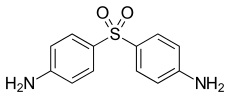
Dapsone
Dapsone, also known as diaminodiphenyl sulfone (DDS),[2] is an antibiotic commonly used in combination with rifampicin and clofazimine for the treatment of leprosy.[3] It is a second-line medication for the treatment and prevention of pneumocystis pneumonia and for the prevention of toxoplasmosis in those who have poor immune function.[3] Additionally, it has been used for acne, dermatitis herpetiformis, and various other skin conditions.[4] Dapsone is available both topically and by mouth.[5]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Aczone, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682128 |
| License data | |
| Pregnancy category | |
| Routes of administration | By mouth, topical |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 70 to 80% |
| Protein binding | 70 to 90% |
| Metabolism | Liver (mostly CYP2E1-mediated) |
| Elimination half-life | 20 to 30 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.001.136 |
| Chemical and physical data | |
| Formula | C12H12N2O2S |
| Molar mass | 248.30 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 175 to 176 °C (347 to 349 °F) |
| |
| |
| (verify) | |
Severe side effects may include a decrease in blood cells, red blood cell breakdown especially in those with glucose-6-phosphate dehydrogenase deficiency (G-6-PD), or hypersensitivity.[3] Common side effects include nausea and loss of appetite.[5] Other side effects include liver inflammation and a number of types of skin rashes.[3] While the safety of use during pregnancy is not entirely clear some physicians recommend that it be continued in those with leprosy.[3] It is of the sulfone class.[3]
Dapsone was first studied as an antibiotic in 1937.[4] Its use for leprosy began in 1945.[4] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[6] The form, which is taken by mouth, is available as a generic drug and not very expensive.[3][7]
Medical uses
Infections
Dapsone is commonly used in combination with rifampicin and clofazimine for the treatment of leprosy.[3] It is also used to both treat and prevent pneumocystis pneumonia (PCP).[3][8] It is also used for toxoplasmosis in people unable to tolerate trimethoprim with sulfamethoxazole.[8]
Dapsone by mouth was one of the first medications used to treat moderate to severe acne vulgaris, and is still occasionally prescribed for the treatment of severe cases.[9][10] A topical form of dapsone is also effective with potentially less side effects.[11]
It is unclear if the combination with pyrimethamine is useful in the prevention of malaria.[12]
Autoimmune disease
- Cutaneous lupus erythematosis. Dapsone is effective and safe in persons with moderate, severe, or refractory cutaneous lupus erythematosis.[13]
- Idiopathic thrombocytopenic purpura. Dapsone is effective and safe for adjunctive glucocorticoid-sparing treatment of persons with idiopathic thrombocytopenic purpura and is preferred over danazol or interferon alpha in those people with antinuclear antibodies.[14]
- Chronic spontaneous urticaria. Dapsone is effective and safe for treatment of second-line therapy for people with chronic spontaneous urticaria in those for whom antihistamines and other first-line agents have failed.[15][16]
- Relapsing polychondritis. There are no clinical trials but there are many case reports that dapsone is effective at doses of 25 mg/day to 200 mg/day for treatment of relapsing polychondritis.[17]
Other
Dermatitis herpetiformis in combination with a gluten-free diet.[3]
Dapsone may be used to treat brown recluse spider bites that become necrotic.[18]
Dapsone is the recommended treatment for erythema elevatum diutinum, as a review found that using oral dapsone alone was effective in 80% of early cases of the disease. However, dapsone can potentially cause severe side effects, meaning that sometimes steroids or other antibiotics should be used instead, although these alternative treatments are much less effective.[19]
An August 2015 review notes that dapsone is reported to be effective against generalized granuloma annulare.[20]
Dapsone has been use as a monomer in the design of dye adsorbent polymers.[21]
Contraindications and precautions
People with porphyria, anemia, cardiac disease, lung disease, HIV infection, G6PD deficiency, and liver impairment are at higher risks of adverse effects when using dapsone.[8] Recommend using pulse oximeter 2x/day to monitor for methemoglobinemia.[22]
Adverse effects
Hypersensitivity reactions occur in 1.4% of persons treated with dapsone, and can be fatal in medical settings with low resources.[23][24] It is a form of severe cutaneous adverse reactions (SCARs) in which a SCARs disorder, primarily the DRESS syndrome or a DRESS syndrome-like reaction occurs.[25][26]
Blood
The most prominent side-effects of this drug are dose-related hemolysis (which may lead to hemolytic anemia) and methemoglobinemia.[27] About 20% of patients treated with dapsone suffer hemolysis[28] and the side-effect is more common and severe in those with glucose-6-phosphate dehydrogenase deficiency, leading to the dapsone-containing antimalarial combination Lapdap being withdrawn from clinical use.[29][30] A case of hemolysis in a neonate from dapsone in breast milk has been reported.[31] Agranulocytosis occurs rarely when dapsone is used alone but more frequently in combination regimens for malaria prophylaxis.[32] Abnormalities in white blood cell formation, including aplastic anemia, are rare, yet are the cause of the majority of deaths attributable to dapsone therapy.[33][34][35]
Liver
Toxic hepatitis and cholestatic jaundice have been reported by the manufacturer. These toxic reactions may also occur as part of the dapsone hypersensitivity syndrome (a form of SCARs-see above) or dapsone syndrome (see below).[25] Dapsone is metabolized by the Cytochrome P450 system, specifically isozymes CYP2D6, CYP2B6, CYP3A4, and CYP2C19.[36] Dapsone metabolites produced by the cytochrome P450 2C19 isozyme are associated with the methemoglobinemia side effect of the drug.
