Causes of mental disorders
A mental disorder is an impairment of the mind causing disruption in normal thinking, feeling, mood, behavior, or social interactions, and accompanied by significant distress or dysfunction.[1][2][3][4]
The causes of mental disorders are regarded as complex and varying depending on the particular disorder and the individual. Although the causes of most mental disorders are not fully understood, researchers have identified a variety of biological, psychological, and environmental factors that can contribute to the development or progression of mental disorders.[5] Most mental disorders are a result of a combination of several different factors rather than just a single factor.[6]
Research results
Risk factors for mental illness include, psychological trauma, adverse childhood experiences, genetic predisposition[7][8][9] and personality traits.[10][11] Correlations of mental disorders with drug use include almost all psychoactive substances, e.g., cannabis,[12] alcohol[13] and caffeine.[14]
Particular mental illnesses have particular risk factors, for instance including unequal parental treatment, adverse life events and drug use in depression,[12][15] migration and discrimination, childhood trauma, bereavement or separation in families, and cannabis use in schizophrenia and psychosis,[12][16] and parenting factors, child abuse,[17] family history (e.g. of anxiety), and temperament and attitudes (e.g. pessimism) in anxiety.[18] Many psychiatric disorders include problems with impulse and other emotional control.
In February 2013 a study found common genetic links between five major psychiatric disorders: autism, ADHD, bipolar disorder, major depressive disorder, and schizophrenia.[19] Abnormal functioning of neurotransmitter systems has been implicated in several mental disorders, including serotonin, norepinephrine, dopamine and glutamate systems. Differences have also been found in the size or activity of certain brain regions in some cases. Psychological mechanisms have also been implicated, such as cognitive (e.g. reasoning) biases, emotional influences, personality dynamics, temperament and coping style. Studies have indicated that variation in genes can play an important role in the development of mental disorders, although the reliable identification of connections between specific genes and specific categories of disorder has proven more difficult. Environmental events surrounding pregnancy and birth have also been implicated. Traumatic brain injury may increase the risk of developing certain mental disorders. There have been some tentative inconsistent links found to certain viral infections, to substance misuse, and to general physical health.
Social influences have been found to be important, including abuse, neglect, bullying, social stress, traumatic events and other negative or overwhelming life experiences. The specific risks and pathways to particular disorders are less clear, however. Aspects of the wider community have also been implicated, including employment problems, socioeconomic inequality, lack of social cohesion, problems linked to migration, and features of particular societies and cultures.
Theories
General theories
There are a number of theories or models seeking to explain the causes (etiology) of mental disorders. These theories may differ in regards to how they explain the cause of the disorder, how they treat the disorder, and their basic classification of mental disorders. There may also be differences in philosophy of mind regarding whether, or how, the mind is considered separately from the brain.
During most of the 20th century, mental illness was believed to be caused by problematic relationships between children and their parents. This view was held well into the late 1990s, in which people still believed this child-parent relationship was a large determinant of severe mental illness, such as depression and schizophrenia. In the 21st century additional factors have been identified such as genetic contributions, though experience always also plays a role. So, the perceived causes of mental illness have changed over time and will most likely continue to alter while more research is done in this area.[20]
Outside the West, community approaches remain a focus.[21]
Medical or biomedical model
An overall distinction is also commonly made between a "medical model" (also known as a biomedical or disease model) and a "social model" (also known as an empowerment or recovery model) of mental disorder and disability, with the former focusing on hypothesized disease processes and symptoms, and the latter focusing on hypothesized social constructionism and social contexts.[22]
Biological psychiatry has tended to follow a biomedical model focused on organic or "hardware" pathology of the brain,[23] where many mental disorders are conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience.[24]
Biopsychosocial model
The primary model of contemporary mainstream Western psychiatry is the biopsychosocial model (BPS), which merges biological, psychological and social factors.[23] For instance one view is that genetics accounts for 40% of a person's susceptibility to mental disorders while psychological and environmental factors account for the other 60%.[25] It may be commonly neglected or misapplied in practice due to being too broad or relativistic, however.
The most common view [26] is that disorders tend to result from genetic dispositions and environmental stressors, combining to cause patterns of distress or dysfunction or, more sharply, trigger disorders (Diathesis-stress model). A practical mixture of models may often be used to explain particular issues and disorders,[23] although there may be difficulty defining boundaries for indistinct psychiatric syndromes.[27]
Psychoanalytic theories
Psychoanalytic theories focus on unresolved internal and relational conflicts. These theories have been posited as overall explanations of mental disorder, although today most psychoanalytic groups are said to adhere to the biopsychosocial model and to accept an eclectic mix of subtypes of psychoanalysis.[23] The psychoanalytic theory was originated by Sigmund Freud. This theory focuses on the impact of unconscious forces on human behavior. According to Freud, the personality is made up of three parts: the id, ego, and superego. The id operates under the pleasure principle, the ego operates under the reality principle, and the superego is the "conscience" and incorporates what is and is not socially acceptable into a person's value system. Also, according to the psychoanalytic theory, there are five stages of psycho-sexual development that everyone goes through: the oral stage, anal stage, phallic stage, latency stage, and genital stage. Mental disorders can be caused by an individual receiving too little or too much gratification in one of the psycho-sexual developmental stages. When this happens, the individual is said to be fixated in that developmental stage.[28][29]
Attachment theory
Attachment theory is a kind of evolutionary-psychological approach sometimes applied in the context for mental disorders, which focuses on the role of early caregiver-child relationships, responses to danger, and the search for a satisfying reproductive relationship in adulthood.[30] According to this theory, the more secure a child's attachment is to a nurturing adult, the more likely that child will maintain healthy relationships with others in their life. As found by the Strange Situation experiment run by Mary Ainsworth based on the formulations of John Bowlby, there are four main patterns of attachment: secure attachment, avoidant attachment, disorganized attachment and ambivalent attachment. These attachment patterns are found cross-culturally.[31] Later research found a fourth pattern of attachment known as disorganized disoriented attachment. Secure attachments reflect trust in the child-caretaker relationship while insecure attachment reflects mistrust. The security of attachment in a child affects the child's emotional, cognitive, and social competence later in life.[32]
Evolutionary psychology
Evolutionary psychology and evolutionary psychiatry posit that many mental disorders involve the dysfunctional operation of mental modules adapted to ancestral physical or social environments but not necessarily to modern ones.[33][34][35][36] Behavioral abnormalities that resemble human mental illness have been found in closely related species (great apes).[37]
Other theories suggest that mental illness could have evolutionary advantages for the species, including enhancing creativity[38] and stress to enhance survival by easily activating the flight-or-fight response in anticipation of danger.
Schizophrenia could have been beneficial in prehistoric times by improving creativity during stressful times, or by helping to disseminate delusional tales that would have aided in group cohesion and finding gullible mates. The paranoia associated with Schizophrenia could have prevented danger from other humans and other animals.
