Knee replacement
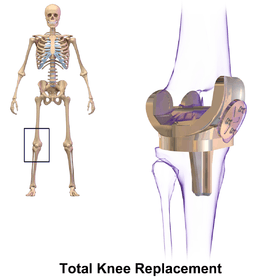
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability. It is most commonly performed for osteoarthritis,[1] and also for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement
| Knee replacement | |
|---|---|
 Knee replacement | |
| Other names | Knee arthroplasty |
| ICD-10-PCS | 0SRD0JZ |
| ICD-9-CM | 81.54 |
| MeSH | D019645 |
| MedlinePlus | 002974 |
| eMedicine | 1250275 |
Other major causes of debilitating pain include meniscus tears, cartilage defects, and ligament tears. Debilitating pain from osteoarthritis is much more common in the elderly.
Knee replacement surgery can be performed as a partial or a total knee replacement.[2] In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
The operation typically involves substantial postoperative pain, and includes vigorous physical rehabilitation. The recovery period may be 12 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility.[3] It is estimated that approximately 82% of total knee replacements will last 25 years.[4]
Medical uses



Knee replacement surgery is most commonly performed in people with advanced osteoarthritis and should be considered when conservative treatments have been exhausted.[5] Total knee replacement is also an option to correct significant knee joint or bone trauma in young patients. Similarly, total knee replacement can be performed to correct mild valgus or varus deformity. Serious valgus or varus deformity should be corrected by osteotomy. Physical therapy has been shown to improve function and may delay or prevent the need for knee replacement. Pain is often noted when performing physical activities requiring a wide range of motion in the knee joint.[6]
Pre-operative preparation
 |
Angles commonly measured before knee replacement surgery: |
To indicate knee replacement in case of osteoarthritis, its radiographic classification and severity of symptoms should both be substantial. Such radiography should consist of weightbearing X-rays of both knees- AP, Lateral, and 30 degrees of flexion. AP and lateral views may not show joint space narrowing, but the 30 degree flexion view is most sensitive for narrowing. Full length projections are also used in order to adjust the prosthesis to provide a neutral angle for the distal lower extremity. Two angles used for this purpose are:
- Hip-knee-shaft angle (HKS),[7] an angle formed between a line through the longitudinal axis of the femoral shaft and its mechanical axis, which is a line from the center of the femoral head to the intercondylar notch of the distal femur.[9]
- Hip-knee-ankle angle (HKA),[8] which is an angle between the femoral mechanical axis and the center of the ankle joint.[9] It is normally between 1.0° and 1.5° of varus in adults.[10]
The patient is to perform range of motion exercises and hip, knee and ankle strengthening as directed daily. Before the surgery is performed, pre-operative tests are done: usually a complete blood count, electrolytes, APTT and PT to measure blood clotting, chest X-rays, ECG, and blood cross-matching for possible transfusion. About a month before the surgery, the patient may be prescribed supplemental iron to boost the hemoglobin in their blood system. Accurate X-rays of the affected knee are needed to measure the size of components which will be needed. Medications such as warfarin and aspirin will be stopped some days before surgery to reduce the amount of bleeding. Patients may be admitted on the day of surgery if the pre-op work-up is done in the pre-anesthetic clinic or may come into hospital one or more days before surgery. Currently there is insufficient quality evidence to support the use of pre-operative physiotherapy in older adults undergoing total knee arthroplasty.[11]
Preoperative education is currently an important part of patient care. There is some evidence that it may slightly reduce anxiety before knee replacement surgery, with low risk of detrimental effects.[12]
Weight loss surgery before a knee replacement does not appear to change outcomes.[13]
Technique
The surgery involves exposure of the front of the knee, with detachment of part of the quadriceps muscle (vastus medialis) from the patella. The patella is displaced to one side of the joint, allowing exposure of the distal end of the femur and the proximal end of the tibia. The ends of these bones are then accurately cut to shape using cutting guides oriented to the long axis of the bones. The cartilages and the anterior cruciate ligament are removed; the posterior cruciate ligament may also be removed but the tibial and fibular collateral ligaments are preserved.[14] Whether the posterior cruciate ligament is removed or preserved depends on the type of implant used, although there appears to be no clear difference in knee function or range of motion favouring either approach.[15] Metal components are then impacted onto the bone or fixed using polymethylmethacrylate (PMMA) cement. Alternative techniques exist that affix the implant without cement. These cement-less techniques may involve osseointegration, including porous metal prostheses. Finally, stability and range of motion is checked, followed by irrigation, hemostasis, placement of hemovacs, and closure.[16]
Femoral replacement
A round ended implant is used for the femur, mimicking the natural shape of the joint. On the tibia the component is flat, although it sometimes has a stem which goes down inside the bone for further stability. A flattened or slightly dished high-density polyethylene surface is then inserted onto the tibial component so that the weight is transferred metal to plastic not metal to metal. During the operation any deformities must be corrected, and the ligaments balanced so that the knee has a good range of movement and is stable and aligned. In some cases the articular surface of the patella is also removed and replaced by a polyethylene button cemented to the posterior surface of the patella. In other cases, the patella is replaced unaltered.

