Flow diverter
A flow diverter is an endovascular prosthesis used to treat intracranial aneurysms.[1] It is placed in the aneurysm's parent artery, covering the neck, in order to divert blood flow and determine a progressive thrombosis of the sac.[2] Flow diverting stents consist of structural Cobalt-chrome or Nitinol alloy wires and often a set of radiopaque wires woven together in a flexible braid. [3]
| Flow diverter | |
|---|---|
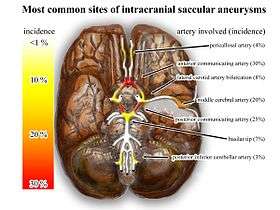 Common sites (intracranial) of saccular aneurysms (treated with flow diverter) | |
| Specialty | Interventional neuroradiology |
| ICD-10-PCS | Z95.828 |
Medical usage
Flow diverters are treatment for intracranial aneurysms alternative to endosaccular coil embolization (although the techniques can be combined, especially in large/giant aneurysms). It is mainly effective in wide neck unerupted saccular aneurysms, that are difficult to coil because of the tendency of the coils to fill the parent artery (referred to as prolapse). Another situation is fusiform shape or circumferential aneurysms. [4] Prior to flow diverters many intracranial aneurysms went untreated.[5]
Risks and complications
The efficacy of flow diverters can be evaluated using a grading system developed by researchers at Oxford Neurovascular and Neuroradiology Research Unit (Kamran et al. 2011), commonly referred to as flow diverter grading system or Kamran grading system.[6] After receiving a cerebral flow diverter, patients are placed on dual antiplatelet therapy for an extended period of time to reduce the likelihood of peri-procedural and post-procedural thromboembolic complications.
The degree of aneurysm occlusion is graded on a five-point scale from 0 (no change in the endoaneurysmal flow) to 4 (complete obliteration of the aneurysm). The patency status of the parent artery is evaluated on a three-point scale, from no change in the parent artery diameter to parent artery occlusion. This grading system is used in clinical practice. It has also been used and adapted by researchers to evaluate and report the effectiveness of flow diverters in general.[7]
References
- Alderazi Yazan J.; Shastri Darshan; Kass-Hout Tareq; Prestigiacomo Charles J.; Gandhi Chirag D. (2014). "Review Article: Flow Diverters for Intracranial Aneurysms". Stroke Research and Treatment. 2014: 1–12. doi:10.1155/2014/415653. PMC 4054970. PMID 24967131.
- Pierot, Laurent (2011). "Flow diverter stents in the treatment of intracranial aneurysms: Where are we?". Journal of Neuroradiology. 38 (1): 40–46. doi:10.1016/j.neurad.2010.12.002. PMID 21257202.
- Thomas, A. J.; Krings, T.; Pereira, V. M.; Moore, J. M.; Phan, K.; Dmytriw, A. A. (2019-03-21). "On Flow Diversion: The Changing Landscape of Intracerebral Aneurysm Management". American Journal of Neuroradiology. 40 (4): 591–600. doi:10.3174/ajnr.A6006. ISSN 0195-6108. PMID 30894358.
- Guo S.; Jiang P.; Liu J.; Yang X; Li Y.; Wu Z. (2017). "A comparative study of CFD of canine model of common carotid fusiform aneurysm and vertebrobasilar fusiform aneurysm in human patients". International Angiology. 37 (1): 32–40. doi:10.23736/S0392-9590.17.03869-X. PMID 28945061.
- Alderazi, Yazan J.; Shastri, Darshan; Kass-Hout, Tareq; Prestigiacomo, Charles J.; Gandhi, Chirag D. (2014). "Flow Diverters for Intracranial Aneurysms". Stroke Research and Treatment. 2014: 415653. doi:10.1155/2014/415653. PMC 4054970. PMID 24967131.
- Kamran M.; Yarnold J.; Grunwald I.Q.; Byrne J.V. (2011). "Assessment of angiographic outcomes after flow diversion treatment of intracranial aneurysms: a new grading schema". Neuroradiology. 53 (7): 501–508. doi:10.1007/s00234-010-0767-5. PMID 20838782.
- Darsaut, Tim E.; Bing, Fabrice; Makoyeva, Alina; Gevry, Guylaine; Salazkin, Igor; Raymond, Jean (2014). "Flow Diversion of Giant Curved Sidewall and Bifurcation Experimental Aneurysms with Very-Low-Porosity Devices". World Neurosurgery. 82 (6): 1120–1126. doi:10.1016/j.wneu.2013.09.036. PMID 24071065.
Further reading
- Jabbour, Pascal M. (2012). Neurovascular surgical techniques (First ed.). New Delhi: Jaypee Medical. ISBN 978-93-5090-088-8. Retrieved 23 September 2015.
- Krishna, Chandan; Sonig, Ashish; Natarajan, Sabareesh K.; Siddiqui, Adnan H. (October 2014). "The Expanding Realm of Endovascular Neurosurgery: Flow Diversion for Cerebral Aneurysm Management". Methodist DeBakey Cardiovascular Journal. 10 (4): 214–219. doi:10.14797/mdcj-10-4-214. PMC 4300059. PMID 25624975.