Rh blood group system
The Rh blood group system is a human blood group system. It is the second most important blood group system, after the ABO blood group system. The Rh blood group system consists of 49 defined blood group antigens,[1] among which the five antigens D, C, c, E, and e are the most important. There is no d antigen. Rh(D) status of an individual is normally described with a positive or negative suffix after the ABO type (e.g., someone who is A Positive has the A antigen and the Rh(D) antigen, whereas someone who is A Negative lacks the Rh(D) antigen). The terms Rh factor, Rh positive, and Rh negative refer to the Rh(D) antigen only. Antibodies to Rh antigens can be involved in hemolytic transfusion reactions and antibodies to the Rh(D) and Rh antigens confer significant risk of hemolytic disease of the fetus and newborn.
The term "Rh" was originally an abbreviation of "Rhesus factor." It was discovered in 1937 by Karl Landsteiner and Alexander S. Wiener, who, at the time, believed it to be a similar antigen found in rhesus macaque red blood cells. It was subsequently learned the human factor is not identical to the rhesus monkey factor, but by then, "Rhesus Group" and like terms were already in widespread, worldwide use. Thus, notwithstanding it is a misnomer, the term survives (e.g., rhesus blood group system and the obsolete terms rhesus factor, rhesus positive, and rhesus negative – all three of which actually refer specifically and only to the Rh D factor and are thus misleading when unmodified). Contemporary practice is to use "Rh" as a term of art instead of "Rhesus" (e.g., "Rh Group," "Rh factors," "Rh D," etc.).
The significance of their discovery was not immediately apparent and was only realized in 1940, after subsequent findings by Philip Levine and Rufus Stetson.[2] The serum that led to the discovery was produced by immunizing rabbits with red blood cells from a rhesus macaque. The antigen that induced this immunization was designated by them as Rh factor to indicate that rhesus blood had been used for the production of the serum.[3]
In 1939, Phillip Levine and Rufus Stetson published in a first case report the clinical consequences of non-recognized Rh factor, hemolytic transfusion reaction, and hemolytic disease of the newborn in its most severe form.[4] It was recognized that the serum of the reported woman agglutinated with red blood cells of about 80% of the people although the then known blood groups, in particular ABO were matched. No name was given to this agglutinin when described. In 1940, Karl Landsteiner and Alexander S. Wiener made the connection to their earlier discovery, reporting a serum that also reacted with about 85% of different human red blood cells.[5]
In 1941, Group O: a patient of Dr. Paul in Irvington, NJ, delivered a normal infant in 1931:[6] this pregnancy was followed by a long period of sterility. The second pregnancy (April, 1941) resulted in an infant suffering icterus gravis.[7] In May 1941, the third anti-Rh serum (M.S.) of Group O became available.[8]
Based on the serologic similarities, Rh factor was later also used for antigens, and anti-Rh for antibodies, found in humans such as those previously described by Levine and Stetson. Although differences between these two sera were shown already in 1942 and clearly demonstrated in 1963, the already widely used term "Rh" was kept for the clinically described human antibodies which are different from the ones related to the rhesus monkey. This real factor found in rhesus macaque was classified in the Landsteiner–Wiener antigen system (antigen LW, antibody anti-LW) in honor of the discoverers.[9][10]
It was recognized that the Rh factor was just one in a system of various antigens. Based on different models of genetic inheritance, two different terminologies were developed; both of them are still in use.
The clinical significance of this highly immunizing D antigen (i.e., Rh factor) was soon realized. Some keystones were to recognize its importance for blood transfusion (including reliable diagnostic tests), hemolytic disease of the newborn (including exchange transfusion), and very importantly the prevention of it by screening and prophylaxis.
The discovery of fetal cell-free DNA in maternal circulation by Holzgrieve et al. led to the noninvasive genotyping of fetal Rh genes in many countries.
Nomenclature
| Fisher–Race | Wiener |
|---|---|
| Dce | R0 |
| DCe | R1 |
| DcE | R2 |
| DCE | RZ |
| d |
The Rh blood group system has two sets of nomenclatures: one developed by Ronald Fisher and R. R. Race, the other by Wiener. Both systems reflected alternative theories of inheritance. The Fisher–Race system, which is more commonly in use today, uses the CDE nomenclature. This system was based on the theory that a separate gene controls the product of each corresponding antigen (e.g., a "D gene" produces D antigen, and so on). However, the d gene was hypothetical, not actual.
