Macular degeneration
Macular degeneration, also known as age-related macular degeneration (AMD or ARMD), is a medical condition which may result in blurred or no vision in the center of the visual field.[1] Early on there are often no symptoms.[1] Over time, however, some people experience a gradual worsening of vision that may affect one or both eyes.[1] While it does not result in complete blindness, loss of central vision can make it hard to recognize faces, drive, read, or perform other activities of daily life.[1] Visual hallucinations may also occur but these do not represent a mental illness.[1]
| Macular degeneration | |
|---|---|
| Other names | Age-related macular degeneration |
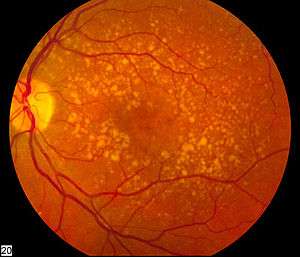 | |
| Picture of the back of the eye showing intermediate age-related macular degeneration | |
| Specialty | Ophthalmology |
| Symptoms | Blurred or no vision in the center of the visual field[1] |
| Complications | Visual hallucinations[1] |
| Usual onset | Older people[1] |
| Types | Early, intermediate, late[1] |
| Causes | Damage to the macula of the retina[1] |
| Risk factors | Genetics, smoking[1] |
| Diagnostic method | Eye examination[1] |
| Prevention | Exercising, eating well, not smoking[1] |
| Treatment | Anti-VEGF medication injected into the eye, laser coagulation, photodynamic therapy[1] |
| Frequency | 6.2 million (2015)[2] |
Macular degeneration typically occurs in older people.[1] Genetic factors and smoking also play a role.[1] It is due to damage to the macula of the retina.[1] Diagnosis is by a complete eye exam.[1] The severity is divided into early, intermediate, and late types.[1] The late type is additionally divided into "dry" and "wet" forms with the dry form making up 90% of cases.[1][3]
Preventive efforts include exercising, eating well, and not smoking.[1] There is no cure or treatment that returns vision already lost.[1] In the wet form, anti-VEGF medication injected into the eye or less commonly laser coagulation or photodynamic therapy may slow worsening.[1] Antioxidant vitamins and minerals do not appear to be useful for prevention.[4] However, dietary supplements may slow the progression in those who already have the disease.[5]
In 2015 it affected 6.2 million people globally.[2] In 2013 it was the fourth most common cause of blindness after cataracts, preterm birth, and glaucoma.[6] It most commonly occurs in people over the age of fifty and in the United States is the most common cause of vision loss in this age group.[1][3] About 0.4% of people between 50 and 60 have the disease, while it occurs in 0.7% of people 60 to 70, 2.3% of those 70 to 80, and nearly 12% of people over 80 years old.[3]
Signs and symptoms


Signs and symptoms of macular degeneration include:
- Visual symptoms
- Distorted vision in the form of metamorphopsia, in which a grid of straight lines appears wavy and parts of the grid may appear blank: Patients often first notice this when looking at things like miniblinds in their home or telephone poles while driving. There may also be central scotomas, shadows or missing areas of vision
- Slow recovery of visual function after exposure to bright light (photostress test)
- Visual acuity drastically decreasing (two levels or more), e.g.: 20/20 to 20/80
- Blurred vision: Those with nonexudative macular degeneration may be asymptomatic or notice a gradual loss of central vision, whereas those with exudative macular degeneration often notice a rapid onset of vision loss (often caused by leakage and bleeding of abnormal blood vessels).
- Trouble discerning colors, specifically dark ones from dark ones and light ones from light ones
- A loss in contrast sensitivity
- Formed visual hallucinations and flashing lights have also been associated with severe visual loss secondary to wet AMD [8]
Macular degeneration by itself will not lead to total blindness. For that matter, only a small number of people with visual impairment are totally blind. In almost all cases, some vision remains, mainly peripheral. Other complicating conditions may lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.[9]
The area of the macula comprises only about 2.1% of the retina, and the remaining 97.9% (the peripheral field) remains unaffected by the disease. Even though the macula provides such a small fraction of the visual field, almost half of the visual cortex is devoted to processing macular information.[10]
The loss of central vision profoundly affects visual functioning. It is quite difficult, for example, to read without central vision. Pictures that attempt to depict the central visual loss of macular degeneration with a black spot do not do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters six inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this difficult to do.
In addition, people with dry macular degeneration often do not experience any symptoms but can experience gradual onset of blurry vision in one or both eyes.[11][12] People with wet macular degeneration may experience acute onset of visual symptoms.[11][12]
Risk factors
- Aging: Advanced age is the strongest predictor of AMD, particularly over 50.[13]
- Family history:
Environment and lifestyle
- Smoking: Smoking tobacco increases the risk of AMD by two to three times that of someone who has never smoked, and may be the most important modifiable factor in its prevention. A review of previous studies found "a strong association between current smoking and AMD. ... Cigarette smoking is likely to have toxic effects on the retina."[14]
- Hypertension (high blood pressure): In the ALIENOR study 2013, early and late AMD were not significantly associated with systolic or diastolic blood pressure (BP), hypertension, or use of antihypertensive medications, but elevated pulse pressure [(PP) systolic BP minus diastolic BP] was significantly associated with an increased risk of late AMD.[15]
- Atherosclerosis[16]
- High cholesterol: Elevated cholesterol may increase the risk of AMD[17]
- Obesity: Abdominal obesity is a risk factor, especially among men[18]
- Fat intake: Consuming high amounts of certain fats, including saturated fats, trans fats, and omega-6 fatty acids, likely contributes to AMD, while monounsaturated fats are potentially protective.[19] In particular, omega-3 fatty acids may decrease the risk of AMD.[20]
- Exposure to UV light from sunlight has been associated with an increased risk of developing AMD, although evidence is weaker than other causes.[12][21]
- Digital screen does not radiate harmful energy against human eyes, but staring at the screen for a long time without pauses does increase eye strain. There is no evidence to support the claim that exposure to digital screen contributes to the risk of macular degeneration.[21][12][22]
Genetics
Recurrence ratios for siblings of an affected individual are three- to sixfold higher than in the general population.[23] Genetic linkage analysis has identified 5 sets of gene variants at three locations on different chromosomes (1, 6 and 10) as explaining at least 50% of the risk. These genes have roles regulating the immune response, inflammatory processes and homeostasis of the retina. Variants of these genes give rise to different kinds of dysfunction in these processes. Over time, this results in accumulation of intracellular and extracellular metabolic debris. This can cause scarring of the retina or breakdown of its vascularization.
