Menstrual disorder
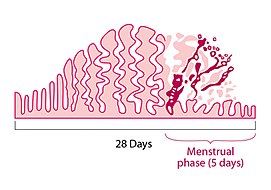
A menstrual disorder is characterized as any abnormal condition with regards to a woman's menstrual cycle. There are many different types of menstrual disorders that vary with signs and symptoms, including pain during menstruation, heavy bleeding, or absence of menstruation. Normal variations can occur in menstrual patterns but generally menstrual disorders can also include periods that come sooner than 21 days apart, more than 3 months apart, or last more than 10 days in duration.[1] Variations of the menstrual cycle are mainly caused by the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, and early detection and management is required in order to minimize the possibility of complications regarding future reproductive ability.[2][3]
Though menstrual disorders were once considered more of a nuisance problem, they are now widely recognized as having a serious impact on society in the form of days lost from work brought about by the pain and suffering experienced by women. These disorders can arise from physiologic sources (pregnancy etc.), pathologic sources (stress, excessive exercise, weight loss, endocrine or structural abnormalities etc.), or iatrogenic sources (secondary to contraceptive use etc.).[4]
Types of menstrual disorders
Premenstrual Disorders
- Premenstrual syndrome (PMS) or premenstrual tension refers to the emotional and physical symptoms that routinely occur in the two weeks leading up to menstruation.[5] Symptoms are usually mild, but 5-8% of women suffer from moderate to severe symptoms that significantly affect daily activities.[6] Symptoms may include anxiety, irritability, mood swings, depression, headache, food cravings, increased appetite, and bloating.[4]
- Premenstrual dysphoric disorder (PMDD) is a severe mood disorder that affects cognitive and physical functions in the week leading up to menstruation. Premenstrual dysphoric disorder is diagnosed with at least one affective, or mood, symptom and at least five physical, mood, and/or behavioral symptoms.[7]
Disorders of cycle length
Normal menstrual cycle length is 22-45 days.[4]
- Amenorrhea is the absence of a menstrual period in a woman of reproductive age. Physiologic states of amenorrhoea are seen during pregnancy and lactation (breastfeeding). Outside of the reproductive years there is absence of menses during childhood and after menopause.[8]
- Irregular menstruation is where there is variation in menstrual cycle length of more than approximately 8 days for a woman. The term metrorrhagia is often used for irregular menstruation that occurs between the expected menstrual periods.[9][10]
- Oligomenorrhea is the medical term for infrequent, often light menstrual periods (intervals exceeding 35 days).[11]
- Polymenorrhea is the medical term for cycles with intervals of 21 days or fewer.[12]
Disorders of flow
Normal menstrual flow length is 3-7 days.[4]
- Abnormal uterine bleeding (AUB) is a broad term used to describe any disruption in bleeding that involves the volume, duration, and/or regularity of flow. Bleeding may occur frequently or infrequently, and can occur between periods, after sexual intercourse, and after menopause. Bleeding during pregnancy is excluded.[13]
- Hypomenorrhea is abnormally light menstrual bleeding.[14]
- Menorrhagia (meno = prolonged, rrhagia = excessive flow/discharge) is an abnormally heavy and prolonged menstrual period.[14]
- Metrorrhagia is bleeding at irregular times, especially outside the expected intervals of the menstrual cycle. If there is excessive menstrual and uterine bleeding other than that caused by menstruation, menometrorrhagia (meno = prolonged, metro = time, rrhagia = excessive flow/discharge) may be diagnosed. Causes may be due to abnormal blood clotting, disruption of normal hormonal regulation of periods or disorders of the endometrial lining of the uterus. Depending upon the cause, it may be associated with abnormally painful periods.[14]
Disorders of ovulation
Disorders of ovulation include oligoovulation and anovulation:[15]
- Anovulation is absence of ovulation when it would be normally expected (in a post-menarchal, premenopausal woman).[16] Anovulation usually manifests itself as irregularity of menstrual periods, that is, unpredictable variability of intervals, duration, or bleeding. Anovulation can also cause cessation of periods (secondary amenorrhea) or excessive bleeding (dysfunctional uterine bleeding).[17]
