Aldehyde dehydrogenase 6 family, member A1
Methylmalonate-semialdehyde dehydrogenase [acylating], mitochondrial (MMSDH) is an enzyme that in humans is encoded by the ALDH6A1 gene.[5][6]
This protein belongs to the aldehyde dehydrogenases family of proteins. This enzyme plays a role in the valine and pyrimidine catabolic pathways. The product of this gene, a mitochondrial methylmalonate semialdehyde dehydrogenase, catalyzes the irreversible oxidative decarboxylation of malonate and methylmalonate semialdehydes to acetyl- and propionyl-CoA. Methylmalonate semialdehyde dehydrogenase deficiency is characterized by elevated beta-alanine, 3-hydroxypropionic acid, and both isomers of 3-amino and 3-hydroxyisobutyric acids in urine organic acids.[6] Methylmalonate semialdehyde dehydrogenase deficiency is caused by mutations in this gene and the resulting protein.[7]
Structure
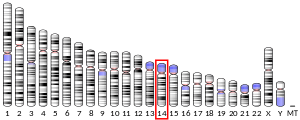
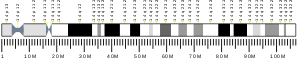
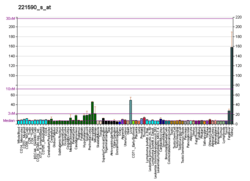
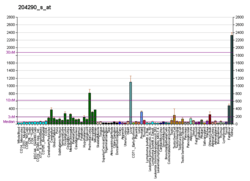
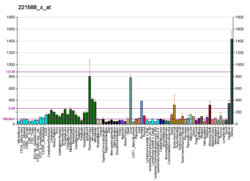
The ALDH6A1 gene is mapped onto 14q24.3, between markers D14S71 and D14S986, and has an exon count of 12.[8][6] The mRNA expression levels of this gene are highest in the kidney and liver, although mRNA levels have been found in many other tissues. The mature protein that this gene translates in humans is 503 amino acids long, which is similar to other enzymes of this family, which all comprise around 500 amino acids. This enzyme localizes to the mitochondria. Unlike other mitochondrial entry sequences, this does not contain as many arginine residues, and is in fact slightly longer.[7]
Function
MMSDH has esterase activity, which is characteristic of the enzymes in the Aldehyde Dehydrogenase family. It is more specifically involved in the valine and thymine catabolism pathways. When the enzyme acts on valine, (S)-3-hydroxyisobutyric acid is generated as an intermediate; this then undergoes oxidation by the enzyme 3-hydroxyisobutyrate dehydrogenase to form (S)-methylmalonic semialdehyde (MMSA). In thymine catabolism, the enzymatic reaction produces (R)-aminoisobutyric acid (AIBA), which is then deaminated to (R)-methylmalonic semialdehyde. These two enantiomers of MMSA are substrates for MMSDH, which catalyzes their oxidative decarboxylation to propionyl-CoA.[9] Both NAD+ and CoA act as cofactors with the enzyme, although they work in opposite directions; NAD+ works to protect the enzyme against proteolysis, but CoA esters diminish that effect.[10]
Clinical significance
Mutations in the ALDH6A1 gene are associated with methylmalonate semialdehyde dehydrogenase deficiency, a rare autosomal recessive inborn error of metabolism with a highly variable phenotype. The disease is passed through autosomal recessive genetics. There have been many individual and familial case studies of this deficiency and the mutations that cause it. Some patients with this disease may be asymptomatic, whereas others show global developmental delay, nonspecific dysmorphic features, and delayed myelination on brain imaging. Meanwhile, some cases have been only identified through elevated levels of various acidic metabolites in the urine, notably 3-hydroxyisobutyric acid.[7][11] This can result from an identified a homozygous 1336G-A transition in the gene, resulting in a change in the 446th residue from glycine to arginine.[12] Another case study, a child from consanguineous patients, presented as significant hypotonia in infancy, poor feeding, and dysmorphic facial features, including narrowed, downslanting palpebral fissures, short convex nose with depressed nasal bridge, microphthalmia, cataracts, and adducted thumbs. Brain imaging showed delayed myelination and thinning of the corpus callosum. Laboratory studies showed 3-hydroxyisobutyric aciduria and mild lactic acidosis.[13] Many case studies since then have presented similar symptoms, although the symptoms may be milder.[14] The mutations identified are generally heterozygous missense mutations: S262Y, P62S, Y172H and R535C.[7]
References
- GRCh38: Ensembl release 89: ENSG00000119711 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000021238 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Kedishvili NY, Popov KM, Rougraff PM, Zhao Y, Crabb DW, Harris RA (Sep 1992). "CoA-dependent methylmalonate-semialdehyde dehydrogenase, a unique member of the aldehyde dehydrogenase superfamily. cDNA cloning, evolutionary relationships, and tissue distribution". The Journal of Biological Chemistry. 267 (27): 19724–9. PMID 1527093.
- "Entrez Gene: ALDH6A1 aldehyde dehydrogenase 6 family, member A1".