Genetic tests are available for some of these gene variations. However, pathogenesis of macular degeneration is a complex interaction between genetics, environment and lifestyle, and presence of unfavorable genetic factors doesn't necessarily predict progression to disease. The three loci where identified gene variants are found are designated:
- Complement Factor H (CFH) on chromosome 1 at location 1q31.3[24]
- HTRA serine peptidase 1/Age Related Maculopathy Susceptibility 2 (HTRA1/ARMS2) on chromosome 10 at location 10q26
- Complement Factor B/Complement Component 2 (CFB/CC2) on chromosome 6 at 6p21.3
Specific genes
- Polymorphisms in genes for complement system proteins: The genes for the complement system proteins factor H (CFH), factor B (CFB) and factor 3 (C3) are strongly associated with a person's risk for developing AMD. CFH is involved in inhibiting the inflammatory response. The mutation in CFH (Y402H) results in reduced ability of CFH to regulate complement on critical surfaces such as the retina and leads to increased inflammatory response within the macula. Absence of the complement factor H-related genes R3 and R1 protects against AMD.[25][26] Two independent studies in 2007 showed a certain common mutation Arg80Gly in the C3 gene, which is a central protein of the complement system, is strongly associated with the occurrence of AMD.[27][28] The authors of both papers consider their study to underscore the influence of the complement pathway in the pathogenesis of this disease.
- In two 2006 studies, another gene that has implications for the disease, called HTRA1 (encoding a secreted serine protease), was identified.[29][30]
- Six mutations of the gene SERPING1 (Serpin Peptidase Inhibitor, Clade G (C1 Inhibitor), Member 1) are associated with AMD. Mutations in this gene can also cause hereditary angioedema.[31]
- Fibulin-5 mutation: Rare forms of the disease are caused by genetic defects in fibulin-5, in an autosomal dominant manner. In 2004, Stone et al. performed a screen on 402 AMD patients and revealed a statistically significant correlation between mutations in fibulin-5 and incidence of the disease.
Mitochondrial related gene polymorphisms
such as that in the MT-ND2 molecule, predicts wet AMD.[32][33]
Pathophysiology

The pathogenesis of age-related macular degeneration is not well known, although some theories have been put forward, including oxidative stress, mitochondrial dysfunction, and inflammatory processes.
The imbalance between the production of damaged cellular components and degradation leads to the accumulation of harmful products, for example, intracellular lipofuscin and extracellular drusen. Incipient atrophy is demarcated by areas of retinal pigment epithelium (RPE) thinning or depigmentation that precede geographic atrophy in the early stages of AMD. In advanced stages of AMD, atrophy of the RPE (geographic atrophy) and/or development of new blood vessels (neovascularization) result in the death of photoreceptors and central vision loss.
In the dry (nonexudative) form, cellular debris called drusen accumulates between the retina and the choroid, causing atrophy and scarring to the retina. In the wet (exudative) form, which is more severe, blood vessels grow up from the choroid (neovascularization) behind the retina which can leak exudate and fluid and also cause hemorrhaging.
Early work demonstrated a family of immune mediators was plentiful in drusen.[34] Complement factor H (CFH) is an important inhibitor of this inflammatory cascade, and a disease-associated polymorphism in the CFH gene strongly associates with AMD.[35][36][37][38][39] Thus an AMD pathophysiological model of chronic low grade complement activation and inflammation in the macula has been advanced.[40][41] Lending credibility to this has been the discovery of disease-associated genetic polymorphisms in other elements of the complement cascade including complement component 3 (C3).[42]
A powerful predictor of AMD is found on chromosome 10q26 at LOC 387715. An insertion/deletion polymorphism at this site reduces expression of the ARMS2 gene though destabilization of its mRNA through deletion of the polyadenylation signal.[43] ARMS2 protein may localize to the mitochondria and participate in energy metabolism, though much remains to be discovered about its function.
Other gene markers of progression risk includes tissue inhibitor of metalloproteinase 3 (TIMP3), suggesting a role for extracellular matrix metabolism in AMD progression.[44] Variations in cholesterol metabolising genes such as the hepatic lipase, cholesterol ester transferase, lipoprotein lipase and the ATP-binding cassette A1 correlate with disease progression. The early stigmata of disease, drusen, are rich in cholesterol, offering face validity to the results of genome-wide association studies.[45]
Stages
In AMD there is a progressive accumulation of characteristic yellow deposits, called drusen (buildup of extracellular proteins and lipids), in the macula (a part of the retina), between the retinal pigment epithelium and the underlying choroid. This accumulation is believed to damage the retina over time. Amyloid beta, which builds up in Alzheimer's disease brains, is one of the proteins that accumulate in AMD, which is a reason why AMD is sometimes called "Alzheimer's of the eye" or "Alzheimer's of the retina".[46] AMD can be divided into 3 stages: early, intermediate, and late, based partially on the extent (size and number) of drusen.[1]
AMD-like pathology begins with small yellow deposits (drusen) in the macula, between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) still have good vision. People with drusen may or may not develop AMD. In fact, the majority of people over age 60 have drusen with no adverse effects. The risk of developing symptoms is higher when the drusen are large and numerous, and associated with the disturbance in the pigmented cell layer under the macula. Large and soft drusen are thought to be related to elevated cholesterol deposits.
Early AMD
Early AMD is diagnosed based on the presence of medium-sized drusen, about the width of an average human hair. Early AMD is usually asymptomatic.[1]
Intermediate AMD
Intermediate AMD is diagnosed by large drusen and/or any retinal pigment abnormalities. Intermediate AMD may cause some vision loss, but, like early AMD, it is usually asymptomatic.[1][47]
Late AMD
In late AMD, enough retinal damage occurs that, in addition to drusen, people will also begin to experience symptomatic central vision loss. The damage can either be the development of atrophy or the onset of neovascular disease. Late AMD is further divided into two subtypes based on the types of damage: Geographic atrophy and Wet AMD (also called Neovascular AMD).[47][1]
Dry AMD
Dry AMD (also called nonexudative AMD) is a broad designation, encompassing all forms of AMD that are not neovascular (wet AMD). This includes early and intermediate forms of AMD, as well as the advanced form of dry AMD known as geographic atrophy. Dry AMD patients tend to have minimal symptoms in the earlier stages; visual function loss occurs more often if the condition advances to geographic atrophy. Dry AMD accounts for 80–90% of cases and tends to progress slowly. In 10–20% of people, dry AMD progresses to the wet type.