The Wiener system used the Rh–Hr nomenclature. This system was based on the theory that there was one gene at a single locus on each of the 2 copies of chromosome 1, each contributing to production of multiple antigens. In this theory, a gene R1 is supposed to give rise to the “blood factors” Rh0, rh′, and rh″ (corresponding to modern nomenclature of the D, C, and E antigens) and the gene r to produce hr′ and hr″ (corresponding to modern nomenclature of the c and e antigens).[11]
Notations of the two theories are used interchangeably in blood banking (e.g., Rho(D) meaning RhD positive). Wiener's notation is more complex and cumbersome for routine use. Because it is simpler to explain, the Fisher–Race theory has become more widely used.
DNA testing has shown that both are partially correct. There are in fact two linked genes, the RHD gene which produces a single immune specificity (anti-D) and the RHCE gene with multiple specificities (anti-C, anti-c, anti-E, anti-e). Thus, Wiener's postulate that a gene could have multiple specificities (something many did not give credence to originally) has been proved to be correct. On the other hand, Wiener's theory that there is only one gene has proved to be incorrect, as has the Fischer–Race theory that there are three genes, rather than the 2. The CDE notation used in the Fisher–Race nomenclature is sometimes rearranged to DCE to more accurately represent the co-location of the C and E encoding on the RhCE gene, and to make interpretation easier.
Antigens
The proteins which carry the Rh antigens are transmembrane proteins, whose structure suggest that they are ion channels.[12] The main antigens are D, C, E, c and e, which are encoded by two adjacent gene loci, the RHD gene which encodes the RhD protein with the D antigen (and variants)[13] and the RHCE gene which encodes the RhCE protein with the C, E, c and e antigens (and variants).[14] There is no d antigen. Lowercase "d" indicates the absence of the D antigen (the gene is usually deleted or otherwise nonfunctional).
Rh phenotypes are readily identified through the presence or absence of the Rh surface antigens. As can be seen in the table below, most of the Rh phenotypes can be produced by several different Rh genotypes. The exact genotype of any individual can only be identified by DNA analysis. Regarding patient treatment, only the phenotype is usually of any clinical significance to ensure a patient is not exposed to an antigen they are likely to develop antibodies against. A probable genotype may be speculated on, based on the statistical distributions of genotypes in the patient's place of origin.
R0 (cDe or Dce) is today most common in Africa. The allele was thus often assumed in early blood group analyses to have been typical of populations on the continent; particularly in areas below the Sahara. Ottensooser et al. (1963) suggested that high R0 frequencies were likely characteristic of the ancient Judea Jews, who had emigrated from Egypt prior to their dispersal throughout the Mediterranean Basin and Europe[15] on the basis of high R0 percentages among Sephardi and Ashkenazi Jews compared to native European populations and the relative genetic isolation of Ashkenazim. However, more recent studies have found R0 frequencies as low as 24.3% among some Afroasiatic-speaking groups in the Horn of Africa,[16] as well as higher R0 frequencies among certain other Afroasiatic speakers in North Africa (37.3%)[17] and among some Palestinians in the Levant (30.4%).[18]
| Phenotype expressed on cell | Genotype expressed in DNA | Prevalence (%) † | |
|---|---|---|---|
| Fisher–Race notation | Wiener notation | ||
| D+ C+ E+ c+ e+ (RhD+) | Dce/DCE | R0RZ | 0.0125 |
| Dce/dCE | R0rY | 0.0003 | |
| DCe/DcE | R1R2 | 11.8648 | |
| DCe/dcE | R1r″ | 0.9992 | |
| DcE/dCe | R2r′ | 0.2775 | |
| DCE/dce | RZr | 0.1893 | |
