Hand washing
Hand washing (or handwashing), also known as hand hygiene, is the act of cleaning one's hands with soap (or equivalent materials) and water to remove viruses/ bacteria/germs/ microorganisms, dirt, grease, or other harmful and unwanted substances stuck to the hands. Drying of the washed hands is part of the process as wet and moist hands are more easily recontaminated.[1][2]
| Hand washing | |
|---|---|
 | |
| Other names | Handwashing, hand hygiene |
The World Health Organization recommends washing hands for at least 20 seconds before/after the following:[3]
- Before and after caring for any sick person
- Before, during, and after preparing food
- Before eating
- After using the toilet (for urination, defecation, menstrual hygiene),
- After helping someone who just used the toilet
- After blowing one's nose, or coughing or sneezing
- After touching an animal, animal feed or animal waste
- After touching garbage
However, if soap and water are not available, hand sanitizer that is at least 60% (v/v) alcohol in water (specifically, ethanol or isopropyl alcohol/isopropanol (rubbing alcohol)) can be used instead, unless hands are visibly excessively dirty or greasy.[4][5] When both hand washing and using hand sanitizer are not available, hands can be cleaned with ash and clean water, although the benefits and harms are uncertain for reducing the spread of viral or bacterial infections.[6]
Hand washing with soap – often, and throughout the day – prevents the spread of many diseases, for example diarrhoea and cholera which are transmitted through fecal–oral route. People can also become infected with respiratory diseases, such as influenza, the common cold or the new Coronavirus also known as COVID-19 if they do not wash their hands before touching their eyes, nose, or mouth (i.e., mucous membranes).
Medical hand hygiene refers to hygiene practices related to medical procedures. Hand washing before administering medicine or medical care can prevent or minimize the spread of disease. The main medical purpose of washing hands is to cleanse the hands of pathogens (bacteria, viruses, or other microorganisms) and chemicals which can cause harm. This is especially important for people who handle food or work in the medical field, but also an important practice for the general public. However, frequent hand washing can lead to skin damage due to drying of the skin.[7]
Symbolic hand washing, using water but no soap to wash hands, is a part of ritual hand washing featured in many religions, including Bahá'í Faith, Hinduism, tevilah and netilat yadayim in Judaism, Lavabo in Christianity, and Wudhu in Islam. Religions also prescribe hygienic hand washing, especially after certain actions. Hinduism, Judaism and Islam mandate washing of hands after using the toilet. And, Hinduism, Buddhism, Sikhism, Judaism and Islam mandate washing of hands before and after every meal.[8]
Public health
Health benefits
Hand washing has many health benefits, including minimizing the spread of influenza, coronavirus, and other infectious diseases;[9][10] preventing infectious causes of diarrhea;[11] decreasing respiratory infections;[12] and reducing infant mortality rate at home birth deliveries.[13] A 2013 study showed that improved hand washing practices may lead to small improvements in the length growth in children under five years of age.[14] In developing countries, childhood mortality rates related to respiratory and diarrheal diseases can be reduced by introducing simple behavioral changes, such as hand washing with soap. This simple action can reduce the rate of mortality from these diseases by almost 50%.[15] Interventions that promote hand washing can reduce diarrhoea episodes by about a third, and this is comparable to providing clean water in low income areas.[16] 48% of reductions in diarrhoea episodes can be associated with hand washing with soap.[17]
Hand washing with soap is the single most effective and inexpensive way to prevent diarrhea and acute respiratory infections (ARI), as automatic behavior performed in homes, schools, and communities worldwide. Pneumonia, a major ARI, is the number one cause of mortality among children under five years old, taking the lives of an estimated 1.8 million children per year. Diarrhea and pneumonia together account for almost 3.5 million child deaths annually.[18] According to UNICEF, turning hand washing with soap before eating and after using the toilet into an ingrained habit can save more lives than any single vaccine or medical intervention, cutting deaths from diarrhea by almost half and deaths from acute respiratory infections by one-quarter. Hand washing is usually integrated together with other sanitation interventions as part of water, sanitation and hygiene (WASH) programmes. Hand washing also protects against impetigo which is transmitted through direct physical contact.[19]
Adverse effects
A small detrimental effect of hand washing is that frequent hand washing can lead to skin damage due to the drying of the skin.[7] A 2012 Danish study found that excessive hand washing can lead to an itchy, flaky skin condition known as hand eczema or hand dermatitis, which is especially common among health-care workers.[20] Too frequent hand washing is also seen as one of the symptoms of obsessive-compulsive disorder (OCD).
When it is recommended
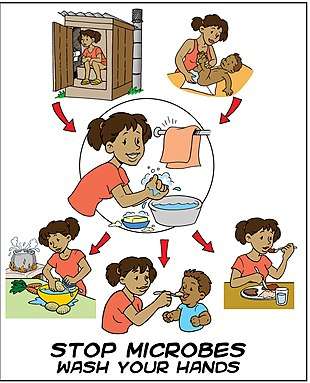
There are five critical times during the day where washing hands with soap is important to reduce fecal-oral transmission of disease: after using the toilet (for urination, defecation, menstrual hygiene), after cleaning a child's bottom (changing nappies), before feeding a child, before eating and before/after preparing food or handling raw meat, fish, or poultry.[21] Other occasions when correct handwashing technique should be practiced in order to prevent the transmission of disease include before and after treating a cut or wound; after sneezing, coughing, or blowing your nose; after touching animal waste or handling animals; and after touching garbage.[22][23]
Behavior change
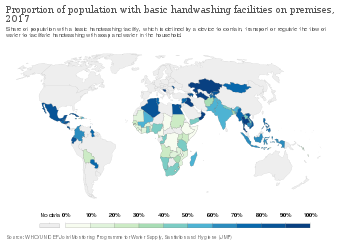
In many countries, there is a low rate of hand washing with soap. A study of hand washing in 54 countries in 2015 found that on average, 38.7% of households practiced hand washing with soap.[24]
A 2014 study showed that Saudi Arabia had the highest rate of 97 percent; the United States near the middle with 77 percent; and China with the lowest rate of 23 percent.[25]
Several behavior change methodologies now exist to increase uptake of the behavior of hand washing with soap at the critical times.[26]
Group hand washing for school children at set times of the day is one option in developing countries to engrain hand washing in children's behaviors.[27] The "Essential Health Care Program" implemented by the Department of Education in the Philippines is an example of at scale action to promote children's health and education.[28] Deworming twice a year, supplemented with washing hands daily with soap, brushing teeth daily with fluoride, is at the core of this national program. It has also been successfully implemented in Indonesia.[29]
Substances used
Soap and detergents
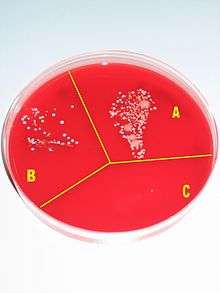
Removal of microorganisms from skin is enhanced by the addition of soaps or detergents to water.[30] The main action of soaps and detergents is to reduce barriers to solution, and increase solubility. Water alone is an inefficient skin cleanser because fats and proteins, which are components of organic soil, are not readily dissolved in water. Cleansing is, however, aided by a reasonable flow of water..
