Fertility
Fertility is the natural capability to produce offspring. As a measure, fertility rate is the number of offspring born per mating pair, individual or population. Fertility differs from fecundity, which is defined as the potential for reproduction (influenced by gamete production, fertilization and carrying a pregnancy to term)[1] A lack of fertility is infertility while a lack of fecundity would be called sterility.
Human fertility depends on factors of nutrition, sexual behavior, consanguinity, culture, instinct, endocrinology, timing, economics, way of life, and emotions.
Demography
In demographic contexts, fertility refers to the actual production of offspring, rather than the physical capability to produce which is termed fecundity.[2][3] While fertility can be measured, fecundity cannot be. Demographers measure the fertility rate in a variety of ways, which can be broadly broken into "period" measures and "cohort" measures. "Period" measures refer to a cross-section of the population in one year. "Cohort" data on the other hand, follows the same people over a period of decades. Both period and cohort measures are widely used.[4]
Period measures
- Crude birth rate (CBR) - the number of live births in a given year per 1,000 people alive at the middle of that year. One disadvantage of this indicator is that it is influenced by the age structure of the population.
- General fertility rate (GFR) - the number of births in a year divided by the number of women aged 15–44, times 1000. It focuses on the potential mothers only, and takes the age distribution into account.
- Child-Woman Ratio (CWR) - the ratio of the number of children under 5 to the number of women 15–49, times 1000. It is especially useful in historical data as it does not require counting births. This measure is actually a hybrid, because it involves deaths as well as births. (That is, because of infant mortality some of the births are not included; and because of adult mortality, some of the women who gave birth are not counted either.)
- Coale's Index of Fertility - a special device used in historical research
Cohort measures
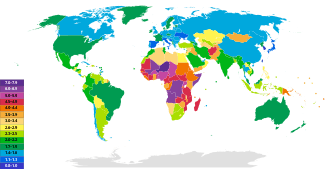
- Total fertility rate (TFR) - the total number of children a woman would bear during her lifetime if she were to experience the prevailing age-specific fertility rates of women. TFR equals the sum for all age groups of 5 times each ASFR rate.[5]
- Gross Reproduction Rate (GRR) - the number of girl babies a synthetic cohort will have. It assumes that all of the baby girls will grow up and live to at least age 50.
- Net Reproduction Rate (NRR) - the NRR starts with the GRR and adds the realistic assumption that some of the women will die before age 49; therefore they will not be alive to bear some of the potential babies that were counted in the GRR. NRR is always lower than GRR, but in countries where mortality is very low, almost all the baby girls grow up to be potential mothers, and the NRR is practically the same as GRR. In countries with high mortality, NRR can be as low as 70% of GRR. When NRR = 1.0, each generation of 1000 baby girls grows up and gives birth to exactly 1000 girls. When NRR is less than one, each generation is smaller than the previous one. When NRR is greater than 1 each generation is larger than the one before. NRR is a measure of the long-term future potential for growth, but it usually is different from the current population growth rate.
Social and economic determinants of fertility
A parent's number of children strongly correlates with the number of children that each person in the next generation will eventually have.[6] Factors generally associated with increased fertility include religiosity,[7] intention to have children,[8] and maternal support.[9] Factors generally associated with decreased fertility include wealth, education,[10] female labor participation,[11] urban residence,[12] cost of housing,[13] intelligence, increased female age and (to a lesser degree) increased male age.
The "Three-step Analysis" of the fertility process was introduced by Kingsley Davis and Judith Blake in 1956 and makes use of three proximate determinants:[14][15] The economic analysis of fertility is part of household economics, a field that has grown out of the New Home Economics. Influential economic analyses of fertility include Becker (1960),[16] Mincer (1963),[17] and Easterlin (1969).[18] The latter developed the Easterlin hypothesis to account for the Baby Boom.