| D+ C+ E+ c+ e− (RhD+) | DcE/DCE | R2RZ | 0.0687 |
| DcE/dCE | R2rY | 0.0014 | |
| DCE/dcE | RZr″ | 0.0058 | |
| D+ C+ E+ c− e+ (RhD+) | DCe/dCE | R1rY | 0.0042 |
| DCE/dCe | RZr′ | 0.0048 | |
| DCe/DCE | R1RZ | 0.2048 | |
| D+ C+ E+ c− e− (RhD+) | DCE/DCE | RZRZ | 0.0006 |
| DCE/dCE | RZrY | < 0.0001 | |
| D+ C+ E− c+ e+ (RhD+) | Dce/dCe | R0r′ | 0.0505 |
| DCe/dce | R1r | 32.6808 | |
| DCe/Dce | R1R0 | 2.1586 | |
| D+ C+ E− c− e+ (RhD+) | DCe/DCe | R1R1 | 17.6803 |
| DCe/dCe | R1r′ | 0.8270 | |
| D+ C− E+ c+ e+ (RhD+) | DcE/Dce | R2R0 | 0.7243 |
| Dce/dcE | R0r″ | 0.0610 | |
| DcE/dce | R2r | 10.9657 | |
| D+ C− E+ c+ e− (RhD+) | DcE/DcE | R2R2 | 1.9906 |
| DcE/dcE | R2r″ | 0.3353 | |
| D+ C− E− c+ e+ (RhD+) | Dce/Dce | R0R0 | 0.0659 |
| Dce/dce | R0r | 1.9950 | |
| D− C+ E+ c+ e+ (RhD−) | dce/dCE | rrY | 0.0039 |
| dCe/dcE | r′r″ | 0.0234 | |
| D− C+ E+ c+ e− (RhD−) | dcE/dCE | r″rY | 0.0001 |
| D− C+ E+ c− e+ (RhD−) | dCe/dCE | r′rY | 0.0001 |
| D− C+ E+ c− e− (RhD−) | dCE/dCE | rYrY | < 0.0001 |
| D− C+ E− c+ e+ (RhD−) | dce/dCe | rr′ | 0.7644 |
| D− C+ E− c− e+ (RhD−) | dCe/dCe | r′r′ | 0.0097 |
| D− C− E+ c+ e+ (RhD−) | dce/dcE | rr″ | 0.9235 |
| D− C− E+ c+ e− (RhD−) | dcE/dcE | r″r″ | 0.0141 |
| D− C− E− c+ e+ (RhD−) | dce/dce | rr | 15.1020 |
† Figures taken from a study performed in 1948 on a sample of 2000 people in the United Kingdom.[19]
| Rh Phenotype | CDE | Patients (%) | Donors (%) |
|---|---|---|---|
| R1r | CcDe | 37.4 | 33.0 |
| R1R2 | CcDEe | 35.7 | 30.5 |
| R1R1 | CDe | 5.7 | 21.8 |
| rr | ce | 10.3 | 11.6 |
| R2r | cDEe | 6.6 | 10.4 |
| R0R0 | cDe | 2.8 | 2.7 |
| R2R2 | cDE | 2.8 | 2.4 |
| rr″ | cEe | – | 0.98 |
| RZRZ | CDE | – | 0.03 |
| rr′ | Cce | 0.8 | – |
Hemolytic disease of the newborn
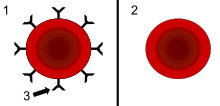
The hemolytic condition occurs when there is an incompatibility between the blood types of the mother and fetus. There is also potential incompatibility if the mother is Rh negative and the father is positive. When any incompatibility is detected, the mother often receives an injection at 28 weeks gestation and at birth to avoid the development of antibodies towards the fetus. These terms do not indicate which specific antigen-antibody incompatibility is implicated. The disorder in the fetus due to Rh D incompatibility is known as erythroblastosis fetalis.
- Hemolytic comes from two words: "hema" (blood) and "lysis" (solution) or breaking down of red blood cells
- Erythroblastosis refers to the making of immature red blood cells
- Fetalis refers to the fetus.
When the condition is caused by the Rh D antigen-antibody incompatibility, it is called Rh D Hemolytic disease of the newborn or Rh disease. Here, sensitization to Rh D antigens (usually by feto-maternal transfusion during pregnancy) may lead to the production of maternal IgG anti-D antibodies which can pass through the placenta. This is of particular importance to D negative females at or below childbearing age, because any subsequent pregnancy may be affected by the Rh D hemolytic disease of the newborn if the baby is D positive. The vast majority of Rh disease is preventable in modern antenatal care by injections of IgG anti-D antibodies (Rho(D) Immune Globulin). The incidence of Rh disease is mathematically related to the frequency of D negative individuals in a population, so Rh disease is rare in old-stock populations of Africa and the eastern half of Asia, and the Indigenous peoples of Oceania and the Americas, but more common in other genetic groups, most especially Western Europeans, but also other West Eurasians, and to a lesser degree, native Siberians, as well as those of mixed-race with a significant or dominant descent from those (e.g. the vast majority of Latin Americans and Central Asians).
- Symptoms and signs in the fetus:
- Enlarged liver, spleen, or heart and fluid buildup in the fetus' abdomen seen via ultrasound.
