced Long Qt Syndrome". Baylor University Medical Center Proceedings. 23 (3): 250–255. doi:10.1080/08998280.2010.11928628. PMC 2900977. PMID 20671821.
- Malm H (December 2012). "Prenatal exposure to selective serotonin reuptake inhibitors and infant outcome". Ther Drug Monit. 34 (6): 607–14. doi:10.1097/FTD.0b013e31826d07ea. PMID 23042258.
- Rahimi R, Nikfar S, Abdollahi M (2006). "Pregnancy outcomes following exposure to serotonin reuptake inhibitors: a meta-analysis of clinical trials". Reproductive Toxicology. 22 (4): 571–575. doi:10.1016/j.reprotox.2006.03.019. PMID 16720091.
- Nikfar S, Rahimi R, Hendoiee N, Abdollahi M (2012). "Increasing the risk of spontaneous abortion and major malformations in newborns following use of serotonin reuptake inhibitors during pregnancy: A systematic review and updated meta-analysis". Daru. 20 (1): 75. doi:10.1186/2008-2231-20-75. PMC 3556001. PMID 23351929.
- Huang H, Coleman S, Bridge JA, Yonkers K, Katon W (2014). "A meta-analysis of the relationship between antidepressant use in pregnancy and the risk of preterm birth and low birth weight". General Hospital Psychiatry. 36 (1): 13–8. doi:10.1016/j.genhosppsych.2013.08.002. PMC 3877723. PMID 24094568.
- Einarson TR, Kennedy D, Einarson A (2012). "Do findings differ across research design? The case of antidepressant use in pregnancy and malformations". J Popul Ther Clin Pharmacol. 19 (2): e334–48. PMID 22946124.
- Riggin L, Frankel Z, Moretti M, Pupco A, Koren G (April 2013). "The fetal safety of fluoxetine: a systematic review and meta-analysis". J Obstet Gynaecol Can. 35 (4): 362–9. doi:10.1016/S1701-2163(15)30965-8. PMID 23660045.
- Koren G, Nordeng HM (February 2013). "Selective serotonin reuptake inhibitors and malformations: case closed?". Semin Fetal Neonatal Med. 18 (1): 19–22. doi:10.1016/j.siny.2012.10.004. PMID 23228547.
- "FDA Advising of Risk of Birth Defects with Paxil" (Press release). U.S. Food and Drug Administration. Archived from the original on 3 December 2013. Retrieved 29 November 2012.
- Ross, Lori E.; Grigoriadis, Sophie; Mamisashvili, Lana; VonderPorten, Emily H.; Roerecke, Michael; Rehm, Jürgen; Dennis, Cindy-Lee; Koren, Gideon; Steiner, Meir; Mousmanis, Patricia; Cheung, Amy (1 April 2013). "Selected Pregnancy and Delivery Outcomes After Exposure to Antidepressant Medication". JAMA Psychiatry. 70 (4): 436–43. doi:10.1001/jamapsychiatry.2013.684. PMID 23446732.
- Lanza di Scalea T, Wisner KL (2009). "Antidepressant Medication Use During Breastfeeding". Clinical Obstetrics and Gynecology. 52 (3): 483–97. doi:10.1097/GRF.0b013e3181b52bd6. PMC 2902256. PMID 19661763.
- Sivagnanam, G (2012). "Antidepressants". Journal of Pharmacology and Pharmacotherapeutics. 3 (3): 287–288. ProQuest 1033762996.
- Goldberg JF, Truman CJ (2003). "Antidepressant-induced mania: An overview of current controversies". Bipolar Disorders. 5 (6): 407–20. doi:10.1046/j.1399-5618.2003.00067.x. PMID 14636364.
- Benazzi F (1997). "Antidepressant-associated hypomania in outpatient depression: a 203-case study in private practice". J Affect Disord. 46 (1): 73–7. doi:10.1016/S0165-0327(97)00082-7. PMID 9387089.
- Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, Hammad TA, Temple R, Rochester G (2009). "Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration". BMJ. 339: b2880. doi:10.1136/bmj.b2880. PMC 2725270. PMID 19671933.
- Friedman RA, Leon AC (2007). "Expanding the black box – depression, antidepressants, and the risk of suicide". N. Engl. J. Med. 356 (23): 2343–6. doi:10.1056/NEJMp078015. PMID 17485726.
