Abscess
An abscess is a collection of pus that has built up within the tissue of the body.[1] Signs and symptoms of abscesses include redness, pain, warmth, and swelling.[1] The swelling may feel fluid-filled when pressed.[1] The area of redness often extends beyond the swelling.[6] Carbuncles and boils are types of abscess that often involve hair follicles, with carbuncles being larger.[7]
| Abscess | |
|---|---|
| Other names | Latin: Abscessus |
 | |
| Five-day-old inflamed epidermal inclusion cyst. The black spot is a keratin plug which connects with the underlying cyst. | |
| Specialty | General surgery, Infectious disease, dermatology |
| Symptoms | Redness, pain, swelling[1] |
| Usual onset | Rapid |
| Causes | Bacterial infection (often MRSA)[1] |
| Risk factors | Intravenous drug use[2] |
| Diagnostic method | Ultrasound, CT scan[1][3] |
| Differential diagnosis | Cellulitis, sebaceous cyst, necrotising fasciitis[3] |
| Treatment | Incision and drainage[4] |
| Frequency | ~1% per year (United States)[5] |
They are usually caused by a bacterial infection.[8] Often many different types of bacteria are involved in a single infection.[6] In the United States and many other areas of the world the most common bacteria present is methicillin-resistant Staphylococcus aureus.[1] Rarely, parasites can cause abscesses; this is more common in the developing world.[3] Diagnosis of a skin abscess is usually made based on what it looks like and is confirmed by cutting it open.[1] Ultrasound imaging may be useful in cases in which the diagnosis is not clear.[1] In abscesses around the anus, computer tomography (CT) may be important to look for deeper infection.[3]
Standard treatment for most skin or soft tissue abscesses is cutting it open and drainage.[4] There appears to be some benefit from also using antibiotics.[9] A small amount of evidence supports not packing the cavity that remains with gauze after drainage.[1] Closing this cavity right after draining it rather than leaving it open may speed healing without increasing the risk of the abscess returning.[10] Sucking out the pus with a needle is often not sufficient.[1]
Skin abscesses are common and have become more common in recent years.[1] Risk factors include intravenous drug use, with rates reported as high as 65% among users.[2] In 2005 in the United States, 3.2 million people went to the emergency department for an abscess.[5] In Australia, around 13,000 people were hospitalized in 2008 with the condition.[11]
Signs and symptoms

Abscesses may occur in any kind of tissue but most frequently within the skin surface (where they may be superficial pustules known as boils or deep skin abscesses), in the lungs, brain, teeth, kidneys, and tonsils. Major complications may include spreading of the abscess material to adjacent or remote tissues, and extensive regional tissue death (gangrene).
The main symptoms and signs of a skin abscess are redness, heat, swelling, pain, and loss of function. There may also be high temperature (fever) and chills.[12] If superficial, abscesses may be fluctuant when palpated; this wave-like motion is caused by movement of the pus inside the abscess.[13]
An internal abscess is more difficult to identify, but signs include pain in the affected area, a high temperature, and generally feeling unwell. Internal abscesses rarely heal themselves, so prompt medical attention is indicated if such an abscess is suspected. An abscess can potentially be fatal depending on where it is located.[14][15]
Causes
Risk factors for abscess formation include intravenous drug use.[16] Another possible risk factor is a prior history of disc herniation or other spinal abnormality,[17] though this has not been proven.
Abscesses are caused by bacterial infection, parasites, or foreign substances. Bacterial infection is the most common cause.[8] Often many different types of bacteria are involved in a single infection.[6] In the United States and many other areas of the world the most common bacteria present is methicillin-resistant Staphylococcus aureus.[1] Among spinal subdural abscesses, methicillin-sensitive Staphylococcus aureus is the most common organism involved.[17]
Rarely parasites can cause abscesses and this is more common in the developing world.[3] Specific parasites known to do this include dracunculiasis and myiasis.[3]
Perianal abscess
Surgery of the anal fistula to drain an abscess treats the fistula and reduces likelihood of its recurrence and the need for repeated surgery.[18] There is no evidence that fecal incontinence is a consequence of this surgery for abscess drainage.[18]
Perianal abscesses can be seen in patients with, for example, inflammatory bowel disease (such as Crohn's disease) or diabetes. Often the abscess will start as an internal wound caused by ulceration, hard stool, or penetrative objects with insufficient lubrication. This wound typically becomes infected as a result of the normal presence of feces in the rectal area, and then develops into an abscess. This often presents itself as a lump of tissue near the anus which grows larger and more painful with time. Like other abscesses, perianal abscesses may require prompt medical treatment, such as an incision and debridement or lancing.
