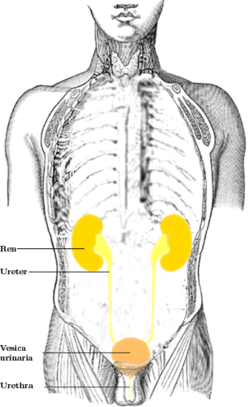
Ureter
The ureters are tubes made of smooth muscle that propel urine from the kidneys to the urinary bladder. In the human adult, the ureters are usually 25–30 cm (10–12 in) long and around 3–4 mm (0.12–0.16 in) in diameter. The ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer in third closest to the bladder that assists with peristalsis.
The ureters can be affected by a number of diseases; including urinary tract infections and kidney stone. Stenosis is when a ureter is narrowed, due to for example chronic inflammation. Congenital abnormalities that affect the ureters can include the development of two ureters on the same side, or abnormally placed ureters. Additionally, reflux of urine from the bladder back up the ureters is a condition commonly seen in children.
The ureters have been identified for at least two thousand years; with the word ureter stemming from the stem uro- relating to urinating and seen in written records since at least the time of Hippocrates. It is however only since the 1500s that the term "ureter" has been consistently used to refer to the modern structure; and only since the development of medical imaging in the 1900s that techniques such as X-ray, CT and ultrasound have been able to view the ureters. The ureters are also seen from the inside using a flexible camera, called ureteroscopy, which was first described in 1964.
Structure
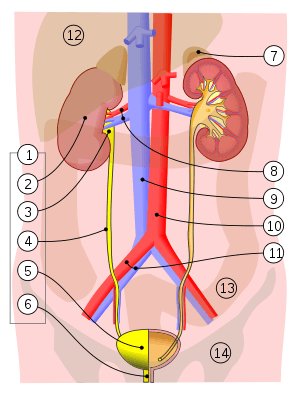
Vessels:
8. Renal artery and vein, 9. Inferior vena cava, 10. Abdominal aorta, 11. Common iliac artery and vein
With transparency:
12. Liver, 13. Large intestine, 14. Pelvis
The ureters are tubular structures, approximately 20–30 cm (7.9–11.8 in) in adults,[1] that pass from the pelvis of each kidney into the bladder. From the renal pelvis, they descend on top of the psoas major muscle to reach the brim of the pelvis. Here, they cross in front of the common iliac arteries. They then pass down along the sides of the pelvis, and finally curve forwards and enter the bladder from its left and right sides at the back of the bladder.[2] The ureters are between 1.5 - 6mm in diameter,[1] and surrounded by a layer of smooth muscle for 1 - 2 cm near their ends just before they enter the bladder.[2]
The ureters enter the bladder from its back surface, traveling 1.5–2 cm (0.59–0.79 in) before opening into the bladder at an angle on its outer back surface at the slit-like ureteric orifices.[2][3] This location is also called the vesicoureteric junction.[4] In the contracted bladder they are about 25 mm (1 in) apart and about the same distance from the internal urethral orifice; in the distended bladder these measurements may be increased to about 50 mm (2 in).[2]
A number of structures pass by, above, and around the ureters on their path down from the kidneys to the bladder.[2] In its upper part, the ureter travels on the psoas major muscle, and sits just behind the peritoneum. As it passes down the muscle, it travels over the genitofemoral nerve and. The inferior vena cava and the abdominal aorta sit to the midline of the right and left ureters respectively.[2] In the lower part of the abdomen, the right ureter sits behind the lower mesentery and the terminal ileum, and the left ureter sits behind the jejunum and the sigmoid colon.[2] As the ureters enter the pelvis, they are surrounded by connective tissue, and travel backwards and outwards, passing in front of the internal iliac arteries and internal iliac veins. They then travel inwards and forwards, crossing the umbilical, inferior vesical and middle rectal arteries.[2] From here, in males they cross under the vas deferens and in front of the seminal vesicles to enter the bladder near the trigone.[2] In females, the ureters pass behind the ovaries, and then travel in the lower midline section of the broad ligament of the uterus. For a short part, the uterine arteries travel on top for a short (2.5cm) period. They then pass by the cervix, travelling inwards towards the bladder.[2]
Blood and lymphatic supply
The ureter has a blood supply which varies along its course, with the arteries that supply the ureters ending in a network of vessels within the adventitia of the ureters.[1] The upper third of the ureter, closest to the kidney, is supplied by the renal arteries.[2] The middle part of the ureter is supplied by the common iliac arteries, direct branches from the abdominal aorta, and gonadal arteries;[1] the gonadal arteries being the testicular artery in men and the ovarian artery in women.[2] The lower third of the ureter, closest to the bladder, is supplied by branches from the internal iliac arteries, mainly the superior and inferior vesical arteries.[1] The arterial supply can be variable, with arteries that contribute include the middle rectal artery, branches directly from the aorta,[1] and, in women, the uterine and vaginal arteries.[2]
