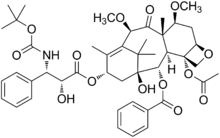
Cabazitaxel
Cabazitaxel (previously XRP-6258, trade name Jevtana) is a semi-synthetic derivative of a natural taxoid.[1] It was developed by Sanofi-Aventis and was approved by the U.S. FDA for the treatment of hormone-refractory prostate cancer on June 17, 2010. It is a microtubule inhibitor, and the fourth taxane to be approved as a cancer therapy.[2]
 | |
| Clinical data | |
|---|---|
| Trade names | Jevtana |
| AHFS/Drugs.com | Consumer Drug Information |
| MedlinePlus | a611009 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.205.741 |
| Chemical and physical data | |
| Formula | C45H57NO14 |
| Molar mass | 835.944 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Cabazitaxel in combination with prednisone is a treatment option for hormone-refractory prostate cancer following docetaxel-based treatment.
Mechanism of action
Taxanes enhance the microtubules stabilization and inhibit the cellular mitosis and division.[3] Moreover, taxanes prevent androgen receptor (AR) signaling by binding cellular microtubules and the microtubule-associated motor protein dynein, thus averting AR nuclear translocation.[4]
Clinical trials
In patients with metastatic castration-resistant prostate cancer (mCRPC), overall survival (OS) is markedly enhanced with cabazitaxel versus mitoxantrone after prior docetaxel treatment. FIRSTANA (ClinicalTrials.gov identifier: NCT01308567) assessed whether cabazitaxel 20 mg/m2 (C20) or 25 mg/m2 (C25) is superior to docetaxel 75 mg/m2 (D75) in terms of OS in patients with chemotherapy-naïve mCRPC. However, C20 and C25 did not demonstrate superiority for OS versus D75 in patients with chemotherapy-naïve mCRPC. Cabazitaxel and docetaxel demonstrated different toxicity profiles, and C20 showed the overall lowest toxicity.[5] In a phase III trial with 755 men for the treatment of castration-resistant prostate cancer, median survival was 15.1 months for patients receiving cabazitaxel versus 12.7 months for patients receiving mitoxantrone. Cabazitaxel was associated with more grade 3–4 neutropenia (81.7%) than mitoxantrone (58%).[6] Common adverse effects with cabazitaxel include neutropenia (including febrile neutropenia) and GIT side effects appeared mainly in diarrhea, whereas, neuropathy was rarely detected.[7]
Pharmacokinetics
Cabazitaxel administration causes a decrease in plasma concentrations showing triphasic kinetics: a mean half life (t1/2) of 2.6 min in the first phase, a mean t1/2 of 1.3 h in the second phase, and a mean t1/2 of 77.3 h in the third phase.[8]
Metabolism
Cabazitaxel is basically metabolized in the liver by [cytochrome P450 (CYP)3A4/5 > CYP2C8], which result in seven plasma metabolites and excreted 20 metabolites. During 14 days after administration, 80% of cabazitaxel is excreted: 76% in the feces and 3.7% as a renal excretion.[9]
Dosing of Cabazitaxel
There are many questions about the optimal use of Cabazitaxel after the approval of using it in the treatment of docetaxel-refractory mCRPC. One question is about the optimal use. Concerning the significant myelosuppression during cabazitaxel administration at 25 mg/m2, a randomized phase III study will appraise the safety and efficacy of cabazitaxel at 20 mg/m2. One more question is about the effectiveness and tolerability of cabazitaxel when it is administered with other therapies. A phase I/II trials are testing the co-administration of cabazitaxel with other therapies (e.g. abiraterone) and investigational agents (e.g. custirsen)[9]
See also
References
- "Cabazitaxel". NCI Drug Dictionary. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. 2011-02-02.
- "Jevtana (cabazitaxel) Injection Approved by U.S. FDA After Priority Review" (Press release). sanofi-aventis. 2010-06-17. Retrieved June 17, 2010.
- Jordan MA, Wilson L (April 2004). "Microtubules as a target for anticancer drugs". Nature Reviews. Cancer. 4 (4): 253–65. doi:10.1038/nrc1317. PMID 15057285.
- Darshan MS, Loftus MS, Thadani-Mulero M, Levy BP, Escuin D, Zhou XK, et al. (September 2011). "Taxane-induced blockade to nuclear accumulation of the androgen receptor predicts clinical responses in metastatic prostate cancer". Cancer Research. 71 (18): 6019–29. doi:10.1158/0008-5472.CAN-11-1417. PMC 3354631. PMID 21799031.
- Oudard S, Fizazi K, Sengeløv L, Daugaard G, Saad F, Hansen S, et al. (October 2017). "Cabazitaxel Versus Docetaxel As First-Line Therapy for Patients With Metastatic Castration-Resistant Prostate Cancer: A Randomized Phase III Trial-FIRSTANA". Journal of Clinical Oncology. 35 (28): 3189–3197. doi:10.1200/JCO.2016.72.1068. PMID 28753384.
- "Cabazitaxel Effective for Hormone Refractory Prostate Cancer After Failure of Taxotere".
- Paller CJ, Antonarakis ES (March 2011). "Cabazitaxel: a novel second-line treatment for metastatic castration-resistant prostate cancer". Drug Design, Development and Therapy. 5: 117–24. doi:10.2147/DDDT.S13029. PMC 3063116. PMID 21448449.
- Mita AC, Denis LJ, Rowinsky EK, Debono JS, Goetz AD, Ochoa L, et al. (January 2009). "Phase I and pharmacokinetic study of XRP6258 (RPR 116258A), a novel taxane, administered as a 1-hour infusion every 3 weeks in patients with advanced solid tumors". Clinical Cancer Research. 15 (2): 723–30. doi:10.1158/1078-0432.CCR-08-0596. PMID 19147780.
- Tsao CK, Cutting E, Martin J, Oh WK (June 2014). "The role of cabazitaxel in the treatment of metastatic castration-resistant prostate cancer". Therapeutic Advances in Urology. 6 (3): 97–104. doi:10.1177/1756287214528557. PMC 4003844. PMID 24883107.
External links
- Cabazitaxel – Official web site of manufacturer.
- Cabazitaxel Prescribing Information – Official prescribing information.
- U.S. National Library of Medicine: Drug Information Portal – Cabazitaxel