Technology
In recent years, that has been an increase in technology assistance with implantation of total knee replacements. Traditionally, knee replacements were performed utilizing mechanical jigs, not unlike those used in carpentry. These mechanical jigs rely on vision and human judgement. Using computer assistance to provide navigation, navigated knee replacements provide assistance in more accurate placement of implanted knee replacements based on mechanical axis. While these implants are placed more accurately, there has not been much improvement in long-term outcomes.[17] Similarly, sensor-based guidance provides accurate feedback to demonstrate soft-tissue tension to assist in guidance of insertion of knee replacements.[18] Robotic-assisted knee replacements take into account both mechanical axis and soft-tissue balancing in order to assist the surgeon in placement of a knee replacement. Short-term outcomes of robotic-assisted knee replacements are promising.[19]
Post-operative pain control
The regional analgesia techniques (neuraxial anesthesia or continuous femoral nerve block[20] or adductor canal block) are used most commonly.[21] Local anesthesia infiltration in the pericapsular area using liposomal bupivacaine provides good analgesia in the post-operative period without increasing the risk for instability or nerve injury.[22] A combined approach of local infiltration analgesia and femoral nerve block to achieve multimodal analgesia is common.
Controversies in Total Knee Replacement
Cemented and CementlessTotal Knee Replacement
The femoral, tibial and patella components of a total knee replacement are fixed to the bone by either using cement or cementless total knee replacement implants. Cemented fixation is performed on the vast majority of total knee replacements performed However, short-term trials suggest that there may be relief of pain.[23] There are concerns regarding tibial loosening after implantation, prohibiting widespread adoptation of cementless knee replacements at this time.[24]
Denervation of the Patella
There is debate regarding denervating the patella. Anterior knee pain is thought to be related to the association of the patella and femoral component. Some surgeons believe that by using electrocautery to denervate the patella, it reduces the chance of anterior knee pain postoperatively.[25][26]
Patella Resurfacing
Many surgeons in the USA perform patella resurfacing routinely, while many surgeons in Asia and Europe do not. Patella resurfacing is performed by removing the cartilage from the surface of the knee and replacing it with polyethylene. Surgeons who do not routinely resurface the patella do not believe that it is a significant contribution to pain when there is no evidence of arthritis to the patellofemoral joint. Some surgeons believe it is not cost-effective to routinely resurface the kneecap and that routine patella resurfacing may lead to increased complications such as patella fracture.[27] Other surgeons are concerned that patients with an unresurfaced patella may have increased pain postoperatively. A meta-analysis evaluating outcomes following patella resurfacing found that routine resurfacing more reliably relieves patient's pain.[28]
Tibia Polyethylene Component
Polyethylene is the plastic component that is inserted between the femoral and tibial components. There are several different polyethylene designs that have been published on in recent years, including Posterior Stabilized (PS), Cruciate Retaining (CR), Bi-Cruciate Retaining (BCR), and Medial Congruent (MC) and mobile bearing.
