Corynebacterium
Corynebacterium (/kɔːˈraɪnəbækˌtɪəriəm, -ˈrɪn-/) is a genus of bacteria that are Gram-positive and aerobic. They are bacilli (rod-shaped), and in some phases of life they are, more particularly, club-shaped, which inspired the genus name (coryneform means "club-shaped").
| Corynebacterium | |
|---|---|
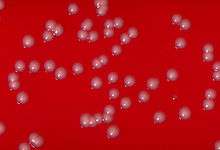 | |
| Corynebacterium ulcerans colonies on a blood agar plate | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Actinobacteria |
| Class: | Actinobacteria |
| Order: | Corynebacteriales |
| Family: | Corynebacteriaceae |
| Genus: | Corynebacterium Lehmann and Neumann 1896 (Approved Lists 1980) emend. Nouioui et al. 2018, nom. approb. |
| Species[1] | |
| |
They are widely distributed in nature in the microbiota of animals (including the human microbiota) and are mostly innocuous, most commonly existing in commensal relationships with their hosts.[2] Some are useful in industrial settings such as C. glutamicum.[3][4] Others can cause human disease, including most notably diphtheria, which is caused by C. diphtheriae. As with various species of a microbiota (including their cousins in the genera Arcanobacterium and Trueperella), they usually are not pathogenic but can occasionally opportunistically capitalize on atypical access to tissues (via wounds) or weakened host defenses.
Taxonomy
The genus Corynebacterium was created by Lehmann and Neumann in 1896 as a taxonomic group to contain the bacterial rods responsible for causing diphtheria. The genus was defined based on morphological characteristics. Based on studies of 16S-rRNA, they have been grouped into the subdivision of gram-positive eubacteria with high G:C content, with close phylogenetic relationship to Arthrobacter, Mycobacterium, Nocardia, and Streptomyces.[5]
The term comes from Greek κορύνη, korýnē 'club, mace, staff, knobby plant bud or shoot'[6] and βακτήριον, baktḗrion 'little rod'.[7] The term "diphtheroids" is used to represent corynebacteria that are non-pathogenic; for example, C. diphtheriae would be excluded. The term diphtheroid comes from Greek διφθέρα, diphthérā 'prepared hide, leather'.[8][9]
Genomics
Comparative analysis of corynebacterial genomes has led to the identification of several conserved signature indels which are unique to the genus. Two examples of these conserved signature indels are a two-amino-acid insertion in a conserved region of the enzyme phosphoribose diphosphate:decaprenyl-phosphate phosphoribosyltransferase and a three-amino-acid insertion in acetate kinase, both of which are found only in Corynebacterium species. Both of these indels serve as molecular markers for species of the genus Corynebacterium. Additionally, 16 conserved signature proteins, which are uniquely found in Corynebacterium species, have been identified. Three of the conserved signature proteins have homologs found in the genus Dietzia, which is believed to be the closest related genus to Corynebacterium. In phylogenetic trees based on concatenated protein sequences or 16S rRNA, the genus Corynebacterium forms a distinct clade, within which is a distinct subclade, cluster I. The cluster is made up of the species C. diptheriae, C. pseudotuberculosis, C. ulcerans, C. aurimucosum, C. glutamicum, and C. efficiens. This cluster is distinguished by several conserved signature indels, such as a two-amino-acid insertion in LepA and a seven- or eight-amino-acid insertions in RpoC. Also, 21 conserved signature proteins are found only in members of cluster I. Another cluster has been proposed, consisting of C. jeikeium and C. urealyticum, which is supported by the presence of 19 distinct conserved signature proteins which are unique to these two species.[10] Corynebateria have a high G+C content ranging from 46-74 mol%.[11]
Characteristics