There are many connections (anastamoses) between the arteries of the ureter,[2] particularly in the adventitia,[5] which means damage to a single vessel does not compromise the blood supply of the ureter.[2][5] Venous drainage mostly parallels that of the arterial supply;[5][2] that is, it begins as a network of smaller veins in the adventitia; with the renal veins draining the upper ureters, and the vesicular and gonadal veins draining the lower ureters.[1]
Lymphatic drainage depends on the position of lymphatic vessels in the ureter.[1] Lymph collects in submucosal, intramuscular and advential lymphatic vessels.[2] Those vessels closer to the kidney drain into renal collecting vessels; into the lateral aortic nodes near the gonadal vessels.[2] The middle part of the ureter drains into the right paracaval and interaortocaval nodes on the right, and the left paraaortic nodes on the left.[1] In the lower ureter, lymph may drain into the common iliac lymph nodes, or lower down in the pelvis to the common, external, or internal iliac lymph nodes.[2]
Nerve supply
The ureters are richly supplied by nerves that form a network (plexus) of nerves, the ureteric plexus that lies in the adventitia of the ureters.[2] This plexus is formed from a number of nerve roots directly (T9-12, L1, and S2-4), as well as branches from other nerve plexuses and nerves; specifically, the upper third of the ureter receives nerve branches from the renal plexus and aortic plexus, the middle part receives branches from the upper hypogastric plexus and nerve, and the lower ureter receives branches from the lower hypogastric plexus and nerve.[2] The plexus is in the adventitia. The these nerves travel in individual bundles and along small blood vessels to form the ureteric plexus.[2] Sensation supplied is sparse close to the kidneys and increases closer to the bladder.[2]
Sensation to the ureters is provided by nerves that come from T11 - L2 segments of the spinal cord.[2] When pain is caused, for example by spasm of the ureters or by a stone, the pain may be referred to the dermatomes of T11 - L2, namely the back and sides of the abdomen, the scrotum (males) or labia majora (females) and upper part of the front of the thigh.[2]
Microanatomy

The ureter is lined by urothelium, a type of transitional epithelium that is capable of responding to stretches in the ureters. The transitional epithelium may appear as a layer of column-shaped cells when relaxed, and of flatter cells when distended. Below the epithelium sits the lamina propria. The lamina propria is made up of loose connective tissue with many elastic fibers interspersed with blood vessels, veins and lymphatics. The ureter is surrounded by two muscular layers, an inner longitudinal layer of muscle, and an outer circular or spiral layer of muscle.[6][7] The lower third of the ureter has a third muscular layer.[7] Beyond these layers sits an adventitia containing blood vessels, lymphatic vessels, and veins.[7]
Development
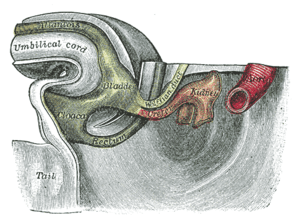
The ureters develop from the ureteric buds, which are outpuchings from the mesonephric duct. This is a duct, derived from mesoderm, found in the early embryo.[8] Over time, the buds elongate, moving into surrounding mesodermal tissue, dilate, and divide into left and right ureters. Eventually, successive divisions from these buds form not only the ureters, but also the pelvis, major and minor calyces, and collecting ducts of the kidneys.[8]
The mesonephric duct is connected with the cloaca, which over the course of development splits into a urogenital sinus and the anorectal canal.[8] The urinary bladder forms from the urogenital sinus. Over time, as the bladder enlarges, it absorbs the surrounding parts of the primitive ureters.[8] Finally, the entry points of the ureters into the bladder move upwards, owing to the upward migration of the kidneys in the developing embryo.[8]
Function
The ureters are a component of the urinary system. Urine, produced by the kidneys, travels along the ureters to the bladder. It does this through regular contractions called peristalsis.[2]
 Ultrasound showing a jet of urine entering the bladder (large black section) through the ureter.