Incisional abscess
An incisional abscess is one that develops as a complication secondary to a surgical incision. It presents as redness and warmth at the margins of the incision with purulent drainage from it.[19] If the diagnosis is uncertain, the wound should be aspirated with a needle, with aspiration of pus confirming the diagnosis and availing for Gram stain and bacterial culture.[19]
Pathophysiology
An abscess is a defensive reaction of the tissue to prevent the spread of infectious materials to other parts of the body.
The organisms or foreign materials kill the local cells, resulting in the release of cytokines. The cytokines trigger an inflammatory response, which draws large numbers of white blood cells to the area and increases the regional blood flow.
The final structure of the abscess is an abscess wall, or capsule, that is formed by the adjacent healthy cells in an attempt to keep the pus from infecting neighboring structures. However, such encapsulation tends to prevent immune cells from attacking bacteria in the pus, or from reaching the causative organism or foreign object.
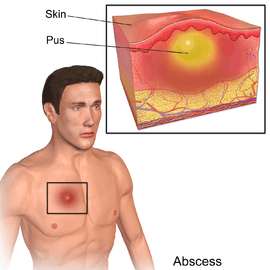 A diagram of an abscess.
A diagram of an abscess.
Diagnosis
An abscess is a localized collection of pus (purulent inflammatory tissue) caused by suppuration buried in a tissue, an organ, or a confined space, lined by the pyogenic membrane.[21] Ultrasound imaging in the emergency department can help in a diagnosis.[22]
Classification
Abscesses may be classified as either skin abscesses or internal abscesses. Skin abscesses are common; internal abscesses tend to be harder to diagnose, and more serious.[12] Skin abscesses are also called cutaneous or subcutaneous abscesses.[23]
IV drug use
For those with a history of intravenous drug use, an X-ray is recommended before treatment to verify that no needle fragments are present.[16] In this population if there is also a fever present, infectious endocarditis should be considered.[16]
Differential
Abscesses should be differentiated from empyemas, which are accumulations of pus in a preexisting, rather than a newly formed, anatomical cavity.
Other conditions that can cause similar symptoms include: cellulitis, a sebaceous cyst, and necrotising fasciitis.[3] Cellulitis typically also has an erythematous reaction, but does not confer any purulent drainage.[19]
Treatment
The standard treatment for an uncomplicated skin or soft tissue abscess is the act of opening and draining.[4] There does not appear to be any benefit from also using antibiotics in most cases.[1] A small amount of evidence did not find a benefit from packing the abscess with gauze.[1]
Incision and drainage


The abscess should be inspected to identify if foreign objects are a cause, which may require their removal. If foreign objects are not the cause, incising and draining the abscess is standard treatment.[4][24]
In critical areas where surgery presents a high risk, it may be delayed or used as a last resort. The drainage of a lung abscess may be performed by positioning the patient in a way that enables the contents to be discharged via the respiratory tract. Warm compresses and elevation of the limb may be beneficial for a skin abscess.
Antibiotics
Most people who have an uncomplicated skin abscess should not use antibiotics.[4] Antibiotics in addition to standard incision and drainage is recommended in persons with severe abscesses, many sites of infection, rapid disease progression, the presence of cellulitis, symptoms indicating bacterial illness throughout the body, or a health condition causing immunosuppression.[1] People who are very young or very old may also need antibiotics.[1] If the abscess does not heal only with incision and drainage, or if the abscess is in a place that is difficult to drain such as the face, hands, or genitals, then antibiotics may be indicated.[1]
In those cases of abscess which do require antibiotic treatment, Staphylococcus aureus bacteria is a common cause and an anti-staphylococcus antibiotic such as flucloxacillin or dicloxacillin is used. The Infectious Diseases Society of America advises that the draining of an abscess is not enough to address community-acquired methicillin-resistant Staphylococcus aureus (MRSA), and in those cases, traditional antibiotics may be ineffective.[1] Alternative antibiotics effective against community-acquired MRSA often include clindamycin, doxycycline, minocycline, and trimethoprim-sulfamethoxazole.[1] The American College of Emergency Physicians advises that typical cases of abscess from MRSA get no benefit from having antibiotic treatment in addition to the standard treatment.[4] If the condition is thought to be cellulitis rather than an abscess, consideration should be given to the possibility of the strep species as a cause, that are still sensitive to traditional anti-staphylococcus agents such as dicloxacillin or cephalexin. This would be in the case of patients that are able to tolerate penicillin. Antibiotic therapy alone without surgical drainage of the abscess is seldom effective due to antibiotics often being unable to get into the abscess and their ineffectiveness at low pH levels.
