Kainic acid
Kainic acid, or kainate, is an acid that naturally occurs in some seaweed. Kainic acid is a potent neuroexcitatory amino acid agonist that acts by activating receptors for glutamate, the principal excitatory neurotransmitter in the central nervous system. Glutamate is produced by the cell's metabolic processes and there are four major classifications of glutamate receptors: NMDA receptors, AMPA receptors, kainate receptors, and the metabotropic glutamate receptors. Kainic acid is an agonist for kainate receptors, a type of ionotropic glutamate receptor. Kainate receptors likely control a sodium channel that produces excitatory postsynaptic potentials (EPSPs) when glutamate binds.[1]
 | |
| Names | |
|---|---|
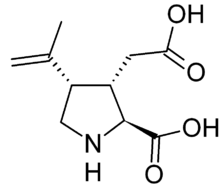
| IUPAC name
(2S,3S,4S)-3-(Carboxymethyl)-4-(prop-1-en-2-yl)pyrrolidine-2-carboxylic acid | |
| Other names
(3S,4S)-3-(Carboxymethyl)-4-prop-1-en-2-yl-L-proline; 2-Carboxy-3-carboxymethyl-4-isopropenyl-pyrrolidine | |
| Identifiers | |
3D model (JSmol) |
|
| 86660 | |
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| KEGG | |
| MeSH | Kainic+acid |
PubChem CID |
|
| UNII | |
CompTox Dashboard (EPA) |
|
| |
| |
| Properties | |
| C10H15NO4 | |
| Molar mass | 213.233 g·mol−1 |
| Melting point | 215 °C (419 °F; 488 K) (decomposes) |
| log P | 0.635 |
| Acidity (pKa) | 2.031 |
| Basicity (pKb) | 11.966 |
| Structure | |
| Monoclinic | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Kainic acid is commonly injected into laboratory animal models to study the effects of experimental ablation. Kainic acid is a direct agonist of the glutamic kainate receptors and large doses of concentrated solutions produce immediate neuronal death by overstimulating neurons to death. Such damage and death of neurons is referred to as an excitotoxic lesion. Thus, in large, concentrated doses kainic acid can be considered a neurotoxin, and in small doses of dilute solution kainic acid will chemically stimulate neurons.[2]
Electrical stimulation of designated areas of the brain are generally administered by passing an electric current through a wire that is inserted into the brain to lesion a particular area of the brain. Electrical stimulation indiscriminately destroys anything in the vicinity of the electrode tip, including neural bodies and axons of neurons passing through; therefore it is difficult to attribute the effects of the lesion to a single area. Chemical stimulation is typically administered through a cannula that is inserted into the brain via stereotactic surgery. Chemical stimulation, while more complicated than electrical stimulation, has the distinct advantage of activating cell bodies, but not nearby axons, because only cell bodies and subsequent dendrites contain glutamate receptors. Therefore, chemical stimulation by kainic acid is more localized than electrical stimulation. Both chemical and electrical lesions potentially cause additional damage to the brain due to the very nature of the inserted electrode or cannula. Therefore, the most effective ablation studies are performed in comparison to a sham lesion that duplicates all the steps of producing a brain lesion except the one that actually causes the brain damage, that is, injection of kainic acid or administration of an electrical shock.
Occurrence
Kainic acid was originally isolated from seaweed in 1953.[3] called "Kainin-sou" or "Makuri" in Japan. "Kainin-sou" is used as an anthelmintic in Japan.
Pharmacological activity
Kainic acid is utilised in primary neuronal cell cultures[4] and in the acute brain slice preparation[5] to study the physiological effect of excitotoxicity and assess the neuroprotective capabilities of potential therapeutics.
Kainic acid is a potent central nervous system excitant that is used in epilepsy research to induce seizures in experimental animals[6], at a typical dose of 10–30 mg/kg in mice. In addition to inducing seizures, kainic acid is excitotoxic and epileptogenic.[7] Kainic acid induces seizures via activation of kainate receptors containing the GluK2 subunit and also through activation of AMPA receptors, for which it serves as a partial agonist.[8] Also, infusion with kainic acid in the hippocampus of animals results in major damage of pyramidal neurons and subsequent seizure activity. Supply shortages beginning in 2000 have caused the cost of kainic acid to rise significantly.
Applications
- antiworming agent
- neuroscience research
- neurodegenerative agent
- modeling of epilepsy[9]
- modeling of Alzheimer's disease
References
- Carlson, Neil R. (2013). Physiology of Behavior. Pearson. pp. 121. ISBN 978-0-205-23939-9.
- Carlson, Neil R. (2013). Physiology of Behavior. Pearson. pp. 152. ISBN 978-0-205-23939-9.
- Moloney, Mark G. (1998). "Excitatory amino acids". Natural Product Reports. 15 (2): 205–219. doi:10.1039/a815205y. PMID 9586226.
- Meade, AJ; Meloni, BP; Mastaglia, FL; Watt, PM; Knuckey, NW (Nov 11, 2010). "AP-1 inhibitory peptides attenuate in vitro cortical neuronal cell death induced by kainic acid". Brain Research. 1360: 8–16. doi:10.1016/j.brainres.2010.09.007. PMID 20833150.
- Craig, Amanda; Housley, Gary; Fath, Thomas (2014). Modeling excitotoxic ischaemic brain injury of cerebellar Purkinje neurons by intravital and in vitro multi-photon laser scanning microscopy. Springer. pp. 105–128. ISBN 978-1-4939-0380-1.
- Barrow, Paul Anthony. A study of the changes in dentate granule cell excitability and inhibition in the kainic acid model of temporal lobe epilepsy. OCLC 53634796.
- Ben-Ari, Y (2012). Kainate and Temporal Lobe Epilepsies: 3 decades of progress. National Center for Biotechnology Information (US). PMID 22787646.
- Fritsch B, Reis J, Gasior M, Kaminski RM, Rogawski MA (April 2014). "Role of GluK1 kainate receptors in seizures, epileptic discharges, and epileptogenesis". Journal of Neuroscience. 34 (17): 5765–75. doi:10.1523/JNEUROSCI.5307-13.2014. PMC 3996208. PMID 24760837.
- Barrow, Paul Anthony. A study of the changes in dentate granule cell excitability and inhibition in the kainic acid model of temporal lobe epilepsy. OCLC 53634796.