Mania and depression could have benefited from seasonal changes by helping to increase energy levels during times of plenty and rejuvenating energy during times of scarcity. In this way mania was activated during the spring and summer to facilitate energy for hunting and depression worked best during the winter, similar to how bears hibernate in the winter to recover their energy levels. This may explain the connection between circadian genes and Bipolar Disorder and may explain the connection between light and seasonal affective disorder.[39]
Factors affecting choices
Some psychiatrists might favour biomedical models because they believe such models make their discipline seem more esteemed.[40]
Biological factors
Biological factors consist of anything physical that can cause adverse effects on a person's mental health. This includes genetics, prenatal damage, infections, exposure to toxins, brain defects or injuries, and substance abuse.[41] Many professionals believe that the sole cause of mental disorders is based upon the biology of the brain and the nervous system.[42]
Mind mentions genetic factors, long-term physical health conditions, and head injuries or epilepsy (affecting behaviour and mood) as factors that may possibly trigger an episode of mental illness.[43]
Genetics
Family-linkage and twin studies have indicated that genetic factors often play an important role in the development of mental disorders. The reliable identification of specific genetic susceptibility to particular disorders, through linkage or association studies, has proven difficult.[44][45] This has been reported to be likely due to the complexity of interactions between genes, environmental events, and early development[46] or to the need for new research strategies.[47] The heritability of behavioral traits associated with mental disorder may be greater in permissive than in restrictive environments, and susceptibility genes probably work through both "within-the-skin" (physiological) pathways and "outside-the-skin" (behavioral and social) pathways.[48] Investigations increasingly focus on links between genes and endophenotypes—more specific traits (including neurophysiological, biochemical, endocrinological, neuroanatomical, cognitive, or neuropsychological)—rather than disease categories.[49][50] With regard to a prominent mental disorder, schizophrenia, for a long time consensus among scientists was that certain alleles (forms of genes) were responsible for schizophrenia, but some research has indicated only multiple, rare mutations thought to alter neurodevelopmental pathways that can ultimately contribute to schizophrenia; virtually every rare structural mutation was different in each individual.[51]
Research has shown that many conditions are polygenic meaning there are multiple defective genes rather than only one that are responsible for a disorder.[41] Schizophrenia and Alzheimer's are both examples of hereditary mental disorders.[25]
The increasing understanding of brain plasticity (neuroplasticity) raises questions of whether some brain differences may be caused by mental illnesses, rather than pre-existing and causing them.
Prenatal damage
Any damage that occurs to a fetus while still in its mother's womb is considered prenatal damage. If the pregnant mother uses drugs or alcohol or is exposed to illnesses or infections then mental disorders can develop in the fetus. According to research, certain conditions, such as autism result from a disruption of early fetal brain progression.[41]
Environmental events surrounding pregnancy and birth have been linked to an increased development of mental illness in the offspring. This includes maternal exposure to serious psychological stress or trauma, conditions of famine, obstetric birth complications, infections, and gestational exposure to alcohol or cocaine. Such factors have been hypothesized to affect specific areas of neurodevelopment within the general developmental context and to restrict neuroplasticity.[52][53]
Infection, disease and toxins
A number of psychiatric disorders have often been tentatively linked with microbial pathogens, particularly viruses; however while there have been some suggestions of links from animal studies, and some inconsistent evidence for infectious and immune mechanisms (including prenatally) in some human disorders, infectious disease models in psychiatry are reported to have not yet shown significant promise except in isolated cases.[54]
There have been some inconsistent findings of links between infection by the parasite Toxoplasma gondii and human mental disorders such as schizophrenia, with the direction of causality unclear.[55][56][57] A number of diseases of the white matter can cause symptoms of mental disorder.[58]
Poorer general health has been found among individuals with severe mental illnesses, thought to be due to direct and indirect factors including diet, bacterial infections, substance use, exercise levels, effects of medications, socioeconomic disadvantages, lowered help-seeking or treatment adherence, or poorer healthcare provision.[59] Some chronic general medical conditions have been linked to some aspects of mental disorder, such as AIDS-related psychosis.
The current research on Lyme disease caused by a deer tick, and related toxins, is expanding the link between bacterial infections and mental illness.[60]
Research shows that infections and exposure to toxins such as HIV and streptococcus cause dementia and OCD respectively.[41][61] The infections or toxins trigger a change in the brain chemistry, which can develop into a mental disorder.
Injury and brain defects
Any damage to the brain can cause a mental disorder. The brain is the control system for the nervous system and the rest of the body. Without it the body cannot function properly.[42]
Higher rates of mood, psychotic, and substance abuse disorders have been found following traumatic brain injury (TBI). Findings on the relationship between TBI severity and prevalence of subsequent psychiatric disorders have been inconsistent, and occurrence has been linked to prior mental health problems as well as direct neurophysiological effects, in a complex interaction with personality and attitude and social influences.[62]
Head trauma is classified as either open or closed head injury. In open head injury the skull is penetrated and brain tissue is destroyed in a localized area. Closed head injury is more common, the skull is not penetrated but there is an impact of the brain against the skull which can create permanent structural damage (e.g. subdural hematoma). With both types, symptoms may disappear or persist over time. It has been found that typically the longer the length of time spent unconscious and the length of post-traumatic amnesia the worse the prognosis for the individual. The cognitive residual symptoms of head trauma are associated with the type of injury (either open head injury or closed head injury) and the amount of tissue destroyed. Symptoms of closed injury head trauma tend to be the experience of intellectual deficits in abstract reasoning ability, judgement, and memory, and also marked personality changes. Symptoms of open injury head trauma tend to be the experience of classic neuropsychological syndromes like aphasia, visual-spatial disorders, and types of memory or perceptual disorders.[63]
Brain tumors are classified as either malignant and benign, and as intrinsic (directly infiltrate the parenchyma of the brain) or extrinsic (grows on the external surface of the brain and produces symptoms as a result of pressure on the brain tissue). Progressive cognitive changes associated with brain tumors may include confusion, poor comprehension, and even dementia. Symptoms tend to depend on the location of the tumor on the brain. For example, tumors on the frontal lobe tend to be associated with the symptoms of impairment of judgment, apathy, and loss of the ability to regulate/modulate behavior.[64]
Findings have indicated abnormal functioning of brainstem structures in individuals with mental disorders such as schizophrenia, and other disorders that have to do with impairments in maintaining sustained attention.[65] Some abnormalities in the average size or shape of some regions of the brain have been found in some disorders, reflecting genes and/or experience. Studies of schizophrenia have tended to find enlarged ventricles and sometimes reduced volume of the cerebrum and hippocampus, while studies of (psychotic) bipolar disorder have sometimes found increased amygdala volume. Findings differ over whether volumetric abnormalities are risk factors or are only found alongside the course of mental health problems, possibly reflecting neurocognitive or emotional stress processes and/or medication use or substance use.[66][67] Some studies have also found reduced hippocampal volumes in major depression, possibly worsening with time depressed.[68]
Neurotransmitter systems
Abnormal levels of dopamine activity have been correlated with a number of disorders (e.g., reduced in ADHD and OCD, and increased in schizophrenia).[69] Dysfunction in serotonin and other monoamine neurotransmitters (e.g., norepinephrine and dopamine), and their associated neural networks, are also moderately correlated with certain mental disorders, including major depression, obsessive compulsive disorder, phobias, posttraumatic stress disorder, and generalized anxiety disorder. Studies of depleted levels of monoamine neurotransmitters show an association with depression and other psychiatric disorders, but "... it should be questioned whether 5-HT [serotonin] represents just one of the final, and not the main, factors in the neurological chain of events underlying psychopathological symptoms...." [70][71]
Simplistic "chemical imbalance" explanations for mental disorders have never received empirical support; and most prominent psychiatrists, neuroscientists, and psychologists have not espoused such ill-defined, facile etiological theories.[72][73] Instead, neurotransmitter systems have been understood in the context of the diathesis-stress or biopsychosocial models. The following 1967 quote from renowned psychiatric and neuroscience researchers exemplifies this more sophisticated understanding (in contrast to the woolly "chemical imbalance" notion).
