Hemolytic disease of the newborn
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis,[1] is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules (one of the five main types of antibodies) produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells (hemolysis). The fetus can develop reticulocytosis and anemia. This fetal disease ranges from mild to very severe, and fetal death from heart failure (hydrops fetalis) can occur. When the disease is moderate or severe, many erythroblasts (immature red blood cells) are present in the fetal blood, and so these forms of the disease can be called erythroblastosis fetalis (or erythroblastosis foetalis).
| Hemolytic disease of the newborn | |
|---|---|
| Other names | HDN |
 | |
| Specialty | Pediatrics, Immunohaematology |
| Complications | heart failure, splenomegaly |
HDFN represents a breach of immune privilege for the fetus or some other form of impairment of the immune tolerance of pregnancy. Various types of HDFN are classified by which alloantigen provokes the response. In order of incidence, the types include ABO, anti-RhD, anti-RhE, anti-Rhc, anti-Rhe, anti-RhC, multiantigen combinations, and anti-Kell.
Signs and symptoms
Signs of hemolytic disease of the newborn include a positive direct Coombs test (also called direct agglutination test), elevated cord bilirubin levels, and hemolytic anemia. It is possible for a newborn with this disease to have neutropenia and neonatal alloimmune thrombocytopenia as well. Hemolysis leads to elevated bilirubin levels. After delivery bilirubin is no longer cleared (via the placenta) from the neonate's blood and the symptoms of jaundice (yellowish skin and yellow discoloration of the whites of the eyes, or icterus) increase within 24 hours after birth. Like other forms of severe neonatal jaundice, there is the possibility of the neonate developing acute or chronic kernicterus, however the risk of kernicterus in HDN is higher because of the rapid and massive destruction of blood cells. It is important to note that isoimmunization is a risk factor for neurotoxicity and lowers the level at which kernicterus can occur. Untreated profound anemia can cause high-output heart failure, with pallor, enlarged liver and/or spleen, generalized swelling, and respiratory distress.
HDN can be the cause of hydrops fetalis, an often-severe form of prenatal heart failure that causes fetal edema.[2]
Complications
Complications of HDN could include kernicterus, hepatosplenomegaly, inspissated (thickened or dried) bile syndrome and/or greenish staining of the teeth, hemolytic anemia and damage to the liver due to excess bilirubin. Conditions that may cause similar symptoms in the newborn period include: acquired hemolytic anemia, congenital toxoplasma, congenital syphilis infection, congenital obstruction of the bile duct, and cytomegalovirus (CMV) infection.
- High at birth or rapidly rising bilirubin[3]
- Prolonged hyperbilirubinemia[3]
- Bilirubin Induced Neurological Dysfunction[4]
- Cerebral Palsy[5]
- Kernicterus[6]
- Neutropenia[7][8]
- Thrombocytopenia[7]
- Hemolytic anemia – Must NOT be treated with iron[9]
- Late onset anemia – Must NOT be treated with iron. Can persist up to 12 weeks after birth.[10][11][12]
Pathophysiology
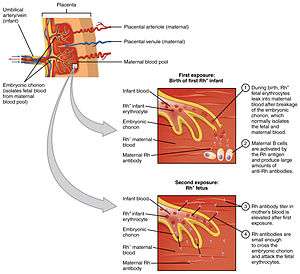
Antibodies are produced when the body is exposed to an antigen foreign to the make-up of the body. If a mother is exposed to a foreign antigen and produces IgG (as opposed to IgM which does not cross the placenta), the IgG will target the antigen, if present in the fetus, and may affect it in utero and persist after delivery. The three most common models in which a woman becomes sensitized toward (i.e., produces IgG antibodies against) a particular antigen are hemorrhage, blood transfusion, and ABO incompatibility.