Geographic atrophy
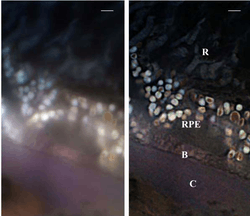
Geographic atrophy (also called atrophic AMD) is an advanced form of AMD in which progressive and irreversible loss of retinal cells leads to a loss of visual function. There are multiple layers that make up the retina, and in geographic atrophy, there are three specific layers that undergo atrophy: the choriocapillaris, retinal pigment epithelium, and the overlying photoreceptors.
The three layers that undergo atrophy in geographic atrophy are all adjacent to each other. The photoreceptors are the most superficial and they are the cells that are responsible for converting energy from the light from the outside world, into an electrical signal to be sent to the brain. There are several functions of the retinal pigment epithelium. One of the main functions of the retinal pigment epithelium is to minimize oxidative stress. It does so by absorbing light, and thus preventing it from getting to the underlying layers. The layers underlying the retinal pigment epithelium are very vascularlized so they have very high oxygen tension. Thus, if light was to get to those layers, many free radicals would form and cause damage to nearby tissues. The deepest layer that undergoes atrophy in geographic atrophy is called the choriocappilaris. It is a capillary network that provides nutrients to the retinal pigment epithelium.
The pathophysiology of geographic atrophy is still uncertain. Some studies questioned whether it was due to a deficient retinal pigment epithelium, leading to increased oxidative stress.[48] Other studies have looked for inflammatory causes of damage.[49] Thus far, the medical community is still not certain. Recent studies have begun to look at each layer individually. They found that decrease blood flow in the choriocapillaris precedes atrophy of the retinal pigment epithelium and the overlying photoreceptors.[50] Since the choriocapillaris is a vascular layer, this maybe be used as an arugment for why geographic atrophy could be a disease due to decreased blood flow.
Wet AMD
Neovascular or exudative AMD, the "wet" form of advanced AMD, causes vision loss due to abnormal blood vessel growth (choroidal neovascularization) in the choriocapillaris, through Bruch's membrane. It is usually, but not always, preceded by the dry form of AMD. The proliferation of abnormal blood vessels in the retina is stimulated by vascular endothelial growth factor (VEGF). Because these blood vessels are abnormal, these are also more fragile than typical blood vessels, which ultimately leads to blood and protein leakage below the macula. Bleeding, leaking, and scarring from these blood vessels eventually cause irreversible damage to the photoreceptors and rapid vision loss if left untreated.
Oxidative stress
Age-related accumulation of low-molecular-weight, phototoxic, pro-oxidant melanin oligomers within lysosomes in the retinal pigment epithelium (RPE) may be partly responsible for decreasing the digestive rate of photoreceptor outer rod segments (POS) by the RPE – autophagy. A decrease in the digestive rate of POS has been shown to be associated with lipofuscin formation – a classic sign associated with AMD.[51][52]
The role of retinal oxidative stress in the cause of AMD by resulting in further inflammation of the macula is suggested by the enhanced rate of disease in smokers and those exposed to UV irradiation.[14][53][54]
Mitochondrial dysfunction may play a role.[55]
Diagnosis
Diagnosis of age-related macular degeneration depends on signs in the macula, not necessarily vision.[56] Wet AMD is typically the advanced progression of dry AMD and will require additional diagnostic tools. Additionally, early diagnosis of wet AMD can prevent further visual deterioration and potentially improve vision.[56]
Diagnosis of dry (or early stage) AMD may include the following clinical examinations as well as procedures and tests:
- The transition from dry to wet AMD can happen rapidly, and if it is left untreated can lead to legal blindness in as little as six months. To prevent this from occurring and to initiate preventive strategies earlier in the disease process, dark adaptation testing may be performed. A dark adaptometer can detect subclinical AMD at least three years earlier than it is clinically evident.[57][57]
- There is a loss of contrast sensitivity, so that contours, shadows, and color vision are less vivid. The loss in contrast sensitivity can be quickly and easily measured by a contrast sensitivity test like Pelli Robson performed either at home or by an eye specialist.
- When viewing an Amsler grid, some straight lines appear wavy and some patches appear blank
- When viewing a Snellen chart, at least 2 lines decline
- In dry macular degeneration, which occurs in 85–90 percent of AMD cases, drusen spots can be seen in Fundus photography
- Using an electroretinogram, points in the macula with a weak or absent response compared to a normal eye may be found
- Farnsworth-Munsell 100 hue test and Maximum Color Contrast Sensitivity test (MCCS) for assessing color acuity and color contrast sensitivity
- Optical coherence tomography is now used by most ophthalmologists in the diagnosis and the follow-up evaluation of the response to treatment with antiangiogenic drugs.
Diagnosis of wet (or late stage) AMD may include the following in addition to the above tests:
- Preferential hyperacuity perimetry changes (for wet AMD). Preferential hyperacuity perimetry is a test that detects drastic changes in vision and involves the macula being stimulated with distorted patterns of dots and the patient identification of where in the visual field this occurs.[58]
- In wet macular degeneration, angiography can visualize the leakage of bloodstream behind the macula. Fluorescein angiography allows for the identification and localization of abnormal vascular processes.
Histology
- Pigmentary changes in the retina – In addition to the pigmented cells in the iris (the colored part of the eye), there are pigmented cells beneath the retina. As these cells break down and release their pigment, dark clumps of released pigment and later, areas that are less pigmented may appear
- Exudative changes: hemorrhages in the eye, hard exudates, subretinal/sub-RPE/intraretinal fluid
- Drusen, tiny accumulations of extracellular material that build up on the retina. While there is a tendency for drusen to be blamed for the progressive loss of vision, drusen deposits can be present in the retina without vision loss. Some patients with large deposits of drusen have normal visual acuity. If normal retinal reception and image transmission are sometimes possible in a retina when high concentrations of drusen are present, then, even if drusen can be implicated in the loss of visual function, there must be at least one other factor that accounts for the loss of vision.