Skin
When used topically, dapsone can cause mild skin irritation, redness, dry skin, burning, and itching. When used together with benzoyl peroxide products, temporary yellow or orange skin discolorations can occur.[37]
Other adverse effects
Other adverse effects include nausea, headache, and rash (which are common), and insomnia, psychosis, and peripheral neuropathy. Effects on the lung occur rarely and may be serious, though are generally reversible.[38]
Dapsone syndrome
Hypersensitivity reactions occur in some patients. This reaction may be more frequent in patients receiving multiple-drug therapy.[39][40][41]
The reaction always involves a rash, may also include fever, jaundice, and eosinophilia, and is likely to be one manifestation of the SCARs reaction viz., the DRESS syndrome (see above).[25][42][43][44][45][46] In general, these symptoms will occur within the first six weeks of therapy or not at all, and may be ameliorated by corticosteroid therapy.[8]
Mechanism of action
As an antibacterial, dapsone inhibits bacterial synthesis of dihydrofolic acid, via competition with para-aminobenzoate for the active site of dihydropteroate synthase, thereby inhibiting nucleic acid synthesis.[47] Though structurally distinct from dapsone, the sulfonamide group of antibacterial drugs also work in this way.
As an anti-inflammatory, dapsone inhibits the myeloperoxidase-H2O2-halide-mediated cytotoxic system in polymorphonucleocytes.[48] As part of the respiratory burst that neutrophils use to kill bacteria, myeloperoxidase converts hydrogen peroxide (H
2O
2) into hypochlorous acid (HOCl). HOCl is the most potent oxidant generated by neutrophils, and can cause significant tissue damage during inflammation. Dapsone arrests myeloperoxidase in an inactive intermediate form, reversibly inhibiting the enzyme. This prevents accumulation of hypochlorous acid, and reduces tissue damage during inflammation.[49][50][51][52][53] Myeloperoxidase inhibition has also been suggested as a neuron-sparing mechanism for reducing inflammation in neurodegenerative diseases such as Alzheimer's disease and stroke.[54]
Dapsone's anti-inflammatory and immunomodulatory effects[55] are thought to be its mechanism of action in treating dermatitis herpetiformis.[56]
Dapsone is an odorless white to creamy-white crystalline powder with a slightly bitter taste.