Fetal-maternal hemorrhage, which is the movement of fetal blood cells across the placenta, can occur during abortion, ectopic pregnancy, childbirth, ruptures in the placenta during pregnancy (often caused by trauma), or medical procedures carried out during pregnancy that breach the uterine wall. In subsequent pregnancies, if there is a similar incompatibility in the fetus, these antibodies are then able to cross the placenta into the fetal bloodstream to attach to the red blood cells and cause their destruction (hemolysis). This is a major cause of HDN, because 75% of pregnancies result in some contact between fetal and maternal blood, and 15–50% of pregnancies have hemorrhages with the potential for immune sensitization. The amount of fetal blood needed to cause maternal sensitization depends on the individual's immune system and ranges from 0.1 mL to 30 mL.[2]
The woman may have received a therapeutic blood transfusion. ABO blood group system and the D antigen of the Rhesus (Rh) blood group system typing are routine prior to transfusion. Suggestions have been made that women of child-bearing age or young girls should not be given a transfusion with Rhc-positive blood or Kell1-positive blood to avoid possible sensitization, but this would strain the resources of blood transfusion services, and it is currently considered uneconomical to screen for these blood groups. HDFN can also be caused by antibodies to a variety of other blood group system antigens, but Kell and Rh are the most frequently encountered.
The third sensitization model can occur in women of blood type O. The immune response to A and B antigens, that are widespread in the environment, usually leads to the production of IgM or IgG anti-A and anti-B antibodies early in life. Women of blood type O are more prone than women of types A and B to making IgG anti-A and anti-B antibodies, and these IgG antibodies are able to cross the placenta. For unknown reasons, the incidence of maternal antibodies against type A and B antigens of the IgG type that could potentially cause hemolytic disease of the newborn is greater than the observed incidence of "ABO disease." About 15% of pregnancies involve a type O mother and a type A or type B child; only 3% of these pregnancies result in hemolytic disease due to A/B/O incompatibility. In contrast to antibodies to A and B antigens, Rhesus antibodies are generally not produced from exposure to environmental antigens. In cases where there is ABO incompatibility and Rh incompatibility, the risk of alloimmunization is decreased because fetal red blood cells are removed from maternal circulation due to anti-ABO antibodies before they can trigger an anti-Rh response.[2]
Antibody specific
- Anti-D is the only preventable form of HDN. Since the 1968 introduction of Rho-D immunoglobulin, (Rhogam), which prevents the production of maternal Rho-D antibodies, the incidence of anti-D HDN has decreased dramatically.[2][13]
- Anti-C and anti-c can both show a negative DAT but still have a severely affected infant.[14][15] An indirect Coombs must also be run.
- Anti-M also recommends antigen testing to rule out the presence of HDN as the direct coombs can come back negative in a severely affected infant.[16]
- Anti-Kell can cause severe anemia regardless of titer.[17] Anti-Kell suppresses the bone marrow,[18] by inhibiting the erythroid progenitor cells.[19][20]
- Kidd antigens are also present on the endothelial cells of the kidneys[21][22]
- One study done by Moran et al., found that titers are not reliable for anti-E. Their most severe case of hemolytic disease of the newborn occurred with titers 1:2. Moran states that it would be unwise routinely to dismiss anti-E as being of little clinical consequence.[23]
Diagnosis
The diagnosis of HDN is based on history and laboratory findings:
Blood tests done on the newborn baby
- Biochemistry tests for jaundice including total and direct bilirubin levels.
- Complete blood count (CBC) which may show a decreased hemoglobin and hematocrit due to red blood cell destruction
- Reticulocyte count which will usually be increased as the bone marrow makes new red blood cells to replace the ones that are being destroyed, and a peripheral blood smear to look at cell morphology. In the presence of significant hemolysis the smear will show schistocytes (fragmented red blood cells), reticulocytosis, and in severe cases Erythroblasts (also known as nucleated red blood cells).