The principal features of the genus Corynebacterium were described by Collins and Cummins in 1986.[12] They are gram-positive, catalase-positive, non-spore-forming, non-motile, rod-shaped bacteria that are straight or slightly curved.[13] Metachromatic granules are usually present representing stored phosphate regions. Their size falls between 2 and 6 μms in length and 0.5 μm in diameter. The bacteria group together in a characteristic way, which has been described as the form of a "V", "palisades", or "Chinese characters". They may also appear elliptical. They are aerobic or facultatively anaerobic, chemoorganotrophs. They are pleomorphic through their lifecycles, they occur in various lengths, and they frequently have thickenings at either end, depending on the surrounding conditions.[14]
Cell wall
The cell wall is distinctive, with a predominance of mesodiaminopimelic acid in the murein wall[2][13] and many repetitions of arabinogalactan, as well as corynemycolic acid (a mycolic acid with 22 to 26 carbon atoms), bound by disaccharide bonds called L-Rhap-(1 → 4)--D-GlcNAc-phosphate. These form a complex commonly seen in Corynebacterium species: the mycolyl-AG–peptidoglican (mAGP).[15]
Culture
Corynebacteria grow slowly, even on enriched media. In terms of nutritional requirements, all need biotin to grow. Some strains also need thiamine and PABA.[12] Some of the Corynebacterium species with sequenced genomes have between 2.5 and 3.0 million base pairs. The bacteria grow in Loeffler's medium, blood agar, and trypticase soy agar (TSA). They form small, grayish colonies with a granular appearance, mostly translucent, but with opaque centers, convex, with continuous borders.[13] The color tends to be yellowish-white in Loeffler's medium. In TSA, they can form grey colonies with black centers and dentated borders that look similar to flowers (C. gravis), or continuous borders (C. mitis), or a mix between the two forms (C. intermedium).
Habitat
Corynebacterium species occur commonly in nature in the soil, water, plants, and food products.[2][13] The nondiphtheiroid Corynebacterium species can even be found in the mucosa and normal skin flora of humans and animals.[2][13] Unusual habitats, such as the preen gland of birds have been recently reported for Corynebacterium uropygiale.[16] Some species are known for their pathogenic effects in humans and other animals. Perhaps the most notable one is C. diphtheriae, which acquires the capacity to produce diphtheria toxin only after interacting with a bacteriophage.[17] Other pathogenic species in humans include: C. amycolatum, C. striatum, C. jeikeium, C. urealyticum, and C. xerosis;[18][19][20][21][22] all of these are important as pathogens in immunosuppressed patients. Pathogenic species in other animals include C. bovis and C. renale.[23] This genus has been found to be part of the human salivary microbiome.[24]
Role in disease
The most notable human infection is diphtheria, caused by C. diphtheriae. It is an acute and contagious infection characterized by pseudomembranes of dead epithelial cells, white blood cells, red blood cells, and fibrin that form around the tonsils and back of the throat.[25] In developed countries, it is an uncommon illness that tends to occur in unvaccinated individuals, especially school-aged children, elderly, neutropenic or immunocompromised patients, and those with prosthetic devices such as prosthetic heart valves, shunts, or catheters. It is more common in developing countries[26] It can occasionally infect wounds, the vulva, the conjunctiva, and the middle ear. It can be spread within a hospital.[27] The virulent and toxigenic strains are lysogenic, and produce an exotoxin formed by two polypeptide chains, which is itself produced when a bacterium is transformed by a gene from the β prophage.[17]
Several species cause disease in animals, most notably C. pseudotuberculosis, which causes the disease caseous lymphadenitis, and some are also pathogenic in humans. Some attack healthy hosts, while others tend to attack the immunocompromised. Effects of infection include granulomatous lymphadenopathy, pneumonitis, pharyngitis, skin infections, and endocarditis. Corynebacterial endocarditis is seen most frequently in patients with intravascular devices.[28] C. tenuis is believed to cause trichomycosis palmellina and trichomycosis axillaris.[29] C. striatum may cause axillary odor.[30] C. minutissimum causes erythrasma.
