Bipolar I disorder
Bipolar I disorder (BD-I; pronounced "type one bipolar disorder") is a type of bipolar spectrum disorder characterized by the occurrence of at least one manic episode, with or without mixed or psychotic features.[1] Most people also, at other times, have one or more depressive episodes, and all experience a hypomanic stage before progressing to full mania.[2]
| Bipolar disorder | |
|---|---|
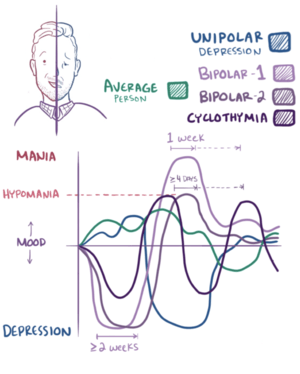 | |
| Graphical representation of Bipolar I, Bipolar II and cyclothymia | |
| Specialty | Psychiatry |
It is a type of bipolar disorder, and conforms to the classic concept of manic-depressive illness, which can include psychosis during mood episodes.[3]
Diagnosis
The essential feature of bipolar I disorder is a clinical course characterized by the occurrence of one or more manic episodes or mixed episodes (DSM-IV-TR, 2000). Often, individuals have had one or more major depressive episodes.[4] One episode of mania is sufficient to make the diagnosis of bipolar disorder; the person may or may not have a history of major depressive disorder.[4] Episodes of substance-induced mood disorder due to the direct effects of a medication, or other somatic treatments for depression, drug abuse, or toxin exposure, or of mood disorder due to a general medical condition need to be excluded before a diagnosis of bipolar I disorder can be made. Bipolar I disorder requires confirmation of only 1 full manic episode for diagnosis, but may be associated with hypomanic and depressive episodes as well.[5] Diagnosis for bipolar II disorder does not include a full manic episode; instead, it requires the occurrence of both a hypomanic episode and a major depressive episode.[5] Bipolar I disorder (and bipolar II disorder) is often comorbid with other disorders including PTSD, substance use disorders and a variety of mood disorders.[6][7] Up to 40% of people with bipolar disorder also present with PTSD, with higher rates occurring in women and individuals with bipolar I disorder.[6] In addition, the episodes must not be better accounted for by schizoaffective disorder or superimposed on schizophrenia, schizophreniform disorder, delusional disorder, or a psychotic disorder not otherwise specified.[8]
Medical assessment
Regular medical assessments are performed to rule-out secondary causes of mania and depression.[9] These tests include complete blood count, glucose, serum chemistry/electrolyte panel, thyroid function test, liver function test, renal function test, urinalysis, vitamin B12 and folate levels, HIV screening, syphilis screening, and pregnancy test, and when clinically indicated, an electrocardiogram (ECG), an electroencephalogram (EEG), a computed tomography (CT scan), and/or a magnetic resonance imagining (MRI) may be ordered.[9] Drug screening includes recreational drugs, particularly synthetic cannabinoids, and exposure to toxins.
DSM-IV-TR
| Dx Code # | Disorder | Description |
|---|---|---|
| 296.0x | Bipolar I disorder | Single manic episode |
| 296.40 | Bipolar I disorder | Most recent episode hypomanic |
| 296.4x | Bipolar I disorder | Most recent episode manic |
| 296.5x | Bipolar I disorder | Most recent episode depressed |
| 296.6x | Bipolar I disorder | Most recent episode mixed |
| 296.7 | Bipolar I disorder | Most recent episode unspecified |
DSM-5
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) was released in May 2013. There are several proposed revisions to occur in the diagnostic criteria of Bipolar I Disorder and its subtypes. For Bipolar I Disorder 296.40 (most recent episode hypomanic) and 296.4x (most recent episode manic), the proposed revision includes the following specifiers: with psychotic features, with mixed features, with catatonic features, with rapid cycling, with anxiety (mild to severe), with suicide risk severity, with seasonal pattern, and with postpartum onset.[10] Bipolar I Disorder 296.5x (most recent episode depressed) will include all of the above specifiers plus the following: with melancholic features and with atypical features.[10] The categories for specifiers will be removed in DSM-5 and criterion A will add or there are at least 3 symptoms of major depression of which one of the symptoms is depressed mood or anhedonia.[10] For Bipolar I Disorder 296.7 (most recent episode unspecified), the listed specifiers will be removed.[10]
The criteria for manic and hypomanic episodes in criteria A & B will be edited. Criterion A will include “and present most of the day, nearly every day,” and criterion B will include “and represent a noticeable change from usual behavior.” These criteria as defined in the DSM-IV-TR have created confusion for clinicians and need to be more clearly defined.[11][12]
There have also been proposed revisions to criterion B of the diagnostic criteria for a Hypomanic Episode, which is used to diagnose For Bipolar I Disorder 296.40, Most Recent Episode Hypomanic. Criterion B lists "inflated self-esteem, flight of ideas, distractibility, and decreased need for sleep" as symptoms of a Hypomanic Episode. This has been confusing in the field of child psychiatry because these symptoms closely overlap with symptoms of attention deficit hyperactivity disorder (ADHD).[11]
Note that many of the above changes are still under active consideration and are not definite. For more information regarding proposed revisions to the DSM-5, please visit their website at dsm5.org.