Prevention
A 2017 Cochrane review found the use of vitamin and mineral supplements, alone or in combination, by the general population did not affect whether or not AMD started.[4]
Management
Treatment of AMD varies depending on the category of the disease at the time of diagnosis. In general, treatment is aimed at slowing down the progression of AMD.[59] As of 2018, there are no treatments to reverse the effects of AMD.[59] Early-stage and intermediate-stage AMD is managed by modifying known risk factors such as smoking and atherosclerosis and making dietary modifications.[59] For intermediate-stage AMD, management also includes antioxidant and mineral supplementation.[59][60][61] Advanced-stage AMD is managed based on the presence of choroidal neovascularization (CNV): dry AMD (no CNV present) or wet AMD (CNV present).[59] No effective treatments exist for dry AMD.[59] The CNV present in wet AMD is managed with vascular endothelial growth factor (VEGF) inhibitors.[59][62][61]
Dry AMD
No medical or surgical treatment is available for this condition.
Wet AMD
Ranibizumab, aflibercept, and brolucizumab are approved VEGF inhibitors for the treatment of CNV in wet AMD.[62][63] All three drugs are administered via intravitreal injection, meaning they are injected directly into the eye. Bevacizumab is another VEGF inhibitor that has been shown to have similar efficacy and safety as the previous two drugs, however, is not currently indicated for AMD.[61] AMD can also be treated with laser coagulation therapy.[64]
A randomized control trial found that bevacizumab and ranibizumab had similar efficacy, and reported no significant increase in adverse events with bevacizumab.[65] A 2014 Cochrane review found that the systemic safety of bevacizumab and ranibizumab are similar when used to treat neovascular AMD, except for gastrointestinal disorders.[66] Bevacizumab however is not FDA approved for treatment of macular degeneration. A controversy in the UK involved the off-label use of cheaper bevacizumab over the approved, but expensive, ranibizumab.[67] Ranibizumab is a smaller fragment, Fab fragment, of the parent bevacizumab molecule specifically designed for eye injections. Other approved antiangiogenic drugs for the treatment of neo-vascular AMD include pegaptanib[68] and aflibercept.[69]
The American Academy of Ophthalmology practice guidelines do not recommend laser coagulation therapy for macular degeneration, but state that it may be useful in people with new blood vessels in the choroid outside of the fovea who don't respond to drug treatment.[70][71] There is strong evidence that laser coagulation will result in the disappearance of drusen but does not affect choroidal neovascularisation.[72] A 2007 Cochrane review on found that laser photocoagulation of new blood vessels in the choroid outside of the fovea is effective and economical method, but that the benefits are limited for vessels next to or below the fovea.[73]
Photodynamic therapy has also been used to treat wet AMD.[74] The drug verteporfin is administered intravenously; light of a certain wavelength is then applied to the abnormal blood vessels. This activates the verteporfin destroying the vessels.
Cataract surgery could improve visual outcomes for people with AMD, though there have been concerns about surgery increasing the progression of AMD. A randomized controlled trial found that people who underwent immediate cataract surgery (within two weeks) had improved visual acuity and better quality of life outcomes than those who underwent delayed cataract surgery (6 months).[75]
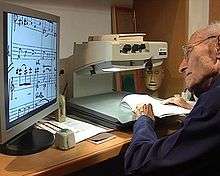
Adaptive devices
Because peripheral vision is not affected, people with macular degeneration can learn to use their remaining vision to partially compensate.[76] Assistance and resources are available in many countries and every state in the U.S.[77] Classes for "independent living" are given and some technology can be obtained from a state department of rehabilitation.
Adaptive devices can help people read. These include magnifying glasses, special eyeglass lenses, computer screen readers, and TV systems that enlarge reading the material.
Computer screen readers such as JAWS or Thunder work with standard Windows computers. Also, Apple devices provide a wide range of features (voice-over, screen readers, Braille etc.).
Video cameras can be fed into standard or special-purpose computer monitors, and the image can be zoomed in and magnified. These systems often include a movable table to move the written material.
Accessible publishing provides larger fonts for printed books, patterns to make tracking easier, audiobooks and DAISY books with both text and audio.
Epidemiology
_world_map_-_DALY_-_WHO2004.svg.png)
The prevalence any age-related macular degeneration is higher in Europeans than in Asians and Africans.[79] There is no difference in prevalence between Asians and Africans. The incidence of age-related macular degeneration and its associated features increases with age and is low in people <55 years of age.[80] Smoking is the strongest modifiable risk factor.[81] Age-related macular degeneration accounts for more than 54% of all vision loss in the white population in the USA. An estimated 8 million Americans are affected with early age-related macular degeneration, of whom over 1 million will develop advanced age-related macular degeneration within the next 5 years. In the UK, age-related macular degeneration is the cause of blindness in almost 42% of those who go blind aged 65–74 years, almost two-thirds of those aged 75–84 years, and almost three-quarters of those aged 85 years or older.
Research directions
Association with other age-related diseases
Studies indicate drusen associated with AMD are similar in molecular composition to Beta-Amyloid (βA) plaques and deposits in other age-related diseases such as Alzheimer's disease and atherosclerosis. This suggests that similar pathways may be involved in the etiologies of AMD and other age-related diseases.[82]
Other types
There are a few other (rare) kinds of macular degeneration with similar symptoms but unrelated in etiology to Wet or Dry age-related macular degeneration. They are all genetic disorders that may occur in childhood or middle age.
- Vitelliform macular dystrophy
- Sorsby's fundus dystrophy is an autosomal dominant, retinal disease characterized by sudden acuity loss resulting from untreatable submacular neovascularisation
- Stargardt's disease (juvenile macular degeneration, STGD) is an autosomal recessive retinal disorder characterized by juvenile-onset macular dystrophy, alterations of the peripheral retina, and subretinal deposition of lipofuscin-like material.
Similar symptoms with a very different etiology and different treatment can be caused by epiretinal membrane or macular pucker or any other condition affecting the macula, such as central serous retinopathy.
Notable cases
References
- "Facts About Age-Related Macular Degeneration". National Eye Institute. June 2015. Archived from the original on 22 December 2015. Retrieved 21 December 2015.
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". The Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Mehta S (September 2015). "Age-Related Macular Degeneration". Primary Care. 42 (3): 377–91. doi:10.1016/j.pop.2015.05.009. PMID 26319344.