Industrial uses
Nonpathogenic species of Corynebacterium are used for very important industrial applications, such as the production of amino acids,[31][32] nucleotides, and other nutritional factors (Martín, 1989); bioconversion of steroids;[33] degradation of hydrocarbons;[34] cheese aging;[35] and production of enzymes.[36] Some species produce metabolites similar to antibiotics: bacteriocins of the corynecin-linocin type,[27][37][38] antitumor agents,[39] etc. One of the most studied species is C. glutamicum, whose name refers to its capacity to produce glutamic acid in aerobic conditions.[40] This is used in the food industry as monosodium glutamate in the production of soy sauce and yogurt.
Species of Corynebacterium have been used in the mass production of various amino acids including glutamic acid, a food additive that is made at a rate of 1.5 million tons/ year. The metabolic pathways of Corynebacterium have been further manipulated to produce lysine and threonine.
L-Lysine production is specific to C. glutamicum in which core metabolic enzymes are manipulated through genetic engineering to drive metabolic flux towards the production of NADPH from the pentose phosphate pathway, and L-4-aspartyl phosphate, the commitment step to the synthesis of L-lysine, lysC, dapA, dapC, and dapF. These enzymes are up-regulated in industry through genetic engineering to ensure adequate amounts of lysine precursors are produced to increase metabolic flux. Unwanted side reactions such as threonine and asparagine production can occur if a buildup of intermediates occurs, so scientists have developed mutant strains of C. glutamicum through PCR engineering and chemical knockouts to ensure production of side-reaction enzymes are limited. Many genetic manipulations conducted in industry are by traditional cross-over methods or inhibition of transcriptional activators.[41]
Expression of functionally active human epidermal growth factor has been brought about in C. glutamicum,[42] thus demonstrating a potential for industrial-scale production of human proteins. Expressed proteins can be targeted for secretion through either the general secretory pathway or the twin-arginine translocation pathway.[43]
Unlike gram-negative bacteria, the gram-positive Corynebacterium species lack lipopolysaccharides that function as antigenic endotoxins in humans.
Species
Most species of corynebacteria are not lipophilic.
Nonlipophilic
The nonlipophilic bacteria may be classified as fermentative and nonfermentative:
- Fermentative corynebacteria
- Corynebacterium diphtheriae group
- Corynebacterium xerosis and Corynebacterium striatum
- Corynebacterium minutissimum
- Corynebacterium amycolatum
- Corynebacterium glucuronolyticum
- Corynebacterium argentoratense
- Corynebacterium matruchotii
- Corynebacterium glutamicum
- Corynebacterium sp.[44]
- Nonfermentative corynebacteria
- Corynebacterium afermentans subsp. afermentans
- Corynebacterium auris
- Corynebacterium pseudodiphtheriticum
- Corynebacterium propinquum[44]
Lipophilic
- Corynebacterium uropygiale[16]
- Corynebacterium jeikeium
- Corynebacterium urealyticum
- Corynebacterium afermentans subsp. lipophilum
- Corynebacterium accolens
- Corynebacterium macginleyi
- CDC coryneform groups F-1 and G
- Corynebacterium bovis[44]
Novel corynebacteria that do not contain mycolic acids
- Corynebacterium kroppenstedtii[45]
References
- "Corynebacterium" (HTML). NCBI taxonomy. Bethesda, MD: National Center for Biotechnology Information. Retrieved 4 February 2019.
- Collins, M. D. (2004). "Corynebacterium caspium sp. nov., from a Caspian seal (Phoca caspica)". International Journal of Systematic and Evolutionary Microbiology. 54 (3): 925–8. doi:10.1099/ijs.0.02950-0. PMID 15143043.
- Poetsch, A. (2011). "Proteomics of corynebacteria: From biotechnology workhorses to pathogens". Proteomics. 11 (15): 3244–3255. doi:10.1002/pmic.201000786. PMID 21674800.
- Burkovski A (editor). (2008). Corynebacteria: Genomics and Molecular Biology. Caister Academic Press. ISBN 978-1-904455-30-1.
- Woese, C. R. (1987). "Bacterial evolution". Microbiological Reviews. 51 (2): 221–71. doi:10.1128/MMBR.51.2.221-271.1987. PMC 373105. PMID 2439888.