Ultrasound showing a jet of urine entering the bladder (large black section) through the ureter.
Clinical significance
Ureteral stones
A kidney stone can move from the kidney and become lodged inside the ureter, which can block the flow of urine, as well as cause a sharp cramp in the back, side, or lower abdomen.[9] Pain often comes in waves lasting up to two hours, then subsides, called renal colic.[10] The affected kidney could then develop hydronephrosis, should a part of the kidney become swollen due to blocked flow of urine.[9] It is classically described that there are three sites in the ureter where a kidney stone will commonly become stuck: where the ureter meets the renal pelvis; where the iliac blood vessels cross the ureters; and where the ureters enter the urinary bladder,[9] however a retrospective case study, which is a primary source, of where stones lodged based on medical imaging did not show many stones at the place where the iliac blood vessels cross.[11]
Most stones are compounds containing calcium such as calcium oxalate and calcium phosphate. The first recommended investigation is a CT scan of the abdomen because it can detect almost all stones. Management includes analgesia, often with nonsteroidal antiinflammatories.[10] Small stones (< 4mm) may pass themselves; larger stones may require lithotripsy, and those with complications such as hydronephrosis or infection may require surgery to remove.[10]
Reflux
Vesicoureteral reflux refers to the reflux of fluid from the bladder into the ureters.[12] This condition can be associated with urinary tract infections, particularly in children, and is present in up to 28 - 36% of children to some degree.[12] A number of forms of medical imaging are available for diagnosis of the condition, with modalities including doppler urinary tract ultrasound, MAG 3 nuclear medicine scaning, and a micturition urethrocystogram. Factors that affect which of these are selected depends if a child is able to receive a urinary catheter, and whether a child is toilet trained.[12] Whether these investigations are performed at the first time a child has an illness, or later and depending on other factors (such as if the causal bacteria is Escherichia coli) differ between US, EU and UK guidelines.[12]
Management is also variable, with differences between international guidelines on issues such as whether prophylactic antibiotics should be used, and whether surgery is recommended.[12] One reason is that the natural history of the majority of vesicoureteral reflux is to improve without any intervention at all.[12] If surgery is considered, it generally involves reattaching the ureters to the bladder, and extending the part of the ureter that it is within the wall of the bladder, with the most common surgical option being Cohen's cross-trigonal reimplantation.[12] It is unclear if there is a role of surgery in vesicoureteral reflux.[13]
Anatomical and surgical abnormalities
Blockage, or obstruction of the ureter can occur,[14] as a result of narrowing within the ureter, or compression or fibrosis of structures around the ureter.[15] Narrowing can result of ureteric stones, masses associated with cancer, and other lesions such as endometriosis tuberculosis and schistosomiasis.[15] External factors such as constipation and retroperitoneal fibrosis can also compress the ureters.[15] Some congenital abnormalities can also result in narrowing or the ureters. Congenital disorders of the ureter and urinary tract affect 10% of infants.[14] These include partial or total duplication of the ureter (a duplex ureter), or the formation of a second irregularly placed (ectopic) ureter;[14] or where the junction with the bladder is malformed or a ureterocoele develops (usually in that location).[15] If the ureters have been resited as a result of surgery, for example due to a kidney transplant or due to past surgery for vesicuureteric reflux, that site may also become narrowed.[16][1]
