Mucin
Mucins (/ˈmjuːsɪn/) are a family of high molecular weight, heavily glycosylated proteins (glycoconjugates) produced by epithelial tissues in most animals.[1] Mucins' key characteristic is their ability to form gels; therefore they are a key component in most gel-like secretions, serving functions from lubrication to cell signalling to forming chemical barriers.[1] They often take an inhibitory role.[1] Some mucins are associated with controlling mineralization, including nacre formation in mollusks,[2] calcification in echinoderms[3] and bone formation in vertebrates.[4] They bind to pathogens as part of the immune system. Overexpression of the mucin proteins, especially MUC1, is associated with many types of cancer.[5]
 | |
| Identifiers | |
|---|---|
| Symbol | Mucin |
| Membranome | 111 |
Although some mucins are membrane-bound due to the presence of a hydrophobic membrane-spanning domain that favors retention in the plasma membrane, most mucins are secreted as principal components of mucus by mucous membranes or are secreted to become a component of saliva.
Genes
At least 20 human mucin genes have been distinguished by cDNA cloning — MUC1, MUC2, MUC3A, MUC3B, MUC4, MUC5AC, MUC5B, MUC6, MUC7, MUC8, MUC12, MUC13, MUC15, MUC16, MUC17, MUC19, and MUC20.[6] A recently identified human mucin gene is MUC21, previously known as chromosome 6 open reading frame 205. The highly polymorphic[7] MUC22 is located near MUC21. The major secreted airway mucins are MUC5AC and MUC5B, while MUC2 is secreted mostly in the intestine but also in the airway.
Protein structure
Mature mucins are composed of two distinct regions:
- The amino- and carboxy-terminal regions are very lightly glycosylated, but rich in cysteines. The cysteine residues participate in establishing disulfide linkages within and among mucin monomers.
- A large central region formed of multiple tandem repeats of 10 to 80 residue sequences in which up to half of the amino acids are serine or threonine. This area becomes saturated with hundreds of O-linked oligosaccharides. N-linked oligosaccharides are also found on mucins, but in less abundance than O-linked sugars.
Function in humans
Mucins have been found to have important functions in defense against bacterial and fungal infections. MUC5B, the predominate mucin in the mouth and female genital tract, has been shown to significantly reduce attachment and biofilm formation of Streptococcus mutans, a bacteria with the potential to form cavities.[8] Unusually, MUC5B does not kill the bacteria but rather maintains it in the planktonic (non-biofilm) phase, thus maintaining a diverse and healthy oral microbiome.[8] Similar effects of MUC5B and other mucins have been demonstrated with other pathogens, such as Candida albicans, Helicobacter pylori, and even HIV.[9][10] In the mouth, mucins can also recruit anti-microbial proteins such as statherins and histatine 1, which further reduces risk of infection.[10]
Glycosylation and aggregation
Mucin genes encode mucin monomers that are synthesized as rod-shape apomucin cores that are post-translationally modified by exceptionally abundant glycosylation.
The dense "sugar coating" of mucins gives them considerable water-holding capacity and also makes them resistant to proteolysis, which may be important in maintaining mucosal barriers.
Mucins are secreted as massive aggregates of proteins with molecular masses of roughly 1 to 10 million Da. Within these aggregates, monomers are linked to one another mostly by non-covalent interactions, although intermolecular disulfide bonds may also play a role in this process.
Secretion
Upon stimulation, MARCKS (myristylated alanine-rich C kinase substrate) protein coordinates the secretion of mucin from mucin-filled vesicles within the specialized epithelial cells.[11] Fusion of the vesicles to the plasma membrane causes release of the mucin, which as it exchanges Ca2+ for Na+ expands up to 600 fold. The result is a viscoelastic product of interwoven molecules which, combined with other secretions (e.g., from the airway epithelium and the submucosal glands in the respiratory system), is called mucus.[12] [13]
Clinical significance
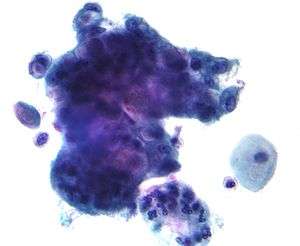
Increased mucin production occurs in many adenocarcinomas, including cancers of the pancreas, lung, breast, ovary, colon and other tissues. Mucins are also overexpressed in lung diseases such as asthma, bronchitis, chronic obstructive pulmonary disease (COPD) or cystic fibrosis.[14] Two membrane mucins, MUC1 and MUC4 have been extensively studied in relation to their pathological implication in the disease process.[15][16][17] Mucins are under investigation as possible diagnostic markers for malignancies and other disease processes in which they are most commonly over- or mis-expressed.
Abnormal deposits of mucin are responsible for the non-pitting facial edema seen in untreated hypothyroidism. This edema is seen in the pretibial area as well.[18]
See also
- Bovine submaxillary mucin coatings
- Verotoxin-producing Escherichia coli
References
- Marin F, Luquet G, Marie B, Medakovic D (2007). Molluscan shell proteins: primary structure, origin, and evolution. Current Topics in Developmental Biology. 80. pp. 209–76. doi:10.1016/S0070-2153(07)80006-8. ISBN 9780123739148. PMID 17950376.
- Marin F, Corstjens P, de Gaulejac B, de Vrind-De Jong E, Westbroek P (July 2000). "Mucins and molluscan calcification. Molecular characterization of mucoperlin, a novel mucin-like protein from the nacreous shell layer of the fan mussel Pinna nobilis (Bivalvia, pteriomorphia)". The Journal of Biological Chemistry. 275 (27): 20667–75. doi:10.1074/jbc.M003006200. PMID 10770949.