- Positive direct Coombs test (might be negative after fetal interuterine blood transfusion)
Blood tests done on the mother
- Positive indirect Coombs test
Blood tests done on the father (rarely needed)
- Erythrocyte antigen status
Types (classified by serology)
Types of HDN are classified by the type of antigens involved. The main types are ABO HDN, Rhesus HDN, Kell HDN, and other antibodies. ABO hemolytic disease of the newborn can range from mild to severe, but generally it is a mild disease. It can be caused by anti-A and anti-B antibodies. Rhesus D hemolytic disease of the newborn (often called Rh disease) is the most common form of severe HDN. Rhesus c hemolytic disease of the newborn can range from a mild to severe disease – is the third most common form of severe HDN.[24] Rhesus e and rhesus C hemolytic disease of the newborn are rare. Combinations of antibodies, for example, anti-Rhc and anti-RhE occurring together can be especially severe.
Anti-Kell hemolytic disease of the newborn is most commonly caused by anti-K 1 antibodies, the second most common form of severe HDN. Over half of the cases of anti-K 1 related HDN are caused by multiple blood transfusions. Antibodies to the other Kell antigens are rare.[24]
Prevention
In cases of Rho(D) incompatibility, Rho(D) immunoglobulin is given to prevent sensitization. However, there is no comparable immunotherapy available for other blood group incompatibilities.[2]
Early pregnancy
- IVIG – IVIG stands for Intravenous Immunoglobulin. It is used in cases of previous loss, high maternal titers, known aggressive antibodies, and in cases where religion prevents blood transfusion. IVIG can be more effective than IUT alone.[25] Fetal mortality was reduced by 36% in the IVIG and IUT group than in the IUT alone group. IVIG and plasmapheresis together can reduce or eliminate the need for an IUT.[26]
- Plasmapheresis – Plasmapheresis aims to decrease the maternal titer by direct plasma replacement and physical removal of antibody.[16] Plasmapheresis and IVIG together can even be used on women with previously hydropic fetuses and fetal losses.[27][28]
Mid- to late- pregnancy
- IUT – Intrauterine Transfusion (IUT) is done either by intraperitoneal transfusion (IPT) or intravenous transfusion (IVT).[29] IVT is preferred over IPT.[30] IUTs are only done until 35 weeks. After that, the risk of an IUT is greater than the risk from post birth transfusion.[31]
- Steroids – Steroids are sometimes given to the mother before IUTs and early delivery to mature the fetal lungs.[31][32]
- Phenobarbital – Phenobarbital is sometimes given to the mother to help mature the fetal liver and reduce hyperbilirubinemia.[32][33]
- Early Delivery – Delivery can occur anytime after the age of viability.[30] Emergency delivery due to failed IUT is possible, along with induction of labor at 35–38 weeks.[31][34]
Rhesus-negative mothers who are pregnant with a rhesus-positive infant are offered Rho(D) immune globulin (RhIG, or RhoGam) at 28 weeks during pregnancy, at 34 weeks, and within 48 hours after delivery to prevent sensitization to the D antigen. It works by binding any fetal red blood cells with the D antigen before the mother is able to produce an immune response and form anti-D IgG.[2] A drawback to pre-partum administration of RhIG is that it causes a positive antibody screen when the mother is tested, which can be difficult to distinguish from natural immunological responses that result in antibody production. Without Rho(D) immunoglobulin, the risk of isoimmunization is approximately 17%; with proper administration the risk is reduced to less than 0.1–0.2%.[2]
After birth testing
- Coombs – in certain instances (when there is concern for blood group incompatibility between mom and baby for example), after birth a baby will have a direct Coombs test run to confirm the antibodies attached to the infant's red blood cells. This test is run on the infant's cord blood.[3]
In some cases, the direct Coombs will be negative but severe, even fatal HDN can occur.[14] An indirect Coombs needs to be run in cases of anti-C,[15] anti-c,[15] and anti-M. Infants with Anti-M are also recommended to receive antigen testing to rule out the presence of HDN.[16] The below tests are often useful in cases of hemolytic disease of the newborn, but are not required for treatment of all newborns.