Cruciate Retaining vs Posterior Cruciate Ligament Sacrificing
The posterior cruciate ligament (PCL) is important to the stability of the knee by preventing posterior subluxation of the tibia, reducing shear stress, increasing flexion and lever arm of the extensor mechanism by inducing femoral rollback upon flexion, and thus minimizing polyethylene abrasion through reducing stress applied to the articular surface.[29][29][29][29] The PS implant uses a post that is built into the implant to accommodate for the loss of PCL. Proponents of retaining the PCL advise that it is difficult to balance a CR knee and un-natural physiologic loads may increase wear of the polyethylene.[29] Multiple studies have demonstrated minimal to no difference between the two designs.[29][29][30]
Medial Congruent Polyethylene and Bicruciate Retaining
Advocates of MC and BCR knee replacements are looking in opposite directions by either decreasing motion or increasing motion of the total knee respectively. MC knee replacements attempt to mimic a more natural knee motion by decreasing motion on the medial aspect of the knee and allowing for increased motion on the lateral aspect of the joint. This mimics the external rotation and abduction of the tibia that is seen during normal ambulation. Several studies have shown improved gait profiles, but long-term studies are needed to demonstrate improved results.[31][32] Conversely, the BCR knee retains the Anterior and Posterior Cruciate Ligaments to try to mimic the normal tension of ligaments of the knee. Concerns of problems of increased revisions led to some designs being pulled from the market.[33]
Mobile Bearing
A mobile bearing design allows for free motion of the polyethylene within the tibial component. Other component designs meanwhile are fixed to the tibia and only articulate at the femur and polyethylene junction.[34] There is no strong evidence that this approach improves knee function, mortality, adverse events, or amount of pain compared to a fixed bearing approach for total knee replacement.[34] Mobile bearing designs are important to ensuring decreased wear rates in hinged knee arthroplasty.[35]
Minimally Invasive Total Knee Replacement
Minimally invasive procedures have been developed in total knee replacement that do not cut the quadriceps tendon. There are different definitions of minimally invasive knee surgery, which may include a shorter incision length, retraction of the patella without eversion (rotating out), and specialized instruments. There are few randomized trials, but studies have found less postoperative pain, shorter hospital stays, and shorter recovery. However, no studies have shown long-term benefits.[3]
Partial knee replacement
Unicompartmental arthroplasty (UKA), also called partial knee replacement, is an option for some people. The knee is generally divided into three "compartments": medial, lateral, and patellofemoral. Most people with arthritis severe enough to consider knee replacement have significant wear in two or more of the above compartments, and are treated with total knee replacement (TKA). A minority of people with osteoarthritis have wear primarily in one compartment, usually the medial, and may be candidates for unicompartmental knee replacement. Advantages of UKA compared to TKA include smaller incision, easier post-op rehabilitation, better postoperative range of motion, shorter hospital stay, less blood loss, lower risk of infection, stiffness, and blood clots, but a harder revision if necessary. Persons with infectious or inflammatory arthritis (rheumatoid arthritis, lupus, psoriasis), or marked deformity are not candidates for this procedure.[36]
Many studies demonstrate higher revision rates associated with partial knee replacements. There is significant variation in revision rates depending on implant design and implantation technique.[37]
Components and zones

Standardized zones around the components are used for specifying for example signs of loosening on radiographic follow-up. There are various classification systems for specifying such zones,[39][40] including by KS (Knee Society) zones published in 2015.[38]
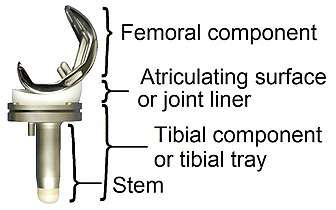 Main components of a knee prosthesis.
Main components of a knee prosthesis. KS zones, anteroposterior (AP) view.[38]
KS zones, anteroposterior (AP) view.[38]
Specific KS zones are as follows, with * meaning that the zone can be specified as "A" (anterior), "P" (posterior), "M" (medial) or "L" (lateral):[38]
- Femoral component (lateral view)
- Zone 1 and 2: Anterior and posterior flange, respectively.