- Boskey AL (2003). "Biomineralization: an overview". Connective Tissue Research. 44 Suppl 1 (1): 5–9. doi:10.1080/713713622. PMID 12952166.
- Midura RJ, Hascall VC (October 1996). "Bone sialoprotein--a mucin in disguise?". Glycobiology. 6 (7): 677–81. doi:10.1093/glycob/6.7.677. PMID 8953277.
- Niv Y (April 2008). "MUC1 and colorectal cancer pathophysiology considerations". World Journal of Gastroenterology. 14 (14): 2139–41. doi:10.3748/wjg.14.2139. PMC 2703837. PMID 18407586.
- Perez-Vilar J, Hill RL (2004). "Mucin Family of Glycoproteins". Encyclopedia of Biological Chemistry (Lennarz & Lane, EDs.). Oxford: Academic Press/Elsevier. 2: 758–764. doi:10.1016/B0-12-443710-9/00411-7. ISBN 9780124437104.
- Norman PJ, Norberg SJ, Guethlein LA, Nemat-Gorgani N, Royce T, Wroblewski EE, Dunn T, Mann T, Alicata C, Hollenbach JA, Chang W, Shults Won M, Gunderson KL, Abi-Rached L, Ronaghi M, Parham P (May 2017). "II". Genome Research. 27 (5): 813–823. doi:10.1101/gr.213538.116. PMC 5411776. PMID 28360230.
- Frenkel, Erica Shapiro; Ribbeck, Katharina (2014-10-24). "Salivary Mucins Protect Surfaces from Colonization by Cariogenic Bacteria". Applied and Environmental Microbiology. 81 (1): 332–338. doi:10.1128/aem.02573-14. ISSN 0099-2240. PMC 4272720. PMID 25344244.
- Kavanaugh, Nicole L.; Zhang, Angela Q.; Nobile, Clarissa J.; Johnson, Alexander D.; Ribbeck, Katharina (2014-11-11). Berman, Judith (ed.). "Mucins Suppress Virulence Traits of Candida albicans". mBio. 5 (6): e01911-14. doi:10.1128/mBio.01911-14. ISSN 2150-7511. PMC 4235211. PMID 25389175.
- Frenkel, Erica Shapiro; Ribbeck, Katharina (January 2015). "Salivary mucins in host defense and disease prevention". Journal of Oral Microbiology. 7 (1): 29759. doi:10.3402/jom.v7.29759. ISSN 2000-2297. PMC 4689954. PMID 26701274.
- Li Y, Martin LD, Spizz G, Adler KB (November 2001). "MARCKS protein is a key molecule regulating mucin secretion by human airway epithelial cells in vitro". The Journal of Biological Chemistry. 276 (44): 40982–90. doi:10.1074/jbc.M105614200. PMID 11533058.
- Rogers DF (September 2007). "Physiology of airway mucus secretion and pathophysiology of hypersecretion". Respiratory Care. 52 (9): 1134–46, discussion 1146–9. PMID 17716382.
- Perez-Vilar J (February 2007). "Mucin granule intraluminal organization". American Journal of Respiratory Cell and Molecular Biology. 36 (2): 183–90. doi:10.1165/rcmb.2006-0291TR. PMC 2176109. PMID 16960124.
- Morrison CB, Markovetz MR, Ehre C (November 2019). "Mucus, Mucins, and Cystic Fibrosis". Pediatr Pulmonol. 54 (Suppl 3): S84–S96. doi:10.1002/ppul.24530. PMID 31715083.
- Singh AP, Moniaux N, Chauhan SC, Meza JL, Batra SK (January 2004). "Inhibition of MUC4 expression suppresses pancreatic tumor cell growth and metastasis". Cancer Research. 64 (2): 622–30. doi:10.1158/0008-5472.CAN-03-2636. PMID 14744777.
- Singh AP, Chauhan SC, Bafna S, Johansson SL, Smith LM, Moniaux N, Lin MF, Batra SK (March 2006). "Aberrant expression of transmembrane mucins, MUC1 and MUC4, in human prostate carcinomas". The Prostate. 66 (4): 421–9. doi:10.1002/pros.20372. PMID 16302265.
- Singh AP, Chaturvedi P, Batra SK (January 2007). "Emerging roles of MUC4 in cancer: a novel target for diagnosis and therapy". Cancer Research. 67 (2): 433–6. doi:10.1158/0008-5472.CAN-06-3114. PMID 17234748.
- Hanberg, Allen "Medical Surgical Nursing: clinical management for positive outcomes" Black and Hawk (Eds.). ElSevier 2009.
Further reading
- Ali MS, Hutton DA, Wilson JA, Pearson JP (September 2005). "Major secretory mucin expression in chronic sinusitis". Otolaryngology–Head and Neck Surgery. 133 (3): 423–8. doi:10.1016/j.otohns.2005.06.005. PMID 16143194.
- Ramsey KA, Rushton ZL, Ehre C (June 2016). "Mucin Agarose Gel Electrophoresis: Western Blotting for High-Molecular-Weight Glycoproteins". J Vis Exp. 112: 54153. doi:10.3791/54153. PMC 4927784. PMID 27341489.
External links
- Mucins at the US National Library of Medicine Medical Subject Headings (MeSH)
- "Mucin" at Dorland's Medical Dictionary