- "Antidepressant Use in Children, Adolescents, and Adults". Archived from the original on 19 December 2016.
- "FDA Medication Guide for Antidepressants". Archived from the original on 18 August 2014. Retrieved 5 June 2014.
- "www.nice.org.uk" (PDF). Archived (PDF) from the original on 18 October 2012.
- Healy D, Aldred G (2005). "Antidepressant drug use and the risk of suicide" (PDF). International Review of Psychiatry. 17 (3): 163–172. doi:10.1080/09540260500071624. PMID 16194787. Archived from the original (PDF) on 21 October 2013.
- Grant JE, Potenza MN, eds. (2012). The Oxford handbook of impulse control disorders. Oxford: Oxford University Press. ISBN 978-0-19-538971-5.
- Csoka AB, Csoka A, Bahrick A, Mehtonen OP (2008). "Persistent sexual dysfunction after discontinuation of selective serotonin reuptake inhibitors". J Sex Med. 5 (1): 227–33. doi:10.1111/j.1743-6109.2007.00630.x. PMID 18173768. S2CID 15471717.
- Healy, David; Le Noury, Joanna; Mangin, Derelie (4 June 2018). "Enduring sexual dysfunction after treatment with antidepressants, 5α-reductase inhibitors and isotretinoin: 300 cases". International Journal of Risk & Safety in Medicine. 29 (3–4): 125–134. doi:10.3233/JRS-180744. PMC 6004900. PMID 29733030.
- Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F (2001). "Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction". J Clin Psychiatry. 62 Suppl 3: 10–21. PMID 11229449.
- Serretti A, Chiesa A (2009). "Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis". J Clin Psychopharmacol. 29 (3): 259–66. doi:10.1097/JCP.0b013e3181a5233f. PMID 19440080. S2CID 1663570.
- Chebili S, Abaoub A, Mezouane B, Le Goff JF (1998). "[Antidepressants and sexual stimulation: the correlation]". Encephale (in French). 24 (3): 180–4. PMID 9696909.
- Keltner NL, McAfee KM, Taylor CL (2009). "Biological Perspectives". Perspectives in Psychiatric Care. 38 (3): 111–6. doi:10.1111/j.1744-6163.2002.tb00665.x. PMID 12385082.
- Ozmenler NK, Karlidere T, Bozkurt A, Yetkin S, Doruk A, Sutcigil L, Cansever A, Uzun O, Ozgen F, Ozsahin A (2008). "Mirtazapine augmentation in depressed patients with sexual dysfunction due to selective serotonin reuptake inhibitors". Hum Psychopharmacol. 23 (4): 321–6. doi:10.1002/hup.929. PMID 18278806. S2CID 39616771.
- Schwasinger-Schmidt, TE; Macaluso, M (8 September 2018). "Other Antidepressants". Handbook of Experimental Pharmacology. 250: 325–355. doi:10.1007/164_2018_167. ISBN 978-3-030-10948-6. PMID 30194544.
- Stimmel GL, Dopheide JA, Stahl SM (1997). "Mirtazapine: An antidepressant with noradrenergic and specific serotonergic effects". Pharmacotherapy. 17 (1): 10–21. doi:10.1002/j.1875-9114.1997.tb03674.x (inactive 27 May 2020). PMID 9017762.
- "mirtazapine (Rx) – Remeron, Remeron SolTab". Medscape. WebMD. Archived from the original on 29 October 2013. Retrieved 19 November 2013.
- Papakostas GI (2008). "Tolerability of modern antidepressants". J Clin Psychiatry. 69 (Suppl E1): 8–13. PMID 18494538.
- Li Z, Maglione M, Tu W, Mojica W, Arterburn D, Shugarman LR, Hilton L, Suttorp M, Solomon V, Shekelle PG, Morton SC (April 2005). "Meta-analysis: pharmacologic treatment of obesity". Ann. Intern. Med. 142 (7): 532–46. doi:10.7326/0003-4819-142-7-200504050-00012. PMID 15809465.
- "Effexor Medicines Data Sheet". Wyeth Pharmaceuticals Inc. 2006. Archived from the original on 17 September 2006. Retrieved 17 September 2006.
- Warner, CH; Bobo, W; Warner, C; Reid, S; Rachal, J (1 August 2006). "Antidepressant discontinuation syndrome". American Family Physician. 74 (3): 449–56. PMID 16913164.