A narrowed ureter may lead to ureteric enlargement (dilation) and cause swelling of the kidneys (hydronephrosis).[14] Associated symptoms may include recurrent infections, pain or blood in the urine; and when tested, kidney function might be seen to decrease.[14] These are considered indications for surgery.[14] Medical imaging, including urinary tract ultrasound, CT or nuclear medicine imaging is conducted to investigate many causes.[14][15] This may involve reinserting the ureters into a new place on the bladder (reimplantion), or narrowing of the ureter.[14] A ureteric stent may be inserted to relieve an obstruction.[17] If the cause cannot be removed, a nephrostomy may be required, which is the insertion of a tube connected to the renal pelvis which directly drains urine into a stoma bag.[18]
Cancer
Cancer of the ureters is known as ureteral cancer. It is usually due to cancer of the urothelium, the cells that line the surface of the ureters. Urothelial cancer is more common after the age of 40, and more common in men than women;[19] other risk factors include smoking and exposure to dyes such as aromatic amines and aldehydes.[19] When cancer is present, the most common symptom in an affected person is blood in the urine; a physical medical examination may be otherwise normal, except in late disease.[19] Ureteral cancer is most often due to cancer of the cells lining the ureter, called transitional cell carcinoma, although it can more rarely occur as a squamous cell carcinoma if the type of cells lining the urethra have changed due to chronic inflammation, such as due to stones or schistosomiasis.[19]
Investigations performed usually include collecting a sample of urine for an inspection for malignant cells under a microscope, called cytology, as well as medical imaging by a CT urogram or ultrasound.[19] If a concerning lesion is seen, a flexible camera may be inserted into the ureters, called ureteroscopy, in order to view the lesion and take a biopsy, and a CT scan will be performed of other body parts (a CT scan of the chest, abdomen and pelvis) to look for additional metastatic lesions.[19] After the cancer is staged, treatment may involve open surgery to remove the affected ureter and kidney if it is involved; or, if the lesion is small, it may be removed via ureteroscopy.[19] Prognosis can vary markedly depending on the tumour grade, with a worse prognosis associated with an ulcerating lesion.[19]
Injury
Injuries to the ureter with certain forms of trauma including penetrating abdominal injuries and injuries at high speeds followed by an abrupt stop (such as a high speed car accident).[20] The ureter can be injur during surgery to nearby structures.[21] It is injured in 0.2 per 1,000 cases of vaginal hysterectomies and 1.3 per 1,000 cases of abdominal hysterectomies,[21] usually near the suspensory ligament of the ovary or near the cardinal ligament, where the ureter runs close to the blood vessels of the uterus.[22]
Imaging
Several forms of medical imaging exist that are used to view the ureters and urinary tract.[23] Ultrasound may be able to show evidence of blockage because of hydronephrosis of the kidneys and renal pelvis.[23] CT scans, including ones where contrast media is injected intravenously to better show the ureters, and with contrast to better show lesions, and to differentiate benign from malignant lesions.[23] Dye may also be injected directly into the ureters or renal tract; an antegrade pyelogram is when contrast is injected directly into the renal pelvis, and a retrograde pyelogram is where dye is injected into the urinary tract via a catheter, and flows backwards into the ureters.[23] More invasive forms of imaging include ureteroscopy, which is the insertion of a flexible endoscope into the urinary tract to view the ureters.[24] Ureteroscopy is most commonly used for medium to large-sized stones when less invasive methods of removal are not able to be used.[24]
Other animals
Ureters are also found in all other amniote species, although different ducts fulfill the same role in amphibians and fish.[25] In marsupials, but not in placental mammals, the ureters pass between the oviducts during embryonic development.[26][27][28]
History
The word "ureter" comes from the Ancient Greek stem "uro" relating to urination, and the first use of the word is seen during the era of Hippocrates to refer to the urethra.[29] The anatomical structure of the ureter was noted by 40 AD. However, the terms "ureter" and "urethra" were variably used to refer to each other thereafter for more than a millennium.[29] It was only in the 1550s that anatomists such as Bartolomeo Eustacchio and Jacques Dubois began to use the terms to specifically and consistently refer to what is in modern English called the ureter and the urethra.[29] Following this, in the 19th and 20th centuries multiple terms relating to the structures such as ureteritis and ureterography, were coined.[29]
Kidney stones have been identified and recorded about as long as written historical records exist.[30] The urinary tract including the ureters, as well as their function to drain urine from the kidneys, has been described by Galen in the second century AD.[31]
The first to examine the ureter through an internal approach, called ureteroscopy, rather than surgery was Hampton Young in 1929.[30] This was improved on by VF Marshall who is the first published use of a flexible endoscope based on fiber optics, which occurred in 1964.[30] The insertion of a drainage tube into the renal pelvis, bypassing the uterers and urinary tract, called nephrostomy, was first described in 1941. Such an approach differed greatly from the open surgical approaches within the urinary system employed during the preceding two millennia.[30]
The first radiological imaging of the ureters first occurred via X-rays, although this was made more difficult by the thick abdomen, which the low power of the original X-rays was not able to penetrate enough to produce clear images.[32] More useful images were able to be produced when Edwin Hurry Fenwick in 1908 pioneered the use of tubes covered in radioopaque material visible to X-rays inserted into the ureters, and in the early 20th century when contrast were injected externally into the urinary tract (retrograde pyelograms).[32] Unfortunately, much of the earlier retrograde pyelograms were complicated by significant damage to the kidneys as a result of contrast based on silver or sodium iodide.[32] Hryntshalk in 1929 pioneered the development of the intravenous urogram, in which contrast is injected into a vein and highlights the kidney and, when excreted, the urinary tract.[32] Things improved with the development by Moses Swick and Leopold Lichtwitz in the late 1920s of relatively nontoxic contrast media, with controversy surrounding publication as to was the primary discoverer.[32] Side-effects associated with imaging improved even more when Tosten Almen published a ground-breaking thesis in 1969 based on the less toxic low-osmolar contrast media, developed based on swimming experiences in lakes with different salinity.[32]
References
- Arthur D. Smith (Editor), Glenn Preminger (Editor), Gopal H. Badlani (Editor), Louis R. Kavoussi (Editor) (2019). "38. Ureteral Anatomy". Smith's textbook of endourology (4th ed.). John Wiley & Sons Ltd. pp. 455–464. ISBN 9781119245193.CS1 maint: multiple names: authors list (link) CS1 maint: extra text: authors list (link)
- Standring, Susan, ed. (2016). "Ureter". Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. pp. 1251–1254. ISBN 9780702052309. OCLC 920806541.
- Standring, Susan, ed. (2016). Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. p. 1259. ISBN 9780702052309. OCLC 920806541.
- Visveswaran, kasi (2009). Essentials of Nephrology, 2/e. BI Publications Pvt Ltd. p. 61. ISBN 978-81-7225-323-3.
- Wein, Alan J. (2011). Campbell-Walsh Urology (10th ed.). Elsevier. p. 31.
- Lowe, Alan Stevens, James S. (2005). Human histology (3rd ed.). Philadelphia & Toronto: Elsevier Mosby. p. 324. ISBN 0-3230-3663-5.
- Young, Barbara; O'Dowd, Geraldine; Woodford, Phillip (2013-11-04). Wheater's functional histology: a text and colour atlas (6th ed.). Philadelphia: Elsevier. p. 314. ISBN 9780702047473.
- Sadley, TW (2019). "Urinary system". Langman's medical embryology (14th ed.). Philadelphia: Wolters Kluwer. pp. 256–266. ISBN 9781496383907.
- Moore, Keith L.; Dalley, Arthur F.; Agur, A. M. R. (2013). Clinically Oriented Anatomy. Lippincott Williams & Wilkins. p. 300. ISBN 978-1-4511-1945-9.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Urolithiasis". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 431–2. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- Ordon, Michael; Schuler, Trevor D.; Ghiculete, Daniela; Pace, Kenneth T.; Honey, R. John D'A. (March 2013). "Third Place: Stones Lodge at Three Sites of Anatomic Narrowing in the Ureter: Clinical Fact or Fiction?". Journal of Endourology. 27 (3): 270–276. doi:10.1089/end.2012.0201.
- Tullus, Kjell (January 2015). "Vesicoureteric reflux in children" (PDF). The Lancet. 385 (9965): 371–379. doi:10.1016/S0140-6736(14)60383-4.
- Najar, M. S.; Saldanha, C. L.; Banday, K. A. (October 2009). "Approach to urinary tract infections". Indian Journal of Nephrology. 19 (4): 129–139. doi:10.4103/0971-4065.59333. ISSN 0971-4065. PMC 2875701. PMID 20535247.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Diseases of the collecting system and ureters". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 433–4. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- "Ureteral obstruction - Symptoms and causes". Mayo Clinic. 2020. Retrieved 6 July 2020.
- Faenza, A.; Nardo, Bruno; Catena, Fausto; Scolari, Maria P.; d'Arcangelo, Giovanni Liviano; Buscaroli, Andrea; Rossi, Cristina; Zompatori, Maurizio (1 October 1999). "Ureteral stenosis after kidney transplantation". Transplant International. 12 (5): 334–340. doi:10.1007/s001470050236. ISSN 1432-2277.
- Sali, Gaurav Mohan; Joshi, Hrishikesh B (23 September 2019). "Ureteric stents: Overview of current clinical applications and economic implications". International Journal of Urology. 27 (1): 7–15. doi:10.1111/iju.14119.
- R, Martin; Baker, H. "Nursing care and management of patients with a nephrostomy". Nursing Times.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Urothelial tumours". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 435–6. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- Stein, D. M.; Santucci, R. A. (July 2015). "An update on urotrauma". Current Opinion in Urology. 25 (4): 323–30. doi:10.1097/MOU.0000000000000184. PMID 26049876.
- Burks, F. N.; Santucci, R. A. (June 2014). "Management of iatrogenic ureteral injury". Therapeutic Advances in Urology. 6 (3): 115–24. doi:10.1177/1756287214526767. PMC 4003841. PMID 24883109.
- Santucci, Richard A. "Ureteral Trauma". Medscape. Retrieved 11 April 2012.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Investigation of renal and urinary tract disease:Imaging". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 389–390. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- "Ureteroscopy". National Kidney Foundation. 2020. Retrieved 2020-07-04.
- Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. p. 378. ISBN 0-03-910284-X.
- Hugh Tyndale-Biscoe; Marilyn Renfree (30 January 1987). Reproductive Physiology of Marsupials. Cambridge University Press. ISBN 978-0-521-33792-2.
- Frederick S. Szalay; Michael J. Novacek; Malcolm C. McKenna (6 December 2012). Mammal Phylogeny: Mesozoic Differentiation, Multituberculates, Monotremes, Early Therians, and Marsupials. Springer Science & Business Media. ISBN 978-1-4613-9249-1.
- C. Hugh Tyndale-Biscoe (2005). Life of Marsupials. Csiro Publishing. pp. 7–. ISBN 978-0-643-09199-3.
- Marx, Franz Josef; Karenberg, Axel (2010). "Uro-words making history: Ureter and urethra". The Prostate: n/a–n/a. doi:10.1002/pros.21129.
- Tefekli, Ahmet; Cezayirli, Fatin (2013). "The History of Urinary Stones: In Parallel with Civilization". The Scientific World Journal. 2013: 1–5. doi:10.1155/2013/423964.
- Nahon, I; Waddington, G; Dorey, G; Adams, R (2011). "The history of urologic surgery: from reeds to robotics". Urologic nursing. 31 (3): 173–80. PMID 21805756.
- Thomas, Adrian M. K.; Banerjee, Arpan K. (2013). "Contrast media and the renal tract". The History of Radiology. OUP Oxford. ISBN 978-0-19-166971-2.