- Evans JR, Lawrenson JG (July 2017). "Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration". The Cochrane Database of Systematic Reviews. 7: CD000253. doi:10.1002/14651858.CD000253.pub4. PMC 6483250. PMID 28756617.
- Evans JR, Lawrenson JG (July 2017). "Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration". The Cochrane Database of Systematic Reviews. 7: CD000254. doi:10.1002/14651858.CD000254.pub4. PMC 6483465. PMID 28756618.
- Vos, Theo; Barber, Ryan M.; Bell, Brad; Bertozzi-Villa, Amelia; Biryukov, Stan; Bolliger, Ian; Charlson, Fiona; Davis, Adrian; Degenhardt, Louisa; Dicker, Daniel; Duan, Leilei; Erskine, Holly; Feigin, Valery L.; Ferrari, Alize J.; Fitzmaurice, Christina; Fleming, Thomas; Graetz, Nicholas; Guinovart, Caterina; Haagsma, Juanita; Hansen, Gillian M.; Hanson, Sarah Wulf; Heuton, Kyle R.; Higashi, Hideki; Kassebaum, Nicholas; Kyu, Hmwe; Laurie, Evan; Liang, Xiofeng; Lofgren, Katherine; Lozano, Rafael; et al. (August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". The Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- "Wayback Machine". 22 October 2013. Archived from the original on 2013-10-22. Retrieved 5 November 2018.
- "Age-Related Macular Degeneration PPP - Updated 2015". American Academy of Ophthalmology. 2015-01-29. Retrieved 2018-11-13.
- Roberts, DL (September 2006). "The First Year – Age Related Macular Degeneration". Marlowe & Company: 100.
- Roberts, DL (September 2006). "The First Year – Age Related Macular Degeneration". Marlowe & Company: 20.
- Cunningham J (March 2017). "Recognizing age-related macular degeneration in primary care". JAAPA. 30 (3): 18–22. doi:10.1097/01.jaa.0000512227.85313.05. PMID 28151737.
- Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY (May 2012). "Age-related macular degeneration". The Lancet. 379 (9827): 1728–38. doi:10.1016/S0140-6736(12)60282-7. PMID 22559899.
- Deangelis MM, Silveira AC, Carr EA, Kim IK (May 2011). "Genetics of age-related macular degeneration: current concepts, future directions". Seminars in Ophthalmology. 26 (3): 77–93. doi:10.3109/08820538.2011.577129. PMC 4242505. PMID 21609220.
- Thornton J, Edwards R, Mitchell P, Harrison RA, Buchan I, Kelly SP (September 2005). "Smoking and age-related macular degeneration: a review of association". Eye. 19 (9): 935–44. doi:10.1038/sj.eye.6701978. PMID 16151432.
- Cougnard-Grégoire A, Delyfer MN, Korobelnik JF, Rougier MB, Malet F, Le Goff M, et al. (March 2013). "Long-term blood pressure and age-related macular degeneration: the ALIENOR study". Investigative Ophthalmology & Visual Science. 54 (3): 1905–12. doi:10.1167/iovs.12-10192. PMID 23404120.
- García-Layana A, Cabrera-López F, García-Arumí J, Arias-Barquet L, Ruiz-Moreno JM (October 2017). "Early and intermediate age-related macular degeneration: update and clinical review". Clinical Interventions in Aging. 12: 1579–1587. doi:10.2147/cia.s142685. PMC 5633280. PMID 29042759.
- Dasari B, Prasanthi JR, Marwarha G, Singh BB, Ghribi O (August 2011). "Cholesterol-enriched diet causes age-related macular degeneration-like pathology in rabbit retina". BMC Ophthalmology. 11: 22. doi:10.1186/1471-2415-11-22. PMC 3170645. PMID 21851605.
- Adams MK, Simpson JA, Aung KZ, Makeyeva GA, Giles GG, English DR, Hopper J, Guymer RH, Baird PN, Robman LD (June 2011). "Abdominal obesity and age-related macular degeneration". American Journal of Epidemiology. 173 (11): 1246–55. doi:10.1093/aje/kwr005. PMID 21422060.
- Parekh N, Voland RP, Moeller SM, Blodi BA, Ritenbaugh C, Chappell RJ, et al. (November 2009). "Association between dietary fat intake and age-related macular degeneration in the Carotenoids in Age-Related Eye Disease Study (CAREDS): an ancillary study of the Women's Health Initiative". Archives of Ophthalmology. 127 (11): 1483–93. doi:10.1001/archophthalmol.2009.130. PMC 3144752. PMID 19901214.
- SanGiovanni JP, Chew EY, Clemons TE, Davis MD, Ferris FL, Gensler GR, et al. (May 2007). "The relationship of dietary lipid intake and age-related macular degeneration in a case-control study: AREDS Report No. 20". Archives of Ophthalmology. 125 (5): 671–9. doi:10.1001/archopht.125.5.671. PMID 17502507.
- Arunkumar R, Calvo CM, Conrady CD, Bernstein PS (May 2018). "What do we know about the macular pigment in AMD: the past, the present, and the future". Eye. 32 (5): 992–1004. doi:10.1038/s41433-018-0044-0. PMC 5944649. PMID 29576617.
- "Are Computer Glasses Worth It?". American Academy of Ophthalmology. 2017-04-27. Retrieved 2020-02-02.
- Maller J, George S, Purcell S, Fagerness J, Altshuler D, Daly MJ, Seddon JM (September 2006). "Common variation in three genes, including a noncoding variant in CFH, strongly influences risk of age-related macular degeneration". Nature Genetics. 38 (9): 1055–9. doi:10.1038/ng1873. PMID 16936732.
- Edwards AO, Ritter R, Abel KJ, Manning A, Panhuysen C, Farrer LA (April 2005). "Complement factor H polymorphism and age-related macular degeneration". Science. 308 (5720): 421–4. Bibcode:2005Sci...308..421E. doi:10.1126/science.1110189. PMID 15761121.
- Hughes AE, Orr N, Esfandiary H, Diaz-Torres M, Goodship T, Chakravarthy U (October 2006). "A common CFH haplotype, with deletion of CFHR1 and CFHR3, is associated with lower risk of age-related macular degeneration". Nature Genetics. 38 (10): 1173–7. doi:10.1038/ng1890. PMID 16998489.
