Sleepwalking
Sleepwalking, also known as somnambulism or noctambulism, is a phenomenon of combined sleep and wakefulness.[1] It is classified as a sleep disorder belonging to the parasomnia family.[2] It occurs during slow wave sleep stage, in a state of low consciousness, with performance of activities that are usually performed during a state of full consciousness. These activities can be as benign as talking, sitting up in bed, walking to a bathroom, consuming food, and cleaning, or as hazardous as cooking, driving a motor vehicle,[3][4] violent gestures, grabbing at hallucinated objects,[5] or even homicide.[6][7]
| Sleepwalking | |
|---|---|
 | |
| John Everett Millais, The Somnambulist, 1871 | |
| Specialty | Psychiatry, Sleep medicine |
Although sleepwalking cases generally consist of simple, repeated behaviors, there are occasionally reports of people performing complex behaviors while asleep, although their legitimacy is often disputed.[8] Sleepwalkers often have little or no memory of the incident, as their consciousness has altered into a state in which memories are difficult to recall. Although their eyes are open, their expression is dim and glazed over.[9] This may last from 30 seconds to 30 minutes.[5]
Sleepwalking occurs during slow-wave sleep (N3) of non-rapid eye movement sleep (NREM sleep) cycles. It typically occurs within the first third of the night when slow-wave sleep is most prominent.[9] Usually, it will occur once in a night, if at all.[5]
Signs and symptoms
Sleepwalking is characterized by:[10]
- partial arousal during non-rapid eye movement (NREM) sleep, typically during the first third of the night
- dream content that may or may not be recalled when awake
- dream-congruent motor behavior that may be simple or complex
- impaired perception of the environment
- impaired judgement, planning and problem-solving.
The sleepwalker's eyes are open but may appear as a glassy-eyed stare or blank expression and pupils are dilated. They are often disoriented, consequent to awakening: the sleepwalker may be confused and perplexed, and might not know why or how they got out of bed; however, the disorientation will fade within minutes. They may talk while sleepwalking, but the talk typically does not make sense to the observer. There are varying degrees of amnesia associated with sleepwalking, ranging from no memory at all, vague memories or a narrative.[11]
Associated disorders
In the study "Sleepwalking and Sleep Terrors in Prepubertal Children"[12] it was found that, if a child had another sleep disorder – such as restless leg syndrome (RLS) or sleep-disorder breathing (SDB) – there was a greater chance of sleepwalking. The study found that children with chronic parasomnias may often also present SDB or, to a lesser extent, RLS. Furthermore, the disappearance of the parasomnias after the treatment of the SDB or RLS periodic limb movement syndrome suggests that the latter may trigger the former. The high frequency of SDB in family members of children with parasomnia provided additional evidence that SDB may manifest as parasomnias in children. Children with parasomnias are not systematically monitored during sleep, although past studies have suggested that patients with sleep terrors or sleepwalking have an elevated level of brief EEG arousals. When children receive polysomnographies, discrete patterns (e.g., nasal flow limitation, abnormal respiratory effort, bursts of high or slow EEG frequencies) should be sought; apneas are rarely found in children. Children's respiration during sleep should be monitored with nasal cannula or pressure transducer system or esophageal manometry, which are more sensitive than the thermistors or thermocouples currently used in many laboratories. The clear, prompt improvement of severe parasomnia in children who are treated for SDB, as defined here, provides important evidence that subtle SDB can have substantial health-related significance. Also noteworthy is the report of familial presence of parasomnia. Studies of twin cohorts and families with sleep terror and sleepwalking suggest genetic involvement of parasomnias. RLS and SDB have been shown to have familial recurrence. RLS has been shown to have genetic involvement.