- κορύνη. Liddell, Henry George; Scott, Robert; A Greek–English Lexicon at the Perseus Project.
- βακτήριον, βακτηρία in Liddell and Scott.
- διφθέρα in Liddell and Scott.
- Harper, Douglas. "diphtheria". Online Etymology Dictionary.
- Gao, B.; Gupta, R. S. (2012). "Phylogenetic Framework and Molecular Signatures for the Main Clades of the Phylum Actinobacteria". Microbiology and Molecular Biology Reviews. 76 (1): 66–112. doi:10.1128/MMBR.05011-11. PMC 3294427. PMID 22390973.
- Bernard, K.A.; Funke, G. (2012). "Genus I. Corynebacterium". In Goodfellow, M.; Kampfer, P.; Busse, H.J.; Trujillo, M.E.; Suzuki, K.; Ludwig, W.; Whitman, W.B. (eds.). Bergey's Manual of Systematic Bacteriology (2nd ed.). Springer. p. 245.
- Collins, M. D.; Cummins, C. S. (1986). "Genus Corynebacterium Lehmann and Neumann 1896, 350AL". In Sneath, P. H. A.; Mair, N. S.; Sharpe, M. E.; Holt, J. G. (eds.). Bergey's Manual of Systematic Bacteriology. 2. Baltimore: Williams & Wilkins. pp. 1266–76.
- Yassin, A. F. (2003). "Corynebacterium glaucum sp. nov". International Journal of Systematic and Evolutionary Microbiology. 53 (3): 705–9. doi:10.1099/ijs.0.02394-0. PMID 12807190.
- Keddie, R. M.; Cure, G. L. (1977). "The Cell Wall Composition and Distribution of Free Mycolic Acids in Named Strains of Coryneform Bacteria and in Isolates from Various Natural Sources". Journal of Applied Bacteriology. 42 (2): 229–52. doi:10.1111/j.1365-2672.1977.tb00689.x. PMID 406255.
- Seidel, M.; Alderwick, L. J.; Sahm, H.; Besra, G. S.; Eggeling, L. (2006). "Topology and mutational analysis of the single Emb arabinofuranosyltransferase of Corynebacterium glutamicum as a model of Emb proteins of Mycobacterium tuberculosis". Glycobiology. 17 (2): 210–9. doi:10.1093/glycob/cwl066. PMID 17088267.
- Braun, Markus Santhosh; Zimmermann, Stefan; Danner, Maria; Rashid, Harun-or; Wink, Michael (2016). "Corynebacterium uropygiale sp. nov., isolated from the preen gland of Turkeys (Meleagris gallopavo)". Systematic and Applied Microbiology. 39 (2): 88–92. doi:10.1016/j.syapm.2015.12.001. PMID 26776107.
- Costa, J. J.; Michel, J. L.; Rappuoli, R; Murphy, J. R. (1981). "Restriction map of corynebacteriophages beta c and beta vir and physical localization of the diphtheria tox operon". Journal of Bacteriology. 148 (1): 124–30. doi:10.1128/JB.148.1.124-130.1981. PMC 216174. PMID 6270058.
- Oteo, Jesús; Aracil, Belén; Ignacio Alós, Juan; Luis Gómez-Garcés, Jose (2001). "Bacteriemias significativas por Corynebacterium amycolatum: Un patógeno emergente" [Significant bacteremias by Corynebacterium amycolatum: an emergent pathogen]. Enfermedades Infecciosas y Microbiología Clínica (in Spanish). 19 (3): 103–6. doi:10.1016/S0213-005X(01)72578-5. PMID 11333587.
- Lagrou, K; Verhaegen, J; Janssens, M; Wauters, G; Verbist, L (1998). "Prospective Study of Catalase-positive Coryneform Organisms in Clinical Specimens: Identification, Clinical Relevance, and Antibiotic Susceptibility". Diagnostic Microbiology and Infectious Disease. 30 (1): 7–15. doi:10.1016/S0732-8893(97)00193-4. PMID 9488824.