- Oligoovulation is infrequent or irregular ovulation (usually defined as cycles of >35 days or <8 cycles a year).[15][18]
Other menstrual disorders
- Dysmenorrhea (or dysmenorrhoea), cramps or painful menstruation, involves menstrual periods that are accompanied by either sharp, intermittent pain or dull, aching pain, usually in the pelvis or lower abdomen.[19]
Signs and symptoms of menstrual disorders

The signs and symptoms of menstrual disorders can cause significant stress. Abnormal uterine bleeding (AUB) has the potential to be one of the most urgent gynecological problems during menstruation. Dysmenorrhea is the most common.[2]
Premenstrual Syndrome (PMS)
Symptoms may include irritability, bloating, depression, food cravings, aggressiveness, and mood swings. Fluid retention and fluctuating weight gain are also reported.[4]
Precipitating risk factors include: stress, alcohol consumption, exercise, smoking, and some medications.[4]
Amenorrhea
Lack of a menses by the age of 16 where secondary sexual characteristics have developed or by the age of 14 where no secondary sexual characteristics have developed (primary amenorrhea), or lack of a menses for more than 3-6 months after first menstruation cycle.[2] Although missing a period is the main sign, other symptoms can include: excess facial, hair loss, headache, changes to vision, milky discharge from the breasts, or absence of breast development. [20]
Abnormal Uterine Bleeding
One-third of women will experience abnormal uterine bleeding in their life. Normal menstrual cycle has a frequency of 24 to 38 days, lasts 7 to 9 days, so bleeding that lasts longer could be considered abnormal. Very heavy bleeding (for example, needing to use 1 or more tampons or sanitary pads every hour) is another symptom.[21]
Dysmenorrhea
Especially painful or persistent menstrual cramping that occurs in the absence of any underlying pelvic disease.[4]
Pain radiating to the low back or upper thighs with onset of menstruation and lasting anywhere from 12–72 hours. Headache, nausea, vomiting, diarrhea, and fatigue may also accompany the pain. Pain may begin gradually, with the first several years of menses, and then intensified as menstruation becomes regular. Patients who also have secondary amenorrhea report symptoms beginning after age 20 and lasting 5–7 days with progressive worsening of pain over time. Pelvic pain is also reported.[4]
Causes of menstrual disorders
There are many causes of menstrual disorders, including uterine fibroids, hormonal imbalances, clotting disorders, cancer, sexually-transmitted infections, polycystic ovary syndrome, and genetics.[22] Uterine fibroids are benign, non-cancerous growths in the uterus that affect most women at some point in their lives and usually does not require treatment unless they cause intolerable symptoms.[23] Stress and lifestyle factors commonly impact menstruation, which includes weight changes, dieting, changes in exercise, travel, and illness.[24]
Amenorrhea
There are different causes depending on the type of menstrual order. Amenorrhea, or the absence of menstruation, is subdivided into primary and secondary amenorrhea. In primary amenorrhea, in which there is a failure to menstruate by the age of 16 with normal sexual development or by 14 without normal sexual development, causes can be from developmental abnormalities of the uterus, ovaries, or genital tract, or endocrine disorders. In secondary amenorrhea, or the absence of menstruation for greater than 6 months, can be caused by the same reasons as primary amenorrhea, as well as polycystic ovary syndrome, pregnancy, chronic illness, and certain drugs like cocaine and opioids.[25]
Hypomenorrhea
Causes of hypomenorrhea, or irregular light periods, include periods around menopause, eating disorders, excessive exercise, thyroid dysfunction, uncontrolled diabetes, Cushing's syndrome, hormonal birth control, and certain medications to treat epilepsy or mental health conditions.[26]
Menorrhagia
Causes of menorrhagia, or heavy menstrual bleeding, include polycystic ovary syndrome, uterine fibroids, endometrial polyps, bleeding disorders, and miscarriage.[26]
Dysmenorrhea