- Fritsche LG, Lauer N, Hartmann A, Stippa S, Keilhauer CN, Oppermann M, et al. (December 2010). "An imbalance of human complement regulatory proteins CFHR1, CFHR3 and factor H influences risk for age-related macular degeneration (AMD)". Human Molecular Genetics. 19 (23): 4694–704. doi:10.1093/hmg/ddq399. PMID 20843825.
- Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H, et al. (August 2007). "Complement C3 variant and the risk of age-related macular degeneration". The New England Journal of Medicine. 357 (6): 553–61. doi:10.1056/NEJMoa072618. PMID 17634448.
- Maller JB, Fagerness JA, Reynolds RC, Neale BM, Daly MJ, Seddon JM (October 2007). "Variation in complement factor 3 is associated with risk of age-related macular degeneration". Nature Genetics. 39 (10): 1200–1. doi:10.1038/ng2131. PMID 17767156.
- Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ, et al. (November 2006). "A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration". Science. 314 (5801): 992–3. Bibcode:2006Sci...314..992Y. doi:10.1126/science.1133811. PMID 17053109.
- Dewan A, Liu M, Hartman S, Zhang SS, Liu DT, Zhao C, Tam PO, Chan WM, Lam DS, Snyder M, Barnstable C, Pang CP, Hoh J (November 2006). "HTRA1 promoter polymorphism in wet age-related macular degeneration". Science. 314 (5801): 989–92. Bibcode:2006Sci...314..989D. doi:10.1126/science.1133807. PMID 17053108.
- Hirschler, Ben (2008-10-07). "Gene discovery may help hunt for blindness cure". Reuters. Archived from the original on October 11, 2008. Retrieved 2008-10-07.
- Udar N, Atilano SR, Memarzadeh M, Boyer DS, Chwa M, Lu S, Maguen B, Langberg J, Coskun P, Wallace DC, Nesburn AB, Khatibi N, Hertzog D, Le K, Hwang D, Kenney MC (June 2009). "Mitochondrial DNA haplogroups associated with age-related macular degeneration". Investigative Ophthalmology & Visual Science. 50 (6): 2966–74. doi:10.1167/iovs.08-2646. PMID 19151382.
- Canter JA, Olson LM, Spencer K, Schnetz-Boutaud N, Anderson B, Hauser MA, Schmidt S, Postel EA, Agarwal A, Pericak-Vance MA, Sternberg P, Haines JL (May 2008). Nicholas Weedon M (ed.). "Mitochondrial DNA polymorphism A4917G is independently associated with age-related macular degeneration". PLOS ONE. 3 (5): e2091. Bibcode:2008PLoSO...3.2091C. doi:10.1371/journal.pone.0002091. PMC 2330085. PMID 18461138.

- Mullins RF, Russell SR, Anderson DH, Hageman GS (May 2000). "Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease". FASEB Journal. 14 (7): 835–46. doi:10.1096/fasebj.14.7.835. PMID 10783137.
- Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI, et al. (May 2005). "A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration". Proceedings of the National Academy of Sciences of the United States of America. 102 (20): 7227–32. doi:10.1073/pnas.0501536102. PMC 1088171. PMID 15870199.
- Chen LJ, Liu DT, Tam PO, Chan WM, Liu K, Chong KK, Lam DS, Pang CP (December 2006). "Association of complement factor H polymorphisms with exudative age-related macular degeneration". Molecular Vision. 12: 1536–42. PMID 17167412.
- Despriet DD, Klaver CC, Witteman JC, Bergen AA, Kardys I, de Maat MP, Boekhoorn SS, Vingerling JR, Hofman A, Oostra BA, Uitterlinden AG, Stijnen T, van Duijn CM, de Jong PT (July 2006). "Complement factor H polymorphism, complement activators, and risk of age-related macular degeneration". JAMA. 296 (3): 301–9. doi:10.1001/jama.296.3.301. PMID 16849663.
- Li M, Atmaca-Sonmez P, Othman M, Branham KE, Khanna R, Wade MS, et al. (September 2006). "CFH haplotypes without the Y402H coding variant show strong association with susceptibility to age-related macular degeneration". Nature Genetics. 38 (9): 1049–54. doi:10.1038/ng1871. PMC 1941700. PMID 16936733.
- Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, Spencer KL, Kwan SY, Noureddine M, Gilbert JR, Schnetz-Boutaud N, Agarwal A, Postel EA, Pericak-Vance MA (April 2005). "Complement factor H variant increases the risk of age-related macular degeneration". Science. 308 (5720): 419–21. Bibcode:2005Sci...308..419H. doi:10.1126/science.1110359. PMID 15761120.
- Rohrer, Bärbel; Long, Qin; Coughlin, Beth; Renner, Brandon; Huang, Yuxiang; Kunchithapautham, Kannan; Ferreira, Viviana P.; Pangburn, Michael K.; Gilkeson, Gary S.; Thurman, Joshua M.; Tomlinson, Stephen; Holers, V. Michael (2010). "A Targeted Inhibitor of the Complement Alternative Pathway Reduces RPE Injury and Angiogenesis in Models of Age-Related Macular Degeneration". Inflammation and Retinal Disease: Complement Biology and Pathology. Advances in Experimental Medicine and Biology. 703. pp. 137–149. doi:10.1007/978-1-4419-5635-4_10. ISBN 978-1-4419-5634-7. PMID 20711712.
- Kunchithapautham K, Rohrer B (July 2011). "Sublytic membrane-attack-complex (MAC) activation alters regulated rather than constitutive vascular endothelial growth factor (VEGF) secretion in retinal pigment epithelium monolayers". The Journal of Biological Chemistry. 286 (27): 23717–24. doi:10.1074/jbc.M110.214593. PMC 3129152. PMID 21566137.
- Yates, John R.W.; Sepp, Tiina; Matharu, Baljinder K.; Khan, Jane C.; Thurlby, Deborah A.; Shahid, Humma; Clayton, David G.; Hayward, Caroline; Morgan, Joanne; Wright, Alan F.; Armbrecht, Ana Maria; Dhillon, Baljean; Deary, Ian J.; Redmond, Elizabeth; Bird, Alan C.; Moore, Anthony T.; Genetic Factors in AMD Study, Group. (9 August 2007). "Complement C3 Variant and the Risk of Age-Related Macular Degeneration". New England Journal of Medicine. 357 (6): 553–561. doi:10.1056/NEJMoa072618. PMID 17634448.