Whereas specific genetic factors may be of importance in the etiology of some, and possibly all, depressions, it is equally conceivable that early experiences of the infant or child may cause enduring biochemical changes, and that these may predispose some individuals to depressions in adulthood. It is not likely that changes in the metabolism of the biogenic amines alone will account for the complex phenomena of normal or pathological affect.[74]
Substance abuse
Substance abuse, especially long-term abuse, can cause or exacerbate many mental disorders. Alcoholism is linked to depression while abuse of amphetamines and LSD can leave a person feeling paranoid and anxious.[75]
Correlations of mental disorders with drug use include cannabis,[12] alcohol and caffeine.[76] Caffeine use is correlated with anxiety[77] and suicide. Illicit drugs have the ability to stimulate particular parts of the brain which can affect development in adolescence. Cannabis has been found to worsen depression and lessen an individual's motivation.[12] Alcohol has the potential to damage "white matter" in the brain which affects thinking and memory. Alcohol has been found to be a serious problem in many countries due to many people participating in excessive drinking or binge drinking.
Life experience and environmental factors
The term "environment" is very loosely defined when it comes to mental illness. Unlike biological and psychological causes, environmental causes are stressors that individuals deal with in everyday life. These stressors range from financial issues to having low self-esteem. Environmental causes are more psychologically based thus making them more closely related.[78] Events that evoke feelings of loss or damage are most likely to cause a mental disorder to develop in an individual.[79] Environmental factors include but are not limited to dysfunctional home life, poor relationships with others, substance abuse, not meeting social expectations, low self-esteem and poverty.[41]
Mind mentions childhood abuse, trauma, violence or neglect, social isolation, loneliness or discrimination, the death of someone close, stress, homelessness or poor housing, social disadvantage, poverty or debt, unemployment, caring for a family member or friend, significant trauma as an adult, such as military combat, and being involved in a serious accident or being the victim of a violent crime as possibly triggering an episode of mental illness.[43]
Repeating generational patterns have been found to be a risk factor for mental illness.[8][9]
Life events and emotional stress
It is reported that treatment in childhood and in adulthood, including sexual abuse, physical abuse, emotional abuse, domestic violence and bullying, has been linked to the development of mental disorders, through a complex interaction of societal, family, psychological and biological factors.[80][81][82][83][84][85] Negative or stressful life events more generally have been implicated in the development of a range of disorders, including mood and anxiety disorders.[86] The main risks appear to be from a cumulative combination of such experiences over time, although exposure to a single major trauma can sometimes lead to psychopathology, including PTSD. Resilience to such experiences varies, and a person may be resistant to some forms of experience but susceptible to others. Features associated with variations in resilience include genetic vulnerability, temperamental characteristics, cognitive set, coping patterns, and other experiences.[87]
For bipolar disorder, stress (such as childhood adversity) is not a specific cause, but does place genetically and biologically vulnerable individuals at risk for a more severe course of illness.[88]
Poor parenting, abuse and neglect
Poor parenting has been found to be a risk factor for depression[15] and anxiety.[17][18] Separation or bereavement in families, and childhood trauma, have been found to be risk factors for psychosis and schizophrenia.[16][89]
Severe psychological trauma such as abuse can wreak havoc on a person's life. Children are much more susceptible to psychological harm from traumatic events than adults. Once again, the reaction to the trauma will vary based on the person as well as the individual's age. The impact of these events is influenced by several factors: the type of event, the length of exposure the individual had to the event, and the extent to which the individual and their family/friends were personally affected by the event. Human-caused disasters, such as a tumultuous childhood affect children more than natural disasters[90]
Neglect is a type of maltreatment related to the failure to provide needed, age-appropriate care, supervision and protection. It is not to be confused with abuse, which, in this context, is defined as any action that intentionally harms or injures another person.[91] Neglect most often happens during childhood by the parents or caretakers. Oftentimes, parents who are guilty of neglect were also neglected as children. The long-term effects of neglect are reduced physical, emotional, and mental health in a child and throughout adulthood.[90]
Adverse childhood experiences
Adverse childhood experiences (ACEs) such as physical or emotional neglect or both, abuse, poverty, malnutrition, and traumatic experiences can have long-lasting negative consequences. Adverse experiences in childhood can affect the structural and functional development of the brain, giving structural and functional abnormalities in later life, and in adulthood.[92][93] The Adverse Childhood Experiences Study has shown a strong dose–response relationship between ACEs and numerous health, social, and behavioral problems throughout a person's lifespan, including suicide attempts and frequency of depressive episodes.[94] A number of adverse childhood experiences can give a level of stress known as toxic stress.[92] A child's neurological development can be disrupted when chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or suffering from a mental illness. As a result, the child's cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt various harmful coping strategies that can contribute to later disease and disability.[94] Childhood adversity is also associated with an increased risk for developing severe mental illnesses, including schizophrenia, and it has been suggested that it could contribute to some features of the illness, including cognitive impairment. Findings from several studies have been mixed but some suggest that cognitive impairment is more related to forms of neglect than any other form of adversity. Underlying mechanisms remain unknown.[93]
Relationships
Relationship issues have been consistently linked to the development of mental disorders, with continuing debate on the relative impact of the home environment or work/school and peer groups. Issues with parenting skills or parental depression or other problems may be a risk factor. Parental divorce appears to increase risk, perhaps only if there is family discord or disorganization, although a warm supportive relationship with one parent may compensate. Details of infant feeding, weaning, toilet training etc. do not appear to be importantly linked to psychopathology. Early social privation, or lack of ongoing, harmonious, secure, committed relationships, have been implicated in the development of mental disorders.[95]
Some approaches, such as certain theories of co-counseling, may see all non-neurological mental disorders as the result of the self-regulating mechanisms of the mind (which accompany the physical expression of emotions) not being allowed to operate.
How an individual interacts with others as well as the quality of relationships can greatly increase or decrease a person's quality of living. Continuous fighting with friends and family can all lead to an increased risk of developing a mental illness. A dysfunctional family may include disobedience, child neglect and/or abuse which occurs regularly. These types of families are often a product of an unhealthy co-dependent relationship on the part of the head of the household (usually to drugs).