- Zone 3: Central box/distal fixation region, where "A" and "P" designate the respective chamfers if visible*
- Zone 4: Stem extension*
- Zone 5: Stem
- Tibial component:
- Zone 1: Anterior on lateral view, medial on anteroposterior (AP) view.
- Zone 2: Posterior on lateral view, lateral on AP view.
- Zone 3: Central keel/stem/peg fixation region*
- Zone 4: Stem extension*
- Zone 5: Inferior aspect of keel or stem
Risks
Risks and complications in knee replacement[41] are similar to those associated with all joint replacements. The most serious complication is infection of the joint, which occurs in <1% of patients. Risk factors for infection are related to both patient and surgical factors.[42] Deep vein thrombosis occurs in up to 15% of patients, and is symptomatic in 2–3%. Nerve injuries occur in 1–2% of patients. Persistent pain or stiffness occurs in 8–23% of patients. Prosthesis failure occurs in approximately 2% of patients at 5 years.[3]
There is increased risk of complications for obese people going through total knee replacement.[43] The morbidly obese should be advised to lose weight before surgery and, if medically eligible, would probably benefit from bariatric surgery.[44]
Fracturing or chipping of the polyethylene platform between the femoral and tibial components may be of concern. These fragments may become lodged in the knee and create pain or may move to other parts of the body. Advancements in implant design have greatly reduced these issues but the potential for concern is still present over the lifespan of the knee replacement.
Deep vein thrombosis
According to the American Academy of Orthopedic Surgeons (AAOS), deep vein thrombosis in the leg is "the most common complication of knee replacement surgery... prevention... may include periodic elevation of patient's legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood."[2]
Fractures
Periprosthetic fractures are becoming more frequent with the aging patient population and can occur intraoperatively or postoperatively. Depending on the location of the fracture and the stability of the prosthesis, these can be treated surgically with open reduction and internal fixation or revision of the prosthesis.
Loss of motion
The knee at times may not recover its normal range of motion (0–135 degrees usually) after total knee replacement. Much of this is dependent on pre-operative function. Most patients can achieve 0–110 degrees, but stiffness of the joint can occur. In some situations, manipulation of the knee under anesthetic is used to reduce post operative stiffness. There are also many implants from manufacturers that are designed to be "high-flex" knees, offering a greater range of motion.
Instability
In some patients, the kneecap dislocates to the outer side of the knee after surgery. This is painful and usually needs to be treated by surgery to realign the kneecap. However, this is quite rare.
Loosening
Loosening of the prosthesis can be indicated on X-ray by thin radiolucent spaces around the implant, or more obviously by implant displacement.[45]
Infection
The current classification of AAOS divides prosthetic infections into four types.[46]
- Type 1 (positive intraoperative culture): Two positive intraoperative cultures
- Type 2 (early postoperative infection): Infection occurring within first month after surgery
- Type 3 (acute hematogenous infection): Hematogenous seeding of site of previously well-functioning prosthesis
- Type 4 (late chronic infection): Chronic indolent clinical course; infection present for more than a month
While it is relatively rare, periprosthetic infection remains one of the most challenging complications of joint arthroplasty. A detailed clinical history and physical remain the most reliable tool to recognize a potential periprosthetic infection. In some cases the classic signs of fever, chills, painful joint, and a draining sinus may be present, and diagnostic studies are simply done to confirm the diagnosis. In reality though, most patients do not present with those clinical signs, and in fact the clinical presentation may overlap with other complications such as aseptic loosening and pain. In those cases diagnostic tests can be useful in confirming or excluding infection.

Modern diagnosis of infection around a total knee replacement is based on the Musculoskeletal Infection Society (MSIS) criteria.[47] They are:
1. There is a sinus tract communicating with the prosthesis; or 2. A pathogen is isolated by culture from at least two separate tissue or fluid samples obtained from the affected prosthetic joint; or
Four of the following six criteria exist:
1.Elevated serum erythrocyte sedimentation rate (ESR>30mm/hr) and serum C-reactive protein (CRP>10 mg/L) concentration,
2.Elevated synovial leukocyte count,
3.Elevated synovial neutrophil percentage (PMN%),
4.Presence of purulence in the affected joint,
5.Isolation of a microorganism in one culture of periprosthetic tissue or fluid, or
6. Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at ×400 magnification.