- Davies, J; Read, J (2019). "A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: Are guidelines evidence-based?". Addictive Behaviors. 97: 111–121. doi:10.1016/j.addbeh.2018.08.027. PMID 30292574.
- Fornaro, M; Anastasia, A; Novello, S; Fusco, A; Pariano, R; De Berardis, D; Solmi, M; Veronese, N; Stubbs, B; Vieta, E; Berk, M; de Bartolomeis, A; Carvalho, AF (2019). "The emergence of loss of efficacy during antidepressant drug treatment for major depressive disorder: An integrative review of evidence, mechanisms, and clinical implications". Pharmacological Research. 139: 494–502. doi:10.1016/j.phrs.2018.10.025. PMID 30385364.
- Pringle, A; McCabe, C; Cowen, PJ; Harmer, CJ (August 2013). "Antidepressant treatment and emotional processing: can we dissociate the roles of serotonin and noradrenaline?". Journal of Psychopharmacology (Oxford, England). 27 (8): 719–31. doi:10.1177/0269881112474523. PMID 23392757. S2CID 38884409.
- Brunton LL, Chabner B, Knollmann BC, eds. (2011). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill Professional. ISBN 978-0-07-162442-8.
- Maes M, Yirmyia R, Noraberg J, Brene S, Hibbeln J, Perini G, Kubera M, Bob P, Lerer B, Maj M (March 2009). "The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression". Metabolic Brain Disease. 24 (1): 27–53. doi:10.1007/s11011-008-9118-1. PMID 19085093. S2CID 4564675.
- Sanacora G, Treccani G, Popoli M (January 2012). "Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders". Neuropharmacology. 62 (1): 63–77. doi:10.1016/j.neuropharm.2011.07.036. PMC 3205453. PMID 21827775.
- Menke A, Klengel T, Binder EB (2012). "Epigenetics, depression and antidepressant treatment". Current Pharmaceutical Design. 18 (36): 5879–5889. doi:10.2174/138161212803523590. PMID 22681167.
- Vialou V, Feng J, Robison AJ, Nestler EJ (January 2013). "Epigenetic mechanisms of depression and antidepressant action". Annual Review of Pharmacology and Toxicology. 53 (1): 59–87. doi:10.1146/annurev-pharmtox-010611-134540. PMC 3711377. PMID 23020296.
- Preskorn SH, Ross R, Stanga CY (2004). "Selective Serotonin Reuptake Inhibitors". In Sheldon H. Preskorn, Hohn P. Feighner, Christina Y. Stanga, Ruth Ross (eds.). Antidepressants: Past, Present and Future. Berlin: Springer. pp. 241–62. ISBN 978-3-540-43054-4.
- Fournier, JC; DeRubeis, RJ; Hollon, SD; Dimidjian, S; Amsterdam, JD; Shelton, RC; Fawcett, J (6 January 2010). "Antidepressant drug effects and depression severity: a patient-level meta-analysis". JAMA. 303 (1): 47–53. doi:10.1001/jama.2009.1943. PMC 3712503. PMID 20051569.
- Kramer, Peter (7 September 2011). "In Defense of Antidepressants". The New York Times. Archived from the original on 12 July 2011. Retrieved 13 July 2011.
- Pies R (April 2010). "Antidepressants Work, Sort of-Our System of Care Does Not". Journal of Clinical Psychopharmacology. 30 (2): 101–104. doi:10.1097/JCP.0b013e3181d52dea. PMID 20520282.
- Pies, Ronald W. (2016). "Antidepressants". Journal of Clinical Psychopharmacology. 36 (1): 1–4. doi:10.1097/jcp.0000000000000455. PMID 26658086.
- Cashman, JR; Ghirmai, S (2009). "Inhibition of serotonin and norepinephrine reuptake and inhibition of phosphodiesterase by multi-target inhibitors as potential agents for depression". Bioorganic & Medicinal Chemistry. 17 (19): 6890–7. doi:10.1016/j.bmc.2009.08.025. PMID 19740668.
- Goldenberg MM (November 2013). "Pharmaceutical approval update". P T. 38 (11): 705–7. PMC 3875258. PMID 24391391.