Losing a loved one, especially at an early age can have lasting effects on an individual. The individual may feel fear, guilt, anger or loneliness. This can drive a person into solitude and depression. They may turn to alcohol and drugs to cope with their feelings.
Divorce is also another factor that can take a toll on both children and adults alike. Divorcees may suffer from emotional adjustment problems due to a loss of intimacy and social connections. Newer statistics show that the negative effects of divorce have been greatly exaggerated.[96] The effects of divorce in children are based on three main factors: the quality of their relationship with each of their parents before the separation, the intensity and duration of the parental conflict, and the parents' ability to focus on the needs of children in their divorce.
Social expectations and esteem
How individuals view themselves ultimately determines who they are, their abilities and what they can be. Having both too low of self-esteem as well as too high of one can be detrimental to an individual's mental health.[97] A person's self-esteem plays a much larger role in their overall happiness and quality of life. Poor self-esteem whether it be too high or too low can result in aggression, violence, self-deprecating behavior, anxiety, and other mental disorders.
Not fitting in with the masses can result in bullying and other types of emotional abuse. Bullying can result in depression, feelings of anger, loneliness.
Poverty
Studies show that there is a direct correlation between poverty and mental illness. The lower the socioeconomic status of an individual the higher the risk of mental illness. Impoverished people are actually two to three times more likely to develop mental illness than those of a higher economic class.
Low levels of self-efficiency and self-worth are commonly experienced by children of disadvantaged families or those from the economic underclass. Theorists of child development have argued that persistent poverty leads to high levels of psychopathology and poor self-concepts.[98]
This increased risk for psychiatric complications remains consistent for all individuals among the impoverished population, regardless of any in-group demographic differences that they may possess.[99] These families must deal with economic stressors like unemployment and lack of affordable housing, which can lead to mental health disorders. A person's socioeconomic class outlines the psychosocial, environmental, behavioral, and biomedical risk factors that are associated with mental health.[100]
According to findings there is a strong association between poverty and substance abuse. Substance abuse only perpetuates a continuous cycle. It can make it extremely difficult for individuals to find and keep jobs. As stated earlier, both financial problems and substance abuse can cause mental illnesses to develop.[101]
Communities and cultures
Mental disorders have been linked to the overarching social, economic and cultural system.[102][103][104][105][106] Some non-Western views take this community approach.[21]
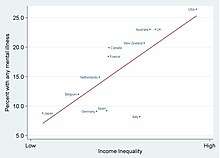
Problems in communities or cultures, including poverty, unemployment or underemployment, lack of social cohesion, and migration, have been associated with the development of mental disorders.[22][87] Stresses and strains related to socioeconomic position (socioeconomic status (SES) or social class) have been linked to the occurrence of major mental disorders, with a lower or more insecure educational, occupational, economic or social position generally linked to more mental disorders.[107] There have been mixed findings on the nature of the links and on the extent to which pre-existing personal characteristics influence the links. Both personal resources and community factors have been implicated, as well as interactions between individual-level and regional-level income levels.[108] The causal role of different socioeconomic factors may vary by country.[109] Socioeconomic deprivation in neighborhoods can cause worse mental health, even after accounting for genetic factors.[110] In addition, minority ethnic groups, including first or second-generation immigrants, have been found to be at greater risk for developing mental disorders, which has been attributed to various kinds of life insecurities and disadvantages, including racism.[111] The direction of causality is sometimes unclear, and alternative hypotheses such as the drift hypothesis sometimes need to be discounted.
Psychological and individual factors, including resilience
Some clinicians believe that psychological characteristics alone determine mental disorders. Others speculate that abnormal behavior can be explained by a mix of social and psychological factors. In many examples, environmental and psychological triggers complement one another resulting in emotional stress, which in turn activates a mental illness[112] Each person is unique in how they will react to psychological stressors. What may break one person may have little to no effect on another. Psychological stressors, which can trigger mental illness, are as follows: emotional, physical or sexual abuse, loss of a significant loved one, neglect and being unable to relate to others.[41]
The inability to relate to others is also known as emotional detachment. Emotional detachment makes it difficult for an individual to empathize with others or to share their own feelings. An emotionally detached person may try to rationalize or apply logic to a situation to which there is no logical explanation. These individuals tend to stress the importance of their independence and may be a bit neurotic.[113] Oftentimes, the inability to relate to others stems from a traumatic event.
Mental characteristics of individuals, as assessed by both neurological and psychological studies, have been linked to the development and maintenance of mental disorders. This includes cognitive or neurocognitive factors, such as the way a person perceives, thinks or feels about certain things;[114][115][116][117][118] or an individual's overall personality,[10] temperament or coping style[119][120][121] or the extent of protective factors or "positive illusions" such as optimism, personal control and a sense of meaning.[122][123]
Notes
- "Mental, behavioural or neurodevelopmental disorders". International Classification of Diseases for Mortality and Morbidity Statistics, 11th rev. (ICD-11 MMS). World Health Organization. April 2019. Retrieved 2019-10-30.
Mental, behavioural and neurodevelopmental disorders are syndromes characterized by clinically significant disturbance in an individual's cognition, emotional regulation, or behaviour that reflects a dysfunction in the psychological, biological, or developmental processes that underlie mental and behavioural functioning. These disturbances are usually associated with distress or impairment in personal, family, social, educational, occupational, or other important areas of functioning.
- Webster's Third New International Dictionary, (Springfield, MA: Merriam-Webster, 1961, rev. 2016), ("mental illness noun, variants: or mental disorder or less commonly mental disease, Definition of mental illness: any of a broad range of medical conditions (such as major depression, schizophrenia, obsessive compulsive disorder, or panic disorder) that are marked primarily by sufficient disorganization of personality, mind, or emotions to impair normal psychological functioning and cause marked distress or disability and that are typically associated with a disruption in normal thinking, feeling, mood, behavior, interpersonal interactions, or daily functioning").
- American Heritage Dictionary of the English Language, 5th ed. (Boston: Houghton Mifflin Harcourt, 2011, rev. 2018), ("mental disorder, n. - Any of various disorders, such as schizophrenia, bipolar disorder, or autism spectrum disorder, characterized by a distressing or disabling impairment of an individual's cognitive, emotional, or social functioning.")
- Oxford English Dictionary, 3rd ed. (Oxford, UK: Oxford University Press, September 2001), ("II. Senses relating to the mind in an unhealthy or abnormal state. 5. a. Designating a temporary or permanent impairment of the mind due to inherited defect, injury, illness, or environment, usually needing special care or rehabilitation. Esp. in mental breakdown, mental deficiency, mental disease, mental disorder, mental incapacity, mental retardation, etc.; see also mental illness n. at Compounds. ... mental illness n. a condition which causes serious abnormality in a person's thinking or behaviour, esp. one requiring special care or treatment; a psychiatric illness. Now somewhat dated, and sometimes avoided as being potentially offensive.").