History
Discovery

In the early 20th century, the German chemist Paul Ehrlich was developing theories of selective toxicity based largely on the ability of certain dyes to kill microbes. Gerhard Domagk, who would later win a Nobel Prize for his efforts, made a major breakthrough in 1932 with the discovery of the antibacterial prontosil red (sulfonamidochrysoidine). Further investigation into the involved chemicals opened the way to sulfa drug and sulfone therapy, first with the discovery of sulfanilamide, the active agent of prontosil, by Daniel Bovet and his team at Pasteur Institute (1935),[58] then with that of dapsone independently by Ernest Fourneau[59] in France and Gladwin Buttle[60] in the United Kingdom.[61]
Proposed use in antimalarial drugs
The spread of drug-resistant malaria in Africa has encouraged the development of new, low-cost antimalarial drugs. Plasmodium falciparum, one of the Plasmodium species that causes malaria, has developed resistance both to chloroquine and sulfadoxine/pyrimethamine, two of the most common treatments for malaria. Artemisinin, another antimalarial drug, had been developed in the 1980s but was too expensive for large-scale use. This led GlaxoSmithKline to develop Lapdap, a combination drug consisting of chlorproguanil and dapsone. Lapdap was licensed in the United Kingdom starting in October 2003.[30]
One advantage of Lapdap had was that chlorproguanil and dapsone are both low-cost drugs. Another was that by virtue of being of a combination drug, it was less likely to cause drug resistance. However, because dapsone causes hemolytic anemia in patients with G6PD deficiency, and because G6PD deficiency affects 10-25% of the population of sub-Saharan Africa, it was discovered that Lapdap is not safe for use in Africa. It was available in many African countries for four years before GlaxoSmithKline took it off the market in February 2008.[30]
Dapsone gel
Dapsone had been reported in a few cases to effectively treat acne, but the risk of hemolytic anemia kept it from being widely used for this purpose. For many years scientists attempted to develop a topical formulation of dapsone that would be as effective against acne as oral dapsone, but without the hemolysis side effect. This was difficult to accomplish because dapsone is highly insoluble in aqueous solvents. In the early 2000s QLT USA developed Aczone, a 5% dapsone gel that was shown to be effective against acne without causing clinically significant declines in hemoglobin levels, even in subjects with G6PD deficiency.[62] In February 2016, the FDA approved a 7.5% dapsone gel. This higher strength has the advantage of a once-daily application, versus twice-daily application of the 5% formulation.[63]
Other uses
Dapsone also find uses as a curing agent in the manufacture of paints, adhesives, composites, powder coats and printed circuit boards.[64][65]
References
- "Dapsone Use During Pregnancy". Drugs.com. 11 November 2019. Retrieved 17 May 2020.
- Thomas L. Lemke (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. p. 1142. ISBN 9780781768795. Archived from the original on 2016-03-04.
- "Dapsone". The American Society of Health-System Pharmacists. Archived from the original on 2015-01-12. Retrieved January 12, 2015.
- Zhu, YI; Stiller, MJ; et al. (2001). "Dapsone and sulfones in dermatology: overview and update". Journal of the American Academy of Dermatology. 45 (3): 420–34. doi:10.1067/mjd.2001.114733. PMID 11511841. S2CID 39874987.
- Joel E. Gallant (2008). Johns Hopkins HIV Guide 2012. Jones & Bartlett Publishers. p. 193. ISBN 9781449619794. Archived from the original on 2016-03-04.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- Greenwood, David (2008). Antimicrobial Drugs: Chronicle of a Twentieth Century Medical Triumph. Oxford University Press. p. 197. ISBN 9780199534845. Archived from the original on 2016-03-04.
- Rossi S, ed. (2006). Australian Medicines Handbook. Adelaide. ISBN 0-9757919-2-3.
- Ross, CM (1961). "The treatment of acne vulgaris with dapsone". Br J Dermatol. 73 (10): 367–70. doi:10.1111/j.1365-2133.1961.tb14398.x. PMID 14494150.
- "Dapsone and Acne Vulgaris". ScienceOfAcne.com. 2012-10-10. Archived from the original on 2012-07-29. Retrieved 2012-08-17.
- Pickert, A; Raimer, S (June 2009). "An evaluation of dapsone gel 5% in the treatment of acne vulgaris". Expert Opinion on Pharmacotherapy. 10 (9): 1515–21. doi:10.1517/14656560903002097. PMID 19505219. S2CID 11880942.
- Croft, AM (29 November 2007). "Malaria: prevention in travellers". Clinical Evidence. 2007. PMC 2943798. PMID 19450348.
- Wallace, Daniel(editor); Chong, Benjamin; Werth, Victoria (2019). "Management of Cutaneous Lupus Erythematosus". Dubois' lupus erythematosus and related syndromes. Edinburgh: Elsevier. pp. 719–726. ISBN 978-0-323-47927-1.CS1 maint: extra text: authors list (link)
- Weber E, Reynaud Q, Fort R, Durupt S, Cathébras P, Durieu I, Lega JC (September 2017). "Immunomodulatory treatments for persistent and chronic immune thrombocytopenic purpura: A PRISMA-compliant systematic review and meta-analysis of 28 studies". Medicine (Baltimore). 96 (37): e7534. doi:10.1097/MD.0000000000007534. PMC 5604622. PMID 28906353.
- Antia C, Baquerizo K, Korman A, Alikhan A, Bernstein JA (October 2018). "Urticaria: A comprehensive review: Treatment of chronic urticaria, special populations, and disease outcomes". J. Am. Acad. Dermatol. 79 (4): 617–633. doi:10.1016/j.jaad.2018.01.023. PMID 30241624.