- American Pharmacists Association (2013). "Vortioxetine: Atypical antidepressant". Archived from the original on 20 November 2015.
- Los Angeles Times (2013). "FDA approves a new antidepressant: Brintellix". Archived from the original on 20 November 2015.
- Hughes ZA, Starr KR, Langmead CJ, et al. (March 2005). "Neurochemical evaluation of the novel 5-HT1A receptor partial agonist/serotonin reuptake inhibitor, vilazodone". European Journal of Pharmacology. 510 (1–2): 49–57. doi:10.1016/j.ejphar.2005.01.018. PMID 15740724.
- Muntner, Stephen M. Stahl; with illustrations by Nancy (2013). Stahl's essential psychopharmacology : neuroscientific basis and practical application (4th ed.). Cambridge: Cambridge University Press. ISBN 978-1107686465.
- Wee S, Woolverton WL (September 2004). "Evaluation of the reinforcing effects of atomoxetine in monkeys: comparison to methylphenidate and desipramine". Drug and Alcohol Dependence. 75 (3): 271–6. doi:10.1016/j.drugalcdep.2004.03.010. PMID 15283948.
- Gasior M, Bergman J, Kallman MJ, Paronis CA (April 2005). "Evaluation of the reinforcing effects of monoamine reuptake inhibitors under a concurrent schedule of food and i.v. drug delivery in rhesus monkeys". Neuropsychopharmacology. 30 (4): 758–64. doi:10.1038/sj.npp.1300593. PMID 15526000.
- Rothman RB, Baumann MH, Dersch CM, et al. (January 2001). "Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin". Synapse. 39 (1): 32–41. doi:10.1002/1098-2396(20010101)39:1<32::AID-SYN5>3.0.CO;2-3. PMID 11071707. S2CID 15573624.
- Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur J Pharmacol. 340 (2–3): 249–258. doi:10.1016/S0014-2999(97)01393-9. PMID 9537821.
- Gillman PK (July 2007). "Tricyclic antidepressant pharmacology and therapeutic drug interactions updated". British Journal of Pharmacology. 151 (6): 737–48. doi:10.1038/sj.bjp.0707253. PMC 2014120. PMID 17471183.
- Trindade, E.; Menon, D.; Topfer, L. A.; Coloma, C. (17 November 1998). "Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis". Canadian Medical Association Journal. 159 (10): 1245–1252. PMC 1229819. PMID 9861221.
- Cristancho, Mario (20 November 2012). "Atypical Depression in the 21st Century: Diagnostic and Treatment Issues". Psychiatric Times. Archived from the original on 2 December 2013. Retrieved 23 November 2013.
- Buigues, J; Vallejo, J (1987). "Therapeutic response to phenelzine in patients with panic disorder and agoraphobia with panic attacks". Journal of Clinical Psychiatry. 48 (2): 55–9. PMID 3542985.
- Liebowitz, MR; Schneier, FR; Campeas, R; Hollander, E; Hatterer, J; Fyer, A; et al. (1992). "Phenelzine vs atenolol in social phobia: A placebo-controlled comparison". Archives of General Psychiatry. 49 (4): 290–300. doi:10.1001/archpsyc.49.4.290. PMID 1558463.
- Versiani M, Nardi AE, Mundim FD, Alves AB, Liebowitz MR, Amrein R. Pharmacotherapy of social phobia. A controlled study with moclobemide and phenelzine. BJP [Internet]. 1992 Sep 1 [cited 2013 Oct 4];161(3):353–60. Available from: Versiani, M.; Nardi, A. E.; Mundim, F. D.; Alves, A. B.; Liebowitz, M. R.; Amrein, R. (1992). "Pharmacotherapy of Social Phobia". British Journal of Psychiatry. 161 (3): 353–360. doi:10.1192/bjp.161.3.353. PMID 1393304.
- Heimberg, RG; Liebowitz, MR; Hope, DA; et al. (1998). "Cognitive behavioral group therapy vs phenelzine therapy for social phobia: 12-week outcome". Arch Gen Psychiatry. 55 (12): 1133–41. doi:10.1001/archpsyc.55.12.1133. PMID 9862558.
- Jarrett, RB; Schaffer, M; McIntire, D; Witt-Browder, A; Kraft, D; Risser, RC (1999). "Treatment of atypical depression with cognitive therapy or phenelzine: A double-blind, placebo-controlled trial". Arch Gen Psychiatry. 56 (5): 431–7. doi:10.1001/archpsyc.56.5.431. PMC 1475805. PMID 10232298.