Solid soap
Solid soap, because of its reusable nature, may hold bacteria acquired from previous uses.[31] A small number of studies which have looked at the bacterial transfer from contaminated solid soap have concluded transfer is unlikely as the bacteria are rinsed off with the foam.[32] The CDC still states "liquid soap with hands-free controls for dispensing is preferable".[33]
Antibacterial soap
Antibacterial soaps have been heavily promoted to a health-conscious public. To date, there is no evidence that using recommended antiseptics or disinfectants selects for antibiotic-resistant organisms in nature.[34] However, antibacterial soaps contain common antibacterial agents such as triclosan, which has an extensive list of resistant strains of organisms. So, even if antibiotic resistant strains aren't selected for by antibacterial soaps, they might not be as effective as they are marketed to be. Besides the surfactant and skin-protecting agent, the sophisticated formulations may contain acids (acetic acid, ascorbic acid, lactic acid) as pH regulator, antimicrobially active benzoic acid and further skin conditioners (aloe vera, vitamins, menthol, plant extracts).[35]
A 2007 meta-analysis from the University of Oregon School of Public Health indicated that plain soaps are as effective as consumer-grade anti-bacterial soaps containing triclosan in preventing illness and removing bacteria from the hands.[36]. Dissenting, a 2011 meta-analysis in the Journal of Food Protection argued that when properly formulated, triclosan can grant a small but detectable improvement, as can chlorhexidine gluconate, iodophor, or povidone.[37][38]
Warm water
Hot water that is still comfortable for washing hands is not hot enough to kill bacteria. Bacteria grow much faster at body temperature (37 °C). WHO considers warm soapy water to be more effective than cold, soapy water at removing natural oils which hold soils and bacteria.[39] But CDC mentions that warm water causes skin irritations more often and its ecological footprint is more significant.[1] Water temperatures from 4 to 40 °C do not differ significantly regarding removal of microbes. The most important factor is proper scrubbing.[40]
Contrary to popular belief, scientific studies have shown that using warm water has no effect on reducing the microbial load on hands.[41][40]
Antiseptics

A hand sanitizer or hand antiseptic is a non-water-based hand hygiene agent. In the late 1990s and early part of the 21st century, alcohol rub non-water-based hand hygiene agents (also known as alcohol-based hand rubs, antiseptic hand rubs, or hand sanitizers) began to gain popularity. Most are based on isopropyl alcohol or ethanol formulated together with a thickening agent such as Carbomer (polymer of acrylic acid) into a gel, or a humectant such as glycerin into a liquid, or foam for ease of use and to decrease the drying effect of the alcohol.[42] Adding diluted hydrogen-peroxide increases further the antimicrobial activity.[43]
Hand sanitizers containing a minimum of 60 to 95% alcohol are efficient germ killers. Alcohol rub sanitizers kill bacteria, multi-drug resistant bacteria (MRSA and VRE), tuberculosis, and some viruses (including HIV, herpes, RSV, rhinovirus, vaccinia, influenza,[44] and hepatitis) and fungi. Alcohol rub sanitizers containing 70% alcohol kill 99.97% (3.5 log reduction, similar to 35 decibel reduction) of the bacteria on hands 30 seconds after application and 99.99% to 99.999% (4 to 5 log reduction) of the bacteria on hands 1 minute after application.[45]
Hand sanitizers are most effective against bacteria and less effective against some viruses. Alcohol-based hand sanitizers are almost entirely ineffective against norovirus (or Norwalk) type viruses, the most common cause of contagious gastroenteritis.[46]
In a 2020 Cochrane review comparing rinse-free hand washing to conventional soap and water techniques and the subsequent impact on school absenteeism found a small but beneficial effect on rinse-free hand washing on illness related absenteeism.[47]
Enough hand antiseptic or alcohol rub must be used to thoroughly wet or cover both hands. The front and back of both hands and between and the ends of all fingers must be rubbed for approximately 30 seconds until the liquid, foam or gel is dry. Finger tips must be washed well too, rubbing them in both palms.[48]
US Centers for Disease Control and Prevention recommend hand washing over hand sanitizer rubs, particularly when hands are visibly dirty.[49] The increasing use of these agents is based on their ease of use and rapid killing activity against micro-organisms; however, they should not serve as a replacement for proper hand washing unless soap and water are unavailable.