None of the above laboratory tests has 100% sensitivity or specificity for diagnosing infection. Specificity improves when the tests are performed in patients in whom clinical suspicion exists. ESR and CRP remain good 1st line tests for screening (high sensitivity, low specificity). Aspiration of the joint remains the test with the highest specificity for confirming infection.
The choice of treatment depends on the type of prosthetic infection.[48]
- Positive intraoperative cultures: Antibiotic therapy alone
- Early post-operative infections: debridement, antibiotics, and retention of prosthesis.
- Acute hematogenous infections: debridement, antibiotic therapy, retention of prosthesis.
- Late chronic: delayed exchange arthroplasty. Surgical débridement and parenteral antibiotics alone in this group has limited success, and standard of care involves exchange arthroplasty.[49]
Appropriate antibiotic doses can be found at the following instructional course lecture by AAOS[46]
Post-operative evaluation

Knee replacement is routinely evaluated by X-ray, including the following measures:

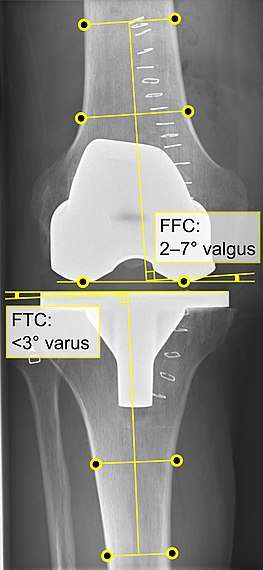 - FFC: frontal femoral component angle. It is typically regarded as optimal when being 2–7° in valgus.[52]
- FFC: frontal femoral component angle. It is typically regarded as optimal when being 2–7° in valgus.[52]
- FTC: frontal tibial component angle, which is regarded as optimal when being at a right angle. A varus position of more than 3° has generally been found to increase the failure rate of the prosthesis.[52]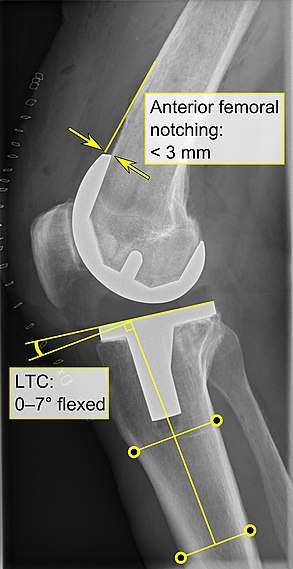 - Anterior femoral notching (the femoral component causing reduced thickness of the distal femur anteriorly), seems to cause an increased risk of fractures when exceeding about 3 mm.[53]
- Anterior femoral notching (the femoral component causing reduced thickness of the distal femur anteriorly), seems to cause an increased risk of fractures when exceeding about 3 mm.[53]
- LTC: lateral (or sagittal) tibial component angle, which is ideally positioned so that the tibia is 0–7° flexed compared to at a right angle with the tibial plate.[52]
Post-operative rehabilitation
The length of post-operative hospitalization is 5 days on average depending on the health status of the patient and the amount of support available outside the hospital setting.[54] Protected weight bearing on crutches or a walker is required until specified by the surgeon[55] because of weakness in the quadriceps muscle[56] In the immediate post-operative period, up to 39% of knee replacement patients experience inadequate pain control.[57]
To increase the likelihood of a good outcome after surgery, multiple weeks of physical therapy is necessary. In these weeks, the therapist will help the patient return to normal activities, as well as prevent blood clots, improve circulation, increase range of motion, and eventually strengthen the surrounding muscles through specific exercises. Whether techniques such as neuromuscular electrical stimulation are effective at promoting gains in knee muscle strength after surgery are unclear.[58] Often range of motion (to the limits of the prosthesis) is recovered over the first two weeks (the earlier the better). Over time, patients are able to increase the amount of weight bearing on the operated leg, and eventually are able to tolerate full weight bearing with the guidance of the physical therapist.[55] After about ten months, the patient should be able to return to normal daily activities, although the operated leg may be significantly weaker than the non-operated leg.[56]