- Hgb – the infant's hemoglobin should be tested from cord blood.[3]
- Reticulocyte count – Reticulocytes are elevated when the infant is producing more red blood cells in response to anemia.[3] A rise in the retic count can mean that an infant may not need additional transfusions.[35] Low retic is observed in infants treated with IUT and in those with HDN from anti-Kell.[15]
- Neutrophils – as neutropenia is one of the complications of HDN, the neutrophil count should be checked.[7][8]
- Thrombocytes - as thrombocytopenia is one of the complications of HDN, the thrombocyte count should be checked.[7]
- Bilirubin should be tested from cord blood.[3]
- Ferritin – because most infants affected by HDN have iron overload, a ferritin must be run before giving the infant any additional iron.[9]
- Newborn Screening Tests – Transfusion with donor blood during pregnancy or shortly after birth can affect the results of the Newborn Screening Tests. It is recommended to wait and retest 10–12 months after last transfusion. In some cases, DNA testing from saliva can be used to rule out certain conditions.
Treatment
After birth, treatment depends on the severity of the condition, but could include temperature stabilization and monitoring, phototherapy, transfusion with compatible packed red blood, exchange transfusion, sodium bicarbonate for correction of acidosis and/or assisted ventilation.
- Phototherapy – Exposure to ultraviolet light (phototherapy) is recommended when the cord bilirubin is 3 or higher. Some doctors use it at lower levels while awaiting lab results.[36] This converts unconjugated bilirubin to an conjugated form that is easier for the infant to clear.
- IVIG - IVIG has been used to successfully treat many cases of HDN. It has been used not only on anti-D, but on anti-E as well.[37] IVIG can be used to reduce the need for exchange transfusion and to shorten the length of phototherapy.[38] The AAP recommends "In isoimmune hemolytic disease, administration of intravenousγ-globulin (0.5-1 g/kg over 2 hours) is recommended if the TSB is rising despite intensive phototherapy or the TSB level is within 2 to 3 mg/dL (34–51 μmol/L) of the exchange level. If necessary, this dose can be repeated in 12 hours (evidence quality B: benefits exceed harms). Intravenous γ-globulin has been shown to reduce the need for exchange transfusions in Rh and ABO hemolytic disease."[36]
- Exchange transfusion – Exchange transfusion is used when bilirubin reaches either the high or medium risk lines on the nonogram provided by the American Academy of Pediatrics (Figure 4).[36] Cord bilirubin >4 is also indicative of the need for exchange transfusion.[39]
Transfusion reactions
Once a woman has antibodies, she is at high risk for a future transfusion reaction if she is in need of a blood transfusion.[40] For this reason, she must carry a medical alert card at all times and inform all doctors and emergency personnel of her antibody status. The absence of antibodies however does not preclude a woman from having a transfusion reaction:
"Acute hemolytic transfusion reactions may be either immune-mediated or nonimmune-mediated. Immune-mediated hemolytic transfusion reactions caused by immunoglobulin M (IgM) anti-A, anti-B, or anti-A,B typically result in severe, potentially fatal complement-mediated intravascular hemolysis. Immune-mediated hemolytic reactions caused by IgG, Rh, Kell, Duffy, or other non-ABO antibodies typically result in extravascular sequestration, shortened survival of transfused red cells, and relatively mild clinical reactions. Acute hemolytic transfusion reactions due to immune hemolysis may occur in patients who have no antibodies detectable by routine laboratory procedures."[41]
For a summary of transfusion reactions in the US, see reference.[42]
Epidemiology
In 2003, the incidence of Rh(D) sensitization in the United States was 6.8 per 1000 live births; 0.27% of women with an Rh incompatible fetus experience alloimmunization.[2]
Other animals
Hemolytic disease of the newborn is most commonly seen in kittens (where it is known as "fading kitten syndrome") and foals. It has also been reported in puppies.