- Liebowitz, MR; Quitkin, FM; Stewart, JW; et al. (1984). "Phenelzine v imipramine in atypical depression: A preliminary report". Arch Gen Psychiatry. 41 (7): 669–77. doi:10.1001/archpsyc.1984.01790180039005. PMID 6375621.
- Walsh, B; Stewart, JW; Roose, SP; Gladis, M; Glassman, AH (1984). "Treatment of bulimia with phenelzine: A double-blind, placebo-controlled study". Arch Gen Psychiatry. 41 (11): 1105–9. doi:10.1001/archpsyc.1983.01790220095015. PMID 6388524.
- Rothschild R, Quitkin HM, Quitkin FM, Stewart JW, Ocepek-Welikson K, McGrath PJ, et al. (1994). "A double-blind placebo-controlled comparison of phenelzine and imipramine in the treatment of bulimia in atypical depressives". International Journal of Eating Disorders. 15 (1): 1–9. doi:10.1002/1098-108X(199401)15:1<1::AID-EAT2260150102>3.0.CO;2-E. PMID 8124322.
- Walsh, BT; Stewart, JW; Roose, SP; Gladis, M; Glassman, AH (1985). "A double-blind trial of phenelzine in bulimia". Journal of Psychiatric Research. 19 (2–3): 485–9. doi:10.1016/0022-3956(85)90058-5. PMID 3900362.
- Walsh, B; Gladis, M; Roose, SP; Stewart, JW; Stetner, F; Glassman, AH (May 1988). "Phenelzine vs placebo in 50 patients with bulimia". Arch Gen Psychiatry. 45 (5): 471–5. doi:10.1001/archpsyc.1988.01800290091011. PMID 3282482.
- Davidson, J; Ingram, J; Kilts, C (1987). "A pilot study of phenelzine in the treatment of post-traumatic stress disorder". The British Journal of Psychiatry. 150 (2): 252–5. doi:10.1192/bjp.150.2.252. PMID 3651684.
- Soloff, PH; Cornelius, J; George, A; Nathan, S; Perel, JM; Ulrich, RF (1993). "Efficacy of phenelzine and haloperidol in borderline personality disorder". Arch Gen Psychiatry. 50 (5): 377–85. doi:10.1001/archpsyc.1993.01820170055007. PMID 8489326.
- Mallinger, AG; Frank, E; Thase, ME; Barwell, MM; DiazGranados, N; Luckenbaugh, DA; et al. (2009). "Revisiting the Effectiveness of Standard Antidepressants in Bipolar Disorder: Are Monoamine Oxidase Inhibitors Superior?". Psychopharmacol Bull. 42 (2): 64–74. PMC 3570273. PMID 19629023.
- Liebowitz, MR; Hollander, E; Schneier, F; Campeas, R; Welkowitz, L; Hatterer, J; Fallon, B (1990). "Reversible and irreversible monoamine oxidase inhibitors in other psychiatric disorders". Acta Psychiatr Scand Suppl. 360: 29–34. doi:10.1111/j.1600-0447.1990.tb05321.x. PMID 2248064.
- "SPRAVATO™ (esketamine) nasal spray FDA label" (PDF). Food and Drug Administration. 5 March 2019. Retrieved 6 March 2019.
- "Depressive Disorders". Merck Manual. Archived from the original on 5 December 2013. Retrieved 30 November 2012.
- Taylor D, Carol P, Shitij K (2012). The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. ISBN 978-0-470-97969-3.
- Cox, Georgina R; Callahan, Patch; Churchill, Rachel; Hunot, Vivien; Merry, Sally N; Parker, Alexandra G; Hetrick, Sarah E (30 November 2014). "Psychological therapies versus antidepressant medication, alone and in combination for depression in children and adolescents" (PDF). Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD008324.pub3. PMID 25433518.