- Arango, Celso; Díaz-Caneja, Covadonga M; McGorry, Patrick D; Rapoport, Judith; Sommer, Iris E; Vorstman, Jacob A; McDaid, David; Marín, Oscar; Serrano-Drozdowskyj, Elena; Freedman, Robert; Carpenter, William (2018). "Preventive strategies for mental health" (PDF). The Lancet Psychiatry. 5 (7): 591–604. doi:10.1016/S2215-0366(18)30057-9. PMID 29773478.
- Lee Anna Clark, et al., "Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health's Research Domain Criteria (RDoC)" (PDF), Psychological Science in the Public Interest 18, no. 2 (2017), 75. https://doi.org/10.1177/1529100617727266 ("... research has shown that psychopathology generally arises from multiple biological, behavioral, psychosocial, and cultural factors, all interacting in complex ways and filtered through an individual’s lifetime of experience. Research also has shown that the outcomes of these factors and their interactions are not clearly definable, distinct diseases, but are instead complex and variable combinations of psychological problems.")
- Sellers, R.; Collishaw, S; et al. (2012). "Risk of psychopathology in adolescent offspring of mothers with psychopathology and recurrent depression". The British Journal of Psychiatry. 202 (2): 108–14. doi:10.1192/bjp.bp.111.104984. PMID 23060622.
- Hancock, KJ; Mitrou, F; et al. (2013). "A three generation study of the mental health relationships between grandparents, parents and children". BMC Psychiatry. 13: 299. doi:10.1186/1471-244X-13-299. PMC 3829660. PMID 24206921.
- Boursnell, M (2011). "Parents with mental Illness: The cycle of intergenerational mental illness". Children Australia. 36 (1): 23–32. doi:10.1375/jcas.36.1.26 – via Academia.edu.
- Jeronimus, BF; Kotov, R; et al. (2016). "Neuroticism's prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: A meta-analysis on 59 longitudinal/prospective studies with 443 313 participants". Psychological Medicine. 46 (14): 1–24. doi:10.1017/S0033291716001653. PMID 27523506.
- Ormel, J; Jeronimus, BF; et al. (2013). "Neuroticism and common mental disorders: Meaning and utility of a complex relationship". Clinical Psychology Review. 33 (5): 686–97. doi:10.1016/j.cpr.2013.04.003. PMC 4382368. PMID 23702592.
- "Cannabis and mental health". Rcpsych.ac.uk. Retrieved 23 April 2013.
- Fergusson, DM; Boden, JM; Horwood, LJ (2009). "Tests of causal links between alcohol abuse or dependence and major depression". Archives of General Psychiatry. 66 (3): 260–6. doi:10.1001/archgenpsychiatry.2008.543. PMID 19255375.
- Winston, AP (2005). "Neuropsychiatric effects of caffeine". Advances in Psychiatric Treatment. 11 (6): 432–9. doi:10.1192/apt.11.6.432.
- Pillemer, K; Suitor, JJ; et al. (2010). "Mothers' Differentiation and depressive symptoms among adult children". Journal of Marriage and Family. 72 (2): 333–45. doi:10.1111/j.1741-3737.2010.00703.x. PMC 2894713. PMID 20607119.
- "The Report". The Schizophrenia Commission. 13 November 2012. Archived from the original on 5 April 2013. Retrieved 23 April 2013.
- National Research Council (Us) Institute Of Medicine (Us) Committee On The Prevention Of Mental Disorders Substance Abuse Among Children, Youth; O'Connell, M. E.; Boat, T.; Warner, K. E. (2009). "Table E-4 Risk Factors for Anxiety". In O'Connell, Mary Ellen; Boat, Thomas; Warner, Kenneth E. (eds.). Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective. National Academies Press. p. 530. doi:10.17226/12480. ISBN 978-0-309-12674-8. PMID 20662125.
- Bienvenu, OJ; Ginsburg, GS (2007). "Prevention of anxiety disorders". International Review of Psychiatry. 19 (6): 647–54. doi:10.1080/09540260701797837. PMID 18092242. S2CID 95140.
- Griffin, Catherine (28 February 2013). "Five Very Different and Major Psych Disorders Have Shared Genetics". Science World Report. Retrieved 28 February 2013.
- Link, BG; Phelan, JC; et al. (1999). "Public conceptions of mental illness: Labels, causes, dangerousness, and social distance". American Journal of Public Health. 89 (9): 1328–33. doi:10.2105/AJPH.89.9.1328. PMC 1508784. PMID 10474548.
- Thomas, P; Bracken, P; Yasmeen, S (2007). "Explanatory models for mental illness: Limitations and dangers in a global context" (PDF). Pak J Neurol Sci. 2 (3): 176–81 – via www.mentalhealth.freeuk.com.
- Pilgrim, David; Rogers, Anne (2005). A sociology of mental health and illness. Milton Keynes: Open University Press. ISBN 978-0-335-21583-6.
- Ghaemi, SN (November 2006). "Paradigms of psychiatry: Eclecticism and its discontents". Current Opinion in Psychiatry. 19 (6): 619–24. doi:10.1097/01.yco.0000245751.98749.52. PMID 17012942.
- Insel, T.R.; Wang, P.S. (2010). "Rethinking mental illness". JAMA. 303 (19): 1970–1971. doi:10.1001/jama.2010.555. PMID 20483974. S2CID 8210144.
- Frey, Rebecca J. "Genetic factors and mental disorders". www.minddisorders.com. Advameg.
- Murthy, Rangaswamy Srinivasa; et al. (2002) [2001]. The World Health Report 2001: Mental Health, New Understanding, New Hope (Reprint ed.). Geneva: World Health Organization. ISBN 9789241562010.
- Kendler, K. S (1999). "Setting boundaries for psychiatric disorders". The American Journal of Psychiatry. 156 (12): 1845–8. doi:10.1176/ajp.156.12.1845 (inactive 2020-07-08). PMID 10588394.
- Segrist, Dan J. (2009). "What's Going on in Your Professor's Head? Demonstrating the Id, Ego, and Superego". Teaching of Psychology. 36 (1): 51–54. doi:10.1080/00986280802529285. S2CID 144552456.
- Westen D (1998). "The scientific legacy of Sigmund Freud: Toward a psychodynamically informed psychological science". Psychological Bulletin. 124 (3): 333–371. CiteSeerX 10.1.1.590.4857. doi:10.1037/0033-2909.124.3.333.
- Crittenden PM (June 2002). "Attachment, information processing, and psychiatric disorder". World Psychiatry. 1 (2): 72–75. PMC 1525137. PMID 16946856.
- Vondra, J. I., & Barnett, D. (1999). A typical attachment in infancy and early childhood among children at developmental risk. Monographs of the Society for Research in Child Development, 64 (3, Serial No. 258).
- Lowder, Gregory; Hansell, James; McWilliams, Nancy. "The Enduring Significance of Psychoanalytic Theory and Practice" (PDF).