Bongaarts' model of components of fertility
Bongaarts proposed a model where the total fertility rate of a population can be calculated from four proximate determinants and the total fecundity (TF). The index of marriage (Cm), the index of contraception (Cc), the index of induced abortion (Ca) and the index of postpartum infecundability (Ci). These indices range from 0 to 1. The higher the index, the higher it will make the TFR, for example a population where there are no induced abortions would have a Ca of 1, but a country where everybody used infallible contraception would have a Cc of 0.
TFR = TF × Cm × Ci × Ca × Cc
These four indices can also be used to calculate the total marital fertility (TMFR) and the total natural fertility (TN).
TFR = TMFR × Cm
TMFR = TN × Cc × Ca
TN = TF × Ci
- Intercourse
- The first step is sexual intercourse, and an examination of the average age at first intercourse, the average frequency outside marriage, and the average frequency inside.
- Conception
- Certain physical conditions may make it impossible for a woman to conceive. This is called "involuntary infecundity." If the woman has a condition making it possible, but unlikely to conceive, this is termed "subfecundity." Venereal diseases (especially gonorrhea, syphilis, and chlamydia) are common causes. Nutrition is a factor as well: women with less than 20% body fat may be subfecund, a factor of concern for athletes and people susceptible to anorexia. Demographer Ruth Frisch has argued that "It takes 50,000 calories to make a baby". There is also subfecundity in the weeks following childbirth, and this can be prolonged for a year or more through breastfeeding. A furious political debate raged in the 1980s over the ethics of baby food companies marketing infant formula in developing countries. A large industry has developed to deal with subfecundity in women and men. An equally large industry has emerged to provide contraceptive devices designed to prevent conception. Their effectiveness in use varies. On average, 85% of married couples using no contraception will have a pregnancy in one year. The rate drops to the 20% range when using withdrawal, vaginal sponges, or spermicides. (This assumes the partners never forget to use the contraceptive.) The rate drops to only 2 or 3% when using the pill or an IUD, and drops to near 0% for implants and 0% for tubal ligation (sterilization) of the woman, or a vasectomy for the man.
- Gestation
- After a fetus is conceived, it may or may not survive to birth. "Involuntary fetal mortality" involves natural abortion, miscarriages and stillbirth (a fetus born dead). Human intervention intentionally causing abortion of the fetus is called "therapeutic abortion".
Fertility biology
Women have hormonal cycles which determine when they can achieve pregnancy. The cycle is approximately twenty-eight days long, with a fertile period of five days per cycle, but can deviate greatly from this norm. Men are fertile continuously, but their sperm quality is affected by their health, frequency of ejaculation, and environmental factors.
Fertility declines with age in both sexes. In women the decline is more rapid, with complete infertility normally occurring around the age of 50.
Pregnancy rates for sexual intercourse are highest when it is done every 1 or 2 days,[19] or every 2 or 3 days.[20] Studies have shown no significant difference between different sex positions and pregnancy rate, as long as it results in ejaculation into the vagina.[21]
Menstrual cycle
A woman's menstrual cycle begins, as it has been arbitrarily assigned, with menses. Next is the follicular phase where estrogen levels build as an ovum matures (due to the follicular stimulating hormone, or FSH) within the ovary. When estrogen levels peak, it spurs a surge of luteinizing hormone (LH) which finishes the ovum and enables it to break through the ovary wall.[23] This is ovulation. During the luteal phase, which follows ovulation LH and FSH cause the post-ovulation ovary to develop into the corpus luteum which produces progesterone. The production of progesterone inhibits the LH and FSH hormones which (in a cycle without pregnancy) causes the corpus luteum to atrophy, and menses to begin the cycle again.
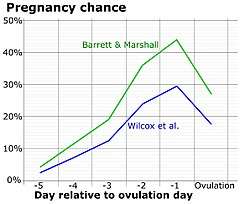
Peak fertility occurs during just a few days of the cycle: usually two days before and two days after the ovulation date.[24] This fertile window varies from woman to woman, just as the ovulation date often varies from cycle to cycle for the same woman.[25] The ovule is usually capable of being fertilized for up to 48 hours after it is released from the ovary. Sperm survive inside the uterus between 48 and 72 hours on average, with the maximum being 120 hours (5 days).