Sleepwalking may also accompany the related phenomenon of night terrors, especially in children. In the midst of a night terror, the affected person may wander in a distressed state while still asleep, and examples of sufferers attempting to run or aggressively defend themselves during these incidents have been reported in medical literature.[13]
In some cases, sleepwalking in adults may be a symptom of a psychological disorder. One study suggests higher levels of dissociation in adult sleepwalkers, since test subjects scored unusually high on the hysteria portion of the "Crown-Crisp Experiential Index".[14] Another suggested that "A higher incidence [of sleepwalking events] has been reported in patients with schizophrenia, hysteria and anxiety neuroses".[15] Also, patients with migraine headaches or Tourette syndrome are 4–6 times more likely to sleepwalk.
Consequences
Most sleepwalkers had injuries at some point during sleepwalking, often minor injuries such as cuts or bruises.[16][17] In rare occasions, however, sleepwalkers have fractured bones and died as the result of a fall.[18][19] Sleepwalkers may also face embarrassment of being found naked in public.[20][21]
Causes
The cause of sleepwalking is unknown. A number of, as yet unproven, hypotheses are suggested for why it might occur, including: delay in the maturity of the central nervous system,[5] increased slow wave sleep,[22] sleep deprivation, fever, and excessive tiredness. There may be a genetic component to sleepwalking. One study found that sleepwalking occurred in 45% of children who have one parent who sleepwalked, and in 60% of children if both parents sleepwalked.[9] Thus, heritable factors may predispose an individual to sleepwalking, but expression of the behavior may also be influenced by environmental factors.[23] Genetic studies using common fruit flies as experimental models reveal a link between night sleep and brain development mediated by evolutionary conserved transcription factors such as AP-2 [24] Sleepwalking may be inherited as an autosomal dominant disorder with reduced penetrance. Genome-wide multipoint parametric linkage analysis for sleepwalking revealed a maximum logarithm of the odds score of 3.14 at chromosome 20q12-q13.12 between 55.6 and 61.4 cM.[25]
Sleepwalking has been hypothesized to be linked to the neurotransmitter serotonin, which also appears to be metabolized differently in migraine patients and people with Tourette syndrome, both populations being four to nine times more likely to experience an episode of sleepwalking.[26] Hormonal fluctuations have been found to contribute to sleepwalking episodes in women, with the likeliness to sleepwalk being higher before the onset of menstruation.[27] It also appears that hormonal changes during pregnancy decrease the likelihood of engaging in sleepwalking [28]
Medications, primarily in four classes—benzodiazepine receptor agonists and other GABA modulators, antidepressants and other serotonergic agents, antipsychotics, and β-blockers— have been associated with sleepwalking.[29] The best evidence of medications causing sleepwalking is for Zolpidem and sodium oxybate—all other reports are based on associations noted in case reports.[29]
A number of conditions, such as Parkinson's disease, are thought to trigger sleepwalking in people without a previous history of sleepwalking.[30]
Diagnosis
Polysomnography is the only accurate assessment of a sleepwalking episode. Because this is costly and sleepwalking episodes are usually infrequent, other measures commonly used include self-, parent-, or partner-report. Three common diagnostic systems that are generally used for sleepwalking disorders are International Classification of Diseases,[1] the International Classification of Sleep Disorders 3,[31] and the Diagnostic and Statistical Manual.[2]
Sleepwalking should not be confused with alcohol- or drug-induced blackouts, which can result in amnesia for events similar to sleepwalking. During an alcohol-induced blackout (drug-related amnesia), a person is able to actively engage and respond to their environment (e.g. having conversations or driving a vehicle), however the brain does not create memories for the events.[32] Alcohol-induced blackouts can occur with blood alcohol levels higher than 0.06g/dl.[33] A systematic review of the literature found that approximately 50% of drinkers have experienced memory loss during a drinking episode and have had associated negative consequences similar to sleepwalkers, including injury and death.[32]
Other differential diagnoses include Rapid eye movement sleep behavior disorder, confusional arousals, and night terrors.
There are two subcategories of sleepwalking:
- sleepwalking with sleep-related eating.