ICD-10
- F31 Bipolar Affective Disorder
- F31.6 Bipolar Affective Disorder, Current Episode Mixed
- F30 Manic Episode
- F30.0 Hypomania
- F30.1 Mania Without Psychotic Symptoms
- F30.2 Mania With Psychotic Symptoms
- F32 Depressive Episode
- F32.0 Mild Depressive Episode
- F32.1 Moderate Depressive Episode
- F32.2 Severe Depressive Episode Without Psychotic Symptoms
- F32.3 Severe Depressive Episode With Psychotic Symptoms
Treatment
Medication
Mood stabilizers are often used as part of the treatment process.[13]
- Lithium is the mainstay in the management of bipolar disorder but it has a narrow therapeutic range and typically requires monitoring[14]
- Anticonvulsants, such as valproate,[15] carbamazepine, or lamotrigine
- Atypical antipsychotics, such as quetiapine,[16][17] risperidone, olanzapine, or aripiprazole
- Electroconvulsive therapy, a psychiatric treatment in which seizures are electrically induced in anesthetized patients for therapeutic effect
Antidepressant-induced mania occurs in 20–40% of people with bipolar disorder. Mood stabilizers, especially lithium, may protect against this effect, but some research contradicts this.[18]
Education
Psychosocial interventions can be used for managing acute depressive episodes and for maintenance treatment to aid in relapse prevention.[19] This includes psycho education, cognitive behavioural therapy (CBT), family-focused therapy (FFT), interpersonal and social-rhythm therapy (IPSRT), and peer support.[19]
Information on the condition, importance of regular sleep patterns, routines and eating habits and the importance of compliance with medication as prescribed. Behavior modification through counseling can have positive influence to help reduce the effects of risky behavior during the manic phase. Additionally, the lifetime prevalence for bipolar I disorder is estimated to be 1%.[20]
See also
- Bipolar disorder
- Bipolar disorders research
- Bipolar II disorder
- Bipolar NOS
- Borderline personality disorder
- Creativity and bipolar disorder
- Cyclothymia
- Detailed listing of DSM-IV-TR bipolar disorder diagnostics codes
- Emotional dysregulation
- International Society for Bipolar Disorders
- Kleine–Levin syndrome
- List of people with bipolar disorder
- Oppositional defiance disorder
- Racing thoughts
- Seasonal affective disorder
References
- "The Two Types of Bipolar Disorder". Psych Central.com. Retrieved 25 November 2015.
- "Bipolar Disorder: Who's at Risk?". Retrieved 22 November 2011.
- "What are the types of bipolar disorder?". Retrieved 22 November 2011.
- "Online Bipolar Tests: How Much Can You Trust Them?". DepressionD. Retrieved 7 January 2012.
- Diagnostic and statistical manual of mental disorders : DSM-5. American Psychiatric Association., American Psychiatric Association. DSM-5 Task Force. (Fifth ed.). Arlington, VA. 2013. ISBN 978-0-89042-559-6. OCLC 847226928.CS1 maint: others (link)
- Cerimele, Joseph M.; Bauer, Amy M.; Fortney, John C.; Bauer, Mark S. (May 2017). "Patients With Co-Occurring Bipolar Disorder and Posttraumatic Stress Disorder: A Rapid Review of the Literature". The Journal of Clinical Psychiatry. 78 (5): e506–e514. doi:10.4088/JCP.16r10897. ISSN 1555-2101. PMID 28570791.