- Liang SE, Hoffmann R, Peterson E, Soter NA (2019). "Use of Dapsone in the Treatment of Chronic Idiopathic and Autoimmune Urticaria". JAMA Dermatol. 155 (1): 90–95. doi:10.1001/jamadermatol.2018.3715. PMC 6439569. PMID 30476976.
- Rapini RP, Warner NB (2006). "Relapsing polychondritis". Clin. Dermatol. 24 (6): 482–5. doi:10.1016/j.clindermatol.2006.07.018. PMID 17113965.
- Forks, TP (2000). "Brown recluse spider bites". J Am Board Fam Pract. 13 (6): 415–23. doi:10.3122/15572625-13-6-415. PMID 11117338.
- Momen, S.E.; Jorizzo, J.; Al-Niaimi, F. (December 2014). "Erythema elevatum diutinum: a review of presentation and treatment". Journal of the European Academy of Dermatology and Venereology. John Wiley & Sons. 28 (12): 1594–1602. doi:10.1111/jdv.12566. PMID 25288365.
- Lukács, J.; Schliemann, S.; Elsner, P. (August 2015). "Treatment of generalized granuloma annulare – a systematic review". Journal of the European Academy of Dermatology and Venereology. John Wiley & Sons. 29 (8): 1467–1480. doi:10.1111/jdv.12976. PMID 25651003.
- Khazaei, Ardeshir; Kazem-Rostami, Masoud; Zare, Abdolkarim; Moosavi-Zare, Ahmad Reza; Sadeghpour, Mahdieh; Afkhami, Abbas (15 September 2013). "Synthesis, characterization, and application of a triazene-based polysulfone as a dye adsorbent". Journal of Applied Polymer Science. 129 (6): 3439–3446. doi:10.1002/app.39069.
- Singh, Shivinder; Sethi, Navdeep; Pandith, Sushmitha; Ramesh, Gouri Shankar (2014). "Dapsone-induced methemoglobinemia: 'Saturation gap'—The key to diagnosis". Journal of Anaesthesiology Clinical Pharmacology. 30 (1): 86. doi:10.4103/0970-9185.125710. PMC 3927300. PMID 24574600.
- Lorenz M, Wozel G, Schmitt J (March 2012). "Hypersensitivity reactions to dapsone: a systematic review". Acta Derm. Venereol. 92 (2): 194–9. doi:10.2340/00015555-1268. PMID 22307940.
- Zhang FR, Liu H, Irwanto A, et al. (October 2013). "HLA-B*13:01 and the dapsone hypersensitivity syndrome". N Engl J Med. 369 (17): 1620–8. doi:10.1056/NEJMoa1213096. PMID 24152261. S2CID 34708642.
- Bocquet H, Bagot M, Roujeau JC (December 1996). "Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS)". Semin Cutan Med Surg. 15 (4): 250–7. doi:10.1016/S1085-5629(96)80038-1. PMID 9069593.
- Tempark T, Satapornpong P, Rerknimitr P, Nakkam N, Saksit N, Wattanakrai P, Jantararoungtong T, Koomdee N, Mahakkanukrauh A, Tassaneeyakul W, Suttisai S, Pratoomwun J, Klaewsongkram J, Rerkpattanapipat T, Sukasem C (December 2017). "Dapsone-induced severe cutaneous adverse drug reactions are strongly linked with HLA-B*13: 01 allele in the Thai population". Pharmacogenetics and Genomics. 27 (12): 429–437. doi:10.1097/FPC.0000000000000306. PMID 28885988. S2CID 4283457.
- Jopling WH (1983). "Side-effects of antileprosy drugs in common use". Lepr Rev. 54 (4): 261–70. doi:10.5935/0305-7518.19830032. PMID 6199637.
- Puavilai S, Chutha S, Polnikorn N, et al. (July 1984). "Incidence of anemia in leprosy patients treated with dapsone". J Med Assoc Thai. 67 (7): 404–7. PMID 6512448.
- "Antimalarial chlorproguanil-dapsone (LapDap™) withdrawn following demonstration of post-treatment haemolytic anaemia in G6PD deficient patients in a Phase III trial of chlorproguanil-dapsone-artesunate (Dacart™) versus artemether-lumefantrine (Coartem®) and confirmation of findings in a comparative trial of LapDap™ versus Dacart ™" (PDF). World Health Organization. 4 March 2008. QSM/MC/IEA.1. Archived (PDF) from the original on 21 October 2012.