- Bauer M, Dopfmer S (1999). "Lithium augmentation in treatment-resistant depression: Meta-analysis of placebo-controlled studies". Journal of Clinical Psychopharmacology. 19 (5): 427–34. doi:10.1097/00004714-199910000-00006. PMID 10505584. S2CID 31979046.CS1 maint: ref=harv (link)
- Guzzetta F, Tondo L, Centorrino F, Baldessarini RJ (March 2007). "Lithium treatment reduces suicide risk in recurrent major depressive disorder". J Clin Psychiatry. 68 (3): 380–83. doi:10.4088/JCP.v68n0304. PMID 17388706. S2CID 10343453.CS1 maint: ref=harv (link)
- Nierenberg AA, Fava M, Trivedi MH, Wisniewski SR, Thase ME, McGrath PJ, Alpert JE, Warden D, Luther JF, Niederehe G, Lebowitz B, Shores-Wilson K, Rush AJ (2006). "A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: A STAR*D report". American Journal of Psychiatry. 163 (9): 1519–30. doi:10.1176/appi.ajp.163.9.1519. PMID 16946176.CS1 maint: ref=harv (link)
- Stahl, Stephen M. (2011). The Prescriber's Guide (Stahl's Essential Psychopharmacology). Cambridge University Press. p. 39.
- Kraus MF, Burch EA (1992). "Methylphenidate hydrochloride as an antidepressant: controversy, case studies, and review". South. Med. J. 85 (10): 985–91. doi:10.1097/00007611-199210000-00012. PMID 1411740.
- Orr, K; Taylor, D (2007). "Psychostimulants in the treatment of depression : a review of the evidence". CNS Drugs. 21 (3): 239–57. doi:10.2165/00023210-200721030-00004. PMID 17338594. S2CID 35761979.
- Weber MM, Emrich HM (1988). "Current and Historical Concepts of Opiate Treatment in Psychiatric Disorders". International Clinical Psychopharmacology. 3 (3): 255–66. doi:10.1097/00004850-198807000-00007. PMID 3153713.
- Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present – a pharmacological and clinical perspective". J. Psychopharmacol. 27 (6): 479–96. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
- Czygan FC (2003). "Kulturgeschichte und Mystik des Johanniskrauts: Vom 2500 Jahre alten Apotropaikum zum aktuellen Antidepressivum" [From a 2500-year-old apotropic comes a current antidepressive. The cultural history and mistique of St. John's wort]. Pharmazie in Unserer Zeit (in German). 32 (3): 184–90. doi:10.1002/pauz.200390062. PMID 12784538.
- Selikoff IJ, Robitzek EH (1952). "Tuberculosis Chemotherapy with Hydrazine Derivatives of Isonicotinic Acid". Chest. 21 (4): 385–438. doi:10.1378/chest.21.4.385. PMID 14906149.
- Healy D (2001). "The Antidepressant Drama". In Weissman M (ed.). The treatment of depression: bridging the 21st century. American Psychiatric Pub. pp. 10–11. ISBN 978-0-88048-397-1.
- Healy D (1996). The psychopharmacologists: interviews. London: Chapman and Hall. p. 8. ISBN 978-1-86036-008-4.
- Healy D (1998). The Psychopharmacologists: Volume 2. A Hodder Arnold Publication. pp. 132–4. ISBN 978-1-86036-010-7.
- Robitzek EH, Selikoff IJ, Mamlok E, Tendlau A (1953). "Isoniazid and Its Isopropyl Derivative in the Therapy of Tuberculosis in Humans: Comparative Therapeutic and Toxicologic Properties". Chest. 23 (1): 1–15. doi:10.1378/chest.23.1.1. PMID 12998444.
- López-Muñoz F, Alamo C, Juckel G, Assion HJ (2007). "Half a Century of Antidepressant Drugs". Journal of Clinical Psychopharmacology. 27 (6): 555–9. doi:10.1097/jcp.0b013e3181bb617. PMID 18004120.
- "Psychic Energizer". Time. 15 April 1957. Archived from the original on 11 August 2013. Retrieved 28 May 2009.
- Kuhn R (1958). "The treatment of depressive states with G 22355 (imipramine hydrochloride)". The American Journal of Psychiatry. 115 (5): 459–64. doi:10.1176/ajp.115.5.459. PMID 13583250.
- "Tranquilizers". Cumberland Mountain Community Services. cmcsb.com. Archived from the original on 16 September 2012. Retrieved 20 November 2013.
- Healy D (1999). "The Three Faces of the Antidepressants: A Critical Commentary on the Clinical-Economic Context of Diagnosis". The Journal of Nervous & Mental Disease. 187 (3): 174–80. doi:10.1097/00005053-199903000-00007. PMID 10086474.