These periods and intervals are important factors for couples using the rhythm method of contraception.
Female fertility
The average age of menarche in the United States is about 12.5 years.[26] In postmenarchal girls, about 80% of the cycles are anovulatory (ovulation does not actually take place) in the first year after menarche, 50% in the third and 10% in the sixth year.[27]
Menopause occurs during a woman's midlife (between ages 48 and 55).[28][29] During menopause, hormonal production by the ovaries is reduced, eventually causing a permanent cessation of the primary function of the ovaries, particularly the creation of the uterine lining (period). This is considered the end of the fertile phase of a woman's life.
The following effects of age and female fertility have been found in women trying to get pregnant, without using fertility drugs or in vitro fertilization (data from 1670 to 1830):[30]
- At age 30
- 75% will have a conception ending in a live birth within one year
- 91% will have a conception ending in a live birth within four years.
- At age 35
- 66% will have a conception ending in a live birth within one year
- 84% will have a conception ending in a live birth within four years.
- At age 40
- 44% will have a conception ending in a live birth within one year
- 64% will have a conception ending in a live birth within four years.
Studies of actual couples trying to conceive have come up with higher results: one 2004 study of 770 European women found that 82% of 35- to 39-year-old women conceived within a year,[31] while another in 2013 of 2,820 Danish women saw 78% of 35- to 40-year-olds conceive within a year.[32]
The use of fertility drugs and/or invitro fertilization can increase the chances of becoming pregnant at a later age.[33] Successful pregnancies facilitated by fertility treatment have been documented in women as old as 67.[34] Studies since 2004 now show that mammals may continue to produce new eggs throughout their lives, rather than being born with a finite number as previously thought. Researchers at the Massachusetts General Hospital in Boston, US, say that if eggs are newly created each month in humans as well, all current theories about the aging of the female reproductive system will have to be overhauled, although at this time this is simply conjecture.[35][36]
According to the March of Dimes, "about 9 percent of recognized pregnancies for women aged 20 to 24 ended in miscarriage. The risk rose to about 20 percent at age 35 to 39, and more than 50 percent by age 42".[37] Birth defects, especially those involving chromosome number and arrangement, also increase with the age of the mother. According to the March of Dimes, "At age 25, your risk of having a baby with Down syndrome is 1 in 1,340. At age 30, your risk is 1 in 940. At age 35, your risk is 1 in 353. At age 40, your risk is 1 in 85. At age 45, your risk is 1 in 35."[38]
Male fertility
Some research suggest that increased male age is associated with a decline in semen volume, sperm motility, and sperm morphology.[39] In studies that controlled for female age, comparisons between men under 30 and men over 50 found relative decreases in pregnancy rates between 23% and 38%.[39] It is suggested that sperm count declines with age, with men aged 50–80 years producing sperm at an average rate of 75% compared with men aged 20–50 years and that larger differences are seen in how many of the seminiferous tubules in the testes contain mature sperm:[39]
- In males 20–39 years old, 90% of the seminiferous tubules contain mature sperm.
- In males 40–69 years old, 50% of the seminiferous tubules contain mature sperm.
- In males 80 years old and older, 10% of the seminiferous tubules contain mature sperm.[40]
Decline in male fertility is influenced by many factors, including lifestyle, environment and psychological factors.[41]
Some research also suggests increased risks for health problems for children of older fathers, but no clear association has been proven.[42] A large scale in Israel study suggested that the children of men 40 or older were 5.75 times more likely than children of men under 30 to have an autism spectrum disorder, controlling for year of birth, socioeconomic status, and maternal age.[43] Increased paternal age is suggested by some to directly correlate to schizophrenia but it is not proven.[44][45][46][47][48]
Australian researchers have found evidence to suggest overweight obesity may cause subtle damage to sperm and prevent a healthy pregnancy. They say fertilization was 40% less likely to succeed when the father was overweight.[49]
The American Fertility Society recommends an age limit for sperm donors of 50 years or less,[50] and many fertility clinics in the United Kingdom will not accept donations from men over 40 or 45 years of age.[51]
Historical trends by country
France
The French pronatalist movement from 1919–1945 failed to convince French couples they had a patriotic duty to help increase their country's birthrate. Even the government was reluctant in its support to the movement. It was only between 1938 and 1939 that the French government became directly and permanently involved in the pronatalist effort. Although the birthrate started to surge in late 1941, the trend was not sustained. Falling birthrate once again became a major concern among demographers and government officials beginning in the 1970s.[52]
United States
From 1800 to 1940, fertility fell in the US. There was a marked decline in fertility in the early 1900s, associated with improved contraceptives, greater access to contraceptives and sexuality information and the "first" sexual revolution in the 1920s.
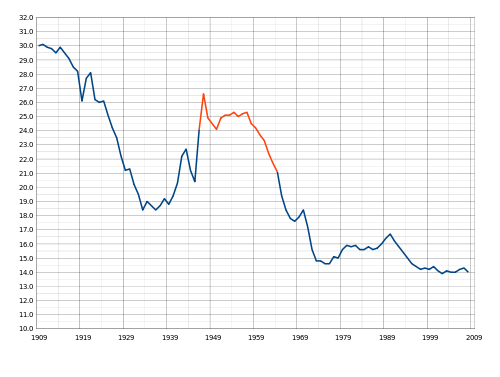
Post-WWII
After 1940 fertility suddenly started going up again, reaching a new peak in 1957. After 1960, fertility started declining rapidly. In the Baby Boom years (1946–1964), women married earlier and had their babies sooner; the number of children born to mothers after age 35 did not increase.[54]
Sexual revolution
After 1960, new methods of contraception became available, ideal family size fell, from 3 to 2 children. Couples postponed marriage and first births, and they sharply reduced the number of third and fourth births.[55]
Infertility
Infertility primarily refers to the biological inability of a person to contribute to conception. Infertility may also refer to the state of a woman who is unable to carry a pregnancy to full term. There are many biological causes of infertility, including some that medical intervention can treat.[56]
See also
- Birth control
- Family economics
- Family planning
- Fecundity
- Fertility clinic
- Fertility tourism
- Fertility deity
- Fertility preservation
- Human Fertilisation and Embryology Authority
- Natural fertility
- Oncofertility
- Reproductive health
- Sub-replacement fertility
- Total fertility rate
- Vasectomy
- Fertility-development controversy
- Fertility factor (demography)
Footnotes
- A., B.; Schultz, Paul T. (June 1976). "Fertility Determinants: A Theory, Evidence, and an Application to Policy Evaluation". Population and Development Review. 2 (2): 293. doi:10.2307/1972043. ISSN 0098-7921. JSTOR 1972043.
- Frank, O. (27 September 2017). "The demography of fertility and infertility". www.gfmer.ch.
- Last, John M. "Fecundity and Fertility". Encyclopedia of Public Health. Archived from the original on 11 August 2009 – via enotes.com.
- For detailed discussions of each measure see Paul George Demeny and Geoffrey McNicoll, Encyclopedia of Population (2003)
- Another way of doing it is to add up the ASFR for age 10-14, 15-19, 20-24, etc., and multiply by 5 (to cover the 5 year interval).
- Murphy, Michael (2013). "Cross-National Patterns of Intergenerational Continuities in Childbearing in Developed Countries". Biodemography and Social Biology. 59 (2): 101–126. doi:10.1080/19485565.2013.833779. ISSN 1948-5565. PMC 4160295. PMID 24215254.
- Hayford, S. R.; Morgan, S. P. (2008). "Religiosity and Fertility in the United States: The Role of Fertility Intentions". Social Forces. 86 (3): 1163–1188. doi:10.1353/sof.0.0000. PMC 2723861. PMID 19672317.
- Lars Dommermuth; Jane Klobas; Trude Lappegård (2014). "Differences in childbearing by time frame of fertility intention. A study using survey and register data from Norway". Part of the research project Family Dynamics, Fertility Choices and Family Policy (FAMDYN)
- Schaffnit, S. B.; Sear, R. (2014). "Wealth modifies relationships between kin and women's fertility in high-income countries". Behavioral Ecology. 25 (4): 834–842. doi:10.1093/beheco/aru059. ISSN 1045-2249.
- Rai, Piyush Kant; Pareek, Sarla; Joshi, Hemlata (2013). "Regression Analysis of Collinear Data using r-k Class Estimator: Socio-Economic and Demographic Factors Affecting the Total Fertility Rate (TFR) in India" (PDF). Journal of Data Science. 11.
- Bloom, David; Canning, David; Fink, Günther; Finlay, Jocelyn (2009). "Fertility, female labor force participation, and the demographic dividend". Journal of Economic Growth. 14 (2): 79–101. doi:10.1007/s10887-009-9039-9.
- Sato, Yasuhiro (30 July 2006), "Economic geography, fertility and migration" (PDF), Journal of Urban Economics, archived from the original (PDF) on 6 February 2016, retrieved 31 March 2008
- Li, Ang (2019). "Fertility intention‐induced relocation: The mediating role of housing markets". Population, Place and Space. 25 (8). doi:10.1002/psp.2265.
- Bongaarts, John (1978). "A Framework for Analyzing the Proximate Determinants of Fertility". Population and Development Review. 4 (1): 105–132. doi:10.2307/1972149. JSTOR 1972149.
- Stover, John (1998). "Revising the Proximate Determinants of Fertility Framework: What Have We Learned in the past 20 Years?". Studies in Family Planning. 29 (3): 255–267. doi:10.2307/172272. JSTOR 172272.
- Becker, Gary S. 1960. "An Economic Analysis of Fertility." In National Bureau Committee for Economic Research, Demographic and Economic Change in Developed Countries, a Conference of the Universities. Princeton, N.J.: Princeton University Press
- Mincer, Jacob. 1963. "Market Prices, Opportunity Costs, and Income Effects," in C. Christ (ed.) Measurement in Economics. Stanford, CA: Stanford University Press
- Easterlin, Richard A. (1975). "An Economic Framework for Fertility Analysis". Studies in Family Planning. 6 (3): 54–63. doi:10.2307/1964934. JSTOR 1964934. PMID 1118873.
- "How to get pregnant". Mayo Clinic. 2016-11-02. Retrieved 2018-02-16.
- "Fertility problems: assessment and treatment, Clinical guideline [CG156]". National Institute for Health and Care Excellence. Retrieved 2018-02-16. Published date: February 2013. Last updated: September 2017
- Dr. Philip B. Imler & David Wilbanks. "The Essential Guide to Getting Pregnant" (PDF). American Pregnancy Association. Archived from the original (PDF) on 2018-06-01. Retrieved 2018-02-16.
- Dunson, D.B.; Baird, D.D.; Wilcox, A.J.; Weinberg, C.R. (1999). "Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation". Human Reproduction. 14 (7): 1835–1839. doi:10.1093/humrep/14.7.1835. ISSN 1460-2350. PMID 10402400.
- Danilovich, Natalia; Babu, P. Suresh; Xing, Weirong; Gerdes, Maria; Krishnamurthy, Hanumanthappa; Sairam, M. Ram (2000-11-01). "Estrogen Deficiency, Obesity, and Skeletal Abnormalities in Follicle-Stimulating Hormone Receptor Knockout (FORKO) Female Mice**This investigation was supported in part by the Canadian Institutes of Health Research". Endocrinology. 141 (11): 4295–4308. doi:10.1210/endo.141.11.7765. ISSN 0013-7227. PMID 11089565.
- "Archived copy". Archived from the original on 2008-12-21. Retrieved 2008-09-22.CS1 maint: archived copy as title (link)
- Creinin, Mitchell D.; Keverline, Sharon; Meyn, Leslie A. (2004). "How regular is regular? An analysis of menstrual cycle regularity". Contraception. 70 (4): 289–92. doi:10.1016/j.contraception.2004.04.012. PMID 15451332.
- Anderson, S. E.; Dallal, G. E.; Must, A. (2003). "Relative Weight and Race Influence Average Age at Menarche: Results From Two Nationally Representative Surveys of US Girls Studied 25 Years Apart". Pediatrics. 111 (4 Pt 1): 844–50. doi:10.1542/peds.111.4.844. PMID 12671122.
- Apter D (February 1980). "Serum steroids and pituitary hormones in female puberty: a partly longitudinal study". Clin. Endocrinol. 12 (2): 107–20. doi:10.1111/j.1365-2265.1980.tb02125.x. PMID 6249519.
- Takahashi, TA; Johnson, KM (May 2015). "Menopause". The Medical Clinics of North America. 99 (3): 521–34. doi:10.1016/j.mcna.2015.01.006. PMID 25841598.
- Bourgeois, F. John; Gehrig, Paola A.; Veljovich, Daniel S. (1 January 2005). Obstetrics and Gynecology Recall. Lippincott Williams & Wilkins. ISBN 9780781748797 – via Google Books.
- A computer simulation run by Henri Leridon, PhD, an epidemiologist with the French Institute of Health and Medical Research:
- Leridon, H. (2004). "Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment". Human Reproduction. 19 (7): 1548–53. doi:10.1093/humrep/deh304. PMID 15205397.
- Dunson, David B.; Baird, Donna D.; Colombo, Bernardo (2004). "Increased Infertility With Age in Men and Women". Obstetrics & Gynecology. 103 (1): 51–6. doi:10.1097/01.AOG.0000100153.24061.45. PMID 14704244.
- Rothman, Kenneth J.; Wise, Lauren A.; Sørensen, Henrik T.; Riis, Anders H.; Mikkelsen, Ellen M.; Hatch, Elizabeth E. (2013). "Volitional determinants and age-related decline in fecundability: a general population prospective cohort study in Denmark". Fertility and Sterility. 99 (7): 1958–64. doi:10.1016/j.fertnstert.2013.02.040. PMC 3672329. PMID 23517858.
- Fertility Nutraceuticals, LLC "How to improve IVF success rates with smart fertility supplement strategy' May 6, 2014
- "Spanish woman ' is oldest mother'". BBC News. 2006-12-30. Retrieved 2006-12-30.
- Couzin, Jennifer (2004). "Reproductive Biology: Textbook Rewrite? Adult Mammals May Produce Eggs After All". Science. 303 (5664): 1593. doi:10.1126/science.303.5664.1593a. PMID 15016968.
- Wallace, WH; Kelsey, TW (2010). "Human Ovarian Reserve from Conception to the Menopause". PLOS ONE. 5 (1): e8772. arXiv:1106.1382. Bibcode:2010PLoSO...5.8772W. doi:10.1371/journal.pone.0008772. PMC 2811725. PMID 20111701.
- "Pregnancy After 35". March of Dimes. Retrieved October 30, 2014.
- "Down syndrome".
- Kidd, Sharon A; Eskenazi, Brenda; Wyrobek, Andrew J (2001). "Effects of male age on semen quality and fertility: a review of the literature". Fertility and Sterility. 75 (2): 237–48. doi:10.1016/S0015-0282(00)01679-4. PMID 11172821.
- Silber, Sherman J. (1991). "Effect of Age on Male Fertility". Seminars in Reproductive Endocrinology. 9 (3): 241–248. doi:10.1055/s-2007-1019415.
- Campagne, Daniel M. (2013). "Can Male Fertility Be Improved Prior to Assisted Reproduction through The Control of Uncommonly Considered Factors?". International Journal of Fertility & Sterility. 6 (4): 214–23. PMC 3850314. PMID 24520443.
- Wiener-Megnazi, Zofnat; Auslender, Ron; Dirnfeld, Martha (1 January 2012). "Advanced paternal age and reproductive outcome". Asian J Androl. 14 (1): 69–76. doi:10.1038/aja.2011.69. PMC 3735149. PMID 22157982.
- Reichenberg, Abraham; Gross, Raz; Weiser, Mark; Bresnahan, Michealine; Silverman, Jeremy; Harlap, Susan; Rabinowitz, Jonathan; Shulman, Cory; Malaspina, Dolores; Lubin, Gad; Knobler, Haim Y.; Davidson, Michael; Susser, Ezra (2006). "Advancing Paternal Age and Autism". Archives of General Psychiatry. 63 (9): 1026–32. doi:10.1001/archpsyc.63.9.1026. PMID 16953005.
- Jaffe, AE; Eaton, WW; Straub, RE; Marenco, S; Weinberger, DR (1 March 2014). "Paternal age, de novo mutations and schizophrenia". Mol Psychiatry. 19 (3): 274–275. doi:10.1038/mp.2013.76. PMC 3929531. PMID 23752248.
- Schulz, S. Charles; Green, Michael F.; Nelson, Katharine J. (1 April 2016). Schizophrenia and Psychotic Spectrum Disorders. Oxford University Press. ISBN 9780199378074 – via Google Books.
- Malaspina, Dolores; Harlap, Susan; Fennig, Shmuel; Heiman, Dov; Nahon, Daniella; Feldman, Dina; Susser, Ezra S. (2001). "Advancing Paternal Age and the Risk of Schizophrenia". Archives of General Psychiatry. 58 (4): 361–7. doi:10.1001/archpsyc.58.4.361. PMID 11296097.
- Sipos, Attila; Rasmussen, Finn; Harrison, Glynn; Tynelius, Per; Lewis, Glyn; Leon, David A; Gunnell, David (2004). "Paternal age and schizophrenia: a population based cohort study". BMJ. 329 (7474): 1070. doi:10.1136/bmj.38243.672396.55. PMC 526116. PMID 15501901.
- Malaspina, Dolores; Corcoran, Cheryl; Fahim, Cherine; Berman, Ariela; Harkavy-Friedman, Jill; Yale, Scott; Goetz, Deborah; Goetz, Raymond; Harlap, Susan; Gorman, Jack (2002). "Paternal age and sporadic schizophrenia: Evidence for de novo mutations". American Journal of Medical Genetics. 114 (3): 299–303. doi:10.1002/ajmg.1701. PMC 2982144. PMID 11920852.
- "Obesity | Fat men linked to low fertility". Sydney Morning Herald. 18 October 2010. Retrieved 19 October 2010.
- Plas, E; Berger, P; Hermann, M; Pflüger, H (2000). "Effects of aging on male fertility?". Experimental Gerontology. 35 (5): 543–51. doi:10.1016/S0531-5565(00)00120-0. PMID 10978677.
- Age Limit of Sperm Donors in the United Kingdom Pdf file Archived October 3, 2008, at the Wayback Machine
- Reggiani, Andrés Horacio (Spring 1996). "Procreating France: The Politics of Demography, 1919-1945". French Historical Studies. 19 (3): 725–54. doi:10.2307/286642. JSTOR 286642.
- CDC Bottom of this page https://www.cdc.gov/nchs/products/vsus.htm "Vital Statistics of the United States, 2003, Volume I, Natality", Table 1-1 "Live births, birth rates, and fertility rates, by race: United States, 1909-2003."
- Oppenheimer, Valerie Kincade. Women's rising employment and the future of the family in industrial societies. OCLC 936722012.
- Bailey, M. J. (2006-02-01). "More Power to the Pill: The Impact of Contraceptive Freedom on Women's Life Cycle Labor Supply". The Quarterly Journal of Economics. 121 (1): 289–320. doi:10.1093/qje/121.1.289. ISSN 0033-5533.
- Makar, Robert S.; Toth, Thomas L. (2002). "The Evaluation of Infertility". American Journal of Clinical Pathology. 117 Suppl: S95–103. doi:10.1309/w8lj-k377-dhra-cp0b. PMID 14569805.
References
This article incorporates material from the Citizendium article "Fertility (demography)", which is licensed under the Creative Commons Attribution-ShareAlike 3.0 Unported License but not under the GFDL.