- sleepwalking with sleep-related sexual behavior (sexsomnia).[2]
Sleep eating involves consuming food while asleep. These sleep eating disorders are more often than not induced for stress related reasons. Another major cause of this sleep eating subtype of sleepwalking is sleep medication, such as Ambien for example (Mayo Clinic). There are a few others, but Ambien is a more widely used sleep aid.[34] Because many sleep eaters prepare the food they consume, there are risks involving burns and such with ovens and other appliances. As expected, weight gain is also a common outcome of this disorder, because food that is frequently consumed contains high carbohydrates. As with sleepwalking, there are ways that sleep eating disorders can be maintained. There are some medications that calm the sleeper so they can get longer and better-quality rest, but activities such as yoga can also be introduced to reduce the stress and anxiety causing the action.[35]
Assessment
An assessment of sleepwalking via polysomnography poses the problem that sleepwalking is less likely to occur in the sleep laboratory, and if an episode occurs, it is usually less complex than what the patient experiences at home.[36][37][38] Therefore, the diagnosis can often be made by assessment of sleep history, time-course and content of the sleep related behaviors.[39] Sometimes, home videos can provide additional information and should be considered in the diagnostic process.[40]
Some features that should always be assessed include:[41]
• Age of onset
• When the episode occurs during the sleep period
• How often these episodes occur (frequency) and how long they last (duration)
• Description of the episode, including behavior, emotions, and thoughts during and after the event
• How responsive the patient is to external stimuli during the episode
• How conscious or aware the patient is, when awakened from an episode
• If the episode is remembered afterwards
• The triggers or precipitating factors
• Sleep–wake pattern and sleep environment
• Daytime sleepiness
• Other sleep disorders that might be present
• Family history for NREM parasomnias and other sleep disorders
• Medical, psychiatric, and neurological history
• Medication and substance use history
Treatment
There have been no clinical trials to show that any psychological or pharmacological intervention is effective in preventing sleepwalking episodes.[10] Despite this, a wide range of treatments have been used with sleepwalkers. Psychological interventions have included psychoanalysis, hypnosis, scheduled or anticipatory waking, assertion training, relaxation training, managing aggressive feelings, sleep hygiene, classical conditioning (including electric shock), and play therapy. Pharmacological treatments have included an anticholinergic (biperiden), antiepileptics (carbamazepine, valproate), an antipsychotic (quetiapine), benzodiazepines (clonazepam, diazepam, flurazepam, imipramine, and triazolam), melatonin, a selective serotonin reuptake inhibitor (paroxetine), a barbiturate (sodium amytal) and herbs.[10]
There is no evidence to show that waking sleepwalkers is harmful or not, though the sleepwalker is likely to be disoriented if awakened as sleepwalking occurs during the deepest stage of sleep.
Unlike other sleep disorders, sleepwalking is not associated with daytime behavioral or emotional problems. This may be because the sleepwalker's sleep is not disturbed—unless they are woken, they are still in a sleep state while sleepwalking.
Maintaining the safety of the sleepwalker and others and seeking treatment for other sleep problems is recommended.[10] Reassurance is recommended if sleepwalking is not causing any problems.[10] However, if it causes distress or there is risk of harm, hypnosis and scheduled waking are recommended as treatments.[10]
Safety planning For those whose sleepwalking episodes turn to be hazardous, a door alarm may offer a measure of protection. There are various kinds of door alarms that can attach to a bedroom door and when the door is opened, the alarm sounds.[42] The intention is that the sound will fully awaken the person and interrupt the sleepwalking episode, or if the sleepwalker lives with others, the sound will prompt them to check on the person.
Sleepwalkers should aim to have their bedrooms on the first floor of a home, apartment, dorm, hotel, etc.
Sleepwalkers should not have easily accessible weapons (loaded guns, knives) in the bedroom or any room of the house for that matter. If there are weapons, they should be locked away with keys secluded from the sleepwalker.[11]
For partners of sleepwalkers who are violent or disturb their sleep, sleeping in another room may lead to better sleep quality and quantity.