Causes of dysmenorrhea, or menstrual pain, include endometriosis, pelvic scarring due to chlamydia or gonorrhea, and intrauterine devices or IUDs.[26] Primary dysmenorrhea is when there is no underlying cause that is identified, and secondary dysmenorrhea is when the menstrual pain is caused by other conditions such as endometriosis, fibroids, or infection.[27]
Diagnosis of menstrual disorders
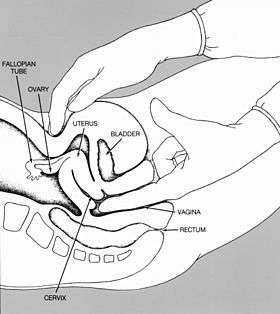
Diagnosis begins with an in-depth medical history and physical exam, including a pelvic exam and sometimes a Pap smear.[28]
Additional testing may include but are not limited to blood tests, hormonal tests, ultrasound, gynecologic ultrasound, magnetic resonance imaging (MRI), hysteroscopy, laparoscopy, endometrial biopsy, and dilation and curettage (D&C).[28]
Treatment of menstrual disorders
Premenstrual syndrome and premenstrual dysphoric disorder
Due to the unclear etiology of premenstrual syndrome and premenstrual dysphoric disorder, symptom relief is the primary goal of treatment. Selective serotonin reuptake inhibitors and spironolactone decrease physical and psychological symptoms associated with premenstrual syndrome. Oral contraceptives may ameliorate physical symptoms of breast tenderness and bloating. Ovarian suppression treatment with gonadotropin-releasing hormone agonist as an off-label use may reduce symptoms but have adverse side effects including decreased bone density. Other less commonly use medications such as alprazolam may reduce anxiety symptoms but has potential for dependence, tolerance, and abuse. Pyridoxine, a form of vitamin B6, may be used as a dietary supplement to relieve overall symptoms.[29][30][31]
Amenorrhea
Successful treatment varies depending on the diagnosis of amenorrhea. In patients with functional hypothalamic amenorrhea due to physical or psychological stress, non-pharmacological options include weight gain, resolution of emotional issues, or decreased intensity of exercise. Patients experiencing amenorrhea due to hypothyroidism may be started with thyroid replacement therapy. Dopamine agonists such as bromocriptine are used in patients with pituitary adenomas. Amenorrhea associated with gonadal dysgenesis or a hypoestrogenic state may be treated with oral contraceptives, patches, or vaginal rings.[4]
Amenorrhea associated with structural anomalies can be addressed with surgical treatment such as gonadectomy.[32]
Menorrhagia
Acute management of menstrual bleeding includes hormonal therapy with estrogen or oral contraceptives until bleeding has stopped followed by a oral contraceptive tapering regimen. Adjunctive therapy may include iron supplements and nonsteroidal anti-inflammatory drugs.[33] Patients who do not respond to hormonal therapy may use antifibrinolytics. Procedural therapy such as a suction curettage and intrauterine balloon tamponade are reserved for patients who do not respond to medication therapy and do not put fertility at risk. Life-threatening situations may consider more invasive procedures such as endometrial ablation, uterine artery embolization, and hysterectomy.[34]
Long-term management include estrogen-containing therapy and progestin therapy.[35]
Dysmenorrhea
Primary dysmenorrhea is commonly treated with nonsteroidal anti-inflammatory drugs such as ibuprofen to reduce moderate to severe pain. Other simple analgesics such as aspirin or acetaminophen are less commonly used but may also reduce short-term pain. Supplements including thiamine and vitamin E may reduce pain in younger women. Non-pharmacological interventions such as the use of external heat are also effective at reducing pain.[36]
See also
References
- "Menstrual disorders". Mount Sinai.
- Deligeoroglou E, Creatsas G (2012). "Menstrual disorders". In Sultan C (ed.). Pediatric and Adolescent Gynecology. Endocrine Development. 22. Basel: Karger Publishers. pp. 160–170. doi:10.1159/000331697. ISBN 978-3-8055-9336-6. PMID 22846527.
- Popat VB, Prodanov T, Calis KA, Nelson LM (2008). "The menstrual cycle: a biological marker of general health in adolescents". Annals of the New York Academy of Sciences. 1135 (1): 43–51. Bibcode:2008NYASA1135...43P. doi:10.1196/annals.1429.040. PMC 2755071. PMID 18574207.
- Krueger MV (2015). "Menstrual Disorders". In South-Paul JE, Matheny SC, Lewis EL (eds.). Current Diagnosis & Treatment: Family Medicine (4 ed.). New York, NY: McGraw-Hill Education. Retrieved 2020-07-31.
- Dickerson LM, Mazyck PJ, Hunter MH (April 2003). "Premenstrual syndrome". American Family Physician. 67 (8): 1743–52. PMID 12725453.