- Luzzatto L (August 2010). "The rise and fall of the antimalarial Lapdap: a lesson in pharmacogenetics". Lancet. 376 (9742): 739–41. doi:10.1016/S0140-6736(10)60396-0. PMID 20599264. S2CID 34866078.
- Sanders SW, Zone JJ, Foltz RL, Tolman KG, Rollins DE (April 1982). "Hemolytic anemia induced by dapsone transmitted through breast milk". Ann Intern Med. 96 (4): 465–6. doi:10.7326/0003-4819-96-4-465. PMID 7065565.
- Firkin FC, Mariani AF (1977). "Agranulocytosis due to dapsone". Med. J. Aust. 2 (8): 247–51. doi:10.5694/j.1326-5377.1977.tb117649.x. PMID 909500.
- Foucauld J, Uphouse W, Berenberg J (1985). "Dapsone and aplastic anemia". Ann. Intern. Med. 102 (1): 139. doi:10.7326/0003-4819-102-1-139_2. PMID 3966740.
- Meyerson MA, Cohen PR (1994). "Dapsone-induced aplastic anemia in a woman with bullous systemic lupus erythematosus". Mayo Clin. Proc. 69 (12): 1159–62. doi:10.1016/s0025-6196(12)65768-1. PMID 7967777.
- Björkman A, Phillips-Howard PA (1991). "Adverse reactions to sulfa drugs: implications for malaria chemotherapy". Bull. World Health Organ. 69 (3): 297–304. PMC 2393107. PMID 1893504.
- Ganesan, S; Sahu, R; Walker, LA; Tekwani, BL (April 2010). "Cytochrome P450-dependent toxicity of dapsone in human erythrocytes". J Appl Toxicol. 30 (3): 271–5. doi:10.1002/jat.1493. PMID 19998329.
- Aczone(Dapsone) Package insert. Irvine CA: Allergan Inc.; September 2008
- Jaffuel D, Lebel B, Hillaire-Buys D, Pene J, Godard P, Michel FB, Blayac JP, Bousquet J, Demolyi P (1998). "Eosinophilic pneumonia induced by dapsone". BMJ. 317 (7152): 181. doi:10.1136/bmj.317.7152.181. PMC 28611. PMID 9665900.
- Richardus JH, Smith TC (1989). "Increased incidence in leprosy of hypersensitivity reactions to dapsone after introduction of multidrug therapy". Lepr Rev. 60 (4): 267–73. doi:10.5935/0305-7518.19890033. PMID 2491425.
- Kumar RH, Kumar MV, Thappa DM (1998). "Dapsone syndrome—a five year retrospective analysis". Indian J Lepr. 70 (3): 271–6. PMID 9801899.
- Rao PN, Lakshmi TS (2001). "Increase in the incidence of dapsone hypersensitivity syndrome—an appraisal". Lepr Rev. 72 (1): 57–62. doi:10.5935/0305-7518.20010009. PMID 11355519.
- Joseph MS (1985). "Hypersensitivity reaction to dapsone. Four case reports". Lepr Rev. 56 (4): 315–20. doi:10.5935/0305-7518.19850034. PMID 4079634.
- Jamrozik K (1986). "Dapsone syndrome occurring in two brothers". Lepr Rev. 57 (1): 57–62. doi:10.5935/0305-7518.19860010. PMID 3702581.
- Hortaleza AR, Salta-Ramos NG, Barcelona-Tan J, Abad-Venida L (1995). "Dapsone syndrome in a Filipino man". Lepr Rev. 66 (4): 307–13. doi:10.5935/0305-7518.19950034. PMID 8637384.
- Tomecki KJ, Catalano CJ (1981). "Dapsone hypersensitivity. The sulfone syndrome revisited". Arch Dermatol. 117 (1): 38–9. doi:10.1001/archderm.1981.01650010044023. PMID 6450569.
- Kromann NP, Vilhelmsen R, Stahl D (1982). "The dapsone syndrome". Arch Dermatol. 118 (7): 531–2. doi:10.1001/archderm.1982.01650190085028. PMID 7092282.
- "Mechanisms of Action of Dapsone in Dermatological Diseases". Dapsone: Clinical Uses in Various Cutaneous Diseases. Medscape Today. Archived from the original on May 17, 2011.
- Galijasevic S (January 2019). "The development of myeloperoxidase inhibitors". Bioorg. Med. Chem. Lett. 29 (1): 1–7. doi:10.1016/j.bmcl.2018.11.031. PMID 30466896.