See also
References
- "erythroblastosis fetalis" at Dorland's Medical Dictionary
- Arraut, Amaryllis (2017-03-09). "Erythrocyte Alloimmunization and Pregnancy: Overview, Background, Pathophysiology". Medscape.
- Murray, N. A; Roberts, I. A G (2007). "Haemolytic disease of the newborn". Archives of Disease in Childhood: Fetal and Neonatal Edition. 92 (2): F83–8. doi:10.1136/adc.2005.076794. PMC 2675453. PMID 17337672.
- Shapiro, Steven M (2004). "Definition of the Clinical Spectrum of Kernicterus and Bilirubin-Induced Neurologic Dysfunction (BIND)". Journal of Perinatology. 25 (1): 54–9. doi:10.1038/sj.jp.7211157. PMID 15578034. S2CID 19663259.
- Blair, Eve; Watson, Linda (2006). "Epidemiology of cerebral palsy". Seminars in Fetal and Neonatal Medicine. 11 (2): 117–25. doi:10.1016/j.siny.2005.10.010. PMID 16338186.
- Lande, Lottie (1948). "Clinical signs and development of survivors of kernicterus due to Rh sensitization". The Journal of Pediatrics. 32 (6): 693–705. doi:10.1016/S0022-3476(48)80225-8. PMID 18866937.
- Koenig, J. M.; Christensen, R. D. (1989). "Neutropenia and thrombocytopenia in infants with Rh hemolytic disease". The Journal of Pediatrics. 114 (4 Pt 1): 625–31. doi:10.1016/s0022-3476(89)80709-7. PMID 2494315.
- Lalezari, P; Nussbaum, M; Gelman, S; Spaet, T. H. (1960). "Neonatal neutropenia due to maternal isoimmunization". Blood. 15 (2): 236–43. doi:10.1182/blood.V15.2.236.236. PMID 14413526.
- Rath, M. E. A.; Smits-Wintjens, V. E. H. J.; Oepkes, D.; Walther, F. J.; Lopriore, E. (2013). "Iron status in infants with alloimmune haemolytic disease in the first three months of life". Vox Sanguinis. 105 (4): 328–33. doi:10.1111/vox.12061. PMID 23802744.
- Mitchell, S; James, A (1999). "Severe late anemia of hemolytic disease of the newborn". Paediatrics & Child Health. 4 (3): 201–3. doi:10.1093/pch/4.3.201. PMC 2828194. PMID 20212966.
- Al-Alaiyan, S.; Al Omran, A. (1999). "Late hyporegenerative anemia in neonates with rhesus hemolytic disease". Journal of Perinatal Medicine. 27 (2): 112–5. doi:10.1515/JPM.1999.014. PMID 10379500. S2CID 32155893.
- Jadala, Hareesh; v., Pooja; k., Raghavendra; m., Prithvish; b., Srinivas (2016). "Late onset severe anemia due to rhesus isoimmunization". International Journal of Contemporary Pediatrics: 1472–3. doi:10.18203/2349-3291.ijcp20163704.
- Basu, Sabita; Kaur, Ravneet; Kaur, Gagandeep (2011). "Hemolytic disease of the fetus and newborn: Current trends and perspectives". Asian Journal of Transfusion Science. 5 (1): 3–7. doi:10.4103/0973-6247.75963. PMC 3082712. PMID 21572705.
- Heddle, N. M.; Wentworth, P; Anderson, D. R.; Emmerson, D; Kelton, J. G.; Blajchman, M. A. (1995). "Three examples of Rh haemolytic disease of the newborn with a negative direct antiglobulin test". Transfusion Medicine. 5 (2): 113–6. doi:10.1111/j.1365-3148.1995.tb00197.x. PMID 7655573.