- Downes, S. (21 May 2014). "Evolutionary Psychology". In Aalta, Edward N. (ed.). Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. Archived from the original on 21 December 2017.
- Baron-Cohen, Simon (1997). The Maladapted Mind: Classic Readings in Evolutionary Psychopathology. East Sussex: Psychology Press. ISBN 978-0-86377-460-7.
- Brüne, M (2002). "Toward an integration of interpersonal and biological processes: Evolutionary psychiatry as an empirically testable framework for psychiatric research". Psychiatry. 65 (1): 48–57. doi:10.1521/psyc.65.1.48.19759. PMID 11980046. S2CID 36634054.
- Nesse, RM (February 2002). "Evolutionary biology: A basic science for psychiatry". World Psychiatry. 1 (1): 7–9. PMC 1489830. PMID 16946805.
- Brune, M; Brunecohrs, U; McGrew, W; Preuschoft, S (2006). "Psychopathology in great apes: Concepts, treatment options and possible homologies to human psychiatric disorders". Neuroscience & Biobehavioral Reviews. 30 (8): 1246–59. doi:10.1016/j.neubiorev.2006.09.002. PMID 17141312. S2CID 10101196.
- Andreasen, N. C. (1987). "Creativity and mental illness: Prevalence rates in writers and their first-degree relatives". American Journal of Psychiatry. 144 (10): 1288–92. doi:10.1176/ajp.144.10.1288. PMID 3499088.
- McClung, Colleen A. (2007). "Circadian genes, rhythms and the biology of mood disorders". Pharmacology & Therapeutics. 114 (2): 222–232. doi:10.1016/j.pharmthera.2007.02.003. PMC 1925042. PMID 17395264.
- Angermeyer, Matthias C; Holzinger, Anita; Carta, Mauro G; Schomerus, Georg (2018). "Biogenetic explanations and public acceptance of mental illness: Systematic review of population studies". British Journal of Psychiatry. 199 (5): 367–72. doi:10.1192/bjp.bp.110.085563. PMID 22045945.
- "Causes of Mental Illness". WebMD.
- Cherry, Kendra. "Causes of Mental Disorders". www.netplaces.com. About.com. Archived from the original on 12 May 2015.
- "What causes mental health problems?". www.mind.org.uk. Mind. Archived from the original on 30 March 2014.
- Insel, TR; Collins, FS (April 2003). "Psychiatry in the genomics era". Am J Psychiatry. 160 (4): 616–20. doi:10.1176/appi.ajp.160.4.616. PMID 12668345.
- Bearden, CE; Reus, VI; Freimer, NB (June 2004). "Why genetic investigation of psychiatric disorders is so difficult". Current Opinion in Genetics & Development. 14 (3): 280–6. doi:10.1016/j.gde.2004.04.005. PMID 15172671.
- Kas, MJ; Fernandes, C; et al. (April 2007). "Genetics of behavioural domains across the neuropsychiatric spectrum: Of mice and men". Mol Psychiatry. 12 (4): 324–30. doi:10.1038/sj.mp.4001979. PMID 17389901. S2CID 30846397.
- Burmeister, M (2006). "Genetics of psychiatric disorders: A primer". Focus. 4 (3): 317. doi:10.1176/foc.4.3.317 (inactive 2020-07-08).
- Kendler, KS (2001). "Twin studies of psychiatric illness". Archives of General Psychiatry. 58 (11): 1005–14. doi:10.1001/archpsyc.58.11.1005. PMID 11695946. S2CID 21257315.
- Bearden, CE; Freimer, NB (June 2006). "Endophenotypes for psychiatric disorders: Ready for primetime?". Trends Genet. 22 (6): 306–13. doi:10.1016/j.tig.2006.04.004. PMID 16697071.
- Glahn, DC; Thompson, PM; Blangero, J (June 2007). "Neuroimaging endophenotypes: Strategies for finding genes influencing brain structure and function" (PDF). Hum Brain Mapp. 28 (6): 488–501. CiteSeerX 10.1.1.582.7919. doi:10.1002/hbm.20401. PMC 6871286. PMID 17440953.
- Walsh, Tom (2008). "Rare Structural Variants Disrupt Multiple Genes in Neurodevelopmental Pathways in Schizophrenia" (PDF). Science. 320 (5875): 539–43. Bibcode:2008Sci...320..539W. doi:10.1126/science.1155174. PMID 18369103. S2CID 14385126. Archived from the original (PDF) on 22 July 2011. Retrieved 11 May 2011.
- Fumagalli, F; Molteni, R; et al. (March 2007). "Stress during development: Impact on neuroplasticity and relevance to psychopathology". Prog. Neurobiol. 81 (4): 197–217. doi:10.1016/j.pneurobio.2007.01.002. PMID 17350153. S2CID 22224892.
- Feldman, P.; Papalia, D. (2012). Experience Human Development (12th ed.). New York, NY: McGraw-Hill. p. 108. ISBN 978-0078035142.
- Pearce, BD (2003). "Modeling the role of infections in the etiology of mental illness". Clinical Neuroscience Research. 3 (4–5): 271–82. doi:10.1016/S1566-2772(03)00098-7. S2CID 53150065.
- Thomas, Hollie V; Thomas, Daniel Rh; Salmon, Roland L; Lewis, Glyn; Smith, Andy P (2004). "Toxoplasma and coxiella infection and psychiatric morbidity: A retrospective cohort analysis". BMC Psychiatry. 4: 32. doi:10.1186/1471-244X-4-32. PMC 526777. PMID 15491496.
- Alvarado-Esquivel, Cosme; Alanis-Quiñones, Olga-Patricia; Arreola-Valenzuela, Miguel-Ángel; Rodríguez-Briones, Alfredo; Piedra-Nevarez, Luis-Jorge; Duran-Morales, Ehecatl; Estrada-Martínez, Sergio; Martínez-García, Sergio-Arturo; Liesenfeld, Oliver (2006). "Seroepidemiology of Toxoplasma gondiiinfection in psychiatric inpatients in a northern Mexican city". BMC Infectious Diseases. 6: 178. doi:10.1186/1471-2334-6-178. PMC 1764421. PMID 17178002.
- Yolken, RH; Torrey, EF (1 January 1995). "Viruses, schizophrenia, and bipolar disorder". Clin Microbiol Rev. 8 (1): 131–45. doi:10.1128/CMR.8.1.131. PMC 172852. PMID 7704891.
- Walterfang, M; Wood, SJ; et al. (September 2005). "Diseases of white matter and schizophrenia-like psychosis". Aust N Z J Psychiatry. 39 (9): 746–56. doi:10.1111/j.1440-1614.2005.01678.x. PMID 16168032.
- Phelan, M; Stradins, L; Morrison, S (February 2001). "Physical health of people with severe mental illness: Can be improved if primary care and mental health professionals pay attention to it". BMJ. 322 (7284): 443–4. doi:10.1136/bmj.322.7284.443. PMC 1119672. PMID 11222406.