- Pletscher A (1991). "The discovery of antidepressants: A winding path". Experientia. 47 (1): 4–8. doi:10.1007/BF02041242. PMID 1999242. S2CID 112210.
- Domino EF (1999). "History of modern psychopharmacology: A personal view with an emphasis on antidepressants". Psychosomatic Medicine. 61 (5): 591–8. doi:10.1097/00006842-199909000-00002. PMID 10511010.
- Wong DT, Bymaster FP, Horng JS, Molloy BB (1975). "A new selective inhibitor for uptake of serotonin into synaptosomes of rat brain: 3-(p-trifluoromethylphenoxy). N-methyl-3-phenylpropylamine". The Journal of Pharmacology and Experimental Therapeutics. 193 (3): 804–11. PMID 1151730.
- Freeman, H (1996). "Tolerability and safety of novel antidepressants". European Psychiatry. 11: 206s. doi:10.1016/0924-9338(96)88597-X.
- Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D (1996). "St John's wort for depression—an overview and meta-analysis of randomised clinical trials". BMJ. 313 (7052): 253–8. doi:10.1136/bmj.313.7052.253. PMC 2351679. PMID 8704532.
- Buettner, C; Mukamal, KJ; Gardiner, P; Davis, RB; Phillips, RS; Mittleman, MA (November 2009). "Herbal supplement use and blood lead levels of United States adults". Journal of General Internal Medicine. 24 (11): 1175–82. doi:10.1007/s11606-009-1050-5. PMC 2771230. PMID 19575271.
- Müller WE (2003). "Current St. John's wort research from mode of action to clinical efficacy". Pharmacological Research. 47 (2): 101–9. doi:10.1016/S1043-6618(02)00266-9. PMID 12543057.
- Nathan PJ (2001). "Hypericum perforatum (St John's Wort): A non-selective reuptake inhibitor? A review of the recent advances in its pharmacology". Journal of Psychopharmacology. 15 (1): 47–54. doi:10.1177/026988110101500109. PMID 11277608. S2CID 36924335.
- Palhano-Fontes, F; Barreto, D; Onias, H; Andrade, KC; Novaes, MM; Pessoa, JA; Mota-Rolim, SA; Osório, FL; Sanches, R; Dos Santos, RG; Tófoli, LF; de Oliveira Silveira, G; Yonamine, M; Riba, J; Santos, FR; Silva-Junior, AA; Alchieri, JC; Galvão-Coelho, NL; Lobão-Soares, B; Hallak, JEC; Arcoverde, E; Maia-de-Oliveira, JP; Araújo, DB (March 2019). "Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial". Psychological medicine. 49 (4): 655–663. doi:10.1017/S0033291718001356. PMID 29903051.
- "Antidepressant Effects of Ayahuasca: a Randomized Placebo Controlled Trial in Treatment Resistant Depression - Full Text View - ClinicalTrials.gov". clinicaltrials.gov.
- White, Rebecca. "Waking up from sadness: Many find trouble getting off antidepressants". Al Jazeera. Archived from the original on 14 July 2014. Retrieved 8 June 2014.
- "By the numbers: Antidepressant use on the rise". apa.org. Retrieved 1 February 2019.
- Davis, Rowenna (11 June 2010). "Antidepressant Use Rises as Recession Feeds Wave of Worry". The Guardian. London. Archived from the original on 15 June 2010. Retrieved 1 July 2010.
- Spence, Ruth. "Focus on: Antidepressant prescribing". QualityWatch. QualityWatch (Nuffield Trust/Health Foundation). Archived from the original on 4 February 2015. Retrieved 12 January 2015.
- "Top 200 generic drugs by units in 2010" (PDF). Archived from the original (PDF) on 15 December 2012."Top 200 brand drugs by units in 2010" (PDF). Archived from the original (PDF) on 22 April 2012.
- "GIPdatabank". Gipdatabank.nl. Archived from the original on 6 December 2008. Retrieved 6 November 2008.
- "Adherence to Long Term Therapies: Evidence for Action" (PDF). World Health Organization. 2003.
