Body dysmorphic disorder
Body dysmorphic disorder (BDD), occasionally still called dysmorphophobia, is a mental disorder characterized by the obsessive idea that some aspect of one's own body part or appearance is severely flawed and therefore warrants exceptional measures to hide or fix it.[1] In BDD's delusional variant, the flaw is imagined.[2] If the flaw is actual, its importance is severely exaggerated.[2] Either way, thoughts about it are pervasive and intrusive, and may occupy several hours a day, causing severe distress and impairing one’s otherwise normal activities. The DSM-5 categorizes BDD in the obsessive–compulsive spectrum, and distinguishes it from anorexia nervosa.
| Body dysmorphic disorder | |
|---|---|
| Other names | Body dysmorphia, dysmorphic syndrome, dysmorphophobia |
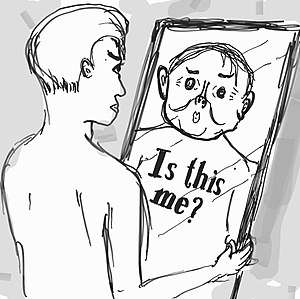 | |
| A cartoon of a patient with body dysmorphia looking in a mirror, seeing a distorted image of himself | |
| Specialty | Psychiatry, clinical psychology |
BDD is estimated to affect from 0.7% to 2.4% of the population.[2] It usually starts during adolescence and affects both men and women.[2][3] The BDD subtype muscle dysmorphia, perceiving the body as too small, affects mostly males.[4] Besides thinking about it, one repetitively checks and compares the perceived flaw, and can adopt unusual routines to avoid social contact that exposes it.[2] Fearing the stigma of vanity, one usually hides the preoccupation.[2] Commonly unsuspected even by psychiatrists, BDD has been underdiagnosed.[2] Severely impairing quality of life via educational and occupational dysfunction and social isolation, BDD has high rates of suicidal thoughts and suicide attempts.[2]
Signs and symptoms
Whereas vanity involves a quest to aggrandize the appearance, BDD is experienced as a quest to merely normalize the appearance.[2] Although delusional in about one of three cases, the appearance concern is usually nondelusional, an overvalued idea.[3]
The bodily area of focus can be nearly any, yet is commonly face, hair, stomach, thighs, or hips.[5] Some half dozen areas can be a roughly simultaneous focus.[2] Many seek dermatological treatment or cosmetic surgery, which typically do not resolve the distress.[2] On the other hand, attempts at self-treatment, as by skin picking, can create lesions where none previously existed.[2]
BDD shares features with obsessive-compulsive disorder,[6] but involves more depression and social avoidance.[1] BDD often associates with social anxiety disorder.[7] Some experience delusions that others are covertly pointing out their flaws.[2] Cognitive testing and neuroimaging suggest both a bias toward detailed visual analysis and a tendency toward emotional hyper-arousal.[8]
Most generally, one experiencing BDD ruminates over the perceived bodily defect several hours daily or longer, uses either social avoidance or camouflaging with cosmetics or apparel, repetitively checks the appearance, compares it to that of other people, and might often seek verbal reassurances.[1][2] One might sometimes avoid mirrors, repetitively change outfits, groom excessively, or restrict eating.[5]
BDD's severity can wax and wane, and flareups tend to yield absences from school, work, or socializing, sometimes leading to protracted social isolation, with some becoming housebound for extended periods.[2] Social impairment is usually greatest, sometimes approaching avoidance of all social activities.[5] Poor concentration and motivation impair academic and occupational performance.[5] The distress of BDD tends to exceed that of either major depressive disorder or type-2 diabetes, and rates of suicidal ideation and attempts are especially high.[2]
Causal factors