- Bozeman PM, Learn DB, Thomas EL (1990). "Assay of the human leukocyte enzymes myeloperoxidase and eosinophil peroxidase". J. Immunol. Methods. 126 (1): 125–33. doi:10.1016/0022-1759(90)90020-v. PMID 2154520.
- Bozeman PM, Learn DB, Thomas EL (1992). "Inhibition of the human leukocyte enzymes myeloperoxidase and eosinophil peroxidase by dapsone". Biochem. Pharmacol. 44 (3): 553–63. doi:10.1016/0006-2952(92)90449-s. PMID 1324677.
- Stendahl O, Molin L, Lindroth M (1983). "Granulocyte-mediated release of histamine from mast cells. Effect of myeloperoxidase and its inhibition by antiinflammatory sulfone compounds". Int. Arch. Allergy Appl. Immunol. 70 (3): 277–84. doi:10.1159/000233335. PMID 6186607.
- Kettle AJ, Gedye CA, Winterbourn CC (1993). "Superoxide is an antagonist of antiinflammatory drugs that inhibit hypochlorous acid production by myeloperoxidase". Biochem. Pharmacol. 45 (10): 2003–10. doi:10.1016/0006-2952(93)90010-t. PMID 8390258.
- Kettle AJ, Winterbourn CC (1991). "Mechanism of inhibition of myeloperoxidase by anti-inflammatory drugs". Biochem. Pharmacol. 41 (10): 1485–92. doi:10.1016/0006-2952(91)90565-m. PMID 1850278.
- Diaz-Ruiz A, Zavala C, Montes S, et al. (November 2008). "Antioxidant, antiinflammatory and antiapoptotic effects of dapsone in a model of brain ischemia/reperfusion in rats". J. Neurosci. Res. 86 (15): 3410–9. doi:10.1002/jnr.21775. PMID 18615706.
- Begon E, Chosidow O, Wolkenstein P (December 2004). "[Disulone]". Ann Dermatol Venereol (in French). 131 (12): 1062–73. doi:10.1016/S0151-9638(04)93842-2. PMID 15692440.
- Uetrecht JP (1995). "Myeloperoxidase as a generator of drug free radicals". Biochem. Soc. Symp. 61: 163–70. doi:10.1042/bss0610163. PMID 8660393. S2CID 12471553.
- Derivatives of p-Nitrothiophenols, by E. Fromm and J. Wittmann
Reports of the German Chemical Society Mai–August 1908 Fromm, E.; Wittmann, J. (May 1908). "Derivate desp-Nitrothiophenols". Berichte der Deutschen Chemischen Gesellschaft. 41 (2): 2264–2273. doi:10.1002/cber.190804102131. - Tréfouël, J. et T.; Nitti, F.; Bovet, D. (23 November 1935). "Activité du p.aminophénylsulfamide sur l'infection streptococcique expérimentale de la souris et du lapin". Comptes rendus des séances de la Société de biologie et de ses filiales (in French). 120: 756. Archived from the original on 3 January 2017.
- Fourneau, E.; Tréfouël, Th. et J.; Nitti, F.; Bovet, D. (1937). "Action antistreptococcique des dérivés sulfurés organiques". Comptes rendus de l'Académie des sciences (in French). 204: 1763. Archived from the original on 2016-02-20.
- Buttle, G.A.H.; Stephenson, D.; Smith, S.; Dewing, T.; Foster, G.E. (June 1937). "Treatment of streptococcal infections in mice with 4:4'diamino-dipheni-sulphone". Lancet. 229 (5936): 1331–4. doi:10.1016/S0140-6736(00)75868-5.
- "Leprosy | 14 History of dapsone and dyes". Archived from the original on 2009-02-12. Retrieved 2009-02-24. (1937)
- Stotland, Mira; Shalita, Alan R.; Kissling, Robert F. (June 2009). "Dapsone 5% Gel: A Review of its Efficacy and Safety in the Treatment of Acne Vulgaris". American Journal of Clinical Dermatology. 10 (4): 221–227. doi:10.2165/00128071-200910040-00002. PMID 19489655. S2CID 19485887.
- "Aczone (dapsone) 7.5% Gel Prescribing Information" (PDF). Allergan. February 2016. Archived (PDF) from the original on 8 August 2016. Retrieved 23 June 2016.
- "ECHA dapsone registration dossier".
- "LAPOX ASH-10".