Culturing the wound is not needed if standard follow-up care can be provided after the incision and drainage.[4] Performing a wound culture is unnecessary because it rarely gives information which can be used to guide treatment.[4]
Packing
In North America, after drainage, an abscess cavity is often packed, perhaps with cloth, in an attempt to protect the healing wound. However, evidence from emergency medicine literature reports that packing wounds after draining causes pain to the person and does not decrease the rate of recurrence, nor bring faster healing, or fewer physician visits.[25]
Loop drainage
More recently, several North American hospitals have opted for less-invasive loop drainage over standard drainage and wound packing. In one study of 143 pediatric outcomes, a failure rate of 1.4% was reported in the loop group versus 10.5% in the packing group (P<.030),[26] while a separate study reported a 5.5% failure rate among loop patients.[27]
Prognosis
Even without treatment, skin abscesses rarely result in death, as they will naturally break through the skin.[3] Other types of abscess are more dangerous. Brain abscesses are fatal if untreated. When treated, the mortality rate reduces to 5–10%, but is higher if the abscess ruptures.[29]
Epidemiology
Skin abscesses are common and have become more common in recent years.[1] Risk factors include intravenous drug use, with rates reported as high as 65% among users.[2] In 2005 in the United States 3.2 million people went to the emergency department for an abscess.[5] In Australia around 13,000 people were hospitalized in 2008 for the disease.[11]
Society and culture
The Latin medical aphorism "ubi pus, ibi evacua" expresses "where there is pus, there evacuate it" and is classical advice in the culture of Western medicine.
Needle exchange programmes often administer or provide referrals for abscess treatment to injection drug users as part of a harm reduction public health strategy.[30][31]
Etymology
An abscess is so called "abscess" because there is an abscessus (a going away or departure) of portions of the animal tissue from each other to make room for the suppurated matter lodged between them.[32]
The word carbuncle is believed to have originated from the Latin: carbunculus, originally a small coal; diminutive of carbon-, carbo: charcoal or ember, but also a carbuncle stone, "precious stones of a red or fiery colour", usually garnets.[33]
Other types
The following types of abscess are listed in the medical dictionary:[34]
- acute abscess
- alveolar abscess
- amebic abscess
- apical abscess
- appendiceal abscess
- Bartholin abscess
- Bezold abscess
- bicameral abscess
- bone abscess
- brain abscess
- Brodie abscess
- bursal abscess
- caseous abscess
- caseous lymphadenitis
- cheesy abscess
- cholangitic abscess
- chronic abscess
- collar stud abscess
- cold abscess
- crypt abscesses
- dental abscess
- periapical abscess
- periodontal abscess
- apical periodontal abscess
- lateral periodontal abscess
- root abscess
- gingival abscess
- lateral alveolar abscess
- pericoronal abscess
- combined periodontic-endodontic abscess
- diffuse abscess
- Douglas abscess
- dry abscess
- Dubois abscesses
- embolic abscess
- fecal abscess
- follicular abscess
- gas abscess
- gravitation abscess
- gummatous abscess
- hidradenitis suppurativa
- hematogenous abscess
- hot abscess
- hypostatic abscess
- ischiorectal abscess
- mastoid abscess
- metastatic abscess
- migrating abscess
- miliary abscess
- Munro abscess
- orbital abscess
- otitic abscess
- palatal abscess
- pancreatic abscess
- parafrenal abscess
- parametric abscess
- paranephric abscess
- parapharyngeal abscess
- parotid
- Pautrier
- pelvic
- perforating
- periappendiceal
- periarticular
- pericemental
- perinephric
- perirectal
- peritonsillar abscess
- periureteral abscess
- phlegmonous abscess
- Pott abscess
- premammary abscess (including subareolar abscess)
- psoas abscess
- pulp abscess
- pyemic abscess
- radicular abscess
- residual abscess
- retrobulbar abscess
- retrocecal abscess
- retropharyngeal abscess
- ring abscess
- satellite abscess
- septicemic abscess
- stellate abscess
- stercoral abscess
- sterile abscess
- stitch abscess
- subdiaphragmatic abscess
- subepidermal abscess
- subhepatic abscess
- subperiosteal abscess
- subphrenic abscess
- subungual abscess
- sudoriferous abscess
- suture abscess
- thymic abscesses
- Tornwaldt abscess
- tropical abscess
- tubo-ovarian abscess
- verminous abscess
- wandering abscess
- worm abscess
References
- Singer, Adam J.; Talan, David A. (Mar 13, 2014). "Management of skin abscesses in the era of methicillin-resistant Staphylococcus aureus" (PDF). The New England Journal of Medicine. 370 (11): 1039–47. doi:10.1056/NEJMra1212788. PMID 24620867. Archived from the original (PDF) on 2014-10-30. Retrieved 2014-09-24.