- Hemolytic Disease of Newborn~workup at eMedicine
- Arora, Satyam; Doda, Veena; Maria, Arti; Kotwal, Urvershi; Goyal, Saurabh (2015). "Maternal anti-M induced hemolytic disease of newborn followed by prolonged anemia in newborn twins". Asian Journal of Transfusion Science. 9 (1): 98–101. doi:10.4103/0973-6247.150968. PMC 4339947. PMID 25722586.
- Van Wamelen, D J.; Klumper, F J.; De Haas, M; Meerman, R H.; Van Kamp, I L.; Oepkes, D (2007). "Obstetric History and Antibody Titer in Estimating Severity of Kell Alloimmunization in Pregnancy". Obstetrics & Gynecology. 109 (5): 1093–8. doi:10.1097/01.AOG.0000260957.77090.4e. PMID 17470588. S2CID 24848319.
- Gowri, Vaidyanathan; Al-Dughaishi, Tamima; Al-Rubkhi, Ikhlasss; Al-Duhli, Maymoona; Al-Harrasi, Yusra (2015). "Alloimmunization due to red cell antibodies in Rhesus positive Omani Pregnant Women: Maternal and Perinatal outcome". Asian Journal of Transfusion Science. 9 (2): 150–4. doi:10.4103/0973-6247.162710. PMC 4562135. PMID 26420934.
- Vaughan, Janet I.; Manning, Monica; Warwick, Ruth M.; Letsky, Elizabeth A.; Murray, Neil A.; Roberts, Irene A.G. (1998). "Inhibition of Erythroid Progenitor Cells by Anti-Kell Antibodies in Fetal Alloimmune Anemia". New England Journal of Medicine. 338 (12): 798–803. doi:10.1056/NEJM199803193381204. PMID 9504940.
- "Kell sensitization can cause fetal anemia, too". Contemporary OB/GYN. UBM Medica. 1 September 2008. Retrieved 23 May 2018.
- Qun Lu, MD (5 February 2009), Kidd Blood Group System (PDF), Los Angeles, California: Department of Pathology and Laboratory Medicine, University of California, Los Angeles, School of Medicine, retrieved 23 May 2018
- Dean, L. (2005). "Chapter 10: The Kidd blood group". Blood Groups and Red Cell Antigens. Bethesda, Maryland: National Center for Biotechnology Information. Retrieved 23 May 2018.
- Moran, P.; Robson, S. C.; Reid, M. M. (2000). "Anti-E in pregnancy". BJOG. 107 (11): 208–11. doi:10.1111/j.1471-0528.2000.tb11662.x. PMID 11117776.
- De Haas, M.; Thurik, F. F.; Koelewijn, J.M.; Van Der Schoot, C.E. (2015). "Haemolytic disease of the fetus and newborn". Vox Sanguinis. 109 (2): 99–113. doi:10.1111/vox.12265. PMID 25899660.
- Voto, L. S.; Mathet, E. R.; Zapaterio, J. L.; Orti, J; Lede, R. L.; Margulies, M (1997). "High-dose gammaglobulin (IVIG) followed by intrauterine transfusions (IUTs): A new alternative for the treatment of severe fetal hemolytic disease". Journal of Perinatal Medicine. 25 (1): 85–8. doi:10.1515/jpme.1997.25.1.85. PMID 9085208. S2CID 22822621.
- Novak, Deborah J.; Tyler, Lisa N.; Reddy, Ramakrishna L.; Barsoom, Michael J. (2008). "Plasmapheresis and intravenous immune globulin for the treatment of D alloimmunization in pregnancy". Journal of Clinical Apheresis. 23 (6): 183–5. doi:10.1002/jca.20180. PMID 19003884.
- Palfi, Miodrag; Hildén, Jan-Olof; Matthiesen, Leif; Selbing, Anders; Berlin, Gösta (2006). "A case of severe Rh (D) alloimmunization treated by intensive plasma exchange and high-dose intravenous immunoglobulin". Transfusion and Apheresis Science. 35 (2): 131–6. doi:10.1016/j.transci.2006.07.002. PMID 17045529.