As with most mental disorders, BDD's cause is likely intricate, altogether biopsychosocial, through an interaction of multiple factors, including genetic, developmental, psychological, social, and cultural.[9][10] BDD usually develops during early adolescence,[5] although many patients note earlier trauma, abuse, neglect, teasing, or bullying.[11] In many cases, social anxiety earlier in life precedes BDD. Though twin studies on BDD are few, one estimated its heritability at 43%.[12] Yet other factors may be introversion,[13] negative body image, perfectionism,[9][14] heightened aesthetic sensitivity,[10] and childhood abuse and neglect.[10][15]
Diagnosis
Estimates of prevalence and gender distribution have varied widely via discrepancies in diagnosis and reporting.[1] In American psychiatry, BDD gained diagnostic criteria in the DSM-IV, but clinicians' knowledge of it, especially among general practitioners, is constricted.[16] Meanwhile, shame about having the bodily concern, and fear of the stigma of vanity, makes many hide even having the concern.[2][17]
Via shared symptoms, BDD is commonly misdiagnosed as social anxiety disorder, obsessive-compulsive disorder, major depressive disorder, or social phobia.[18][19] Correct diagnosis can depend on specialized questioning and correlation with emotional distress or social dysfunction.[20] Estimates place the Body Dysmorphic Disorder Questionnaire's sensitivity at 100% (0% false negatives) and specificity at 92.5% (7.5% false positives).[21]
Treatment
Anti-depressant medication, such as selective serotonin reuptake inhibitors (SSRIs), and cognitive-behavioral therapy (CBT) are considered effective.[5][22][23] SSRIs can help relieve obsessive-compulsive and delusional traits, while cognitive-behavioral therapy can help patients recognize faulty thought patterns.[5] Before treatment, it can help to provide psychoeducation, as with self-help books and support websites.[5]
History
In 1886, Enrico Morselli reported a disorder that he termed dysmorphophobia.[24] In 1980, the American Psychiatric Association recognized the disorder, while categorizing it as an atypical somatoform disorder, in the third edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM).[3] Classifying it as a distinct somatoform disorder, the DSM-III's 1987 revision switched the term to body dysmorphic disorder.[3]
Published in 1994, DSM-IV defines BDD as a preoccupation with an imagined or trivial defect in appearance, a preoccupation causing social or occupational dysfunction, and not better explained as another disorder, such as anorexia nervosa.[3][25] Published in 2013, the DSM-5 shifts BDD to a new category (obsessive–compulsive spectrum), adds operational criteria (such as repetitive behaviors or intrusive thoughts), and notes the subtype muscle dysmorphia (preoccupation that one's body is too small or insufficiently muscular or lean).
References
- Cororve, Michelle; Gleaves, David (August 2001). "Body dysmorphic disorder: A review of conceptualizations, assessment, and treatment strategies". Clinical Psychology Review. 21 (6): 949–970. doi:10.1016/s0272-7358(00)00075-1. PMID 11497214.
- Bjornsson AS; Didie ER; Phillips KA (2010). "Body dysmorphic disorder". Dialogues Clin Neurosci. 12 (2): 221–32. PMC 3181960. PMID 20623926.
- Mufaddel Amir, Osman Ossama T, Almugaddam Fadwa, Jafferany Mohammad (2013). "A review of body dysmorphic disorder and Its presentation in different clinical settings". Primary Care Companion for CNS Disorders. 15 (4). doi:10.4088/PCC.12r01464. PMC 3869603. PMID 24392251.CS1 maint: multiple names: authors list (link)
- Katharine A Phillips, Understanding Body Dysmorphic Disorder: An Essential Guide (New York: Oxford University Press, 2009), pp 50–51.
- Katharine A Phillips, "Body dysmorphic disorder: Recognizing and treating imagined ugliness", World Psychiatry, 2004 Feb;3(1):12-7.
- Fornaro M, Gabrielli F, Albano C, et al. (2009). "Obsessive-compulsive disorder and related disorders: A comprehensive survey". Annals of General Psychiatry. 8: 13. doi:10.1186/1744-859X-8-13. PMC 2686696. PMID 19450269.
- Fang Angela; Hofmann Stefan G (Dec 2010). "Relationship between social anxiety disorder and body dysmorphic disorder". Clinical Psychology Review. 30 (8): 1040–1048. doi:10.1016/j.cpr.2010.08.001. PMC 2952668. PMID 20817336.