- Langrod, Pedro Ruiz, Eric C. Strain, John G. (2007). The substance abuse handbook. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 373. ISBN 9780781760454. Archived from the original on 2017-09-06.
- Marx, John A. Marx (2014). "Skin and Soft Tissue Infections". Rosen's emergency medicine : concepts and clinical practice (8th ed.). Philadelphia, PA: Elsevier/Saunders. pp. Chapter 137. ISBN 1455706051.
- American College of Emergency Physicians, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Emergency Physicians, archived from the original on March 7, 2014, retrieved January 24, 2014
- Taira, BR; Singer, AJ; Thode HC, Jr; Lee, CC (Mar 2009). "National epidemiology of cutaneous abscesses: 1996 to 2005". The American Journal of Emergency Medicine. 27 (3): 289–92. doi:10.1016/j.ajem.2008.02.027. PMID 19328372.
- Elston, Dirk M. (2009). Infectious Diseases of the Skin. London: Manson Pub. p. 12. ISBN 9781840765144. Archived from the original on 2017-09-06.
- Marx, John A. Marx (2014). "Dermatologic Presentations". Rosen's emergency medicine : concepts and clinical practice (8th ed.). Philadelphia, PA: Elsevier/Saunders. pp. Chapter 120. ISBN 1455706051.
- Cox, Carol Turkington, Jeffrey S. Dover; medical illustrations, Birck (2007). The encyclopedia of skin and skin disorders (3rd ed.). New York, NY: Facts on File. p. 1. ISBN 9780816075096. Archived from the original on 2017-09-06.
- Vermandere, M; Aertgeerts, B; Agoritsas, T; Liu, C; Burgers, J; Merglen, A; Okwen, PM; Lytvyn, L; Chua, S; Vandvik, PO; Guyatt, GH; Beltran-Arroyave, C; Lavergne, V; Speeckaert, R; Steen, FE; Arteaga, V; Sender, R; McLeod, S; Sun, X; Wang, W; Siemieniuk, RAC (6 February 2018). "Antibiotics after incision and drainage for uncomplicated skin abscesses: a clinical practice guideline". BMJ (Clinical research ed.). 360: k243. doi:10.1136/bmj.k243. PMC 5799894. PMID 29437651.
- Singer, Adam J.; Thode, Henry C., Jr; Chale, Stuart; Taira, Breena R.; Lee, Christopher (May 2011). "Primary closure of cutaneous abscesses: a systematic review" (PDF). The American Journal of Emergency Medicine. 29 (4): 361–66. doi:10.1016/j.ajem.2009.10.004. PMID 20825801. Archived from the original (PDF) on 2015-07-22.
- Vaska, VL; Nimmo, GR; Jones, M; Grimwood, K; Paterson, DL (Jan 2012). "Increases in Australian cutaneous abscess hospitalisations: 1999-2008". European Journal of Clinical Microbiology & Infectious Diseases. 31 (1): 93–96. doi:10.1007/s10096-011-1281-3. PMID 21553298.
- United Kingdom National Health Service 'Abscess' Archived 2014-10-30 at the Wayback Machine
- Churchill Livingstone medical dictionary (16th ed.). Edinburgh: Churchill Livingstone. 2008. ISBN 9780080982458.
- Ferri, Fred F. (2014). Ferri's Clinical Advisor 2015 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 20. ISBN 9780323084307.
- Fischer, Josef E.; Bland, Kirby I.; Callery, Mark P. (2006). Mastery of Surgery. Lippincott Williams & Wilkins. p. 1033. ISBN 9780781771658.