Frequent use of alcohol-based hand sanitizers can cause dry skin unless emollients and/or skin moisturizers are added to the formula. The drying effect of alcohol can be reduced or eliminated by adding glycerin and/or other emollients to the formula[42]. In clinical trials, alcohol-based hand sanitizers containing emollients caused substantially less skin irritation and dryness than soaps or antimicrobial detergents. Allergic contact dermatitis, contact urticaria syndrome or hypersensitivity to alcohol or additives present in alcohol hand rubs rarely occur.[50] The lower tendency to induce irritant contact dermatitis became an attraction as compared to soap and water hand washing.
Despite their effectiveness, non-water agents do not cleanse the hands of organic material, but simply disinfect them. It is for this reason that hand sanitizers are not as effective as soap and water at preventing the spread of many pathogens, since the pathogens still remain on the hands.
Alcohol-free hand sanitizer efficacy is heavily dependent on the ingredients and formulation, and historically has significantly under-performed alcohol and alcohol rubs. More recently, formulations that use benzalkonium chloride have been shown to have persistent and cumulative antimicrobial activity after application,[51] unlike alcohol, which has been shown to decrease in efficacy after repeated use, probably due to progressive adverse skin reactions.[52]
Wipes
Hand washing using hand sanitizing wipes is an alternative during traveling in the absence of soap and water.[53] Alcohol-based hand sanitizer should contain at least 60% alcohol.[54]
Ash or mud
Many people in low-income communities cannot afford soap and use ash or soil instead. The World Health Organization recommended ash or sand as an alternative to soap when soap is not available.[55] Evidence quality to support the use of ash to wash hands is poor and it is not clear if washing hands with ash is effective at reducing viral or bacterial spreading compared to washing with mud, not washing, or with washing with water alone.[6] One concern is that if the soil or ash is contaminated with microorganisms it may increase the spread of disease rather than decrease it,[56] however, there is also no clear evidence to determine the level of risk.[6] Like soap, ash is also a disinfecting agent because in contact with water, it forms an alkaline solution.[57]
Techniques
Correct handwashing technique recommended by the US Centers for Disease Control for prevention of transmission of disease includes the following steps:[58]
- Wet hands with warm or cold running water.[58] Running water is recommended because standing basins may be contaminated, while the temperature of the water does not seem to make a difference.[1]
- Lather hands by rubbing them with a generous amount of soap, including the backs of hands, between fingers, and under nails.[58] Soap lifts germs from the skin, and studies show that people tend to wash their hands more thoroughly when soap is used rather than water alone.[1]
- Scrub for at least 20 seconds.[58] Scrubbing creates friction, which helps remove germs from skin, and scrubbing for longer periods removes more germs.[1]
- Rinse well under running water.[58] Rinsing in a basin can recontaminate hands.[1]
- Dry with a clean towel or allow to air dry.[58] Wet and moist hands are more easily recontaminated.[1]
The most commonly missed areas are the thumb, the wrist, the areas between the fingers, and under fingernails. Artificial nails and chipped nail polish may harbor microorganisms.[59] Moisturizing lotion is often recommended to keep the hands from drying out; dry skin can lead to skin damage which can increase the risk for the transmission of infection.[59]
Technologies and design aspects
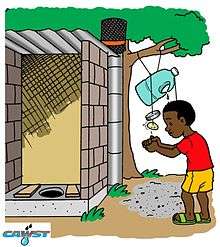
Low-cost options when water is scarce
Various low-cost options can be made to facilitate hand washing where tap-water and/or soap is not available e.g. pouring water from a hanging jerrycan or gourd with suitable holes and/or using ash if needed in developing countries.[60]
In situations with limited water supply (such as schools or rural areas in developing countries), there are water-conserving solutions, such as "tippy-taps" and other low-cost options.[61] A tippy-tap is a simple technology using a jug suspended by a rope, and a foot-operated lever to pour a small amount of water over the hands and a bar of soap.[62]
Low-cost handwashing technologies for households may differ from facilities for multiple users.[63] For households, options include tippy taps, bucket/container with tap, conventional tap with/without basin, valve/tap fitted to bottles, bucket and cup, camp sink.[63] Options for multiple users include: adapting household technologies for multiple users, water container fitted to a pipe with multiple taps, water container fitted to a pipe with holes.[63]
 Schoolchildren washing their hands before eating lunch in 1940s United States
Schoolchildren washing their hands before eating lunch in 1940s United States_(5601466470).jpg) Tanzanian drawing of a tippy tap with soap for hand washing at a school
Tanzanian drawing of a tippy tap with soap for hand washing at a school.jpg) Students washing their hands with a simple handwasher at a school in Zimbabwe
Students washing their hands with a simple handwasher at a school in Zimbabwe- Hand washer
Drying with towels or hand driers
Effective drying of the hands is an essential part of the hand hygiene process. Therefore, the proper drying of hands after washing should be an integral part of the hand hygiene process in health care.[2] However, there is some debate over the most effective form of drying in public toilets. A growing volume of research suggests paper towels are much more hygienic than the electric hand dryers found in many public toilets. A review in 2012 concluded that "From a hygiene standpoint, paper towels are superior to air dryers; therefore, paper towels should be recommended for use in locations in which hygiene is paramount, such as hospitals and clinics."[2]
Jet-air dryers were found to be capable of blowing micro-organisms from the hands and the unit and potentially contaminating other users and the environment up to 2 metres away.[64] In the same study in 2008 (sponsored by the paper-towel industry the European Tissue Symposium), use of a warm-air hand dryer spread micro-organisms only up to 0.25 metres from the dryer, and paper towels showed no significant spread of micro-organisms.
Accessibility
Making handwashing facilities accessible (inclusive) to everyone is crucial to maintain handwashing behaviour.[63]:27 Considerations for accessibility include age, disability, seasonality (with rains and muddiness), location and more. Important aspects for good accessibility include: Placement of the technology, paths, ramps, steps, type of tap, soap placement.[63]:27
Medical use
Medical hand-washing became mandatory long after Hungarian physician Ignaz Semmelweis discovered its effectiveness (in 1846) in preventing disease in a hospital environment.[65] There are electronic devices that provide feedback to remind hospital staff to wash their hands when they forget.[66] One study has found decreased infection rates with their use.[67]
Method
Medical hand-washing is for a minimum of 15 seconds, using generous amounts of soap and water or gel to lather and rub each part of the hands.[68] Hands should be rubbed together with digits interlocking. If there is debris under fingernails, a bristle brush may be used to remove it. Since germs may remain in the water on the hands, it is important to rinse well and wipe dry with a clean towel.[69] After drying, the paper towel should be used to turn off the water (and open any exit door if necessary). This avoids re-contaminating the hands from those surfaces.
The purpose of hand-washing in the health-care setting is to remove pathogenic microorganisms ("germs") and avoid transmitting them. The New England Journal of Medicine reports that a lack of hand-washing remains at unacceptable levels in most medical environments, with large numbers of doctors and nurses routinely forgetting to wash their hands before touching patients, thus transmitting microorganisms.[70] One study showed that proper hand-washing and other simple procedures can decrease the rate of catheter-related bloodstream infections by 66 percent.[71]
The World Health Organization has published a sheet demonstrating standard hand-washing and hand-rubbing in health-care sectors.[72] The draft guidance of hand hygiene by the organization can also be found at its website for public comment.[39] A relevant review was conducted by Whitby et al.[73] Commercial devices can measure and validate hand hygiene, if demonstration of regulatory compliance is required.
The World Health Organization has "Five Moments" for washing hands:
- before patient care
- after environmental contact
- after exposure to blood/body fluids
- before an aseptic task, and
- after patient care.
The addition of antiseptic chemicals to soap ("medicated" or "antimicrobial" soaps) confers killing action to a hand-washing agent. Such killing action may be desired prior to performing surgery or in settings in which antibiotic-resistant organisms are highly prevalent.[74]
To 'scrub' one's hands for a surgical operation, it is necessary to have a tap that can be turned on and off without touching it with the hands, some chlorhexidine or iodine wash, sterile towels for drying the hands after washing, and a sterile brush for scrubbing and another sterile instrument for cleaning under the fingernails. All jewelry should be removed. This procedure requires washing the hands and forearms up to the elbow, usually 2–6 minutes. Long scrub-times (10 minutes) are not necessary. When rinsing, water on the forearms must be prevented from running back to the hands. After hand-washing is completed, the hands are dried with a sterile cloth and a surgical gown is donned.
Effectiveness in healthcare settings
To reduce the spread of germs, it is better to wash the hands or use a hand antiseptic before and after tending to a sick person.
For control of staphylococcal infections in hospitals, it has been found that the greatest benefit from hand-cleansing came from the first 20% of washing, and that very little additional benefit was gained when hand cleansing frequency was increased beyond 35%.[75] Washing with plain soap results in more than triple the rate of bacterial infectious disease transmitted to food as compared to washing with antibacterial soap.[76]
Comparing hand-rubbing with alcohol-based solution with hand washing with antibacterial soap for a median time of 30 seconds each showed that the alcohol hand-rubbing reduced bacterial contamination 26% more than the antibacterial soap.[77] But soap and water is more effective than alcohol-based hand rubs for reducing H1N1 influenza A virus[78] and Clostridium difficile spores from hands.[79]
Interventions to improve hand hygiene in healthcare settings can involve education for staff on hand washing, increasing the availability of alcohol-based hand rub, and written and verbal reminders to staff.[80] There is a need for more research into which of these interventions are most effective in different healthcare settings.[80]
Developing countries
.jpg)
In developing countries, hand washing with soap is recognized as a cost-effective, essential tool for achieving good health, and even good nutrition.[28] However, a lack of reliable water supply, soap or hand washing facilities in people's homes, at schools and at the workplace make it a challenge to achieve universal hand washing behaviors. For example, in most of rural Africa hand washing taps close to every private or public toilet are scarce, even though cheap options exist to build hand washing stations.[61] However, low hand washing rates rather can also be the result of engrained habits rather than due to a lack of soap or water.[82]
Hand washing at a global level has its own indicator within Sustainable Development Goal 6, Target 6.2 which states "By 2030, achieve access to adequate and equitable sanitation and hygiene for all and end open defecation, paying special attention to the needs of women and girls and those in vulnerable situations.[81] The corresponding Indicator 6.2.1 is formulated as follows: Proportion of population using (a) safely managed sanitation services and (b) a hand-washing facility with soap and water" (see map to the right with data worldwide from 2017).
Promotion campaigns
The promotion and advocacy of hand washing with soap can influence policy decisions, raise awareness about the benefits of hand washing and lead to long-term behavior change of the population.[83] For this to work effectively, monitoring and evaluation are necessary. A systematic review of 70 studies found that community-based approaches are effective at increasing hand washing in LMICs, while social marketing campaigns are less effective.[84]
One example for hand washing promotion in schools is the "Three Star Approach" by UNICEF that encourages schools to take simple, inexpensive steps to ensure that students wash their hands with soap, among other hygienic requirements. When minimum standards are achieved, schools can move from one to ultimately three stars.[85] Building hand washing stations can be a part of hand washing promotion campaigns that are carried out in order to reduce diseases and child mortality.
Global Hand washing Day is another example of an awareness-raising campaign that is trying to achieve behavior change.[86]
As a result of the ongoing COVID-19 pandemic, UNICEF promoted the adoption of a handwashing emoji.[87]
Designing handwashing facilities that encourage use can use the following aspects:[63]
- Nudges, cues and reminders
- Handwashing facilities should be placed at convenient locations to encourage people to use them regularly and at the right times; they should be attractive and well maintained.
Cost effectiveness
Few studies have considered the overall cost effectiveness of hand washing in developing countries in relationship to DALYs averted. However, one review suggests that promoting hand washing with soap is significantly more cost-effective than other water and sanitation interventions.[88]
| Intervention | Costs (US$/DALY) |
|---|---|
| Hand-pump or standpost | 94 |
| House water connection | 223 |
| Water sector regulation | 47 |
| Basic sanitation – construction and promotion | ≤270 |
| Sanitation promotion only | 11.2 |
| Hygiene promotion | 3.4 |
History

The importance of hand washing for human health – particularly for people in vulnerable circumstances like mothers who had just given birth or wounded soldiers in hospitals – was first recognized in the mid 19th century by two pioneers of hand hygiene: the Hungarian physician Ignaz Semmelweis who worked in Vienna, Austria and Florence Nightingale, the English "founder of modern nursing".[89] At that time most people still believed that infections were caused by foul odors called miasmas.
In the 1980s, foodborne outbreaks and healthcare-associated infections led the United States Centers for Disease Control and Prevention to more actively promote hand hygiene as an important way to prevent the spread of infection. The outbreak of swine flu in 2009 and the COVID-19 pandemic in 2020 led to increased awareness in many countries of the importance of washing hands with soap to protect oneself from such infectious diseases.[10] For example, posters with "correct hand washing techniques" were hung up next to hand washing sinks in public toilets and in the toilets of office buildings and airports in Germany.
Society and culture
Moral aspects
The phrase "washing one's hands of" something, means declaring one's unwillingness to take responsibility for the thing or share complicity in it. It originates from the bible passage in Matthew where Pontius Pilate washed his hands of the decision to crucify Jesus Christ, but has become a phrase with a much wider usage in some English communities.
In Shakespeare's Macbeth, Lady Macbeth begins to compulsively wash her hands in an attempt to cleanse an imagined stain, representing her guilty conscience regarding crimes she had committed and induced her husband to commit.
It has also been found that people, after having recalled or contemplated unethical acts, tend to wash hands more often than others, and tend to value hand washing equipment more. Furthermore, those who are allowed to wash their hands after such a contemplation are less likely to engage in other "cleansing" compensatory actions, such as volunteering.[90][91]
Religion
Religions prescribe hand washing for both hygienic and symbolic purposes.[8]
Symbolic hand washing, using water but no soap to wash hands, is a part of ritual hand washing featured in many religions, including Bahá'í Faith, Hinduism, tevilah and netilat yadayim in Judaism, Lavabo in Christianity, and Wudhu in Islam.[8]
Religions also prescribe hygienic hand washing, especially after certain actions. Hinduism, Judaism and Islam mandate washing of hands after using the toilet. And, Hinduism, Buddhism, Sikhism, Judaism and Islam mandate washing of hands before and after every meal.[8]
See also
- Antibiotic resistance
- Food safety
- Global Handwashing Day
- Nosocomial infection
- Occupational biosafety
- Public health
- Patient safety
- Rubbing alcohol
- Didier Pittet, an infectious diseases expert
References
- "Show Me the Science – How to Wash Your Hands". www.cdc.gov. 4 March 2020. Retrieved 6 March 2020.
- Huang, Cunrui; Ma, Wenjun; Stack, Susan (1 August 2012). "The Hygienic Efficacy of Different Hand-Drying Methods: A Review of the Evidence". Mayo Clinic Proceedings. 87 (8): 791–798. doi:10.1016/j.mayocp.2012.02.019. PMC 3538484. PMID 22656243.
- https://www.youtube.com/watch?v=3PmVJQUCm4E
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020.
- Centers for Disease Control (2 April 2020). "When and How to Wash Your Hands". cdc.gov.
- Paludan-Müller, Asger Sand; Boesen, Kim; Klerings, Irma; Jørgensen, Karsten Juhl; Munkholm, Klaus (28 April 2020). "Hand cleaning with ash for reducing the spread of viral and bacterial infections: a rapid review". Cochrane Database of Systematic Reviews. 4: CD013597. doi:10.1002/14651858.cd013597. ISSN 1465-1858. PMC 7192094. PMID 32343408.
- e Borges, Lizandra Ferreira de Almeida; Silva, BL; Gontijo Filho, PP (2007). "Hand washing: Changes in the skin flora". American Journal of Infection Control. 35 (6): 417–20. doi:10.1016/j.ajic.2006.07.012. PMID 17660014.
- "Religious and cultural aspects of hand hygiene". WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care.
- Cowling, Benjamin J.; et al. (2009). "Facemasks and Hand Hygiene to Prevent Influenza Transmission in Households". Annals of Internal Medicine. 151 (7): 437–46. doi:10.7326/0003-4819-151-7-200910060-00142. PMID 19652172.
- "Getting your workplace ready for COVID-19" (PDF). World Health Organization. 27 February 2020. Retrieved 27 March 2020.
- Luby, Stephen P.; Agboatwalla, Mubina; Painter, John; Altaf, Arshad; Billhimer, Ward; Keswick, Bruce; Hoekstra, Robert M. (2006). "Combining drinking water treatment and hand washing for diarrhoea prevention, a cluster randomized controlled trial". Tropical Medicine & International Health. 11 (4): 479–89. doi:10.1111/j.1365-3156.2006.01592.x. PMID 16553931.
- Scott, Beth; et al. "Protecting Children from Diarrhoea and Acute Respiratory Infections: The Role of Hand Washing Promotion in Water and Sanitation Programmes" (PDF). Archived from the original (PDF) on 28 June 2009. Retrieved 21 May 2009.
- Rhee, V.; Mullany, L. C.; Khatry, S. K.; Katz, J.; Leclerq, S. C.; Darmstadt, G. L.; Tielsch, J. M. (2008). "Impact of Maternal and Birth Attendant Hand-washing on Neonatal Mortality in Southern Nepal". Arch Pediatr Adolesc Med. 162 (7): 603–08. doi:10.1001/archpedi.162.7.603. PMC 2587156. PMID 18606930.
- Dangour, Alan D (1996). "Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children" (PDF). Reviews (8): CD009382. doi:10.1002/14651858.CD009382.pub2. PMID 23904195.
- Curtis, Val; Cairncross, Sandy (May 2003). "Effect of washing hands with soap on diarrhoea risk in the community: a systematic review". The Lancet Infectious Diseases. 3 (5): 275–81. doi:10.1016/S1473-3099(03)00606-6. PMID 12726975.
- Ejemot, Regina I; Ehiri, John E; Meremikwu, Martin M; Critchley, Julia A (2009). "Cochrane review: Hand washing for preventing diarrhoea". Evidence-Based Child Health: A Cochrane Review Journal. 4 (2): 893–939. doi:10.1002/ebch.373. ISSN 1557-6272.
- Cairncross, S.; Hunt, C.; Boisson, S.; Bostoen, K.; Curtis, V.; Fung, I. C.; Schmidt, W. P. (2010). "Water, sanitation and hygiene for the prevention of diarrhoea". International Journal of Epidemiology. 39 (Supplement 1): i193–i205. doi:10.1093/ije/dyq035. ISSN 0300-5771. PMC 2845874. PMID 20348121.
- The State of the World’s Children 2008. Child Survival. UNICEF
- "Impetigo". NHS. Retrieved 11 March 2020.
- "Too-Clean Hands Can Lead to Eczema". EverydayHealth.com. Retrieved 24 January 2020.
- "UNICEF Malawi". www.unicef.org. Retrieved 5 January 2020.
- "When and How to Wash Your Hands | Handwashing | CDC". www.cdc.gov. 4 December 2019. Retrieved 7 March 2020.
- "The right way to wash your hands". Mayo Clinic. Retrieved 7 March 2020.
- "JMP handwashing dataset". Archived from the original on 2 April 2016. Retrieved 20 March 2017.
WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation
- BreakingWeb. "Les Français et le savonnage des mains après être allé aux toilettes". BVA Group (in French). Retrieved 9 February 2020.
- Abdi & Gautam, R. & O.P, Approaches to promoting behaviour-change around handwashing-with-soap Archived 21 March 2017 at the Wayback Machine
- UNICEF, GIZ (2016). Scaling up group handwashing in schools – Compendium of group washing facilities across the globe. New York; Eschborn, Germany
- UNICEF (2012) Raising Even More Clean Hands: Advancing Health, Learning and Equity through WASH in Schools, Joint Call to Action
- School Community Manual – Indonesia (formerly Manual for teachers), Fit for School. GIZ Fit for School, Philippines. 2014. ISBN 978-3-95645-250-5.
- "DOUBLE HAND WASHING WITH A FINGERNAIL BRUSH HACCP – HITM: food science safety and HACCP training and certification provider". 2 July 2019. Archived from the original on 2 July 2019. Retrieved 8 April 2020.
- McBride ME (August 1984). "Microbial flora of in-use soap products". Appl. Environ. Microbiol. 48 (2): 338–41. doi:10.1128/AEM.48.2.338-341.1984. PMC 241514. PMID 6486782.
- Heinze, JE; Yackovich, F (1988). "Washing with contaminated bar soap is unlikely to transfer bacteria". Epidemiology and Infection. 101 (1): 135–42. doi:10.1017/s0950268800029290. PMC 2249330. PMID 3402545.
- "Infection Control: Frequently Asked Questions – Hand Hygiene". Centers for Disease Control and Prevention. Retrieved 30 September 2016.
- Weber DJ, Rutala WA (2006). "Use of germicides in the home and the healthcare setting: is there a relationship between germicide use and antibiotic resistance?". Infect Control Hosp Epidemiol. 27 (10): 1107–19. doi:10.1086/507964. PMID 17006819.
- US5942478A, "Microbicidal and sanitizing soap compositions", issued 1997-09-04
- "Plain soap as effective as antibacterial but without the risk". Retrieved 17 August 2007.
- MONTVILLE, REBECCA; SCHAFFNER, DONALD W. (1 November 2011). "A Meta-Analysis of the Published Literature on the Effectiveness of Antimicrobial Soaps". Journal of Food Protection. 74 (11): 1875–1882. doi:10.4315/0362-028X.JFP-11-122. PMID 22054188.
- "Antibacterial Soap Has Poor Killing Power". Scientific American. 24 September 2015. Retrieved 14 April 2020.
- World Health Organization. "WHO Guidelines on Hand Hygiene in Health Care (Advanced Draft)" (PDF). Retrieved 21 July 2008.
- Michaels, B.; Gangar, V.; Schultz, A.; Arenas, M.; Curiale, M.; Ayers, T.; Paulson, D. (2002). "Water temperature as a factor in handwashing efficacy". Food Service Technology. 2 (3): 139–49. doi:10.1046/j.1471-5740.2002.00043.x.
- Laestadius JG, Dimberg L (April 2005). "Hot water for handwashing – where is the proof?". J. Occup. Environ. Med. 47 (4): 434–35. doi:10.1097/01.jom.0000158737.06755.15. PMID 15824636.
- Menegueti, Mayra Gonçalves; Laus, Ana Maria; Ciol, Márcia Aparecida; Auxiliadora-Martins, Maria; Basile-Filho, Anibal; Gir, Elucir; Pires, Daniela; Pittet, Didier; Bellissimo-Rodrigues, Fernando (24 June 2019). "Glycerol content within the WHO ethanol-based handrub formulation: balancing tolerability with antimicrobial efficacy". Antimicrobial Resistance & Infection Control. 8 (1): 109. doi:10.1186/s13756-019-0553-z. ISSN 2047-2994. PMC 6591802. PMID 31285821.
- Information, National Center for Biotechnology (2009). WHO-recommended handrub formulations. World Health Organization.
- Larson, E. L.; Cohen, B.; Baxter, K. A. (2012). "Analysis of alcohol-based hand sanitizer delivery systems: Efficacy of foam, gel, and wipes against influenza A (H1N1) virus on hands". American Journal of Infection Control. 40 (9): 806–09. doi:10.1016/j.ajic.2011.10.016. PMID 22325728.
- Rotter M. (1999). "Hand washing and hand disinfection". Hospital Epidemiology and Infection Control. 87.
- "Preventing Norovirus Infection". www.cdc.gov. 9 March 2018. Retrieved 17 May 2018.
- Munn, Zachary; Tufanaru, Catalin; Lockwood, Craig; Stern, Cindy; McAneney, Helen; Barker, Timothy H. (9 April 2020). "Rinse-free hand wash for reducing absenteeism among preschool and school children". The Cochrane Database of Systematic Reviews. 4: CD012566. doi:10.1002/14651858.CD012566.pub2. ISSN 1469-493X. PMC 7141998. PMID 32270476.
- Nina A. Gold; Usha Avva. "Alcohol Sanitizer". StatPearls Publishing via National Center for Biotechnology Information, U.S. National Library of Medicine. Retrieved 12 March 2020.
- "Handwashing: Clean Hands Save Lives". Center for Disease Control and Prevention. 16 March 2020. Retrieved 26 July 2012.
- Hibbard JS (2005). "Analyses comparing the antimicrobial activity and safety of current antiseptic agents: a review". J Infus Nurs. 28 (3): 194–207. doi:10.1097/00129804-200505000-00008. PMID 15912075.
- Garcia R, Hibbard JS. Antimicrobial activity of a recently approved chlorhexidine isopropyl alcohol antiseptic vs. 70% isopropyl alcohol: a randomized, blind trial. An verbal presentation at the 28th Annual Educational Conference and International Meeting of the Association for Professionals in Infection Control and Epidemiology, 12 June 2001.
- Dyer DL, Gerenraich KB, Wadhams PS (August 1998). "Testing a new alcohol-free hand sanitizer to combat infection". AORN J. 68 (2): 239–41, 243–44, 247–51. doi:10.1016/S0001-2092(06)62517-9. PMID 9706236.
- Butz AM, Laughon BE, Gullette DL, Larson EL (April 1990). "Alcohol-impregnated wipes as an alternative in hand hygiene". American Journal of Infection Control. 18 (2): 70–76. doi:10.1016/0196-6553(90)90084-6. PMID 2337257.
- When and How to Wash Your Hands | Handwashing | CDC
- "Water Sanitation Health. How can personal hygiene be maintained in difficult circumstances?". WHO. 2014. Retrieved 12 March 2020.
- Blomfield S F and Nath K J 2009: Use of ash and mud for handwashing in low income communities. The International Scientific Forum on Home Hygiene Accessed Oct. 2014 http://www.ifh-homehygiene.org/best-practice-review/use-ash-and-mud-handwashing-low-income-communities
- Howard et al. 2002: Healthy Villages A guide for communities and community health workers; Chapter 8 Personal, domestic and community hygiene. WHO. Accessed Oct. 2014. http://www.who.int/water_sanitation_health/hygiene/settings/hvchap8.pdf
- "When and How to Wash Your Hands". www.cdc.gov. 4 December 2019. Retrieved 6 March 2020.
- Wilkinson, Judith M., and Leslie A. Treas.Fundamentals of nursing. 2nd ed. Philadelphia: F.A. Davis Co., 2011. Print
- "The Hygiene Improvement Project (HIP) – Tippy-Tap: A simple low-cost technology for handwashing when water is scarce". USAID. Archived from the original on 25 October 2014. Retrieved 30 September 2015.
- Morgan, P. (2011). Hand washing devices – How to make and use. Aquamor Pvt Ltd., Zimbabwe
- Rao, Ankita (11 September 2014). "When Low-Tech Solutions Win". Slate. ISSN 1091-2339.
- Coultas, M. and Iyer, R. with Myers, J. (2020). Handwashing Compendium for Low Resource Settings: A Living Document. Edition 1, The Sanitation Learning Hub, Brighton: IDS, ISBN 978-1-78118-638-1 (alternative URL)
- A comparative study of three different hand drying methods: paper towel, warm air dryer, jet air dryer’ by Keith Redway and Shameem Fawdar of the School of Biosciences, University of Westminster London
- Davis, Rebecca (2015). "The Doctor Who Championed Hand-Washing And Briefly Saved Lives". NPR.
- Boyce, JM (October 2011). "Measuring healthcare worker hand hygiene activity: current practices and emerging technologies". Infection Control and Hospital Epidemiology. 32 (10): 1016–28. doi:10.1086/662015. PMID 21931253.
- Swoboda, SM; Earsing, K; Strauss, K; Lane, S; Lipsett, PA (February 2004). "Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit". Critical Care Medicine. 32 (2): 358–63. doi:10.1097/01.CCM.0000108866.48795.0F. PMID 14758148.
- Larson EL (August 1995). "APIC guideline for handwashing and hand antisepsis in health care settings". Am J Infect Control. 23 (4): 251–69. doi:10.1016/0196-6553(95)90070-5. PMID 7503437.
- World Health Organization. "Surgical Handrubbing Technique" (PDF). Cite journal requires
|journal=(help) - Goldmann D (2006). "System failure versus personal accountability – the case for clean hands". N. Engl. J. Med. 355 (2): 121–23. doi:10.1056/NEJMp068118. PMID 16837675.
- Pronovost P; Needham D; Berenholtz S; et al. (2006). "An intervention to decrease catheter-related bloodstream infections in the ICU". N. Engl. J. Med. 355 (26): 2725–32. doi:10.1056/NEJMoa061115. PMID 17192537.
- World Health Organization. "How to Handrub & How to Handwash" (PDF). Retrieved 21 July 2008.
- Whitby, M.; Pessoa-Silva, CL; McLaws, ML; Allegranzi, B; Sax, H; Larson, E; Seto, WH; Donaldson, L; Pittet, D (2007). "Behavioural considerations for hand hygiene practices: the basic building blocks". Journal of Hospital Infection. 65 (1): 1–8. doi:10.1016/j.jhin.2006.09.026. PMID 17145101.
- WHO Guidelines on Hand Hygiene in Health Care
- Beggs CB, Shepherd SJ, Kerr KG (2008). "Increasing the frequency of hand washing by healthcare workers does not lead to commensurate reductions in staphylococcal infection in a hospital ward". BMC Infectious Diseases. 8: 114. doi:10.1186/1471-2334-8-114. PMC 2553083. PMID 18764942.
- Fischler GE, Fuls JL, Dail EW, Duran MH, Rodgers ND, Waggoner AL (2007). "Effect of hand wash agents on controlling the transmission of pathogenic bacteria from hands to food". Journal of Food Protection. 70 (12): 2873–77. doi:10.4315/0362-028X-70.12.2873. PMID 18095447.
- Girou E, Loyeau S, Legrand P, Oppein F, Brun-Buisson C (2002). "Efficacy of handrubbing with alcohol based solution versus standard handwashing with antiseptic soap: randomised clinical trial". BMJ (Clinical Research Ed.). 325 (7360): 362. doi:10.1136/bmj.325.7360.362. PMC 117885. PMID 12183307.
- Grayson ML, Melvani S, Druce J, Barr IG, Ballard SA, Johnson PD, Mastorakos T, Birch C (2009). "Efficacy of soap and water and alcohol-based hand-rub preparations against live H1N1 influenza virus on the hands of human volunteers". Clinical Infectious Diseases. 48 (3): 285–91. doi:10.1086/595845. PMID 19115974.
- Jabbar U, Leischner J, Kasper D, Gerber R, Sambol SP, Parada JP, Johnson S, Gerding DN (2010). "Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands". Infection Control and Hospital Epidemiology. 31 (6): 565–70. doi:10.1086/652772. PMID 20429659.
- Gould, Dinah J.; Moralejo, Donna; Drey, Nicholas; Chudleigh, Jane H.; Taljaard, Monica (2017). "Interventions to improve hand hygiene compliance in patient care". The Cochrane Database of Systematic Reviews. 9: CD005186. doi:10.1002/14651858.CD005186.pub4. ISSN 1469-493X. PMC 6483670. PMID 28862335.
- Ritchie, Roser, Mispy, Ortiz-Ospina (2018) "Measuring progress towards the Sustainable Development Goals." (SDG 6) SDG-Tracker.org, website
- Curtis, V., Scott, B., Cardosi, J. (2000). The Handwashing Handbook – A guide for developing a hygiene promotion program to increase handwashing with soap. The International Bank for Reconstruction and Development/The World Bank
- Vujcic, J., Ram, P.K. (2013). UNICEF Handwashing Promotion – Monitoring and Evaluation Module. UNICEF, New York
- De Buck, Emmy; Van Remoortel, Hans; Hannes, Karin; Govender, Thashlin; Naidoo, Selvan; Avau, Bert; Veegaete, Axel Vande; Musekiwa, Alfred; Lutje, Vittoria; Cargo, Margaret; Mosler, Hans‐Joachim (19 May 2017). "Approaches to promote handwashing and sanitation behaviour change in low‐ and middle‐income countries: a mixed method systematic review". Campbell Systematic Reviews. 13 (1): 1–447. doi:10.4073/csr.2017.7. ISSN 1891-1803.
- UNICEF, GIZ (2013). Field Guide: The Three Star Approach for WASH in Schools. United Nations Children's Fund and Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ), Eschborn, Germany
- PPPHW (2014). Global Handwashing Day Planner's Guide, 3rd edition, prepared by FHI 360 for the Global Public-Private Partnership for Handwashing with Soap
- "What about a handwashing emoji??!". www.unicef.org. Retrieved 13 March 2020.
- Cairncross, S; Valdmanis, V (2006). "41: Water Supply, Sanitation, and Hygiene Promotion" (PDF). In Jamison, D.T.; Breman, J.G.; Measham, A.R.; et al. (eds.). Disease Control Priorities in Developing Countries (Second ed.). World Bank Group. pp. 771–92. doi:10.1596/978-0-8213-6179-5. ISBN 978-0-8213-6179-5.
- "The Global Public-Private Partnership for Handwashing". globalhandwashing.org. Retrieved 18 April 2015.
- Benedict Carey (12 September 2006). "Lady Macbeth Not Alone in Her Quest for Spotlessness". The New York Times.
- Zhong CB, Liljenquist K (2006). "Washing away your sins: threatened morality and physical cleansing". Science. 313 (5792): 1451–52. Bibcode:2006Sci...313.1451Z. CiteSeerX 10.1.1.181.571. doi:10.1126/science.1130726. PMID 16960010.
Schnall S, Benton J, Harvey S (2005). "Clean Conscience: Cleanliness Reduces the Severity of Moral Judgments". Psychological Science. 16 (10): 780–84. doi:10.1111/j.1467-9280.2005.01614.x. PMID 16181440.
Sources
- Carrico, Amanda R.; Spoden, Micajah (1 July 2013). "The Environmental Cost of Misinformation: Why the Recommendation to Use Elevated Temperatures for Handwashing is Problematic". International Journal of Consumer Studies. 37 (4): 433–441. doi:10.1111/ijcs.12012. PMC 3692566. PMID 23814480.
Further reading
- Miryam Z. Wahrman (2016). The Hand Book: Surviving in a Germ-Filled World. ForeEdge. ISBN 978-1611689174.
External links
- Hand Hygiene: Why, How & When? (PDF from the World Health Organization)




- Centers for Disease Control on hand hygiene in healthcare settings
- Global Public-Private Partnership for Hand washing
- Photos of low-cost hand washing installations in developing countries (collected by Sustainable Sanitation Alliance)
- OCD and Hand Washing
- WHO: How to handwash with soap and water (video)