Epidemiology
The lifetime prevalence of sleepwalking is estimated to be 4.6%–10.3%. A meta-analysis of 51 studies, that included more than 100,000 children and adults, found that sleepwalking is more common in children with an estimated 5%, compared with 1.5% of adults, sleepwalking at least once in the previous 12 months. The rate of sleepwalking has not been found to vary across ages during childhood.[43]
History
Sleepwalking has attracted a sense of mystery, but was not seriously investigated and diagnosed until the 19th century. The German chemist and parapsychologist Baron Karl Ludwig von Reichenbach (1788–1869) made extensive studies of sleepwalkers and used his discoveries to formulate his theory of the Odic force.[44]
Sleepwalking was initially thought to be a dreamer acting out a dream.[5] For example, in one study published by the Society for Science & the Public in 1954, this was the conclusion: "Repression of hostile feelings against the father caused the patients to react by acting out in a dream world with sleepwalking, the distorted fantasies they had about all authoritarian figures, such as fathers, officers and stern superiors."[45] This same group published an article twelve years later with a new conclusion: "Sleepwalking, contrary to most belief, apparently has little to do with dreaming. In fact, it occurs when the sleeper is enjoying his most oblivious, deepest sleep—a stage in which dreams are not usually reported."[46] More recent research has discovered that sleepwalking is actually a disorder of NREM (non-rapid eye movement) arousal.[5] Acting out a dream is the basis for a REM (rapid eye movement) sleep disorder called REM Behavior Disorder (or REM Sleep Behavior Disorder, RSBD).[5] More accurate data about sleep is due to the invention of technologies, such as the electroencephalogram (EEG) by Hans Berger in 1924 and BEAM by Frank Duffy in the early 1980s.[47]
In 1907, Sigmund Freud spoke about sleepwalking to the Vienna Psychoanalytic Society (Nunberg and Federn). He believed that sleepwalking was connected to fulfilling sexual wishes and was surprised that a person could move without interrupting their dream. At that time, Freud suggested that the essence of this phenomenon was the desire to go to sleep in the same area as the individual had slept in childhood. Ten years later, he speculated about somnambulism in the article "A Metapsychological Supplement to the Theory of Dreams" (1916–17 [1915]). In this essay, he started to clarify and expand his hypothetical ideas on dreams. The dreams is a fragile equilibrium that is only partially successful because the repressed unconscious impulses of the unconscious system. This does not obey the wishes of the ego and maintain their countercathexis. Another reason why dreams are partially successful is because certain preconscious daytime thoughts can be resistant and these can retain a part of their cathexis as well. It is probable how unconscious impulses and day residues can come together and result in a conflict. Freud then wondered about the outcome of this wishful impulse, which represents an unconscious instinctual demand and then it becomes a dream wish in the preconscious. Furthermore, Freud stated that this unconscious impulse could be expressed as mobility during sleep. This would be what is observed in somnambulism, though what actually makes it possible remains unknown.[48]
Society and culture
Opera
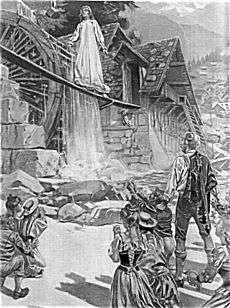
Vincenzo Bellini's 1831 Italian opera semiseria, La sonnambula, the plot of which is centered on the question of the innocence of the betrothed and soon-to-be married Amina; who, upon having been discovered in the bedchamber of a stranger, and despite the assurances of that stranger that Amina was entirely innocent, has been rejected by her enraged fiancé, Elvino — who, then, decides to marry another. In fact, when stressed, Amina was susceptible to somnambulism; and had come to be in the stranger's bedchamber by sleep-walking along a high parapet (in full view of the opera's audience). Elvino, who later observes the (exhausted by all the fuss) Amina, sleep-walking across a very high, very unstable, and very rickety bridge at the local mill, realizes his mistake, abandons his plans of marriage to the other woman, and re-unites with Amina.