- Symptoms and signs in the newborn:
- Anemia that creates the newborn's pallor (pale appearance).
- Jaundice or yellow discoloration of the newborn's skin, sclera or mucous membrane. This may be evident right after birth or after 24–48 hours after birth. This is caused by bilirubin (one of the end products of red blood cell destruction).
- Enlargement of the newborn's liver and spleen.
- The newborn may have severe edema of the entire body.
- Dyspnea or difficulty breathing.
Population data
According to a comprehensive study, the worldwide frequency of Rh-positive and Rh-negative blood types is approximately 94% and 6%, respectively. The same study concluded that the share of the population with Rh-negative blood type is set to fall further in the future primarily due to low population growth in Europe.[21] The frequency of Rh factor blood types and the RhD neg allele gene differs in various populations.
| Population | Rh(D) Neg | Rh(D) Pos | Rh(D) Neg alleles |
|---|---|---|---|
| African Americans | ∼ 7% | 93% | ∼ 26% |
| Albania[23] | 10.86% | 89% | weak D 1.4% |
| Basques[24] | 21%–36% | 65% | ∼ 60% |
| Britain[25] | 17% | 83% | |
| China[25] | < 1% | > 99% | |
| Ethiopians[25] | 1%–21% | 99%–79% | |
| Europeans (others) | 16% | 84% | 40% |
| India[25] | 0.6%–8.4% | 99.4%–91.6% | |
| Indonesia[25] | < 1% | > 99% | |
| Japan[25] | < 1% | > 99% | |
| Koreans[26] | < 1% | > 99% | |
| Madagascar[25] | 1% | 99% | |
| Moroccans[27] | 9.5% | 90.5% | |
| Moroccans (High Atlas)[28] | ∼ 29% | 71% | |
| Native Americans | ∼ 1% | 99% | ∼ 10% |
| Nigeria[29] | 6% | 94% | |
| Saudi Arabia[30] | 8.8% | 91.2% | 29.5% |
| Subequatorial Africa[25] | 1%–3% | 99%–97% | |
| United States[25] | 15% | 85% | |
Inheritance
If both of a child's parents are Rh negative, the child will definitely be Rh negative. Otherwise the child may be Rh positive or Rh negative, depending on the parents' specific genotypes.[31]
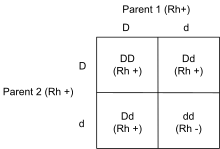
The D antigen is inherited as one gene (RHD) (on the short arm of the first chromosome, p36.13–p34.3) with various alleles. Though very much simplified, one can think of alleles that are positive or negative for the D antigen. The gene codes for the RhD protein on the red cell membrane. D− individuals who lack a functional RHD gene do not produce the D antigen, and may be immunized by D+ blood.
The epitopes for the next 4 most common Rh antigens, C, c, E and e are expressed on the highly similar RhCE protein that is genetically encoded in the RHCE gene, also found on chromosome 1. It has been shown that the RHD gene arose by duplication of the RHCE gene during primate evolution. Mice have just one RH gene.[32]
The RHAG gene, which is responsible for encoding Rh-associated glycoprotein (RhAG), is found on chromosome 6a.
The polypeptides produced from the RHD and RHCE genes form a complex on the red blood cell membrane with the Rh-associated glycoprotein.[33]
Function
On the basis of structural homology it has been proposed that the product of RHD gene, the RhD protein, is a membrane transport protein of uncertain specificity (CO2 or NH3) and unknown physiological role.[34][35] The three-dimensional structure of the related RHCG protein and biochemical analysis of the RhD protein complex indicates that the RhD protein is one of three subunits of an ammonia transporter.[36][37] Three recent studies[38][39][40] have reported a protective effect of the RhD-positive phenotype, especially RhD heterozygosity, against the negative effect of latent toxoplasmosis on psychomotor performance in infected subjects. RhD-negative compared to RhD-positive subjects without anamnestic titres of anti-Toxoplasma antibodies have shorter reaction times in tests of simple reaction times. And conversely, RhD-negative subjects with anamnestic titres (i.e. with latent toxoplasmosis) exhibited much longer reaction times than their RhD-positive counterparts. The published data suggested that only the protection of RhD-positive heterozygotes was long term in nature; the protection of RhD-positive homozygotes decreased with duration of the infection while the performance of RhD-negative homozygotes decreased immediately after the infection. The overall change in reaction times was always larger in the RhD-negative group than in the RhD-positive.