For post-operative knee replacement patients, immobility is a factor precipitated by pain and other complications. Mobility is known as an important aspect of human biology that has many beneficial effects on the body system.[59] It is well documented in literature that physical immobility affects every body system and contributes to functional complications of prolonged illness.[60] In most medical-surgical hospital units that perform knee replacements, ambulation is a key aspect of nursing care that is promoted to patients. Early ambulation can decrease the risk of complications associated with immobilization such as pressure ulcers, deep vein thrombosis (DVT), impaired pulmonary function, and loss of functional mobility.[61] Nurses’ promotion and execution of early ambulation on patients has found that it greatly reduces the complications listed above, as well as decreases length of stay and costs associated with further hospitalization.[61] Nurses may also work with teams such as physical therapy and occupational therapy to accomplish ambulation goals and reduce complications.[62]
Continuous passive motion (CPM) is a postoperative therapy approach that uses a machine to move the knee continuously through a specific range of motion, with the goal of preventing joint stiffness and improving recovery.[63][64] There is no evidence that CPM therapy leads to a clinically significant improvement in range of motion, pain, knee function, or quality of life.[64] CPM is inexpensive, convenient, and assists patients in therapeutic compliance. However, CPM should be used in conjunction with traditional physical therapy.[63] In unusual cases where the person has a problem which prevents standard mobilization treatment, then CPM may be useful.[63]
Cryotherapy, also known as 'cold therapy' is sometimes recommended after surgery for pain relief and to limit swelling of the knee. Cryotherapy involves the application of ice bags or cooled water to the skin of the knee joint. However, the evidence that cryotherapy reduces pain and swelling is very weak and the benefits after total knee replacement surgery have been shown to be very small.[65]
Some physicians and patients may consider having ultrasonography for deep venous thrombosis after knee replacement.[66] However, this kind of screening should be done only when indicated because to perform it routinely would be unnecessary health care.[66] If a medical condition exists that could cause deep vein thrombosis, a physician can choose to treat patients with cryotherapy and intermittent pneumatic compression as a preventive measure.
Neither gabapentin nor pregabalin have been found to be useful for pain following a knee replacement.[67] A Cochrane review concluded that early multidisciplinary rehabilitation programs may produce better results at the rate of activity and participation.[68]
Frequency
With 718,000 hospitalizations, knee arthroplasty accounted for 4.6% of all United States operating room procedures in 2011—making it one of the most common procedures performed during hospital stays.[69][70] The number of knee arthroplasty procedures performed in U.S. hospitals increased 93% between 2001 and 2011.[71] A study of United States community hospitals showed that in 2012, among hospitalizations that involved an OR procedure, knee arthroplasty was the OR procedure performed most frequently during hospital stays paid by Medicare (10.8 percent of stays) and by private insurance (9.1 percent). Knee arthroplasty was not among the top five most frequently performed OR procedures for stays paid by Medicaid or for uninsured stays.[72]
By 2030, the demand for primary total knee arthroplasty is projected to increase to 3.48 million surgeries performed annually in the U.S.[73]
See also
- Autologous chondrocyte implantation
- Microfracture surgery
- Knee osteoarthritis
- Osseointegration
- Meniscus transplant
References
- Simon H Palmer (27 June 2012). "Total Knee Arthroplasty". Medscape Reference.
- "Total Knee Replacement". American Academy of Orthopedic Surgeons. December 2011.
- Leopold SS (April 2009). "Minimally invasive total knee arthroplasty for osteoarthritis". N. Engl. J. Med. 360 (17): 1749–58. doi:10.1056/NEJMct0806027. PMID 19387017.