- Ruma, Michael S.; Moise, Kenneth J.; Kim, Eunhee; Murtha, Amy P.; Prutsman, Wendy J.; Hassan, Sonia S.; Lubarsky, Suzanne L. (2007). "Combined plasmapheresis and intravenous immune globulin for the treatment of severe maternal red cell alloimmunization". American Journal of Obstetrics and Gynecology. 196 (2): 138.e1–6. doi:10.1016/j.ajog.2006.10.890. PMID 17306655.
- Deka, Dipika (2016). "Intrauterine Transfusion". Journal of Fetal Medicine. 27 (3): 13–17. doi:10.1007/s40556-016-0072-4. PMID 26811110. S2CID 42005756.
- Erythrocyte Alloimmunization and Pregnancy at eMedicine
- Moise Jr, Kenneth J (15 March 2018). "Intrauterine fetal transfusion of red cells". UpToDate. UpToDate, Inc. Retrieved 31 March 2018.
- Hemolytic Disease of Newborn~treatment at eMedicine
- UNC Detection & Prevention: Isoimmunization Protocol (PDF), University of North Carolina, School of Medicine at Chapel Hill, October 2001, retrieved 23 May 2018
- Rimon, E.; Peltz, R.; Gamzu, R.; Yagel, S.; Feldman, B.; Chayen, B.; Achiron, R.; Lipitz, S. (2006). "Management of Kell isoimmunization — evaluation of a Doppler-guided approach". Ultrasound in Obstetrics and Gynecology. 28 (6): 814–20. doi:10.1002/uog.2837. PMID 16941575.
- "Hemolytic Disease of the Newborn" (PDF), Intensive Care Nursery House Staff Manual, Children's Hospital at University of California, San Francisco, Medical Center, pp. 121–124, retrieved 23 May 2018
- American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. (2004). "Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation". Pediatrics. 114 (1): 297–316. doi:10.1542/peds.114.1.297. PMID 15231951.
- Onesimo, Roberta; Rizzo, Daniela; Ruggiero, Antonio; Valentini, Piero (2010). "Intravenous Immunoglobulin therapy for anti-E hemolytic disease in the newborn". The Journal of Maternal-Fetal & Neonatal Medicine. 23 (9): 1059–61. doi:10.3109/14767050903544751. PMID 20092394. S2CID 25144401.
- Gottstein, R (2003). "Systematic review of intravenous immunoglobulin in haemolytic disease of the newborn". Archives of Disease in Childhood: Fetal and Neonatal Edition. 88 (1): F6–10. doi:10.1136/fn.88.1.F6. PMC 1755998. PMID 12496219.
- Hemolytic Disease of Newborn~followup at eMedicine
- Strobel, Erwin (2008). "Hemolytic Transfusion Reactions". Transfusion Medicine and Hemotherapy. 35 (5): 346–353. doi:10.1159/000154811. PMC 3076326. PMID 21512623.
- Transfusion Reactions at eMedicine
- "Fatalities Reported to FDA Following Blood Collection and Transfusion: Annual Summary for Fiscal Year 2011", Vaccines, Blood & Biologics, U.S. Food and Drug Administration, 8 May 2012, archived from the original on 11 November 2012
Further reading
- Geifmanholtzman, O; Wojtowycz, M; Kosmas, E; Artal, R (1997). "Female alloimmunization with antibodies known to cause hemolytic disease". Obstetrics & Gynecology. 89 (2): 272–5. doi:10.1016/S0029-7844(96)00434-6. PMID 9015034. S2CID 36953155.
- Mollison, PL; Engelfriet CP; Contreras M (1997). Blood Transfusion in Clinical Medicine (10th ed.). Oxford, UK: Blackwell Science. ISBN 978-0-86542-881-2.
- Blood Groups and Red Blood Cell Antigens: Hemolytic disease of the newborn
External links
| Classification | |
|---|---|
| External resources |