- Hunt, Glenn E.; Malhi, Gin S.; Cleary, Michelle; Lai, Harry Man Xiong; Sitharthan, Thiagarajan (December 2016). "Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990-2015: Systematic review and meta-analysis". Journal of Affective Disorders. 206: 331–349. doi:10.1016/j.jad.2016.07.011. ISSN 1573-2517. PMID 27476137.
- "Bipolar Disorder Residential Treatment Center Los Angeles". PCH Treatment. Retrieved 25 November 2015.
- Bobo, William V. (October 2017). "The Diagnosis and Management of Bipolar I and II Disorders: Clinical Practice Update". Mayo Clinic Proceedings. 92 (10): 1532–1551. doi:10.1016/j.mayocp.2017.06.022. ISSN 0025-6196. PMID 28888714.
- American Psychiatric Association (22 May 2013). Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. doi:10.1176/appi.books.9780890425596. ISBN 978-0-89042-555-8.
- Issues pertinent to a developmental approach to bipolar disorder in DSM-5. American Psychiatric Association. 2010.
- Diagnostic and Statistical Manual of Mental Disorders (4th ed. text revision). Washington, DC: American Psychiatric Association. 2000. pp. 345–392.
- Schwartz, Jeremy (20 July 2017). "Can People Recover From Bipolar Disorder?". US News and World Report.
- Burgess, Sally SA; Geddes, John; Hawton, Keith KE; Taylor, Matthew J.; Townsend, Ellen; Jamison, K.; Goodwin, Guy (2001). "Lithium for maintenance treatment of mood disorders | Cochrane". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD003013. PMC 7005360. Retrieved 9 March 2016.
- MacRitchie, Karine; Geddes, John; Scott, Jan; Haslam, D. R.; Silva De Lima, Mauricio; Goodwin, Guy (2003). "Valproate for acutre mood episodes in bipolar disorder | Cochrane". Cochrane Database of Systematic Reviews (1): CD004052. doi:10.1002/14651858.CD004052. PMID 12535506. Retrieved 9 March 2016.
- Datto, Catherine (11 March 2016). "Bipolar II compared with bipolar I disorder: baseline characteristics and treatment response to quetiapine in a pooled analysis of five placebo-controlled clinical trials of acute bipolar depression". Annals of General Psychiatry. 15: 9. doi:10.1186/s12991-016-0096-0. PMC 4788818. PMID 26973704.
- Young, Allan (February 2014). "A Randomised, Placebo-Controlled 52-Week Trial of Continued Quetiapine Treatment in Recently Depressed Patients With Bipolar I And Bipolar II Disorder". World Journal of Biological Psychiatry. 15 (2): 96–112. doi:10.3109/15622975.2012.665177. PMID 22404704.
- Goldberg, Joseph F; Truman, Christine J (1 December 2003). "Antidepressant-induced mania: an overview of current controversies". Bipolar Disorders. 5 (6): 407–420. doi:10.1046/j.1399-5618.2003.00067.x. ISSN 1399-5618. PMID 14636364.
- Yatham, Lakshmi N.; Kennedy, Sidney H.; Parikh, Sagar V.; Schaffer, Ayal; Bond, David J.; Frey, Benicio N.; Sharma, Verinder; Goldstein, Benjamin I.; Rej, Soham; Beaulieu, Serge; Alda, Martin (2018). "Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder". Bipolar Disorders. 20 (2): 97–170. doi:10.1111/bdi.12609. ISSN 1399-5618. PMC 5947163. PMID 29536616.
- Merikangas, Kathleen R.; Akiskal, Hagop S.; Angst, Jules; Greenberg, Paul E.; Hirschfeld, Robert M.A.; Petukhova, Maria; Kessler, Ronald C. (1 May 2007). "Lifetime and 12-Month Prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication". Archives of General Psychiatry. 64 (5): 543–552. doi:10.1001/archpsyc.64.5.543. ISSN 0003-990X. PMC 1931566. PMID 17485606.