- Evans, Jonathan T; Walker, Robert W; Evans, Jonathan P; Blom, Ashley W; Sayers, Adrian; Whitehouse, Michael R (February 2019). "How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up". The Lancet. 393 (10172): 655–663. doi:10.1016/S0140-6736(18)32531-5. PMC 6381229. PMID 30782341.
- Van Manen, MD; Nace, J; Mont, MA (November 2012). "Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners". The Journal of the American Osteopathic Association. 112 (11): 709–715. PMID 23139341.
- Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC (February 2000). "Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial". Ann. Intern. Med. 132 (3): 173–81. doi:10.7326/0003-4819-132-3-200002010-00002. PMID 10651597.
- Cooke TD, Sled EA, Scudamore RA (2007). "Frontal plane knee alignment: a call for standardized measurement". J Rheumatol. 34 (9): 1796–801. PMID 17787049.
- W-Dahl, Annette; Toksvig-Larsen, Sören; Roos, Ewa M (2009). "Association between knee alignment and knee pain in patients surgically treated for medial knee osteoarthritis by high tibial osteotomy. A one year follow-up study". BMC Musculoskeletal Disorders. 10 (1): 154. doi:10.1186/1471-2474-10-154. ISSN 1471-2474. PMC 2796991. PMID 19995425.
- Cherian, Jeffrey J.; Kapadia, Bhaveen H.; Banerjee, Samik; Jauregui, Julio J.; Issa, Kimona; Mont, Michael A. (2014). "Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications". Current Reviews in Musculoskeletal Medicine. 7 (2): 89–95. doi:10.1007/s12178-014-9218-y. ISSN 1935-973X. PMC 4092202. PMID 24671469.
- Sheehy, L.; Felson, D.; Zhang, Y.; Niu, J.; Lam, Y.-M.; Segal, N.; Lynch, J.; Cooke, T.D.V. (2011). "Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study". Osteoarthritis and Cartilage. 19 (1): 58–64. doi:10.1016/j.joca.2010.09.011. ISSN 1063-4584. PMC 3038654. PMID 20950695.
- Chesham, Ross Alexander; Shanmugam, Sivaramkumar (13 October 2016). "Does preoperative physiotherapy improve postoperative, patient-based outcomes in older adults who have undergone total knee arthroplasty? A systematic review". Physiotherapy Theory and Practice. 33 (1): 9–30. doi:10.1080/09593985.2016.1230660. PMID 27736286. S2CID 23316275.
- McDonald, S; Page, MJ; Beringer, K; Wasiak, J; Sprowson, A (13 May 2014). "Preoperative education for hip or knee replacement". The Cochrane Database of Systematic Reviews (5): CD003526. doi:10.1002/14651858.CD003526.pub3. PMC 7154584. PMID 24820247.
- Smith, TO; Aboelmagd, T; Hing, CB; MacGregor, A (September 2016). "Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? Systematic review and meta-analysis" (PDF). The Bone & Joint Journal. 98-B (9): 1160–6. doi:10.1302/0301-620x.98b9.38024. PMID 27587514.
- Verra, Wiebe C.; van den Boom, Lennard G. H.; Jacobs, Wilco; Clement, Darren J.; Wymenga, Ate A. B.; Nelissen, Rob G. H. H. (11 October 2013). "Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis". The Cochrane Database of Systematic Reviews (10): CD004803. doi:10.1002/14651858.CD004803.pub3. ISSN 1469-493X. PMC 6599815. PMID 24114343.
- Verra, WC; van den Boom, LG; Jacobs, W; Clement, DJ; Wymenga, AA; Nelissen, RG (11 October 2013). "Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis". The Cochrane Database of Systematic Reviews (10): CD004803. doi:10.1002/14651858.CD004803.pub3. PMC 6599815. PMID 24114343.
- Scott MD R. Posterior cruciate-retaining total knee arthroplasty. J Med Ins. 2017;2017(20). doi:https://doi.org/10.24296/jomi/20
- Picard, Frederic; Deep, Kamal; Jenny, Jean Yves (November 2016). "Current state of the art in total knee arthroplasty computer navigation". Knee Surgery, