Spastic cerebral palsy
Spastic cerebral palsy is the type of cerebral palsy characterized by spasticity or high muscle tone often resulting in stiff, jerky movements.[1] Cases of spastic CP are further classified according to the part or parts of the body that are most affected.[2] Such classifications include spastic diplegia, spastic hemiplegia, spastic quadriplegia, and in cases of single limb involvement, spastic monoplegia.[3]
| Spastic cerebral palsy | |
|---|---|
 | |
| A child with spastic cerebral palsy | |
| Specialty | Neurology |
Spastic cerebral palsy affects the motor cortex[1] of the brain, a specific portion of the cerebral cortex responsible for the planning and completion of voluntary movement.[4] Spastic CP is the most common type of overall cerebral palsy, representing roughly 80% of cases.[2] Spastic CP is a permanent condition and will affect an individual across the lifespan.[5] The brain injury that causes spastic CP remains stable over time, but the way spasticity affects a person can change.[1] For example, with age they may develop bone deformities from the pull of spastic muscles, muscular deterioration, and loss of range of motion in a joint.[1] Thus, individuals with spastic CP often have different support needs with time.[6]
Signs and symptoms
People with the spastic type of CP typically have muscles that are "tight" or stiff due to high muscle tone.[2] Symptoms of spastic cerebral palsy vary as the disability can affect individuals differently.[2] However, they typically appear in infancy and early childhood and most children are diagnosed in the first two years of life.[7] The main indicator of spastic cerebral palsy is a delay in reaching motor milestones.[2] The following are some common early signs, though the presence of a listed symptom does not definitively mean that a child has spastic CP:[2]
Prior to 6 months
- Legs crossing when a child is picked up, also called scissoring [8]
- Stiffness[8]
- Head "lagging" when the child is picked up[8]
6–10 months
Older than 12 months of age
Walking with an unsteady, uneven, or stiff gait[9]
Spastic CP is distinguished from other forms of cerebral palsy by its prominent symptom of spasticity or stiff, tight movements and gait patterns such as the scissor gait.[1] However, spasticity as a symptom is also seen in other conditions such as stroke and multiple sclerosis.[1] Thus, the presence of spasticity alone does not warrant a conclusive diagnosis of spastic cerebral palsy.
Changes in spasticity and corresponding postures may also occur with other brain activity, such as excitement, fear or anxiety, or even pain, which increase muscle tension.
A person with spastic CP will commonly show, in addition to higher muscle tone, persistent primitive reflexes, greater stretch reflexes, plantar reflex, and ankle clonus.[10]
A third of people with cerebral palsy have seizures - this is most common in spastic CP.[11] Audiovisual, cognitive compromise and behavioral disorders can occur.
Cause
Spastic cerebral palsy is caused by malformation of or damage to the parts of the brain that control movement.[12] What exactly makes some children susceptible to such brain damage is often unknown but it is believed that cerebral palsy may be the result of causal pathways, or chains of events that cause or increase the likelihood of brain injury.[13] Most of the time, children are born with the brain damage resulting in spastic cerebral palsy, but a small percentage experience the damage shortly after birth following a stroke, head injury, or infection.[12]
The following are types of brain damage that can result in spastic cerebral palsy:
- cerebral dysgenesis[12]
- periventricular leukomalacia[12]
- brain bleeds[12]
- Hypoxic ischaemic encephalopathy[12]
Risk factors
The following medical conditions are associated with increased likelihood of spastic cerebral palsy, as well as with other types of cerebral palsy:
Diagnosis
There is no single test to diagnose spastic cerebral palsy. It is typically diagnosed by age 2, though milder cases may go undetected for a longer time.[12] A doctor will typically use a series of tests to assess developmental progress in growth, muscle control, coordination, vision, hearing, and posture.[12] Continuous loss of motor skills likely indicates a condition other than spastic CP such as a genetic muscle disease[12] Some metabolic disorders mimic spastic cerebral palsy and can be ruled out using a Magnetic resonance imaging test (MRI).[12]
Some tests to assess a child suspected to have spastic cerebral palsy are:
These tests are imaging techniques used to produce pictures of the brain and to examine them for areas of damage that indicate a diagnosis of spastic cerebral palsy.[12] A child with a spastic CP diagnosis will likely be referred to screening for other conditions associated with spastic cerebral palsy such as epilepsy (seizure disorder), intellectual disability, and visual impairment.[14]
Types
Scientific classifications
The types of spastic cerebral palsy are generally distinguished by the primary areas of the body that are affected.[2]
- Spastic hemiplegia Hemiplegia is a type of cerebral palsy affecting one vertical half of the body (such as one arm and one leg).[15] The affected side of the body is opposite the affected area of the brain in hemiplegia.[15] For example, if the right side of the brain is damaged, the person will have weakness or paralysis on the left side of the body.[15] People with hemiplegia typically favor an arm or hand and may keep the weaker hand in a fist.[15] Typically, people that have spastic hemiplegia are the most ambulatory of all the forms, although they generally have dynamic equinus (a limping instability) on the affected side and are primarily prescribed ankle-foot orthoses to prevent said equinus.[16]
- Spastic diplegia describes spastic CP in which muscle tightness predominantly occurs in the legs.[2] The arms may be somewhat affected or not affected at all.[2]
- Spastic monoplegia is one single limb being affected.[3]
- Spastic triplegia is three limbs being affected.[17]
- Spastic quadriplegia is all four limbs more or less equally affected.[18] People with spastic quadriplegia are rarely able to ambulate without assistance and may not stand at all.[8] Among the forms of spastic CP, quad CP is more likely to co-occur with seizures and mild to moderate intellectual disability.[8]
In spastic cerebral palsy in children with low birth weights, 25% of children had hemiplegia, 37.5% had quadriplegia, and 37.5% had diplegia.[19] No one person with a particular type of spastic CP presents in exactly the same way.
Treatment
There is no cure for spastic cerebral palsy and no way to reverse the initial brain injury.[20] However, various treatments and assistive devices can help mitigate pain and allow those affected to have a higher quality of life. Different combinations of treatments are right for each individual and are determined by individuals and their care team.
Some common interventions are:
- Physical therapy- exercises to develop balance and strength and to learn skills such as walking, rolling, or driving a wheelchair.[20]
- Occupational therapy- therapy to help an individual develop strategies to complete activities of daily living such as dressing, toileting, and bathing either independently or with a level of assistance that is safe and comfortable.[20]
- Orthotics- braces and splints to improve posture and positioning (usually on legs or arms).[20]
- Assistive devices- Wheelchairs, crutches, and walkers may help someone with spastic CP navigate safely.[20] Different devices may be used in different settings or for longer distances. People with cerebral palsy use 3-5 times the energy as those without when moving;[8] thus, a device such as a wheelchair may reduce fatigue.
- Speech therapy- Therapy to help someone speak more clearly, swallow more safely, or use a communication device[12] such as a DynaVox
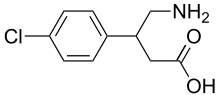
- Medication- Certain medications can reduce stiffness from overactive muscles and decrease pain. Examples are botulinum toxin or baclofen, with the latter delivered orally or via an intrathecal pump.[8]
- Surgery- In some cases, orthopedic and/or neurological surgeries are recommended when pain and stiffness interfere with participation in meaningful activities and other treatments are not effective.[8]
Prognosis
Every case of spastic cerebral palsy is different. Some people with this type of CP can accomplish activities of daily living independently, while some need the assistance of a personal care aide for certain tasks, and others need 24-hour support.[21] About 1/3 of people with cerebral palsy cannot walk, about 1/2 have intellectual disabilities, and 3/4 experience some level of chronic pain.[21] There is limited research on adults with spastic CP.[22] The brain injury causing CP does not progress or change, but the functional impact and thus, one's needs may change with age.[7]
Some issues specific to adults with spastic and other forms of cerebral palsy are:
- Premature aging[8]
- Fatigue[8]
- Pain[8]
- Arthritis[8]
- Depression and anxiety[8]
- Post impairment syndrome[8]
Regardless of their particular expression of spastic cerebral palsy, affected individuals can lead fulfilling lives. Improved physical accessibility in society and increased social acceptance can increase community participation.[23] Workforce participation of people with CP has almost doubled in the last four decades.[24] Social inclusion and the presence or absence of policy to address discrimination, in addition to medical intervention, influences the outlook for people living with spastic cerebral palsy.[23]
See also
References
- "Spastic cerebral palsy". Cerebral Palsy Alliance. 2015-11-18. Retrieved 2020-03-10.
- "What is Cerebral Palsy?". Centers for Disease Control and Prevention. 2019-04-30. Retrieved 2020-03-04.
- "Cerebral palsy spastic monoplegic". Genetic and Rare Diseases Information Center (GARD). Retrieved 2020-03-10.
- Knierim, James (2020). "Chapter 3: The motor cortex". Neuroscience online: An electronic textbook of the neurosciences from the University of Texas at Houston. Retrieved 4 March 2020.
- "Spastic diplegia cerebral palsy". Genetic and Rare Diseases Information Center (GARD). 7 August 2018. Retrieved 2020-03-10.
- Haak, Peterson; Lenski, Madeleine; Hidecker, Mary Jo Cooley; Li, Min; Paneth, Nigel (2009). "Cerebral palsy and aging". Developmental Medicine and Child Neurology. 51 (4): 16–23. doi:10.1111/j.1469-8749.2009.03428.x. ISSN 0012-1622. PMC 4183123. PMID 19740206.
- Shrader, MD, M. Wade; Salzbrenner, APRN, Margaret. "Spastic cerebral palsy (for parents)". Kidshealth. Retrieved 16 March 2020.
- "Cerebral Palsy: Hope Through Research | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Retrieved 2020-03-16.
- "Cerebral palsy - Symptoms and causes". Mayo Clinic. Retrieved 2020-03-20.
- Sobralske, Mary C. (2013). "Common Physical or Sensory Disabilities". In Eddy, Linda L. (ed.). Caring for children with special healthcare needs and their families a handbook for healthcare professionals. Ames, Iowa: Wiley-Blackwell. p. 13. ISBN 9781118783290.
- Shaikh, SafiyaImtiaz; Hegade, Ganapati (2017). "Role of anesthesiologist in the management of a child with cerebral palsy". Anesthesia: Essays and Researches. 11 (3): 544–549. doi:10.4103/0259-1162.194569. PMC 5594763. PMID 28928544.
- "Cerebral Palsy: Hope Through Research | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Retrieved 2020-03-23.
- "What Causes Cerebral Palsy? | Cerebral Palsy Alliance". Cerebral Palsy Alliance. Retrieved 2020-03-24.
- "How does cerebral palsy affect people? | Cerebral Palsy Alliance". Cerebral Palsy Alliance. Retrieved 2020-03-23.
- "Hemiplegia". CHASA. Retrieved 2020-03-31.
- Birol Balaban, Evren Yasar, Ugur Dal, Kamil Yazicioglu, Haydar Mohur & Tunc Alp Kalyon "The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy" Disability and Rehabilitation, January 2007; 29(2): 139–144
- Panteliadis, Christos P.; Strassburg, Hans-Michael (2004). Cerebral Palsy: Principles and Management. Thieme. p. 19. ISBN 9781588902955. Retrieved 15 January 2017.
- "Cerebral palsy spastic quadriplegic | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 15 January 2017.
- O’Shea, TM (2008). "Diagnosis, Treatment, and Prevention of Cerebral Palsy". Clinical Obstet Gynecol. 51 (4): 816–28. doi:10.1097/GRF.0b013e3181870ba7. PMC 3051278. PMID 18981805.
- "What are common treatments for cerebral palsy?". National Institute of Child Health and Human Development. Retrieved 2020-04-05.
- "How does cerebral palsy affect people? | Cerebral Palsy Alliance". Cerebral Palsy Alliance. Retrieved 2020-04-05.
- Gyoung Yi, MD, You; Jung, MD, Se Hee; Bang, MD, Moon Suk (28 June 2019). "Emerging Issues in Cerebral Palsy Associated With Aging: A Physiatrist Perspective". Annals of Rehabilitation Medicine. 43 (3): 241–249. doi:10.5535/arm.2019.43.3.241. PMC 6637058. PMID 31311245.
- CDC (2019-09-04). "Disability and Health Inclusion Strategies | CDC". Centers for Disease Control and Prevention. Retrieved 2020-04-05.
- "Cerebral Palsy Outlook / Prognosis". Cleveland Clinic. Retrieved 2020-04-05.