Origin of RHD polymorphism
For a long time, the origin of RHD polymorphism was an evolutionary enigma.[41][42][43] Before the advent of modern medicine, the carriers of the rarer allele (e.g. RhD-negative women in a population of RhD positives or RhD-positive men in a population of RhD negatives) were at a disadvantage as some of their children (RhD-positive children born to preimmunised RhD-negative mothers) were at a higher risk of fetal or newborn death or health impairment from hemolytic disease. It was suggested that higher tolerance of RhD-positive heterozygotes against Toxoplasma-induced impairment of reaction time [38][39] and Toxoplasma-induced increase of risk of traffic accident[40] could counterbalance the disadvantage of the rarer allele and could be responsible both for the initial spread of the RhD allele among the RhD-negative population and for a stable RhD polymorphism in most human populations. It was also suggested that differences in the prevalence of Toxoplasma infection between geographical regions (0–95%) could also explain the striking variation in the frequency of RhD-negative alleles between populations. According to some parasitologists,[38] it is possible that the better psychomotor performance of RhD-negative subjects in the Toxoplasma-free population could be the reason for spreading of the “d allele” (deletion) in the European population. In contrast to the situation in Africa and certain (but not all) regions of Asia, the abundance of wild cats (definitive hosts of Toxoplasma gondii) in Europe was very low before the advent of the domestic cat.
Weak D
In serologic testing, D positive blood is easily identified. Units that are D negative are often retested to rule out a weaker reaction. This was previously referred to as Du, which has been replaced.[44]:322 By definition, weak D phenotype is characterized by negative reaction with anti-D reagent at immediate spin (IS), negative reaction after 37 °C incubation, and positive reaction at anti-human globulin (AHG) phase. Weak D phenotype can occur in several ways. In some cases, this phenotype occurs because of an altered surface protein that is more common in people of European descent. An inheritable form also occurs, as a result of a weakened form of the R0 gene. Weak D may also occur as "C in trans", whereby a C gene is present on the opposite chromosome to a D gene (as in the combination R0r', or "Dce/dCe"). The testing is difficult, since using different anti-D reagents, especially the older polyclonal reagents, may give different results.
The practical implication of this is that people with this sub-phenotype will have a product labeled as "D positive" when donating blood. When receiving blood, they are sometimes typed as a "D negative", though this is the subject of some debate. Most "Weak D" patients can receive "D positive" blood without complications.[44]:323 However, it is important to correctly identify the ones that have to be considered D+ or D−. This is important, since most blood banks have a limited supply of "D negative" blood and the correct transfusion is clinically relevant. In this respect, genotyping of blood groups has much simplified this detection of the various variants in the Rh blood group system.
Partial D
It is important to differentiate weak D (due to a quantitative difference in the D antigen) from partial D (due to a qualitative difference in the D antigen). Simply put, the weak D phenotype is due to a reduced number of D antigens on a red blood cell. In contrast, the partial D phenotype is due to an alteration in D-epitopes. Thus, in partial D, the number of D antigens is not reduced but the protein structure is altered. These individuals, if alloimmunized to D, can produce an anti-D antibody. Therefore, partial D patients who are donating blood should be labeled as D-positive but, if receiving blood, they should be labeled as D-negative and receive D-negative units.[33]
In the past, partial D was called 'D mosaic' or 'D variant.' Different partial D phenotypes are defined by different D epitopes on the outer surface of the red blood cell membrane. More than 30 different partial D phenotypes have been described.[33]
Rhnull phenotype
Rhnull individuals have no Rh antigens (no Rh or RhAG) on their red blood cells.[45] This rare condition[45] has been called "Golden Blood".[46] As a consequence of Rh antigen absence, Rhnull red blood cells also lack LW and Fy5 and show weak expression of S, s, and U antigens. Red blood cells lacking Rh/RhAG proteins have structural abnormalities (such as stomatocytosis) and cell membrane defects that can result in hemolytic anemia.[33][45] Only 43 individuals have been reported to have it worldwide. The last reported carrier is a Pakistani girl named Ranam Rao. Only 9 active donors have been reported.[46] Its properties make it attractive in numerous medical applications, but scarcity makes it expensive to transport and acquire.[47]
Other Rh group antigens
Currently, 50 antigens have been described in the Rh group system; among those described here, the D, C, c, E and e antigens are the most important. The others are much less frequently encountered or are rarely clinically significant. Each is given a number, though the highest assigned number (CEST or RH57 according to the ISBT terminology) is not an accurate reflection of the antigens encountered since many (e.g. Rh38) have been combined, reassigned to other groups, or otherwise removed.[44]:324
Rh antibodies
Rh antibodies are IgG antibodies which are acquired through exposure to Rh-positive blood (generally either through pregnancy or transfusion of blood products). The D antigen is the most immunogenic of all the non-ABO antigens. Approximately 80% of individuals who are D-negative and exposed to a single D-positive unit will produce an anti-D antibody. The percentage of alloimmunization is significantly reduced in patients who are actively exsanguinating.[48]
All Rh antibodies except D display dosage (antibody reacts more strongly with red cells homozygous for an antigen than cells heterozygous for the antigen (EE stronger reaction vs Ee).