Jenny Lind and James Braid
In August 1847, the famous soprano Jenny Lind visited Manchester, and gave two performances as Amina. The outstanding difference between Lind and her contemporaries was that, "whilst the beauty of her voice was far greater than any other in living memory (thus, the Swedish Nightingale), what really set her apart was her outstanding ability to act"; and, moreover, in performing as Amina, rather than walking along a wide and well-protected walkway (as the others did), she routinely acrobatically balanced her way along narrow planks.[49]
While she was in Manchester—on the basis that, at the time, many characterized "hypnotism" as "artificial somnambulism",[50] and that, from a rather different perspective, her stage performance could also be described as one of "artificial" (rather than spontaneous) somnambulism—her friends arranged for her to visit the local surgeon James Braid, who had discovered hypnotism in 1841:[51][52]
- "Mr. Braid, surgeon, whose discoveries in hypnotism are well known, having invited the fair impersonator of a somnambulist to witness some of the abnormal feats of a real somnambulist, artificially thrown into that state, it was arranged that a private séance should take place [on Friday, 3 September 1847]." Manchester Guardian, 8 September 1847.
Drama
- The sleepwalking scene (Act V Scene 1) from William Shakespeare's tragic play Macbeth (1606) is one of the most famous scenes in all of literature.
- In Oulton's two act farce The Sleep-Walker; or, Which is the Lady (1812), "Somno", a histrionic failed-actor-turned-manservant relives his wished-for roles when sleepwalking.
Literature
- In Bram Stoker's novel Dracula the character Lucy Westenra is described as a sleepwalker. It is while sleepwalking that Count Dracula lures and attacks her.
Sleepwalking as a legal defense
Sleepwalking can sometimes result in injury, assault, or the death of someone else. Because these sleepwalking behaviours occur without volition, sleepwalking can be used as a legal defense.[53]
Alternative explanations, such as malingering and alcohol and drug-induced amnesia, need to be excluded. The differential diagnosis may also include other conditions in which violence related to sleep is a risk, such as REM Sleep Behavior Disorder (RSBD), fugue states, and episodic wandering."[54] In the 1963 case Bratty v Attorney-General for Northern Ireland, Lord Morris stated, "Each set of facts must require a careful examination of its own circumstances, but if by way of taking an illustration it were considered possible for a person to walk in his sleep and to commit a violent crime while genuinely unconscious, then such a person would not be criminally liable for that act."[55]
In the case of the law, an individual can be accused of non-insane automatism or insane automatism. The first is used as a defense for temporary insanity or involuntary conduct, resulting in acquittal. The latter results in a "special verdict of not guilty by reason of insanity."[56] This verdict of insanity can result in a court order to attend a mental institution.[57]
Other examples of legal cases involving sleepwalking in the defense include:
- 1846, Albert Tirrell used sleepwalking as a defense against charges of murdering Maria Bickford, a prostitute living in a Boston brothel.
- 1981, Steven Steinberg, of Scottsdale, Arizona was accused of killing his wife and acquitted on the grounds of temporary insanity.[58]
- 1991, R v Burgess: Burgess was accused of hitting his girlfriend on the head with a wine bottle and then a video tape recorder. Found not guilty, at Bristol Crown Court, by reason of insane automatism.[59]
- 1992, R. v. Parks: Parks was accused of killing his mother-in-law and attempting to kill his father-in-law. He was acquitted by the Supreme Court of Canada.[58]
- 1994, Pennsylvania v. Ricksgers: Ricksgers was accused of killing his wife. He was sentenced to life in prison without parole.[60]
- 1999, Arizona v. Falater: Falater, of Phoenix, Arizona, was accused of killing his wife. The court concluded that the murder was too complex to be committed while sleepwalking. Falater was convicted of first-degree murder and sentenced to life with no possibility of parole.[58]
- 2001, California v. Reitz: Stephen Reitz killed his lover, Eva Weinfurtner. He told police he had no recollection of the attack but he had "flashbacks" of believing he was in a scuffle with a male intruder. His parents testified in court that he had been a sleepwalker from childhood but the court was not convinced and convicted Reitz of first-degree murder in 2004.[60]
- 2008, Brian Thomas was accused of killing his wife while he dreamt she was an intruder, whilst on holiday in West Wales.[61] Thomas was found not guilty.[62]
References
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Version 2016. Geneva: World Health Organization.
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, D.C.: American Psychiatric Publishing.
- "I went driving and motorbiking in my sleep". BBC News. 2017-12-11. Retrieved 2020-02-27.
- SLEEP: Sex While Sleeping Is Real, and May Be No Joke, Michael Smith, MedPage Today Staff Writer, Published: June 19, 2006, access date 08-11-2011
- Swanson, Jenifer, ed. "Sleepwalking." Sleep Disorders Sourcebook. MI: Omnigraphics, 1999. 249–254, 351–352.
- "Sleepwalk to Murder". 10 October 2008. Archived from the original on 10 October 2008.CS1 maint: BOT: original-url status unknown (link)
- "CNN - 'Sleepwalker' convicted of murder". 25 June 1999. Retrieved 13 January 2015.
- Rachel Nowak (2004-10-15). "Sleepwalking woman had sex with strangers". New Scientist. Retrieved 2007-04-30.
- Lavie, Peretz, Atul Malhotra, and Giora Pillar. Sleep disorders : diagnosis, management and treatment : a handbook for clinicians. London: Martin Dunitz, 2002. 146–147.
- Stallman, HM (2017). "Assessment and treatment of sleepwalking in clinical practice". Australian Family Physician. 46 (8): 590–593. PMID 28787563.
- Schenck, Carlos H. Sleep: The Mysteries, The Problems, and The Solutions. New York: Avery/Penguin Group, 2007. Print.
- Guilleminault, Christian; Palombini, Luciana; Pelayo, Rafael; Chervin, Ronald D. (1 January 2003). "Sleepwalking and Sleep Terrors in Prepubertal Children: What Triggers Them?". Pediatrics. 111 (1): e17–e25. doi:10.1542/peds.111.1.e17. PMID 12509590 – via pediatrics.aappublications.org.
- "Sleep terrors (night terrors) - Symptoms and causes". Mayo Clinic. Retrieved 2019-03-25.
- Crisp, A.H.; Matthews, BM; Oakey, M; Crutchfield, M; et al. (1990). "Sleepwalking, night terrors, and consciousness". British Medical Journal. 300 (6721): 360–362. doi:10.1136/bmj.300.6721.360. PMC 1662124. PMID 2106985.
- Orme, J.E. (1967), "The Incidence of Sleepwalking in Various Groups", Acta Psychiatrica Scandinavica, Vol 43, Iss 3, pp 279–28.
- Milliet N, Ummenhofer W. Somnambulism and trauma: case report and short review of the literature. J Trauma. 1999;47(2):420–2
- Sillesen NH, Nielsen LT, Bonde C. Complex injuries associated with somnambulism. Ugeskr Laeger. 2010;172(50):3489–90
- "Sleepwalker dies after falling from hotel window following night out with work colleagues". 2014-01-03.
- "Tragedy as sleepwalker plunges to death from hotel window". 2014-01-02.
- "Naked sleepwalker stumbles out of city hotel then makes an odd request to police". 2016-05-22.
- "Sleep walker mows lawn naked". 2005-03-21.
- Pressman. "Factors that predispose, prime and precipitate NREM parasomnias in adults: clinical and forensic implications." Sleep Med Rev 11.1 (2007):5–30.
- Kales, A.; Soldatos, C. R.; Bixler, E. O.; Ladda, R. L.; Charney, D. S.; Weber, G.; Schweitzer, P. K. (1 August 1980). "Hereditary factors in sleepwalking and night terrors". The British Journal of Psychiatry. 137 (2): 111–118. doi:10.1192/bjp.137.2.111. PMID 7426840.