- Yonkers KA, O'Brien PM, Eriksson E (April 2008). "Premenstrual syndrome". Lancet. 371 (9619): 1200–10. doi:10.1016/S0140-6736(08)60527-9. PMC 3118460. PMID 18395582.
- Hantsoo L, Epperson CN (November 2015). "Premenstrual Dysphoric Disorder: Epidemiology and Treatment". Current Psychiatry Reports. 17 (11): 87. doi:10.1007/s11920-015-0628-3. PMC 4890701. PMID 26377947.
- "Amenorrhea". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2017.
- "Definition of Metrorrhagia". MedicineNet.com.
- Dunn A (2017). "7 Causes of Cramps before Periods". Medplux.
- "Oligomenorrhea". The Free Dictionary.
- "Polymenorrhea". Healthline. 2018.
- "Abnormal uterine bleeding: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2020-07-31.
- Long WN (1990). "Abnormal Vaginal Bleeding". In Walker HK, Hall WD, Hurst JW (eds.). Clinical Methods: The History, Physical, and Laboratory Examinations (3rd ed.). Boston: Butterworths. ISBN 978-0-409-90077-4. PMID 21250125. Retrieved 2020-07-30.
- "Ovulation Disorders - Jefferson University Hospitals". hospitals.jefferson.edu. Retrieved 2020-08-04.
- "Ovulation Disorders". Jefferson Health.
- "Anovulatory Cycle: When You Don't Release an Oocyte". Healthline. 2018.
- Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, et al. (2018). "Evaluation of Amenorrhea, Anovulation, and Abnormal Bleeding". Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. PMID 25905367.
- Calis KA (2020). "Dysmenorrhea: Practice Essentials, Background, Pathophysiology". MedScape. WebMD LLC.
- "What are the symptoms of amenorrhea?". NIH. Retrieved 2020-08-02.
- Davis E, Sparzak PB (2020). "Abnormal Uterine Bleeding (Dysfunctional Uterine Bleeding)". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30422508. Retrieved 2020-07-30.
- "Menstrual Disorders". Baylor College of Medicine.
- "Uterine Fibroids". Baylor College of Medicine.
- "Abnormal Menstruation (Periods): Types, Causes & Treatment". Cleveland Clinic.
- Hickey M, Balen A (2003). "Menstrual disorders in adolescence: investigation and management". Human Reproduction Update. 9 (5): 493–504. doi:10.1093/humupd/dmg038. PMID 14640381.
- "What causes menstrual irregularities?". Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
- "Dysmenorrhea: Painful Periods". The American College of Obstetricians and Gynecologists.
- "Menstrual Disorders". Baylor College of Medicine. Retrieved July 30, 2020.
- Biggs WS, Demuth RH (October 2011). "Premenstrual syndrome and premenstrual dysphoric disorder". American Family Physician. 84 (8): 918–24. PMID 22010771.
- Kwan I, Onwude JL (2008). "Premenstrual Syndrome". American Family Physician. 77 (1): 82. ISSN 0002-838X.
- Kwan I, Onwude JL (August 2015). "Premenstrual syndrome". BMJ Clinical Evidence. 2015: 0806. PMC 2907788. PMID 26303988.
- Yoon JY, Cheon CK (September 2019). "Evaluation and management of amenorrhea related to congenital sex hormonal disorders". Annals of Pediatric Endocrinology & Metabolism. 24 (3): 149–157. doi:10.6065/apem.2019.24.3.149. PMC 6790874. PMID 31607107.
- "Heavy Menstrual Bleeding". Centers for Disease Control and Prevention. U.S. Centers for Disease Control and Prevention (CDC). 2015. Retrieved 2020-07-28.
- Costlow LS (May 2020). "Heavy Menstrual Bleeding in Adolescents: ACOG Management Recommendations". American Family Physician. 101 (10): 633–635. PMID 32412210.
- Wouk N, Helton M (April 2019). "Abnormal Uterine Bleeding in Premenopausal Women". American Family Physician. 99 (7): 435–443. PMID 30932448.
- Latthe P, Champaneria R, Khan K (2012). "Dysmenorrhea". American Family Physician. 85 (4): 386–387. ISSN 0002-838X.