- Fritsche LG, Loenhardt T, Janssen A, Fisher SA, Rivera A, Keilhauer CN, Weber BH (July 2008). "Age-related macular degeneration is associated with an unstable ARMS2 (LOC387715) mRNA". Nature Genetics. 40 (7): 892–6. doi:10.1038/ng.170. PMID 18511946.
- Chen W, Stambolian D, Edwards AO, Branham KE, Othman M, Jakobsdottir J, et al. (April 2010). "Genetic variants near TIMP3 and high-density lipoprotein-associated loci influence susceptibility to age-related macular degeneration". Proceedings of the National Academy of Sciences of the United States of America. 107 (16): 7401–6. Bibcode:2010PNAS..107.7401C. doi:10.1073/pnas.0912702107. PMC 2867722. PMID 20385819.
- Neale BM, Fagerness J, Reynolds R, Sobrin L, Parker M, Raychaudhuri S, Tan PL, Oh EC, Merriam JE, Souied E, Bernstein PS, Li B, Frederick JM, Zhang K, Brantley MA, Lee AY, Zack DJ, Campochiaro B, Campochiaro P, Ripke S, Smith RT, Barile GR, Katsanis N, Allikmets R, Daly MJ, Seddon JM (April 2010). "Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC)". Proceedings of the National Academy of Sciences of the United States of America. 107 (16): 7395–400. Bibcode:2010PNAS..107.7395N. doi:10.1073/pnas.0912019107. PMC 2867697. PMID 20385826.
- Ratnayaka JA, Serpell LC, Lotery AJ (August 2015). "Dementia of the eye: the role of amyloid beta in retinal degeneration". Eye. 29 (8): 1013–26. doi:10.1038/eye.2015.100. PMC 4541342. PMID 26088679.
- Ferris FL, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, Sadda SR (April 2013). "Clinical classification of age-related macular degeneration". Ophthalmology. 120 (4): 844–51. doi:10.1016/j.ophtha.2012.10.036. PMID 23332590.
- X. Shaw, Peter; Stiles, Travis; Douglas, Christopher; Ho, Daisy; Fan, Wei; Du, Hongjun; Xiao, Xu (2016). "Oxidative stress, innate immunity, and age-related macular degeneration". AIMS Molecular Science. 3 (2): 196–221. doi:10.3934/molsci.2016.2.196. PMC 4882104. PMID 27239555.
- Kauppinen, Anu; Paterno, Jussi J.; Blasiak, Janusz; Salminen, Antero; Kaarniranta, Kai (6 February 2016). "Inflammation and its role in age-related macular degeneration". Cellular and Molecular Life Sciences. 73 (9): 1765–1786. doi:10.1007/s00018-016-2147-8. PMC 4819943. PMID 26852158.
- Thulliez, Marie; Zhang, Qinqin; Shi, Yingying; Zhou, Hao; Chu, Zhongdi; de Sisternes, Luis; Durbin, Mary K.; Feuer, William; Gregori, Giovanni; Wang, Ruikang K.; Rosenfeld, Philip J. (June 2019). "Correlations between Choriocapillaris Flow Deficits around Geographic Atrophy and Enlargement Rates Based on Swept-Source OCT Imaging". Ophthalmology Retina. 3 (6): 478–488. doi:10.1016/j.oret.2019.01.024. PMID 31174669.
- Sarangarajan, Rangaprasad; Apte, Shireesh. P. (2005). "Melanin Aggregation and Polymerization: Possible Implications in Age-Related Macular Degeneration". Ophthalmic Research. 37 (3): 136–141. doi:10.1159/000085533. PMID 15867475.
- John Lacey, "Harvard Medical signs agreement with Merck to develop potential therapy for macular degeneration Archived 2007-06-07 at the Wayback Machine", 23 May 2006
- Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD (May 2004). "Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study". Archives of Ophthalmology. 122 (5): 750–7. doi:10.1001/archopht.122.5.750. PMID 15136324.
- Szaflik JP, Janik-Papis K, Synowiec E, Ksiazek D, Zaras M, Wozniak K, Szaflik J, Blasiak J (October 2009). "DNA damage and repair in age-related macular degeneration". Mutation Research. 669 (1–2): 169–76. doi:10.1016/j.mrfmmm.2009.06.008. PMID 19559717.
- Barot M, Gokulgandhi MR, Mitra AK (December 2011). "Mitochondrial dysfunction in retinal diseases". Current Eye Research. 36 (12): 1069–77. doi:10.3109/02713683.2011.607536. PMC 4516173. PMID 21978133.
- National Guideline Alliance (UK) (2018). Age-related macular degeneration: diagnosis and management. National Institute for Health and Care Excellence: Clinical Guidelines. London: National Institute for Health and Care Excellence (UK). ISBN 9781473127876. PMID 29400919.
- Owsley C, McGwin G, Clark ME, Jackson GR, Callahan MA, Kline LB, Witherspoon CD, Curcio CA (February 2016). "Delayed Rod-Mediated Dark Adaptation Is a Functional Biomarker for Incident Early Age-Related Macular Degeneration". Ophthalmology. 123 (2): 344–51. doi:10.1016/j.ophtha.2015.09.041. PMC 4724453. PMID 26522707.
- Faes L, Bodmer NS, Bachmann LM, Thiel MA, Schmid MK (July 2014). "Diagnostic accuracy of the Amsler grid and the preferential hyperacuity perimetry in the screening of patients with age-related macular degeneration: systematic review and meta-analysis". Eye. 28 (7): 788–96. doi:10.1038/eye.2014.104. PMC 4094801. PMID 24788016.
- Bishop P. Age-related macular degeneration. BMJ Best Practice. 2018.
- Evans JR, Lawrenson JG (July 2017). "Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration". The Cochrane Database of Systematic Reviews. 7: CD000253. doi:10.1002/14651858.cd000253.pub4. PMC 6483250. PMID 28756617.
- Lawrenson JG, Evans JR (April 2015). "Omega 3 fatty acids for preventing or slowing the progression of age-related macular degeneration" (PDF). The Cochrane Database of Systematic Reviews (4): CD010015. doi:10.1002/14651858.cd010015.pub3. PMC 7087473. PMID 25856365.