- Kaplan, Jessica E.; Keeley, Robert D.; Engel, Matthew; Emsermann, Caroline; Brody, David (July 2013). "Aspects of patient and clinician language predict adherence to antidepressant medication". Journal of the American Board of Family Medicine. 26 (4): 409–420. doi:10.3122/jabfm.2013.04.120201. PMID 23833156.
- Ho, SC; Chong, HY; Chaiyakunapruk, N; Tangiisuran, B; Jacob, SA (15 March 2016). "Clinical and economic impact of non-adherence to antidepressants in major depressive disorder: A systematic review". Journal of Affective Disorders. 193: 1–10. doi:10.1016/j.jad.2015.12.029. PMID 26748881.
- Ecks S (2005). "Pharmaceutical Citizenship: Antidepressant Marketing and the Promise of Demarginalization in India". Anthropology & Medicine. 12 (3): 239–254. doi:10.1080/13648470500291360. PMID 26873669. S2CID 23046695.
- Lock M, Nguyen VK (2010). ""Local Biologies and Human Difference". An anthropology of biomedicine (1st ed.). Chichester, West Sussex: Wiley-Blackwell. pp. 83–109. ISBN 978-1-4051-1071-6.
- Zhou Z, Zhen J, Karpowich NK, Goetz RM, Law CJ, Reith ME, Wang DN (2007). "LeuT-desipramine structure reveals how antidepressants block neurotransmitter reuptake". Science. 317 (5843): 1390–3. Bibcode:2007Sci...317.1390Z. doi:10.1126/science.1147614. PMC 3711652. PMID 17690258.
- Fong PP (2001). "Antidepressants in Aquatic Organisms: A Wide Range of Effects". In Daughton CG, Jones-Lepp TJ (eds.). Pharmaceuticals and personal care products in the environment: scientific and regulatory issues. Washington, DC: American Chemical Society. pp. 264–281. ISBN 978-0-8412-3739-1.
- Brooks BW, Chambliss CK, Stanley JK, Ramirez A, Banks KE, Johnson RD, Lewis RJ (2005). "Determination of select antidepressants in fish from an effluent-dominated stream". Environ. Toxicol. Chem. 24 (2): 464–9. doi:10.1897/04-081r.1. PMID 15720009.
- Fent K, Weston AA, Caminada D (2006). "Ecotoxicology of human pharmaceuticals". Aquat. Toxicol. 76 (2): 122–59. doi:10.1016/j.aquatox.2005.09.009. PMID 16257063.
- Winberg S, Carter CG, McCarthy JD, He XY, Nilsson GE, Houlihan DF (1993). "Feeding rank and brain serotonergic activity in rainbow trout Onchorhynchus my kiss". J. Exp. Biol. 179: 197–211.
- Huber R, Smith K, Delago A, Isaksson K, Kravitz EA (1997). "Serotonin and aggressive motivation in crustaceans: altering the decision to retreat". Proc. Natl. Acad. Sci. U.S.A. 94 (11): 5939–42. Bibcode:1997PNAS...94.5939H. doi:10.1073/pnas.94.11.5939. PMC 20885. PMID 9159179.
- Perreault HA, Semsar K, Godwin J (2003). "Fluoxetine treatment decreases territorial aggression in a coral reef fish". Physiol. Behav. 79 (4–5): 719–24. doi:10.1016/S0031-9384(03)00211-7. PMID 12954414. S2CID 39464936.
- Di Poi C, Darmaillacq AS, Dickel L, Boulouard M, Bellanger C (2013). "Effects of perinatal exposure to waterborne fluoxetine on memory processing in the cuttlefish Sepia officinalis". Aquat. Toxicol. 132–133: 84–91. doi:10.1016/j.aquatox.2013.02.004. PMID 23474317.
- "Pharmacokinetics of selective serotonin reuptake inhibitors" (PDF). Archived from the original (PDF) on 23 May 2014.
- Nentwig G (2007). "Effects of pharmaceuticals on aquatic invertebrates. Part II: the antidepressant drug fluoxetine". Arch. Environ. Contam. Toxicol. 52 (2): 163–70. doi:10.1007/s00244-005-7190-7. PMID 17160491. S2CID 22309647.
Further reading
- Stahl SM (1997). Psychopharmacology of Antidepressants. Informa Healthcare. ISBN 978-1-85317-513-8.
External links
| Look up antidepressant in Wiktionary, the free dictionary. |