If anti-E is detected, the presence of anti-c should be strongly suspected (due to combined genetic inheritance). It is therefore common to select c-negative and E-negative blood for transfusion patients who have an anti-E. Anti-c is a common cause of delayed hemolytic transfusion reactions.[33]
References
- Dean, Laura. Blood Groups and Red Cell Antigens [Internet].. Bethesda (MD): National Center for Biotechnology Information (US); 2005, Chapter. 7.
- Landsteiner, K.; Weiner, A. (1940). "An Agglutinable Factor in Human Blood Recognized by Immune Sera for Rhesus Blood". Exp Biol Med (Maywood). 43 (1): 223. doi:10.3181/00379727-43-11151.
- Landsteiner K, Wiener AS (1941). "Studies on an agglutinogen (Rh) in human blood reacting with anti-rhesus sera and with human isoantibodies". J Exp Med. 74 (4): 309–320. doi:10.1084/jem.74.4.309. PMC 2135190. PMID 19871137.
- Levine P, Stetson RE (1939). "An unusual case of intragroup agglutination". JAMA. 113 (2): 126–7. doi:10.1001/jama.1939.72800270002007a.
- Landsteiner K, Wiener AS (1940). "An agglutinable factor in human blood recognized by immune sera for rhesus blood". Proc Soc Exp Biol Med. 43: 223–4. doi:10.3181/00379727-43-11151.
- "Rev Bernard Charles "Bernie" Schlegel (1930-1991)..." www.findagrave.com. Retrieved 2018-05-17.
- Levine, Philip; Burnham, Lyman; Katzin, E.M.; Vogel, Peter (December 1941). "The role of iso-immunization in the pathogenesis of erythroblastosis fetalis". American Journal of Obstetrics and Gynecology. 42 (6): 925–937. doi:10.1016/S0002-9378(41)90260-0. ISSN 0002-9378.
- Levine, Philip; Burnham, Lyman; Katzin, E.M.; Vogel, Peter (December 1941). "The role of iso-immunization in the pathogenesis of erythroblastosis fetalis". American Journal of Obstetrics and Gynecology. 42 (6): 925–937. doi:10.1016/S0002-9378(41)90260-0. ISSN 0002-9378.
- Avent ND, Reid ME (2000). "The Rh blood group system: a review". Blood. 95 (2): 375–387. doi:10.1182/blood.V95.2.375. PMID 10627438.
- Scott ML (2004). "The complexities of the Rh system". Vox Sang. 87 (Suppl. 1): S58–S62. doi:10.1111/j.1741-6892.2004.00431.x. PMID 15200606.
- Weiner, Alexander S. (1 February 1949). "Genetics and Nomenclature of the Rh–Hr Blood Types". Antonie van Leeuwenhoek. 15 (1): 17–28. doi:10.1007/BF02062626. ISSN 0003-6072.
- "dbRBC – Blood Group Antigen Gene Mutation Database". www.ncbi.nlm.nih.gov. Archived from the original on 2011-02-13. Retrieved 2010-06-15.
- "RHD Rh blood group, D antigen [Homo sapiens] – Gene Result". nlm.nih.gov. Retrieved 2010-06-15.
- "RHCE Rh blood group, CcEe antigens [Homo sapiens] – Gene Result". nlm.nih.gov. Archived from the original on 2010-03-20. Retrieved 2010-06-15.
- Ottensooser, F.; et al. (1963). "Blood groups of a population of Ashkenazi Jews in Brazil". American Journal of Physical Anthropology. 21 (1): 41–48. doi:10.1002/ajpa.1330210106. PMID 13940710. Retrieved 29 August 2017.