- Marcadier JL, Smith AM, Pohl D, Schwartzentruber J, Al-Dirbashi OY, Majewski J, Ferdinandusse S, Wanders RJ, Bulman DE, Boycott KM, Chakraborty P, Geraghty MT (9 July 2013). "Mutations in ALDH6A1 encoding methylmalonate semialdehyde dehydrogenase are associated with dysmyelination and transient methylmalonic aciduria". Orphanet Journal of Rare Diseases. 8: 98. doi:10.1186/1750-1172-8-98. PMC 3710243. PMID 23835272.
- Chambliss KL, Gray RG, Rylance G, Pollitt RJ, Gibson KM (Jul 2000). "Molecular characterization of methylmalonate semialdehyde dehydrogenase deficiency". Journal of Inherited Metabolic Disease. 23 (5): 497–504. doi:10.1023/A:1005616315087. PMID 10947204.
- Kedishvili NY, Popov KM, Rougraff PM, Zhao Y, Crabb DW, Harris RA (Sep 1992). "CoA-dependent methylmalonate-semialdehyde dehydrogenase, a unique member of the aldehyde dehydrogenase superfamily. cDNA cloning, evolutionary relationships, and tissue distribution". The Journal of Biological Chemistry. 267 (27): 19724–9. PMID 1527093.
- Kedishvili NY, Popov KM, Harris RA (Oct 1991). "The effect of ligand binding on the proteolytic pattern of methylmalonate semialdehyde dehydrogenase". Archives of Biochemistry and Biophysics. 290 (1): 21–6. doi:10.1016/0003-9861(91)90586-8. PMID 1898092.
- Pollitt RJ, Green A, Smith R (1985). "Excessive excretion of beta-alanine and of 3-hydroxypropionic, R- and S-3-aminoisobutyric, R- and S-3-hydroxyisobutyric and S-2-(hydroxymethyl)butyric acids probably due to a defect in the metabolism of the corresponding malonic semialdehydes". Journal of Inherited Metabolic Disease. 8 (2): 75–9. doi:10.1007/bf01801669. PMID 3939535.
- Gray RG, Pollitt RJ, Webley J (Aug 1987). "Methylmalonic semialdehyde dehydrogenase deficiency: demonstration of defective valine and beta-alanine metabolism and reduced malonic semialdehyde dehydrogenase activity in cultured fibroblasts". Biochemical Medicine and Metabolic Biology. 38 (1): 121–4. doi:10.1016/0885-4505(87)90069-7. PMID 3117077.
- Shield JP, Gough R, Allen J, Newbury-Ecob R (Jul 2001). "3-Hydroxyisobutyric aciduria: phenotypic heterogeneity within a single family". Clinical Dysmorphology. 10 (3): 189–91. doi:10.1097/00019605-200107000-00007. PMID 11446412.
- Sass JO, Walter M, Shield JP, Atherton AM, Garg U, Scott D, Woods CG, Smith LD (May 2012). "3-Hydroxyisobutyrate aciduria and mutations in the ALDH6A1 gene coding for methylmalonate semialdehyde dehydrogenase". Journal of Inherited Metabolic Disease. 35 (3): 437–42. doi:10.1007/s10545-011-9381-x. PMID 21863277.
External links
- Human ALDH6A1 genome location and ALDH6A1 gene details page in the UCSC Genome Browser.
Further reading
- Kuiper H, Spötter A, Williams JL, Distl O, Drögemüller C (2005). "Physical mapping of CHX10, ALDH6A1, and ABCD4 on bovine chromosome 10q34". Cytogenetic and Genome Research. 109 (4): 533. doi:10.1159/000084217. PMID 15909363.
- Anderson NL, Polanski M, Pieper R, Gatlin T, Tirumalai RS, Conrads TP, Veenstra TD, Adkins JN, Pounds JG, Fagan R, Lobley A (Apr 2004). "The human plasma proteome: a nonredundant list developed by combination of four separate sources". Molecular & Cellular Proteomics. 3 (4): 311–26. doi:10.1074/mcp.M300127-MCP200. PMID 14718574.
- Chambliss KL, Gray RG, Rylance G, Pollitt RJ, Gibson KM (Jul 2000). "Molecular characterization of methylmalonate semialdehyde dehydrogenase deficiency". Journal of Inherited Metabolic Disease. 23 (5): 497–504. doi:10.1023/A:1005616315087. PMID 10947204.
- Suzuki Y, Yoshitomo-Nakagawa K, Maruyama K, Suyama A, Sugano S (Oct 1997). "Construction and characterization of a full length-enriched and a 5'-end-enriched cDNA library". Gene. 200 (1–2): 149–56. doi:10.1016/S0378-1119(97)00411-3. PMID 9373149.
- Maruyama K, Sugano S (Jan 1994). "Oligo-capping: a simple method to replace the cap structure of eukaryotic mRNAs with oligoribonucleotides". Gene. 138 (1–2): 171–4. doi:10.1016/0378-1119(94)90802-8. PMID 8125298.