- Barrett, Richard E., Donald J. Bogue, and Douglas L. Anderton. The Population of the United States 3rd Edition (1997) compendium of data
- Campagne, Daniel M (2013). "Can Male Fertility Be Improved Prior to Assisted Reproduction through The Control of Uncommonly Considered Factors?". International Journal of Fertility & Sterility. 6 (4): 214–23. PMC 3850314. PMID 24520443.
- Coale, Ansley J. and Susan C. Watkins, eds. The Decline of Fertility in Europe, (1986)
- Eversley, D. E. C. Social Theories of Fertility and the Malthusian Debate (1959) online edition
- Garrett, Eilidh ety al. Family Size in England and Wales: Place, Class, and Demography, 1891-1911(2001) online edition
- Grabill, Wilson H.. Clyde V. Kiser, Pascal K. Whelpton. The Fertility of American Women (1958), influential study at the peak of the Baby Boom online edition
- GuzmÁn, JosÉ Miguel et al. The Fertility Transition in Latin America (1996) online edition
- Haines, Michael R. and Richard H. Steckel (eds.), A Population History of North America. Cambridge University Press, 2000, 752 pp. advanced scholarship
- Hawes, Joseph M. and Elizabeth I. Nybakken, eds. American Families: a Research Guide and Historical Handbook. (Greenwood Press, 1991)
- Klein, Herbert S. A Population History of the United States. Cambridge University Press, 2004. 316 pp
- Knox, P. L. et al. The United States: A Contemporary Human Geography. Longman, 1988. 287 pp.
- Kohler, Hans-Peter Fertility and Social Interaction: An Economic Perspective (2001) online edition
- Leete, Richard. Dynamics of Values in Fertility Change (1999) online edition
- Lovett, Laura L. Conceiving the Future: Pronatalism, Reproduction, and the Family in the United States, 1890–1938, (2007) 236 pages;
- Mintz Steven and Susan Kellogg. Domestic Revolutions: a Social History of American Family Life. (1988)
- Pampel, Fred C.; Peters, H. Elizabeth (1995). "The Easterlin Effect". Annual Review of Sociology. 21: 163–194. doi:10.1146/annurev.so.21.080195.001115. PMID 12291060.
- Population Reference Bureau, Population Handbook (5th ed. 2004) online (5th ed. 2004).
- Reed, James. From Private Vice to Public Virtue: The Birth Control Movement and American Society Since 1830. 1978.
- Tarver, James D. The Demography of Africa (1996) online edition
- Weeks, John R. Population: An Introduction to Concepts and Issues (10th ed. 2007), standard textbook
Journals
- Demography — Scope and links to issue contents & abstracts.
- Journal of Population Economics
- Population and Development Review — Aims and abstract & supplement links.
- Population Bulletin — Each issue on a current population topic.
- Population Studies —Aims and scope.
- Review of Economics of the Household
Further reading
- Josef Ehmer, Jens Ehrhardt, Martin Kohli (Eds.): Fertility in the History of the 20th Century: Trends, Theories, Policies, Discourses. Historical Social Research 36 (2), 2011.
- Fertility treatment and clinics in the UK - HFEA
- Jorge Chavarro (2009) The Fertility Diet: Groundbreaking Research Reveals Natural Ways to Boost Ovulation and Improve Your Chances of Getting Pregnant, McGraw-Hill Professional. ISBN 978-0-07-162710-8
- Bock J (2002). "Introduction: evolutionary theory and the search for a unified theory of fertility" (PDF). Am. J. Hum. Biol. 14 (2): 145–8. doi:10.1002/ajhb.10039. PMID 11891930.
- Jones C (March 2008). "Ethical and legal conundrums of postmodern procreation". Int J Gynaecol Obstet. 100 (3): 208–10. doi:10.1016/j.ijgo.2007.09.031. PMID 18062970.
- Fertility statistics from the Commission on Population Growth and the American Future (1972)
External links
- United Nations World Population Prospects, the 2008 Revision, Data on fertility trends worldwide