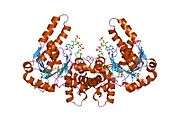
Hydroxyacyl-Coenzyme A dehydrogenase
Hydroxyacyl-Coenzyme A dehydrogenase (HADH) is an enzyme which in humans is encoded by the HADH gene.[5][6]
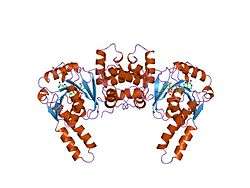
Structure
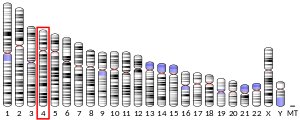
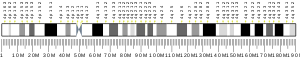
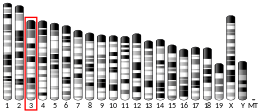
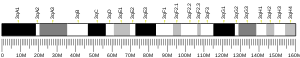
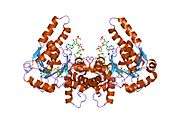
The HADH gene is located on the 4th chromosome, with its specific location being identified as 4q22-q26. The gene has 10 exons.[7] The HADH gene encodes a 34.3 kDa protein that has 314 amino acids and 124 observed peptides.[8][9]
Function
This gene is a member of the 3-hydroxyacyl-CoA dehydrogenase gene family. The encoded protein functions in the mitochondrial matrix to catalyze the oxidation of straight-chain 3-hydroxyacyl-CoAs as part of the beta-oxidation pathway. Its enzymatic activity is highest with medium-chain-length fatty acids.[7]
Clinical significance
Mutations in this gene cause one form of familial hyperinsulinemic hypoglycemia.[10] A deficiency is associated with 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. Mutations also cause 3-hydroxyacyl-CoA dehydrogenase deficiency. There are a wide variety of mutations that have been identified to cause this disease. Among them are missense mutations (A40T, P258L, D57G, Y226H) and nonsense mutations (R236X) in the protein, and splicing mutations (261+1G>A, 710-2A>G) and some small deletions (587delC) in the cDNA.[11] One mutation, 636+471G>T in the HADH gene, was shown to create a cryptic splice donor site and an out-of-frame pseudoexon.[12] Most of the described cases have homozygous mutations. This disease has fairly homogenous clinical presentation across cases. The symptoms first appear in early life, between 1.5 hours post birth and 3 years of age, and the most common symptoms are hypoglycemia and seizures/convulsions directly related to the hypoglycemia. There are other clinical presentations that have been identified, namely: myoglobinuria, dicarboxylic aciduria, feeding difficulties in infancy, muscular hypotonia, hepatic steatosis, growth delay, hypertrophic cardiomyopathy, dilated cardiomyopathy, hepatic necrosis, and fulminant hepatic failure. The disorder may be diagnosed by either the analysis of the molecular genetics of the individual, or by detection of abnormal metabolite levels in blood and/or plasma. Individuals with this deficiency have an elevated amount of 3-hydroxyglutarate excreted through the urine; a heightened level of C4-OH acylcarnitine in the blood plasma is also a characteristic of this FAO disorder. Most documented cases thus far have shown that individuals are responsive to diazoxide treatment, and highlight the need for diagnosis and treatment administration as early as possible in order to correct hypoglycemia and avoid irreversible brain damage.[11]
Interactions
HADH has been shown to interact with Vpr, such that HIV-1 Vpr regulates mitochondrial respiration and enhances the activity of hydroxyacyl-CoA dehydrogenase (HADH) through PPARbeta/delta.[13]
See also
- 3-hydroxyacyl-CoA dehydrogenase
- hydroxyacyl-CoA dehydrogenase/3-ketoacyl-CoA thiolase/enoyl-CoA hydratase (trifunctional protein), alpha subunit
References
- GRCh38: Ensembl release 89: ENSG00000138796 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000027984 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Craig I, Tolley E, Bobrow M (1976). "A preliminary analysis of the segregation of human hydroxyacyl coenzyme A dehydrogenase in human-mouse somatic cell hybrids". Cytogenetics and Cell Genetics. 16 (1–5): 114–7. doi:10.1159/000130568. PMID 975867.
- Yang SY, He XY, Schulz H (Oct 2005). "3-Hydroxyacyl-CoA dehydrogenase and short chain 3-hydroxyacyl-CoA dehydrogenase in human health and disease". The FEBS Journal. 272 (19): 4874–83. doi:10.1111/j.1742-4658.2005.04911.x. PMID 16176262.
- "Entrez Gene: HADH".
- Zong NC, Li H, Li H, Lam MP, Jimenez RC, Kim CS, Deng N, Kim AK, Choi JH, Zelaya I, Liem D, Meyer D, Odeberg J, Fang C, Lu HJ, Xu T, Weiss J, Duan H, Uhlen M, Yates JR, Apweiler R, Ge J, Hermjakob H, Ping P (Oct 2013). "Integration of cardiac proteome biology and medicine by a specialized knowledgebase". Circulation Research. 113 (9): 1043–53. doi:10.1161/CIRCRESAHA.113.301151. PMC 4076475. PMID 23965338.
- "Hydroxyacyl-coenzyme A dehydrogenase, mitochondrial". Cardiac Organellar Protein Atlas Knowledgebase (COPaKB).
- Molven A, Matre GE, Duran M, Wanders RJ, Rishaug U, Njølstad PR, Jellum E, Søvik O (Jan 2004). "Familial hyperinsulinemic hypoglycemia caused by a defect in the SCHAD enzyme of mitochondrial fatty acid oxidation". Diabetes. 53 (1): 221–7. doi:10.2337/diabetes.53.1.221. PMID 14693719.
- Martins E, Cardoso ML, Rodrigues E, Barbot C, Ramos A, Bennett MJ, Teles EL, Vilarinho L (Jun 2011). "Short-chain 3-hydroxyacyl-CoA dehydrogenase deficiency: the clinical relevance of an early diagnosis and report of four new cases". Journal of Inherited Metabolic Disease. 34 (3): 835–42. doi:10.1007/s10545-011-9287-7. PMID 21347589.
- Flanagan SE, Xie W, Caswell R, Damhuis A, Vianey-Saban C, Akcay T, Darendeliler F, Bas F, Guven A, Siklar Z, Ocal G, Berberoglu M, Murphy N, O'Sullivan M, Green A, Clayton PE, Banerjee I, Clayton PT, Hussain K, Weedon MN, Ellard S (Jan 2013). "Next-generation sequencing reveals deep intronic cryptic ABCC8 and HADH splicing founder mutations causing hyperinsulinism by pseudoexon activation". American Journal of Human Genetics. 92 (1): 131–6. doi:10.1016/j.ajhg.2012.11.017. PMC 3542457. PMID 23273570.
- Shrivastav S, Zhang L, Okamoto K, Lee H, Lagranha C, Abe Y, Balasubramanyam A, Lopaschuk GD, Kino T, Kopp JB (Sep 2013). "HIV-1 Vpr enhances PPARβ/δ-mediated transcription, increases PDK4 expression, and reduces PDC activity". Molecular Endocrinology. 27 (9): 1564–76. doi:10.1210/me.2012-1370. PMC 3753422. PMID 23842279.
External links
- GeneReviews/NCBI/NIH/UW entry on Familial Hyperinsulinism
- Overview of all the structural information available in the PDB for UniProt: Q16836 (Hydroxyacyl-coenzyme A dehydrogenase, mitochondrial) at the PDBe-KB.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.