- Khalil, PN; Huber-Wagner, S; Altheim, S; Bürklein, D; Siebeck, M; Hallfeldt, K; Mutschler, W; Kanz, GG (Sep 22, 2008). "Diagnostic and treatment options for skin and soft tissue abscesses in injecting drug users with consideration of the natural history and concomitant risk factors". European Journal of Medical Research. 13 (9): 415–24. PMID 18948233.
- Kraeutler, MJ; Bozzay, JD; Walker, MP; John, K (Oct 24, 2014). "Spinal subdural abscess following epidural steroid injection". J Neurosurg Spine. 22 (1): 90–3. doi:10.3171/2014.9.SPINE14159. PMID 25343407.
- Malik, Ali Irqam; Nelson, Richard L; Tou, Samson; Malik, Ali Irqam (2010). "Incision and drainage of perianal abscess with or without treatment of anal fistula". Reviews. doi:10.1002/14651858.CD006827.pub2.
- Duff, Patrick (2009). "Diagnosis and Management of Postoperative Infection". The Global Library of Women's Medicine. doi:10.3843/GLOWM.10032. ISSN 1756-2228. Archived from the original on 2014-07-14.
- "UOTW #66 - Ultrasound of the Week". Ultrasound of the Week. 7 January 2016. Archived from the original on 2 November 2016. Retrieved 27 May 2017.
- Robins/8th/68
- Barbic, D; Chenkin, J; Cho, DD; Jelic, T; Scheuermeyer, FX (10 January 2017). "In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis". BMJ Open. 7 (1): e013688. doi:10.1136/bmjopen-2016-013688. PMC 5253602. PMID 28073795.
- Medline Plus 'Abscess' Archived 2016-04-07 at the Wayback Machine
- Green, James; Saj Wajed (2000). Surgery: Facts and Figures. Cambridge University Press. ISBN 1-900151-96-0.
- Bergstrom, KG (Jan 2014). "News, views, and reviews. Less may be more for MRSA: the latest on antibiotics, the utility of packing an abscess, and decolonization strategies". Journal of Drugs in Dermatology. 13 (1): 89–92. PMID 24385125.
- Ladde JG, Baker S, Rodgers CN, Papa L (2015). "The LOOP technique: a novel incision and drainage technique in the treatment of skin abscesses in a pediatric ED". The American Journal of Emergency Medicine. 33 (2): 271–76. doi:10.1016/j.ajem.2014.10.014. PMID 25435407.
- Tsoraides SS, Pearl RH, Stanfill AB, Wallace LJ, Vegunta RK (2010). "Incision and loop drainage: a minimally invasive technique for subcutaneous abscess management in children". Journal of Pediatric Surgery. 45 (3): 606–09. doi:10.1016/j.jpedsurg.2009.06.013. PMID 20223328.
- Kronborg O, Olsen H (1984). "Incision and drainage v. incision, curettage and suture under antibiotic cover in anorectal abscess. A randomized study with 4-year follow-up". Acta Chirurgica Scandinavica. 150 (8): 689–92. PMID 6397949.
- Bokhari, Maria R.; Mesfin, Fassil B. (2019), "Brain Abscess", StatPearls, StatPearls Publishing, PMID 28722871, retrieved 2019-07-28
- Tomolillo, CM; Crothers, LJ; Aberson, CL (2007). "The damage done: a study of injection drug use, injection related abscesses and needle exchange regulation". Substance Use & Misuse. 42 (10): 1603–11. doi:10.1080/10826080701204763. PMID 17918030.
- Fink, DS; Lindsay, SP; Slymen, DJ; Kral, AH; Bluthenthal, RN (May 2013). "Abscess and self-treatment among injection drug users at four California syringe exchanges and their surrounding communities". Substance Use & Misuse. 48 (7): 523–31. doi:10.3109/10826084.2013.787094. PMC 4334130. PMID 23581506.
- Collier's New Encyclopedia, 'Abscess'.
- OED, "Carbuncle": 1 stone, 3 medical
- "Abscess". Medical Dictionary – Dictionary of Medicine and Human Biology. Archived from the original on 2013-02-05. Retrieved 2013-01-24.
External links
| Look up abscess in Wiktionary, the free dictionary. |
| Wikimedia Commons has media related to Abscesses. |
- MedlinePlus Encyclopedia: Abscess
- MedlinePlus Encyclopedia: Skin Abscess

- . Encyclopædia Britannica (11th ed.). 1911.
- "Abscess". MedlinePlus. U.S. National Library of Medicine.
| Classification | |
|---|---|
| External resources |