- Mental Disorders: MedlinePlus
- Perry, SW (1990). "Organic mental disorders caused by HIV: Update on early diagnosis and treatment". The American Journal of Psychiatry. 147 (6): 696–710. doi:10.1176/ajp.147.6.696. PMID 2188514.
- Fann, JR; Burington, B; et al. (January 2004). "Psychiatric illness following traumatic brain injury in an adult health maintenance organization population". Arch Gen Psychiatry. 61 (1): 53–61. doi:10.1001/archpsyc.61.1.53. PMID 14706944.
- Turner, Samuel M.; Hersen, Michel, eds. (1984). Adult Psychopathology and Diagnosis. Wiley Series on Personality Processes (2nd ed.). Canada: John Wiley. pp. 44–5. ISBN 978-0471089698.CS1 maint: ref=harv (link)
- Turner & Hersen (1984), pp. 45-6
- Mirsky, AF; Duncan, CC (2005). "Pathophysiology of mental illness: A view from the fourth ventricle". Int J Psychophysiol. 58 (2–3): 162–78. doi:10.1016/j.ijpsycho.2005.06.004. PMID 16213042.
- McDonald, C; Marshall, N; et al. (2006). "Regional brain morphometry in patients with schizophrenia or bipolar disorder and their unaffected relatives". American Journal of Psychiatry. 163 (3): 478–87. doi:10.1176/appi.ajp.163.3.478. PMID 16513870. S2CID 6432461.
- Velakoulis, D; Wood, SJ; et al. (2006). "Hippocampal and Amygdala Volumes According to Psychosis Stage and Diagnosis". Archives of General Psychiatry. 63 (2): 139–49. doi:10.1001/archpsyc.63.2.139. PMID 16461856.
- Colla, M; Kronenberg, G; et al. (2007). "Hippocampal volume reduction and HPA-system activity in major depression". Journal of Psychiatric Research. 41 (7): 553–60. doi:10.1016/j.jpsychires.2006.06.011. PMID 17023001.
- Iversen, SD; Iversen, LL (May 2007). "Dopamine: 50 years in perspective". Trends Neurosci. 30 (5): 188–93. doi:10.1016/j.tins.2007.03.002. PMID 17368565. S2CID 22686973.
- Marazziti, D. (2017). Understanding the role of serotonin in psychiatric diseases. F1000Research, 6, 180. doi:10.12688/f1000research.10094.1 PMC5325064.
- Ruhé, HG; Mason, NS; Schene, AH (April 2007). "Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: A meta-analysis of monoamine depletion studies". Mol Psychiatry. 12 (4): 331–59. doi:10.1038/sj.mp.4001949. PMID 17389902. S2CID 17386706.
- "Psychiatry's New Brain-Mind and the Legend of the "Chemical Imbalance" | Psychiatric Times". www.psychiatrictimes.com. Retrieved 2018-06-24.
- Hindmarch, I (2002). "Beyond the monoamine hypothesis: Mechanisms, molecules and methods". European Psychiatry. 17 Suppl 3: 294–9. doi:10.1016/S0924-9338(02)00653-3. PMID 15177084.
- Schildkraut, J. J., & Kety, S. S. (1967). Biogenic amines and emotion. Science, 156(3771), 21-30.
- "Effects of Alcohol and Drug Abuse; ...On your Health". Bowles Center for Alcohol Studies: University of North Carolina, Chapel Hill. Archived from the original on 22 May 2013. Retrieved 8 June 2013.
- Winston, AP (2005). "Neuropsychiatric effects of caffeine". Advances in Psychiatric Treatment. 11 (6): 432–9. doi:10.1192/apt.11.6.432.
- Vilarim, MM; Rocha Araujo, DM; Nardi, AE (2011). "Caffeine challenge test and panic disorder: a systematic literature review". Expert Review of Neurotherapeutics. 11 (8): 1185–95. doi:10.1586/ern.11.83. PMID 21797659. S2CID 5364016.
- "Causes of Mental Illness". www.mentalhealth.jami.org.uk.
- Schmidt, CW (2007). "Environmental connections: A deeper look into mental illness". Environmental Health Perspectives. 115 (8): A404, A406–10. doi:10.1289/ehp.115-a404. PMC 1940091. PMID 17687431.
- Spataro, J; Mullen, PE; et al. (2004). "Impact of child sexual abuse on mental health: Prospective study in males and females". The British Journal of Psychiatry. 184 (5): 416–21. doi:10.1192/bjp.184.5.416. PMID 15123505.
- Maughan, B; McCarthy, G (1997). "Childhood adversities and psychosocial disorders". British Medical Bulletin. 53 (1): 156–69. doi:10.1093/oxfordjournals.bmb.a011597. PMID 9158291. S2CID 2647938.
- Teicher, MH; Samson, JA; et al. (June 2006). "Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment". Am J Psychiatry. 163 (6): 993–1000. doi:10.1176/appi.ajp.163.6.993. PMID 16741199.
- Kessler, RC; Davis, CG; Kendler, KS (September 1997). "Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey". Psychol. Med. 27 (5): 1101–19. doi:10.1017/S0033291797005588. PMID 9300515.
- Pirkola, S; Isometsä, E; et al. (2005). "Childhood adversities as risk factors for adult mental disorders". Social Psychiatry and Psychiatric Epidemiology. 40 (10): 769–77. doi:10.1007/s00127-005-0950-x. PMID 16205853. S2CID 11844418.
- MacMillan, HL; Fleming, JE; et al. (2001). "Childhood abuse and lifetime psychopathology in a community sample". American Journal of Psychiatry. 158 (11): 1878–83. doi:10.1176/appi.ajp.158.11.1878. PMID 11691695. S2CID 7873719.
- Jeronimus, BF; Ormel, J; et al. (2013). "Negative and positive life events are associated with small but lasting change in neuroticism". Psychological Medicine. 43 (11): 2403–15. doi:10.1017/S0033291713000159. PMID 23410535. S2CID 43717734.
- Rutter, M (2000). "Psychosocial influences: Critiques, findings, and research needs". Dev. Psychopathol. 12 (3): 375–405. doi:10.1017/S0954579400003072. PMID 11014744.
- Miklowitz, DJ; Chang, KD (2008). "Prevention of bipolar disorder in at-risk children: Theoretical assumptions and empirical foundations". Development and Psychopathology. 20 (3): 881–97. doi:10.1017/S0954579408000424. PMC 2504732. PMID 18606036.
- Varese, F; Smeets, F; et al. (2012). "Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort Studies". Schizophrenia Bulletin. 38 (4): 661–71. doi:10.1093/schbul/sbs050. PMC 3406538. PMID 22461484.
- Feldman & Papalia (2012), p. 347
- medical-dictionary.com
- Pearce, J; Murray, C; Larkin, W (July 2019). "Childhood adversity and trauma: experiences of professionals trained to routinely enquire about childhood adversity". Heliyon. 5 (7): e01900. doi:10.1016/j.heliyon.2019.e01900. PMC 6658729. PMID 31372522.