- Boc, SF; Martone, JD (1995). "Osteomyelitis caused by Corynebacterium jeikeium". Journal of the American Podiatric Medical Association. 85 (6): 338–9. doi:10.7547/87507315-85-6-338. PMID 7602508.
- Kono, M.; Sasatsu, M.; Aoki, T. (1983). "R Plasmids in Corynebacterium xerosis Strains". Antimicrobial Agents and Chemotherapy. 23 (3): 506–8. doi:10.1128/aac.23.3.506. PMC 184682. PMID 6847177.
- Pitcher, D.G. (1983). "Deoxyribonucleic acid base composition of Corynebacterium diphtheriaeand other corynebacteria with cell wall type IV". FEMS Microbiology Letters. 16 (2–3): 291–5. doi:10.1111/j.1574-6968.1983.tb00305.x.
- Hirsbrunner, G; Lang, J; Nicolet, J; Steiner, A (1996). "Nephrektomie nach chronischer, unilateraler, eitriger Pyelonephritis beim Rind" [Nephrectomy for chronic, unilateral suppurative pyleonephritis in cattle]. Tierarztliche Praxis (in German). 24 (1): 17–21. PMID 8720950.
- Wang, Kun; Lu, Wenxin; Tu, Qichao; Ge, Yichen; He, Jinzhi; Zhou, Yu; Gou, Yaping; Nostrand, Joy D Van; Qin, Yujia; Li, Jiyao; Zhou, Jizhong; Li, Yan; Xiao, Liying; Zhou, Xuedong (10 March 2016). "Preliminary analysis of salivary microbiome and their potential roles in oral lichen planus". Scientific Reports. 6 (1): 22943. Bibcode:2016NatSR...622943W. doi:10.1038/srep22943. PMC 4785528. PMID 26961389.
- "Difteria: MedlinePlus enciclopedia médica". www.nlm.nih.gov.
- Iizuka, Hideyo; Furuta, Joana Akiko; Oliveira, Edison P. Tavares de (1980). "Difteria: Situação imunitária de uma população infantil urbana de São Paulo, SP, Brasil" [Diphtheria. Immunity in an infant population in the City of S. Paulo, SP, Brazil]. Revista de Saúde Pública (in Portuguese). 14 (4): 462–8. doi:10.1590/S0034-89101980000400005. PMID 7268290.
- Kerry-Williams, S. M.; Noble, W. C. (2009). "Plasmids in group JK coryneform bacteria isolated in a single hospital". Journal of Hygiene. 97 (2): 255–63. doi:10.1017/S0022172400065347. PMC 2083551. PMID 3023480.
- León, Cristóbal; Ariza, Javier (2004). "Guías para el tratamiento de las infecciones relacionadas con catéteres intravasculares de corta permanencia en adultos: Conferencia de consenso SEIMC-SEMICYUC" [Guidelines for the treatment of infections related to short-stay intravascular catheters in adults: consensus conference SEIMC-SEMICYUC]. Enfermedades Infecciosas y Microbiología Clínica (in Spanish). 22 (2): 92–7. doi:10.1157/13056889.
- Trichomycosis axilarris at eMedicine
- Natsch, A.; Gfeller, H.; Gygax, P.; Schmid, J. (2005). "Isolation of a bacterial enzyme releasing axillary malodor and its use as a screening target for novel deodorant formulations1". International Journal of Cosmetic Science. 27 (2): 115–22. doi:10.1111/j.1467-2494.2004.00255.x. PMID 18492161.
- Hongo, M.; Oki, T.; Ogata, S. (1972). "Phage contamination and control". In Yamada, K.; Kinoshita, S; Tsunoda, T.; Aida, K. (eds.). The Microbial Production of Amino Acids. New York: John Wiley. pp. 63–83.
- Yamada, K.; Kinoshita, S.; Tsunoda, T.; Aida, K., eds. (1972). The Microbial Production of Amino Acids. New York: Wiley.
- Constantinides, Alkis (1980). "Steroid transformation at high substrate concentrations using immobilized Corynebacterium simplex cells". Biotechnology and Bioengineering. 22 (1): 119–36. doi:10.1002/bit.260220110. PMID 7350926.
