Polycythemia
Polycythemia (also known as polycythaemia or polyglobulia) is a disease state in which the hematocrit (the volume percentage of red blood cells in the blood) and/or hemoglobin concentration are elevated in peripheral blood.
| Polycythemia | |
|---|---|
| Other names | Polyglobulia |
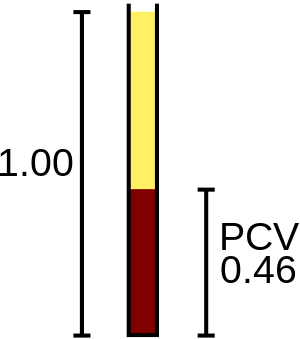 | |
| Packed cell volume diagram. | |
| Specialty | Hematology |
It can be due to an increase in the number of red blood cells[1] ("absolute polycythemia") or to a decrease in the volume of plasma ("relative polycythemia").[2] Polycythemia is sometimes called erythrocytosis, but the terms are not synonymous, because polycythemia refers to any increase in red blood cells, whereas erythrocytosis only refers to a documented increase of red cell mass.
The emergency treatment of polycythemia (e.g., in hyperviscosity or thrombosis) is by phlebotomy (removal of blood from the circulation). Depending on the underlying cause, phlebotomy may also be used on a regular basis to reduce the hematocrit. Cytostatics such as busulfan and hydroxyurea are sometimes used for long-term management of polycythemia.
Absolute polycythemia
The overproduction of red blood cells may be due to a primary process in the bone marrow (a so-called myeloproliferative syndrome), or it may be a reaction to chronically low oxygen levels or, rarely, a malignancy. Alternatively, additional red blood cells may have been received through another process—for example, being over-transfused (either accidentally or, as blood doping, deliberately) or being the recipient twin in a pregnancy, undergoing twin-to-twin transfusion syndrome.
Primary polycythemia
Primary polycythemias are due to factors intrinsic to red cell precursors. Polycythemia vera (PCV), polycythemia rubra vera (PRV), or erythremia, occurs when excess red blood cells are produced as a result of an abnormality of the bone marrow.[3] Often, excess white blood cells and platelets are also produced. PCV is classified as a myeloproliferative disease. Symptoms include headaches and vertigo, and signs on physical examination include an abnormally enlarged spleen and/or liver. In some cases, affected individuals may have associated conditions including high blood pressure or formation of blood clots. Transformation to acute leukemia is rare. Phlebotomy is the mainstay of treatment. A hallmark of polycythemia is an elevated hematocrit, with Hct > 55% seen in 83% of cases.[4] A somatic (non-hereditary) mutation (V617F) in the JAK2 gene is found in 95% of cases, though also present in other myeloproliferative disorders.[5]
Primary familial polycythemia, also known as primary familial and congenital polycythemia (PFCP), exists as a benign hereditary condition, in contrast with the myeloproliferative changes associated with acquired PCV. In many families, PFCP is due to an autosomal dominant mutation in the EPOR erythropoietin receptor gene.[6] PFCP can cause an increase of up to 50% in the oxygen-carrying capacity of the blood; skier Eero Mäntyranta had PFCP, which is considered to have given him a large advantage in endurance events.[7]
Secondary polycythemia
Secondary polycythemia is caused by either natural or artificial increases in the production of erythropoietin, hence an increased production of erythrocytes. In secondary polycythemia, 6 to 8 million and occasionally 9 million erythrocytes may occur per cubic millimeter of blood. Secondary polycythemia resolves when the underlying cause is treated.
Secondary polycythemia in which the production of erythropoietin increases appropriately is called physiologic polycythemia.
Conditions which may result in a physiologically appropriate polycythemia include:
- Altitude related – This physiologic polycythemia is a normal adaptation to living at high altitudes (see altitude sickness). Many athletes train at high altitude to take advantage of this effect—a legal form of blood doping. Some individuals believe athletes with primary polycythemia may have a competitive advantage due to greater stamina. However, this has yet to be proven due to the multifaceted complications associated with this condition.
- Hypoxic disease-associated – for example in cyanotic heart disease where blood oxygen levels are reduced significantly, may also occur as a result of hypoxic lung disease such as COPD and as a result of chronic obstructive sleep apnea.
- Iatrogenic – Secondary polycythemia can be induced directly by phlebotomy (blood letting) to withdraw some blood, concentrate the erythrocytes, and return them to the body.
- Genetic – Heritable causes of secondary polycythemia also exist and are associated with abnormalities in hemoglobin oxygen release. This includes patients who have a special form of hemoglobin known as Hb Chesapeake, which has a greater inherent affinity for oxygen than normal adult hemoglobin. This reduces oxygen delivery to the kidneys, causing increased erythropoietin production and a resultant polycythemia. Hemoglobin Kempsey also produces a similar clinical picture. These conditions are relatively uncommon.