- Green, MF; Horan, WP; Lee, J (June 2019). "Nonsocial and social cognition in schizophrenia: current evidence and future directions". World Psychiatry. 18 (2): 146–161. doi:10.1002/wps.20624. PMC 6502429. PMID 31059632.
- "Adverse Childhood Experiences". samhsa.gov. Rockville, Maryland, United States: Substance Abuse and Mental Health Services Administration. Archived from the original on 2016-10-09.
- Heinrich, LM; Gullone, E (October 2006). "The clinical significance of loneliness: A literature review". Clin Psychol Rev. 26 (6): 695–718. doi:10.1016/j.cpr.2006.04.002. PMID 16952717.
- "Psychological and Emotional Aspects of Divorce". www.meditate.com.
- Mann, M; Hosman, CM; et al. (2004). "Self-esteem in a broad-spectrum approach for mental health promotion". Health Education Research. 19 (4): 357–72. doi:10.1093/her/cyg041. PMID 15199011.
- McLeod, Jane D; Shanahan, Michael J (1993). "Poverty, Parenting, and Children's Mental Health". American Sociological Review. 58 (3): 351–66. doi:10.2307/2095905. JSTOR 2095905.
- Livingston Bruce Martha (1991). "Poverty and psychiatric status: Longitudinal evidence from the New Haven Epidemiologic Catchment Area Study". Archives of General Psychiatry. 48 (5): 470–474. doi:10.1001/archpsyc.1991.01810290082015. PMID 2021300.
- "Mental Illness and Poverty: A Fact Sheet" (PDF). www.fccmh.org. Florida Council for Community Mental Health. January 2007. Archived from the original (PDF) on 2017-08-30.
- Substance Abuse and Poverty | Addiction
- Fee, D (2000). Pathology and the Postmodern: Mental Illness as Discourse and Experience. London: Sage. ISBN 9780761952534.
- Al-Issa, Ihsan (1995). Handbook of Culture and Mental Illness: An International Perspective. New York: International Universities Press. ISBN 978-0-8236-2288-7.
- Krause, I (2006). "Hidden points of view in cross-cultural psychotherapy and ethnography". Transcultural Psychiatry. 43 (2): 181–203. doi:10.1177/1363461506064848. PMID 16893871.
- Bergin, Allen E.; Richards, P.J. (2000). Handbook of Psychotherapy and Religious Diversity. American Psychological Association (APA). ISBN 978-1-55798-624-5.
- Lipsedge, Maurice; Littlewood, Roland (1997). Aliens and Alienists: Ethnic Minorities and Psychiatry (3rd ed.). New York: Routledge. ISBN 978-0-415-15725-4.
- Muntaner, C; Eaton, WW; et al. (2004). "Socioeconomic position and major mental disorders". Epidemiologic Reviews. 26: 53–62. doi:10.1093/epirev/mxh001. PMID 15234947.
- Lorant, V; Deliège, D; et al. (2003). "Socioeconomic inequalities in depression: a meta-analysis". American Journal of Epidemiology. 157 (2): 98–112. doi:10.1093/aje/kwf182. PMID 12522017.
- Araya, R; Lewis, G; et al. (2003). "Education and income: Which is more important for mental health?". Journal of Epidemiology and Community Health. 57 (7): 501–5. doi:10.1136/jech.57.7.501. PMC 1732519. PMID 12821693.
- Caspi, A; Taylor, A; et al. (2000). "Neighborhood deprivation affects children's mental health: Environmental risks identified in a genetic design". Psychological Science. 11 (4): 338–42. doi:10.1111/1467-9280.00267. PMID 11273396.
- Chakraborty, A; McKenzie, K (2002). "Does racial discrimination cause mental illness?". The British Journal of Psychiatry. 180 (6): 475–7. doi:10.1192/bjp.180.6.475. PMID 12042221.
- Ahn, W-k; Proctor, CC; Flanagan, EH (2009). "Mental health clinicians' beliefs about the biological, psychological, and environmental bases of mental disorders". Cognitive Science. 33 (2): 147–182. doi:10.1111/j.1551-6709.2009.01008.x. PMC 2857376. PMID 20411158.
- Schreiner, Michael (8 December 2011). "Detached Personality". Evolution Counseling. Michael Schreiner. Archived from the original on 7 October 2013. Retrieved 11 June 2013.
- Iacoviello, BM; Alloy, LB; et al. (July 2006). "The course of depression in individuals at high and low cognitive risk for depression: A prospective study". J. Affect. Disord. 93 (1–3): 61–9. doi:10.1016/j.jad.2006.02.012. PMID 16545464.
- Peer, JE; Rothmann, TL; et al. (December 2004). "Social cognitive bias and neurocognitive deficit in paranoid symptoms: evidence for an interaction effect and changes during treatment". Schizophrenia Research. 71 (2–3): 463–71. doi:10.1016/j.schres.2004.03.016. PMID 15474917. S2CID 41056028.
- Bell, V; Halligan, PW; Ellis, HD (May 2006). "Explaining delusions: A cognitive perspective". Trends Cogn Sci. 10 (5): 219–26. doi:10.1016/j.tics.2006.03.004. PMID 16600666. S2CID 24541273.
- Weems, CF; Costa, NM; et al. (March 2007). "Cognitive errors, anxiety sensitivity, and anxiety control beliefs: Their unique and specific associations with childhood anxiety symptoms". Behav Modif. 31 (2): 174–201. doi:10.1177/0145445506297016. PMID 17307934.
- Brunelin, J; d'Amato, T; et al. (2007). "Impaired verbal source monitoring in schizophrenia: An intermediate trait vulnerability marker?". Schizophrenia Research. 89 (1–3): 287–92. doi:10.1016/j.schres.2006.08.028. PMID 17029909. S2CID 3017757.
- Gil, S; Caspi, Y (2006). "Personality traits, coping style, and perceived threat as predictors of posttraumatic stress disorder after exposure to a terrorist attack: A prospective study". Psychosom. Med. 68 (6): 904–9. doi:10.1097/01.psy.0000242124.21796.f8. PMID 17079704. S2CID 44659291.
- Brandes, M; Bienvenu, OJ (August 2006). "Personality and anxiety disorders". Curr Psychiatry Rep. 8 (4): 263–9. doi:10.1007/s11920-006-0061-8. PMID 16879789. S2CID 24264114.
- Christensen, MV; Kessing, LV (2006). "Do personality traits predict first onset in depressive and bipolar disorder?". Nord J Psychiatry. 60 (2): 79–88. doi:10.1080/08039480600600300. PMID 16635925.
- Taylor, SE; Stanton, AL (2007). "Coping resources, coping processes, and mental health". Annual Review of Clinical Psychology. 3: 377–401. doi:10.1146/annurev.clinpsy.3.022806.091520. PMID 17716061. S2CID 18631465.
- Mathews, A; MacLeod, C (2005). "Cognitive vulnerability to emotional disorders". Annual Review of Clinical Psychology. 1 (1): 167–95. doi:10.1146/annurev.clinpsy.1.102803.143916. PMID 17716086. S2CID 11460988.