- Cooper, D. G.; Zajic, J. E.; Gracey, D. E. (1979). "Analysis of corynomycolic acids and other fatty acids produced by Corynebacterium lepus grown on kerosene". Journal of Bacteriology. 137 (2): 795–801. doi:10.1128/JB.137.2.795-801.1979. PMC 218359. PMID 422512.
- Lee, Chang-Won; Lucas, Serge; Desmazeaud, Michel J. (1985). "Phenylalanine and tyrosine catabolism in some cheese coryneform bacteria". FEMS Microbiology Letters. 26 (2): 201–5. doi:10.1111/j.1574-6968.1985.tb01591.x.
- Khurana, Sumit; Sanli, Gulsah; Powers, David B.; Anderson, Stephen; Blaber, Michael (2000). "Molecular modeling of substrate binding in wild-type and mutant Corynebacteria 2,5-diketo-D-gluconate reductases". Proteins: Structure, Function, and Genetics. 39 (1): 68–75. CiteSeerX 10.1.1.661.3412. doi:10.1002/(SICI)1097-0134(20000401)39:1<68::AID-PROT7>3.0.CO;2-Y. PMID 10737928.
- Kerry-Williams, S.M.; Noble, W.C. (1984). "Plasmid-associated bacteriocin production in a JK-type coryneform bacterium". FEMS Microbiology Letters. 25 (2–3): 179–82. doi:10.1111/j.1574-6968.1984.tb01451.x.
- Suzuki, Takeo; Honda, Haruo; Katsumata, Ryoichi (1972). "Production of Antibacterial Compounds Analogous to Chloramphenicol by a n-Paraffin-grown Bacterium". Agricultural and Biological Chemistry. 36 (12): 2223–8. doi:10.1271/bbb1961.36.2223.
- Milas, Luka; Scott, Martin T. (1978). "Antitumor Activity of Corynebacterium Parvum". In Ford, Marvella E.; Watson, Dennis K. (eds.). Advances in Cancer Research. 26. pp. 257–306. doi:10.1016/S0065-230X(08)60090-1. ISBN 978-0-12-809878-3. PMID 343523. Missing or empty
|title=(help) - Abe, Shigeo; Takayama, KEN-Ichiro; Kinoshita, Shukuo (1967). "Taxonomical Studies on Glutamic Acid-Producing Bacteria". The Journal of General and Applied Microbiology. 13 (3): 279–301. doi:10.2323/jgam.13.279.
- Kjeldsen, Kjeld Raunkjær (2009). Optimization of an industrial L-lysine producing Corynebacterium glutamicum strain (PhD Thesis). Technical University of Denmark. OCLC 826400572.
- Date, M.; Itaya, H.; Matsui, H.; Kikuchi, Y. (2006). "Secretion of human epidermal growth factor by Corynebacterium glutamicum". Letters in Applied Microbiology. 42 (1): 66–70. doi:10.1111/j.1472-765X.2005.01802.x. PMID 16411922.
- Meissner, Daniel; Vollstedt, Angela; Van Dijl, Jan Maarten; Freudl, Roland (2007). "Comparative analysis of twin-arginine (Tat)-dependent protein secretion of a heterologous model protein (GFP) in three different Gram-positive bacteria". Applied Microbiology and Biotechnology. 76 (3): 633–42. doi:10.1007/s00253-007-0934-8. PMID 17453196.
- Funke, G; von Graevenitz, A; Clarridge Je, 3rd; Bernard, K. A. (1997). "Clinical microbiology of coryneform bacteria". Clinical Microbiology Reviews. 10 (1): 125–59. doi:10.1128/CMR.10.1.125. PMC 172946. PMID 8993861.