- Sarwar S, Clearfield E, Soliman MK, Sadiq MA, Baldwin AJ, Hanout M, Agarwal A, Sepah YJ, Do DV, Nguyen QD (February 2016). "Aflibercept for neovascular age-related macular degeneration". The Cochrane Database of Systematic Reviews. 2: CD011346. doi:10.1002/14651858.cd011346.pub2. PMC 5030844. PMID 26857947.
- Nguyen, Quan Dong (2020). "Brolucizumab: Evolution through Preclinical and Clinical Studies and the Implications for the Management of Neovascular Age-Related Macular Degeneration". Ophthalmology. doi:10.1016/j.ophtha.2019.12.031. PMID 32107066. Retrieved 17 March 2020.
- Virgili G, Bini A (July 2007). "Laser photocoagulation for neovascular age-related macular degeneration". The Cochrane Database of Systematic Reviews (3): CD004763. doi:10.1002/14651858.cd004763.pub2. PMID 17636773.
- Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Culliford LA, Reeves BC (October 2013). "Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial". The Lancet. 382 (9900): 1258–67. doi:10.1016/S0140-6736(13)61501-9. PMID 23870813.
- Moja L, Lucenteforte E, Kwag KH, Bertele V, Campomori A, Chakravarthy U, D'Amico R, Dickersin K, Kodjikian L, Lindsley K, Loke Y, Maguire M, Martin DF, Mugelli A, Mühlbauer B, Püntmann I, Reeves B, Rogers C, Schmucker C, Subramanian ML, Virgili G (September 2014). Moja L (ed.). "Systemic safety of bevacizumab versus ranibizumab for neovascular age-related macular degeneration". The Cochrane Database of Systematic Reviews. 9 (9): CD011230. doi:10.1002/14651858.CD011230.pub2. hdl:2434/273140. PMC 4262120. PMID 25220133.
- Copley, Caroline; Hirschler, Ben (April 24, 2012). "Novartis challenges UK Avastin use in eye disease". Reuters. Archived from the original on May 22, 2013.
- "FDA Approves New Drug Treatment for Age-Related Macular Degeneration". FDA.gov. U.S. Food and Drug Administration. Archived from the original on 2015-11-20.
- FDA approves Eylea for macular degeneration Archived 2013-05-28 at the Wayback Machine
- "Age-Related Macular Degeneration PPP – Updated 2015". American Academy of Ophthalmology Preferred Practice Pattern. 29 January 2015. Archived from the original on 21 October 2016. Retrieved 22 October 2016.
- Lindsley K, Li T, Ssemanda E, Virgili G, Dickersin K (April 2016). "Interventions for Age-Related Macular Degeneration: Are Practice Guidelines Based on Systematic Reviews?". Ophthalmology. 123 (4): 884–97. doi:10.1016/j.ophtha.2015.12.004. PMC 4808456. PMID 26804762.
- Virgili G, Michelessi M, Parodi MB, Bacherini D, Evans JR (October 2015). "Laser treatment of drusen to prevent progression to advanced age-related macular degeneration". The Cochrane Database of Systematic Reviews. 10 (10): CD006537. doi:10.1002/14651858.CD006537.pub3. PMC 4733883. PMID 26493180.
- Virgili G, Bini A (July 2007). "Laser photocoagulation for neovascular age-related macular degeneration". The Cochrane Database of Systematic Reviews (3): CD004763. doi:10.1002/14651858.CD004763.pub2. PMID 17636773.
- Meads C (2003). "Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation". Health Technology Assessment. 7 (9): v–vi, 1–98. doi:10.3310/hta7090. PMID 12709292.
- Casparis H, Lindsley K, Kuo IC, Sikder S, Bressler NM (February 2017). "Surgery for cataracts in people with age-related macular degeneration". The Cochrane Database of Systematic Reviews. 2: CD006757. doi:10.1002/14651858.CD006757.pub4. PMC 3480178. PMID 28206671.
- "Low Vision Rehabilitation Delivery Model". Mdsupport.org. Archived from the original on 2010-11-07. Retrieved 2011-01-11.
- "Agencies, Centers, Organizations, & Societies". Mdsupport.org. 2005-09-01. Archived from the original on 2011-06-11. Retrieved 2011-01-11.
- "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 2009-11-11. Retrieved Nov 11, 2009.
- Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY (February 2014). "Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis". The Lancet. Global Health. 2 (2): e106–16. doi:10.1016/S2214-109X(13)70145-1. PMID 25104651.
- "Age-related macular degeneration - Symptoms, diagnosis and treatment". BMJ Best Practice. Retrieved 2018-11-13.
- Velilla S, García-Medina JJ, García-Layana A, Dolz-Marco R, Pons-Vázquez S, Pinazo-Durán MD, Gómez-Ulla F, Arévalo JF, Díaz-Llopis M, Gallego-Pinazo R (2013). "Smoking and age-related macular degeneration: review and update". Journal of Ophthalmology. 2013: 895147. doi:10.1155/2013/895147. PMC 3866712. PMID 24368940.
- Mullins RF, Russell SR, Anderson DH, Hageman GS, et al. (May 2000). "Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease". FASEB Journal. 14 (7): 835–46. doi:10.1096/fasebj.14.7.835. PMID 10783137.
- John S, Natarajan S, Parikumar P, Shanmugam PM, Senthilkumar R, Green DW, Abraham SJ (2013). "Choice of Cell Source in Cell-Based Therapies for Retinal Damage due to Age-Related Macular Degeneration: A Review". Journal of Ophthalmology. 2013: 1–9. doi:10.1155/2013/465169. PMC 3654320. PMID 23710332.
- Carr AJ, Smart MJ, Ramsden CM, Powner MB, da Cruz L, Coffey PJ (July 2013). "Development of human embryonic stem cell therapies for age-related macular degeneration". Trends in Neurosciences. 36 (7): 385–95. doi:10.1016/j.tins.2013.03.006. PMID 23601133.
- "Judi Dench 'can't read any more due to failing eyesight Archived 2016-10-19 at the Wayback Machine", The Guardian, 23 February 2014
- "Joan bows out to a standing ovation Archived 2016-04-20 at the Wayback Machine", The Guardian, 13 May 2014
- "Patrons of the Macular Society Archived 2013-02-08 at the Wayback Machine", Macular Society. (notable for doing the voice of Wallace from Wallace and Gromit until 2012)
External links
| Classification | |
|---|---|
| External resources |