- Kucherenko, Mariya M.; Ilangovan, Vinodh; Herzig, Bettina; Shcherbata, Halyna R.; Bringmann, Henrik (2016-01-01). "TfAP-2 is required for night sleep in Drosophila". BMC Neuroscience. 17 (1): 72. doi:10.1186/s12868-016-0306-3. ISSN 1471-2202. PMC 5103423. PMID 27829368.
- "Neurology" Journal, January 4, 2011 76:12-13 published by the American Academy of Neurology www.Neurology.org
- Barabas, Gabor; Matthews, Wendy S.; Ferrari, Michael (2008). "Somnambulism in Children with Tourette Syndrome". Developmental Medicine & Child Neurology. 26 (4): 457–460. doi:10.1111/j.1469-8749.1984.tb04471.x. PMID 6148287.
- Schenck, C. H., & Mahowald, M. W. (1995b). Two cases of premenstrual sleep terrors and injurious sleep-walking. Journal of Psychosomatic Obstetrics & Gynecology, 16, 79–84.
- Hedman, C., Pohjasvaara, T., Tolonen, U., Salmivaara, A., & Myllyla, V. (2002). Parasomnias decline during pregnancy. Acta Neurologica Scandinavica, 105, 209–214.
- Stallman, HM; Kohler, M; White, J (February 2018). "Medication induced sleepwalking: A systematic review". Sleep Medicine Reviews. 37: 105–113. doi:10.1016/j.smrv.2017.01.005. PMID 28363449.
- Poryazova, R; Waldvogel, D; Bassetti, CL (October 2007). "Sleepwalking in patients with Parkinson disease". Archives of Neurology. 64 (10): 1524–7. doi:10.1001/archneur.64.10.1524. PMID 17923637.
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders – Third Edition (ICSD-3). Author.
- Wetherill, Reagan R.; Fromme, Kim (2016). "Alcohol-Induced Blackouts: A Review of Recent Clinical Research with Practical Implications and Recommendations for Future Studies". Alcoholism: Clinical and Experimental Research. 40 (5): 922–935. doi:10.1111/acer.13051. PMC 4844761. PMID 27060868.
- Hartzler, Bryan; Fromme, Kim (2003). "Fragmentary and en bloc blackouts: Similarity and distinction among episodes of alcohol-induced memory loss". Journal of Studies on Alcohol. 64 (4): 547–550. doi:10.15288/jsa.2003.64.547. PMID 12921196.
- Staff, Mayo Clinic. "Sleep-related Eating Disorders". Mayo Clinic. Retrieved 5 May 2014.
- Clinic, Cleveland. "Sleep-Related Eating Disorders". Cleveland Clinic. Retrieved 5 May 2014.
- Blatt, I., Peled, R., Gadoth, N., & Lavie, P. (1991). The value of sleep recording in evaluating somnambulism in young adults. Electroencephalography & Clinical Neurophysiology, 78, 407–412.
- Joncas, S., Zadra, A., Paquet, J., & Montplaisir, J. (2002). The value of sleep deprivation as a diagnostic tool in adult sleepwalkers. Neurology, 58, 936–940.
- Kales, A., Soldatos, C. R., Caldwell, A. B., Kales, J. D., Humphrey, F. J., 2nd, Charney, D. S., & Schweitzer, P. K. (1980). Somnambulism. Clinical characteristics and personality patterns. Archives of General Psychiatry, 37, 1406–1410.
- Hublin, C., Kaprio, J., Partinen, M., Heikkila, K., & Koskenvuo, M. (1997). Prevalence and genetics of sleepwalking: A population-based twin study. Neurology, 48, 177–181.
- Kavey, N. B., Whyte, J., Resor, S. R., Jr., & Gidro-Frank, S. (1990). Somnambulism in adults. Neurology, 40, 749–752.
- Zadra, Antonio; Pilon, Mathieu (2012-03-01). Parasomnias II. Oxford University Press. doi:10.1093/oxfordhb/9780195376203.013.0028.
