Cervical polyp
A cervical polyp is a common benign polyp or tumour on the surface of the cervical canal.[1] They can cause irregular menstrual bleeding but often show no symptoms. Treatment consists of simple removal of the polyp and prognosis is generally good. About 1% of cervical polyps will show neoplastic change which may lead to cancer. They are most common in post-menarche, pre-menopausal women who have been pregnant.
| Cervical polyp | |
|---|---|
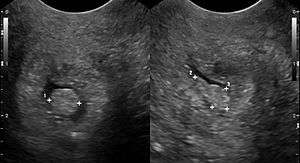 | |
| Cervical polyp on ultrasound | |
| Specialty | Gynecology |
Signs and symptoms
Cervical polyps often show no symptoms.[2] Where there are symptoms, they include intermenstrual bleeding, abnormally heavy menstrual bleeding (menorrhagia), vaginal bleeding in post-menopausal women, bleeding after sex and thick white vaginal or yellowish discharge (leukorrhoea).[3][4][5][6]
Cause
The cause of cervical polyps is uncertain, but they are often associated with inflammation of the cervix.[7] They may also occur as a result of raised levels of estrogen or clogged cervical blood vessels.[3]
Diagnosis
Cervical polyps can be seen during a pelvic examination as red or purple projections from the cervical canal.[3] Diagnosis can be confirmed by a cervical biopsy which will reveal the nature of the cells present.[3]
Structure
Cervical polyps are finger-like growths, generally less than 1 cm in diameter.[3][4] They are generally bright red in colour, with a spongy texture.[2] They may be attached to the cervix by a stalk (pedunculated) and occasionally prolapse into the vagina where they can be mistaken for endometrial polyps or submucosal fibroids.[4]
Treatment
Cervical polyps can be removed using ring forceps.[8] They can also be removed by tying surgical string around the polyp and cutting it off.[3] The remaining base of the polyp can then be removed using a laser or by cauterisation.[3] If the polyp is infected, an antibiotic may be prescribed.[3]
Prognosis
99% of cervical polyps will remain benign and 1% will at some point show neoplastic change.[9] Cervical polyps are unlikely to regrow.[3]
Epidemiology
Cervical polyps are most common in women who have had children and perimenopausal women.[2] They are rare in pre-menstrual girls and uncommon in post-menopausal women.[6]
See also
References
- Boon, Mathilde E.; Albert J. H. Suurmeijer (1996). The Pap Smear. Taylor & Francis. p. 87. ISBN 3-7186-5857-7.
- Zuber, Thomas J.; E. J. Mayeaux (2004). Atlas of Primary Care Procedures. Lippincott Williams & Wilkins. pp. 254–256. ISBN 0-7817-3905-5.
- Smith, Melanie N. (2006-05-10). "Cervical polyps". MEDLINE. Retrieved 2007-11-05.
- Bates, Jane (1997). Practical Gynaecological Ultrasound. Cambridge University Press. p. 77. ISBN 1-900151-51-0.
- Papadakis, Maxine A.; Stephen J. McPhee; Roni F. Zeiger (2005). Current Consult Medicine 2006. McGraw-Hill Professional. p. 60. ISBN 0-07-145892-1.
- Bosze, Peter; David M. Luesley (2004). Eagc Course Book on Colposcopy. Informa Health Care. p. 66. ISBN 963-00-7356-0.
- "Cervical Polyps" (PDF). Doncaster and Bassetlaw Hospitals (NHS). Archived from the original (PDF) on 2007-02-07. Retrieved 2007-10-21.
- Moore, Anne (2001-09-20). "How Should I Treat Postcoital Bleeding in a Premenopausal Patient?". Medscape.com. Retrieved 2007-10-21.
- Tillman, Elizabeth. "Short Instructor Materials" (PDF). Centers for Disease Control and Prevention. Archived from the original on 2006-04-23. Retrieved 2007-10-21.CS1 maint: BOT: original-url status unknown (link)
External links
| Classification | |
|---|---|
| External resources |