Carboxyhemoglobin
Carboxyhemoglobin or carboxyhaemoglobin (symbol COHb or HbCO) is a stable complex of carbon monoxide and hemoglobin (Hb) that forms in red blood cells upon contact with carbon monoxide (CO). Carboxyhemoglobin is often mistaken for the compound formed by the combination of carbon dioxide and hemoglobin, which is actually carbaminohemoglobin. Exposure to small concentrations of CO hinder the ability of Hb to deliver oxygen to the body, because carboxyhemoglobin forms more readily than does oxyhemoglobin (HbO2). CO is produced in normal metabolism and is also a common chemical. Tobacco smoking (through carbon monoxide inhalation) raises the blood levels of COHb by a factor of several times from its normal concentrations.
Affinity of Hb for CO
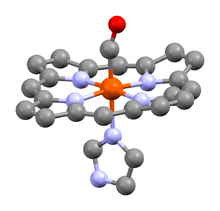
Hemoglobin contains four heme groups each capable of reversibly binding to one oxygen molecule.[2] Oxygen binding to any of these sites causes a conformational change in the protein, facilitating binding to each of the other sites. Carbon monoxide binds to hemoglobin at the same sites as oxygen, but approximately 210 times more tightly.[3] Normally, oxygen would bind to hemoglobin in the lungs and be released in areas with low oxygen partial pressure (e.g. active muscles).[4] When carbon monoxide binds to hemoglobin, it cannot be released as easily as oxygen. The slow release rate of carbon monoxide causes an accumulation of CO-bound hemoglobin molecules as exposure to carbon monoxide continues. Because of this, fewer hemoglobin particles are available to bind and deliver oxygen, thus causing the gradual suffocation associated with carbon monoxide poisoning.
Carbon monoxide as a poison
Since COHb releases carbon monoxide slowly, less hemoglobin will be available to transport oxygen from the lungs to the rest of the body. Conversion of most Hb to COHb results in death - known medically as carboxyhemoglobinemia[5] or carbon monoxide poisoning.[6] Smaller amounts COHb lead to oxygen deprivation of the body causing tiredness, dizziness, and unconsciousness.
COHb has a half-life in the blood of 4 to 6 hours. This time can be reduced to 70 to 35 minutes with administration of pure oxygen (the lower number applying when oxygen is administered with 4 to 5% CO2 to cause hyperventilation). Additionally, treatment in a hyperbaric chamber is a more effective manner of reducing the half-life of COHb than administering oxygen alone. This treatment involves pressurizing the chamber with pure oxygen at an absolute pressure close to three atmospheres, allowing the body's fluids, instead of the crippled hemoglobin bonded to CO, to absorb oxygen and to pass free oxygen on to hypoxic tissues. In effect, the need for hemoglobin in the blood is (partially) bypassed. Supplemental oxygen takes advantage of Le Chatelier's principle to quicken the decomposition of carboxyhemoglobin back to hemoglobin:
HbCO + O2 ⇌ Hb + CO + O2 ⇌ HbO2 + CO
COHb increases risk of blood clot. It is thought that through this mechanism, smoking increases the risk of having thromboembolic disease.
Pregnant smokers may give birth to babies of a lower birth mass. In addition to vasoconstriction of the placenta, another theory is that since fetal hemoglobin takes up carbon monoxide more readily than in an adult, therefore the fetus of a smoker will suffer from mild hypoxia, potentially retarding its development.
Carbon monoxide as normal biological metabolite and potential pharmaceutical
In biology, carbon monoxide is naturally produced by the action of heme oxygenase 1 and 2 on the heme from hemoglobin breakdown. This process produces a certain amount of carboxyhemoglobin in normal persons, even if they do not breathe carbon monoxide.
Following the first report that carbon monoxide is a normal neurotransmitter in 1993,[7][8] as well as one of three gasses which naturally modulate inflammatory responses in the body (the other two being nitric oxide and hydrogen sulfide), carbon monoxide has received a great deal of clinical attention as a biological regulator. In many tissues, all three gases are known to act as anti-inflammatories, vasodilators and encouragers of neovascular growth.[9] However, the issues are complex, as neovascular growth is not always beneficial, since it plays a role in tumor growth, and also the damage from wet macular degeneration, a disease for which smoking (a major source of carbon monoxide in the blood, several times more than natural production) increases the risk from 4 to 6 times.
Studies involving carbon monoxide have been conducted in many laboratories throughout the world for its anti-inflammatory and cytoprotective properties. These properties could potentially be used to prevent the development of a series of pathological conditions including ischemic reperfusion injury, transplant rejection, atherosclerosis, severe sepsis, severe malaria or autoimmunity. Clinical tests involving humans have been performed. As of 2009, however, the results had not yet been released.[10]
Based on the therapeutic potential of carbon monoxide, pharmaceutical efforts have focused on development of carbon monoxide-releasing molecules and selective heme oxygenase inducers.
References
- Vásquez GB, Ji X, Fronticelli C, Gilliland GL (1998). "Human Carboxyhemoglobin at 2.2 Å Resolution: Structure and Solvent Comparisons of R-State, R2-State and T-State Hemoglobins" (PDF). Acta Crystallogr. D. 54 (3): 355–366. doi:10.1107/S0907444997012250. PMID 9761903.
- Berg JM, Tymoczko JL, Stryer L (2002). Biochemistry (5th ed.). New York: W H Freeman. ISBN 978-0-7167-3051-4.
- Berg JM, Tymoczko JL, Stryer L (2011). Biochemistry (7th ed.). New York: W H Freeman. ISBN 978-1-4292-7635-1.
- Schmidt-Nielsen K (1997). Animal Physiology: Adaptation and Environment (Fifth ed.). Cambridge, UK: Cambridge University Press. ISBN 978-0-521-57098-5.
- López-Herce J, Borrego R, Bustinza A, Carrillo A (September 2005). "Elevated carboxyhemoglobin associated with sodium nitroprusside treatment". Intensive Care Medicine. 31 (9): 1235–8. doi:10.1007/s00134-005-2718-x. PMID 16041521.
- Roth D, Hubmann N, Havel C, Herkner H, Schreiber W, Laggner A (June 2011). "Victim of carbon monoxide poisoning identified by carbon monoxide oximetry". The Journal of Emergency Medicine. 40 (6): 640–2. doi:10.1016/j.jemermed.2009.05.017. PMID 19615844.
- Kolata G (26 January 1993). "Carbon Monoxide Gas Is Used by Brain Cells As a Neurotransmitter". The New York Times.
- Verma A, Hirsch DJ, Glatt CE, Ronnett GV, Snyder SH (January 1993). "Carbon monoxide: a putative neural messenger". Science. 259 (5093): 381–4. doi:10.1126/science.7678352. PMID 7678352.
- Li L, Hsu A, Moore PK (September 2009). "Actions and interactions of nitric oxide, carbon monoxide and hydrogen sulphide in the cardiovascular system and in inflammation--a tale of three gases!". Pharmacology & Therapeutics. 123 (3): 386–400. doi:10.1016/j.pharmthera.2009.05.005. PMID 19486912.
- Johnson CY (October 16, 2009). "Poison gas may carry a medical benefit". The Boston Globe. Retrieved October 16, 2009.
External links
- Carboxyhemoglobin at the US National Library of Medicine Medical Subject Headings (MeSH)