Conditions where the secondary polycythemia is not as a result of physiologic adaptation and occurs irrespective of body needs include:
- Neoplasms – Renal cell carcinoma or liver tumors, von Hippel-Lindau disease, and endocrine abnormalities including pheochromocytoma and adrenal adenoma with Cushing's syndrome.
- People whose testosterone levels are high because of the use of anabolic steroids, including athletes who abuse steroids, or people on testosterone replacement for hypogonadism or transgender hormone replacement therapy, as well as people who take erythropoietin, may develop secondary polycythemia.
Altered oxygen sensing
Inherited mutations in three genes which all result in increased stability of hypoxia-inducible factors, leading to increased erythropoietin production, have been shown to cause erythrocytosis:
- Chuvash polycythemia is an autosomal recessive form of erythrocytosis which is endemic in patients from Chuvashia, an autonomous republic within the Russian Federation. Chuvash polycythemia is associated with homozygosity for a C598T mutation in the von Hippel-Lindau gene (VHL), which is needed for the destruction of hypoxia-inducible factors in the presence of oxygen.[8] Clusters of patients with Chuvash polycythemia have been found in other populations, such as on the Italian island of Ischia, located in the Bay of Naples.[9]
- PHD2 erythrocytosis: Heterozygosity for loss-of-function mutations of the PHD2 gene are associated with autosomal dominant erythrocytosis and increased hypoxia-inducible factors activity.[10][11]
- HIF2α erythrocytosis: Gain-of-function mutations in HIF2α are associated with autosomal dominant erythrocytosis[12] and pulmonary hypertension.[13]
Relative polycythemia
Relative polycythemia is an apparent rise of the erythrocyte level in the blood; however, the underlying cause is reduced blood plasma (hypovolemia, cf. dehydration). Relative polycythemia is often caused by loss of body fluids, such as through burns, dehydration, and stress. A specific type of relative polycythemia is Gaisböck syndrome. In this syndrome, primarily occurring in obese men, hypertension causes a reduction in plasma volume, resulting in (amongst other changes) a relative increase in red blood cell count.[14]
See also
- Cytopenia, a decrease in blood cell count
- Capillary leak syndrome, another cause of hemoconcentration
References
- "absolute polycythemia" at Dorland's Medical Dictionary
- "relative polycythemia" at Dorland's Medical Dictionary
- MedlinePlus Encyclopedia: Polycythemia vera
- Jacques Wallach; Interpretation of Diagnostic Tests, 7th Ed.; Lippencott Williams & Wilkins
- Current Medical Diagnosis & Treatment. McGraw Hill Lange. 2008. p. 438.
- OMIM – Polycythemia, Primary Familial snd Congenital; PFCP
- Guardian newspaper: interview with Malcolm Gladwell, 29 September 2013
- Ang SO, Chen H, Hirota K, et al. (December 2002). "Disruption of oxygen homeostasis underlies congenital Chuvash polycythemia". Nat. Genet. 32 (4): 614–21. doi:10.1038/ng1019. PMID 12415268. S2CID 15582610.
- Perrotta S, Nobili B, Ferraro M, et al. (January 2006). "Von Hippel-Lindau-dependent polycythemia is endemic on the island of Ischia: identification of a novel cluster". Blood. 107 (2): 514–29. doi:10.1182/blood-2005-06-2422. PMID 16210343. S2CID 17065771.
- Percy MJ, Zhao Q, Flores A, et al. (January 2006). "A family with erythrocytosis establishes a role for prolyl hydroxylase domain protein 2 in oxygen homeostasis". Proc. Natl. Acad. Sci. U.S.A. 103 (3): 654–59. doi:10.1073/pnas.0508423103. PMC 1334658. PMID 16407130.
- Percy MJ, Furlow PW, Beer PA, Lappin TR, McMullin MF, Lee FS (September 2007). "A novel erythrocytosis-associated PHD2 mutation suggests the location of a HIF binding groove". Blood. 110 (6): 2193–96. doi:10.1182/blood-2007-04-084434. PMC 1976349. PMID 17579185.
- Percy MJ, Furlow PW, Lucas GS, et al. (January 2008). "A gain-of-function mutation in the HIF2A gene in familial erythrocytosis". N. Engl. J. Med. 358 (2): 162–68. doi:10.1056/NEJMoa073123. PMC 2295209. PMID 18184961.
- Gale DP, Harten SK, Reid CD, Tuddenham EG, Maxwell PH (August 2008). "Autosomal dominant erythrocytosis and pulmonary arterial hypertension associated with an activating HIF2 alpha mutation". Blood. 112 (3): 919–21. doi:10.1182/blood-2008-04-153718. PMID 18650473. S2CID 14580718.
- Stefanini, Mario; Urbas, John V.; Urbas, John E. (July 1978). "Gaisböck's syndrome: its hematologic, biochemical and hormonal parameters". Angiology. 29 (7): 520–33. doi:10.1177/000331977802900703. ISSN 0003-3197. PMID 686487. S2CID 42326090.
External links
| Classification | |
|---|---|
| External resources |