- Collins, M. D.; Falsen, E.; Akervall, E.; Sjoden, B.; Alvarez, A. (1998). "Note: Corynebacterium kroppenstedtii sp. nov., a novel corynebacterium that does not contain mycolic acids". International Journal of Systematic Bacteriology. 48 (4): 1449–54. doi:10.1099/00207713-48-4-1449. PMID 9828448.
| Wikispecies has information related to Corynebacterium |
Further reading
- Burkovski, Andreas, ed. (2008). Corynebacteria: Genomics and Molecular Biology. Caister Academic Press. ISBN 978-1-904455-30-1.
- Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 978-0-8385-8529-0.CS1 maint: extra text: authors list (link)
- Database of Corynebacterial Transcription Factors and Regulatory Networks
- Rollins, David M. University of Maryland: Pathogentic Microbiology: Corynebacterium
- Khamis, A.; Raoult, D.; Scola, B. La (2004). "rpoB gene sequencing for identification of Corynebacterium species". Journal of Clinical Microbiology. 42 (9): 3925–3931. doi:10.1128/jcm.42.9.3925-3931.2004.
- Poetsch, A.; Haußmann, U.; Burkovski, A. (2011). "Proteomics of corynebacteria: From biotechnology workhorses to pathogens". Proteomics. 2011 (11): 3244–3255. doi:10.1002/pmic.201000786. PMID 21674800.
- Goldenberger, D.; et al. (2014). "Extended characterization of Corynebacterium pyruviciproducens based on clinical strains from Canada and Switzerland". Journal of Clinical Microbiology. 52 (9): 3180–3183. doi:10.1128/jcm.00792-14.
- Hacker, E.; et al. (2015). "Colonization of human epithelial cell lines by Corynebacterium ulcerans from human and animal sources". Microbiology (United Kingdom). 161 (8): 1582–1591. doi:10.1099/mic.0.000121.
- Bernard, K. A.; Munro, C.; Wiebe, D.; Ongsanso, E. (2002). "Characteristics of rare or recently described Corynebacterium species recovered from human clinical material in Canada". Journal of Clinical Microbiology. 40 (11): 4375–4381. doi:10.1128/jcm.40.11.4375-4381.2002.
- Bittel, M.; Gastiger, S.; Amin, B.; Hofmann, J.; Burkovski, A. (2018). "Surface and Extracellular Proteome of the Emerging Pathogen Corynebacterium ulcerans". Proteomes. 6 (2): 18. doi:10.3390/proteomes6020018.
- Ventura, M.; et al. (2007). "Genomics of Actinobacteria: Tracing the Evolutionary History of an Ancient Phylum". Microbiology and Molecular Biology Reviews. 71 (3): 495–548. doi:10.1128/mmbr.00005-07. PMC 2168647. PMID 17804669.
- Hansmeier, N.; Chao, T. C.; Kalinowski, J.; Pühler, A.; Tauch, A. (2006). "Mapping and comprehensive analysis of the extracellular and cell surface proteome of the human pathogen Corynebacterium diphtheriae". Proteomics. 2006 (6): 2465–2476. doi:10.1002/pmic.200500360.
- Riegel, P.; Ruimy, R.; Christen, R.; Monteil, H. (1996). "Species identities and antimicrobial susceptibilities of Corynebacteria isolated from various clinical sources". European Journal of Clinical Microbiology and Infectious Diseases. 15 (8): 657–662. doi:10.1007/bf01691153.
- Riegel, P; Ruimy, R; Christen, R; Monteil, H (1996). "Species identities and antimicrobial susceptibilities of corynebacteria isolated from various clinical sources". European Journal of Clinical Microbiology & Infectious Diseases. 15 (8): 657–62. doi:10.1007/bf01691153.
- Carfora, V.; et al. (2018). "Non-toxigenic Corynebacterium ulcerans sequence types 325 and 339 isolated from two dogs with ulcerative lesions in Italy. [Internet]". Journal of Veterinary Diagnostic Investigation. 30 (3): 447–450. doi:10.1177/1040638718764786.
- Nishio, Y.; et al. (2007). "Evolutionary process of amino acid biosynthesis in Corynebacterium at the whole genome level. [Internet]". Molecular Biology and Evolution. 21 (9): 1683–1691. doi:10.1093/molbev/msh175.