- Harrison, Geoffrey Ainsworth; et al. (1969). "The effects of altitudinal variation in Ethiopian populations". Philosophical Transactions of the Royal Society of London B: Biological Sciences. 256 (805): 147–182. Bibcode:1969RSPTB.256..147H. doi:10.1098/rstb.1969.0040.
- Ammaria Aouar Metri; et al. (2012). "A genetic study of nine populations from the region of Tlemcen in Western Algeria: a comparative analysis on the Mediterranean scale". Anthropological Science. 120 (3): 209–216. doi:10.1537/ase.120618. Archived from the original on 29 August 2017. Retrieved 28 August 2017.
- Skaik, Younis Abed El-Wahhab (July–December 2011). "The Rh allele frequencies in Gaza city in Palestine". Asian Journal of Transfusion Science. 5 (2): 150–152. doi:10.4103/0973-6247.83241. PMC 3159245. PMID 21897594.
- Race RR, Mourant AE (1948). "The Rh Chromosome Frequencies in England" (PDF). Blood. 3 (6): 689–695. doi:10.1182/blood.V3.6.689.689. PMID 18860341. Retrieved 2010-11-14.
- Canatan, Duran; Nilgün Acar; Banu Kiliç (1999). "Rh Subgroups and Kell Antigens in Patients With Thalassemia and in Donors in Turkey" (PDF). Turkish Journal of Medical Sciences. 29: 155–7. Archived from the original (PDF) on 2008-12-17. Retrieved 2008-10-17.
- "Blood Type Frequencies by Country including the Rh Factor – Rhesus Negative".
- Mack, Steve (March 21, 2001). "Re: Is the RH negative blood type more prevalent in certain ethnic groups?". MadSci Network. Archived from the original on February 24, 2011.
- Xhetani M, et al. (June 2014). "Distribution of Rhesus blood group antigens and weak D alleles in the population of Albania = Blood Transfusion Journal". Blood Transfusion. 12 (4): 565–569. doi:10.2450/2014.0240-13. PMC 4212038. PMID 24960662.
- Touinssi M, Chiaroni J, Degioanni A, De Micco P, Dutour O, Bauduer F (2004). "Distribution of rhesus blood group system in the French basques: a reappraisal using the allele-specific primers PCR method". Human Heredity. 58 (2): 69–72. doi:10.1159/000083027. PMID 15711086.
- Golassa, Lemu; et al. (2017). "High rhesus (Rh (D)) negative frequency and ethnic-group based ABO blood group distribution in Ethiopia". BMC Research Notes. 10 (1): 330. doi:10.1186/s13104-017-2644-3. PMC 5530478. PMID 28747227.
- Kim, Ji Yeon; Kim, Sung Yeun; Kim, Chong-Ahm; Yon, Gyu Sung; Park, Sung Sup (March 4, 2005). "Molecular characterization of D– Korean persons: development of a diagnostic strategy". Transfusion. 45 (3): 345–352. doi:10.1111/j.1537-2995.2005.04311.x. PMID 15752151.
- EL Wafi, M; EL Housse, H; Nourichafi, N; Bouisk, K; Benajiba, M; Habti, N (2016). "Prevalence of weak D phenotype among D negative C/E+ blood donors in Morocco" (PDF). International Journal of Blood Transfusion and Immunohematolology. 6 (1): 3–7. doi:10.5348/ijbti-2016-22-OA-2 (inactive 2020-01-25). Archived (PDF) from the original on August 28, 2016. Retrieved February 3, 2018.
- Weinstock, Christof (January 2014). "It is worthwhile filling in the remaining blank spots for blood group antigen frequencies". Blood Transfusion. 12 (1): 3–6. doi:10.2450/2013.0192-13. PMC 3926725. PMID 24120599.
- Enosolease ME, Bazuaye GN (January 2008). "Distribution of ABO and Rh-D blood groups in the Benin area of Niger-Delta: Implication for regional blood transfusion". Asian Journal of Transfusion Science. 2 (1): 3–5. doi:10.4103/0973-6247.39502. PMC 2798756. PMID 20041069.
- Eweidah, M. H.; Rahiman, S.; Ali, M. D. H.; Al-Shamary, A. M. D. (April 2011). "Distribution of ABO and Rhesus (RHD) Blood Groups in Al-Jouf Province of the Saudi Arabia" (PDF). The Anthropologist. 13 (2): 99–102. doi:10.1080/09720073.2011.11891182. Archived (PDF) from the original on January 2, 2013. Retrieved February 3, 2018.