- Buchanan Ben G, Rossell Susan L, Castle David J (Feb 2011). "Body dysmorphic disorder: A review of nosology, cognition and neurobiology". Neuropsychiatry. 1 (1): 71–80. doi:10.2217/npy.10.3.
- Katharine A Phillips, Understanding Body Dysmorphic Disorder: An Essential Guide (New York: Oxford University Press, 2009), ch 9.
- Feusner, J.D.; Neziroglu, F; Wilhelm, S.; Mancusi, L.; Bohon, C. (2010). "What causes BDD: Research findings and a proposed model". Psychiatric Annals. 40 (7): 349–355. doi:10.3928/00485713-20100701-08. PMC 3859614. PMID 24347738.
- Brody, Jane E. (2010-03-22). "When your looks take over your life". The New York Times. Retrieved 13 March 2017.
- Browne, Heidi A.; Gair, Shannon L.; Scharf, Jeremiah M.; Grice, Dorothy E. (2014-01-01). "Genetics of obsessive-Compulsive Disorder and Related Disorders". Psychiatric Clinics of North America. 37 (3): 319–335. doi:10.1016/j.psc.2014.06.002. PMC 4143777. PMID 25150565.
- Veale D (2004). "Body dysmorphic disorder". British Medical Journal. 80 (940): 67–71. doi:10.1136/pmj.2003.015289. PMC 1742928. PMID 14970291.
- Hartmann, A (2014). "A comparison of self-esteem and perfectionism in anorexia nervosa and body dysmorphic disorder". Journal of Nervous and Mental Disease. 202 (12): 883–888. doi:10.1097/nmd.0000000000000215. PMID 25390930.
- Didie E, Tortolani C, Pope C, Menard W, Fay C, Phillips K (2006). "Childhood abuse and neglect in body dysmorphic disorder". Child Abuse and Neglect. 30 (10): 1105–1115. doi:10.1016/j.chiabu.2006.03.007. PMC 1633716. PMID 17005251.
- Katharine A Phillips. The Broken Mirror. Oxford University Press, 1996. p. 39.
- Prazeres AM, Nascimento AL, Fontenelle LF (2013). "Cognitive-behavioral therapy for body dysmorphic disorder: A review of its efficacy". Neuropsychiatric Disease and Treatment. 9: 307–16. doi:10.2147/NDT.S41074. PMC 3589080. PMID 23467711.
- "Body Dysmorphic Disorder". Anxiety and Depression Association of America. Anxiety and Depression Association of America. Retrieved 2 January 2019.
- Katharine A Phillips. The Broken Mirror. Oxford University Press, 1996. p. 47.
- Phillips, Katherine; Castle, David (November 3, 2001). "British Medical Journal". BMJ. 323 (7320): 1015–1016. doi:10.1136/bmj.323.7320.1015. PMC 1121529. PMID 11691744.
- Grant, Jon; Won Kim, Suck; Crow, Scott (2001). "Prevalence and Clinical Features of Body Dysmorphic Disorder in Adolescent and Adult Psychiatric Inpatients". J Clin Psychiatry. 62 (7): 517–522. doi:10.4088/jcp.v62n07a03. PMID 11488361.
- Harrison, A.; Fernández de la Cruz, L.; Enander, J.; Radua, J.; Mataix-Cols, D. (2016). "Cognitive-behavioral therapy for body dysmorphic disorder: A systematic review and meta-analysis of randomized controlled trials". Clinical Psychology Review. 48: 43–51. doi:10.1016/j.cpr.2016.05.007. PMID 27393916.
- Jc, Ipser; C, Sander; Dj, Stein (2009-01-21). "Pharmacotherapy and Psychotherapy for Body Dysmorphic Disorder". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD005332.pub2. PMC 7159283. PMID 19160252.
- Hunt TJ; Thienhaus O; Ellwood A (July 2008). "The mirror lies: Body dysmorphic disorder". American Family Physician. 78 (2): 217–22. PMID 18697504.
- Diagnostic and Statistical Manual of Mental Disorders (Fourth text revision ed.). American Psychiatric Association, Washington DC. 2000. pp. 507–10.
External links
| Classification | |
|---|---|
| External resources |