- e.g., https://ilcaustralia.org.au/search_category_paths/636
- Stallman, HM; Kohler, M (2016). "Prevalence of Sleepwalking: A Systematic Review and Meta-Analysis". PLOS ONE. 11 (11): e0164769. Bibcode:2016PLoSO..1164769S. doi:10.1371/journal.pone.0164769. PMC 5104520. PMID 27832078.
- Kushida, Clete. 2012. Encyclopedia of Sleep.. Academic Press. p. 155. ISBN 1283895471.
- Society for Science & the Public. "Sleepwalking Cause." The Science News-Letter. 27 February 1954: 132.
- Society for Science & the Public. "Sleepwalker Not Dreaming." The Science News-Letter, 25 June 1966: 508
- "Electroencephalography", Medical Discoveries, 2009.
- "Somnambulism". International Dictionary of Psychoanalysis. 2005.
- Yeates, L.B., James Braid: Surgeon, Gentleman Scientist, and Hypnotist, Ph.D. Dissertation, School of History and Philosophy of Science, Faculty of Arts & Social Sciences, University of New South Wales, January 2013. Yeates (2013), p.788.
- For example, Pritchard J.C., A Treatise on Insanity and Other Disorders Affecting the Mind, Sherwood, Gilbert and Piper, (London), 1835, p.p.410.
- "Jenny Lind at the Manufacturing Establishments", Manchester Guardian, No.1947, (Saturday, 4 September 1847), p.7, col.C; "Jenny Lind and the Hypnotic Somnambulist", Manchester Guardian, No.1948, (Wednesday, 8 September 1847), p.5, col.F; "Jenny Lind and the Manchester Somnambulists", Newcastle Courant, No.9015, (Saturday, 17 September 1847), p.2, col.E; "Jenny Lind and Hypnotism", The Medical Times, Vol.16, No.416, (18 September 1847), p.602; and "Jenny Lind and Mesmerism", The Lady's Newspaper, No.39, (Saturday, 25 September 1847) p.294, col.A.
- Storer, H., "Jenny Lind and the Somnambulist", The Critic: A Journal for Readers, Authors, and Publishers, Vol.6, No.145, (9 October 1847), p.238; Braid, J., "(Letter to Dr. Storer, written on 28 September 1847)", The Critic: A Journal for Readers, Authors, and Publishers, Vol.6, No.145, (9 October 1847), p.238.
- Popat, S; Winslade, W (2015). "While You Were Sleepwalking: Science and Neurobiology of Sleep Disorders & the Enigma of Legal Responsibility of Violence During Parasomnia". Neuroethics. 8 (2): 203–214. doi:10.1007/s12152-015-9229-4. PMC 4506454. PMID 26203309.
- Culebras, Antonio. "Somnambulism." Clinical Handbook of Sleep Disorders, Massachusetts: Butterworth-Heinemann, 1996. 317–319.
- Mackay, Irene (1992). "The Sleepwalker is Not Insane". The Modern Law Review. 55 (5): 715–716. doi:10.1111/j.1468-2230.1992.tb02845.x.
- Canadian Legal Information Institute. R v. Parks. 1992.
- Lederman, Eliezer. "Non-Insane and Insane Automatism: Reducing the Significance of a Problematic Distinction." The International and Comparative Law Quarterly 34.4 (1985): 819.
- Martin, Lawrence. "Can sleepwalking be a murder defense?", 2009.
- Heaton-Armstrong A (Editor), Shepherd E (Editor), Wolchover D (Editor) (2002). Analysing Witness Testimony: Psychological, Investigative and Evidential Perspectives: A Guide for Legal Practitioners and Other Professionals. Blackstone Press. ISBN 978-1-85431-731-5.CS1 maint: multiple names: authors list (link) CS1 maint: extra text: authors list (link)
- Lyon, Lindsay. "7 Criminal Cases that Involved the 'Sleepwalking Defense.'", US News and World Report. May 2009.
- de Bruxelles, Simon (18 November 2009). "Sleepwalker Brian Thomas admits killing wife while fighting intruders in nightmare". The Times. London. Retrieved 2009-12-26.
- "Login".