- "ABO inheritance patterns". Inheritance patterns of blood groups. Australian Red Cross Blood Service. Archived from the original on 1 November 2013. Retrieved 30 October 2013.
- Wagner FF, Flegel WA (Mar 2002). "RHCE represents the ancestral RH position, while RHD is the duplicated gene". Blood. 99 (6): 2272–3. doi:10.1182/blood-2001-12-0153. PMID 11902138.
- Mais, DD. ASCP Quick Compendium of Clinical Pathology, 2nd Ed. Chicago, ASCP Press, 2009.
- Kustu S, Inwood W (2006). "Biological gas channels for NH3 and CO2: evidence that Rh (rhesus) proteins are CO2 channels". Transfusion Clinique et Biologique. 13 (1–2): 103–110. doi:10.1016/j.tracli.2006.03.001. PMID 16563833.
- Biver S, Scohy S, Szpirer J, Szpirer C, André B, Marini AM (2006). "Physiological role of the putative ammonium transporter RhCG in the mouse". Transfusion Clinique et Biologique. 13 (1–2): 167–8. doi:10.1016/j.tracli.2006.03.003. PMID 16564721.
- Gruswitz F, Chaudhary S, Ho JD, Schlessinger A, Pezeshki B, Ho CM, Sali A, Westhoff CM, Stroud RM (2010). "Function of human Rh based on structure of RhCG at 2.1 A". Proceedings of the National Academy of Sciences. 107 (21): 9638–9643. doi:10.1073/pnas.1003587107. PMC 2906887. PMID 20457942.
- Westhoff CM (2007). "The Structure and Function of the Rh Antigen Complex". Seminars in Hematology. 44 (1): 42–50. doi:10.1053/j.seminhematol.2006.09.010. PMC 1831834. PMID 17198846.
- Novotná M, Havlícek J, Smith AP, Kolbeková P, Skallová A, Klose J, Gasová Z, Písacka M, Sechovská M, Flegr J (2008). "Toxoplasma and reaction time: Role of toxoplasmosis in the origin, preservation and geographical distribution of Rh blood group polymorphism" (PDF). Parasitology. 135 (11): 1253–61. doi:10.1017/S003118200800485X. PMID 18752708.
- Flegr J, Novotná M, Lindová J, Havlícek J (2008). "Neurophysiological effect of the Rh factor. Protective role of the RhD molecule against Toxoplasma-induced impairment of reaction times in women" (PDF). Neuroendocrinology Letters. 29 (4): 475–481. PMID 18766148.
- Flegr J, Klose J, Novotná M, Berenreitterová M, Havlícek J (2009). "Increased incidence of traffic accidents in Toxoplasma-infected military drivers and protective effect RhD molecule revealed by a large-scale prospective cohort study". BMC Infect. Dis. 9: 72. doi:10.1186/1471-2334-9-72. PMC 2692860. PMID 19470165.
- Haldane JBF (1942). "Selection against heterozygosis in Man". Annals of Eugenics. 11: 333–340. doi:10.1111/j.1469-1809.1941.tb02297.x.
- Fisher RA, Race RR, Taylor GL (1944). "Mutation and the Rhesus reaction". Nature. 153 (3873): 106. Bibcode:1944Natur.153..106F. doi:10.1038/153106b0.
- Li CC (1953). "Is the Rh facing a crossroad? A critique of the compensation effect". Am Nat. 87 (835): 257–261. doi:10.1086/281782.
- Brecher ME (2005). Technical Manual (15th ed.). Bethesda MD: American Association of Blood Banks. ISBN 978-1-56395-196-1.
- Cartron, J.P. (December 1999). "RH blood group system and molecular basis of Rh-deficiency". Best Practice & Research Clinical Haematology. 12 (4): 655–689. doi:10.1053/beha.1999.0047. PMID 10895258.
- "Rhnull, the Rarest Blood Type on Earth, Has Been Called the "Golden Blood"". Curiosity.com. Retrieved 2019-06-05.
- Bailey, Penny. "The man with the golden blood". Mosaic Science. Mosaic. Retrieved 16 January 2019.
- Roback et al. AABB Technical Manual, 16th Ed. Bethesda, AABB Press, 2008.
External links
- Rh at BGMUT Blood Group Antigen Gene Mutation Database at NCBI, NIH
- Article commemorating the first appearance of the Rh factor in the New York Times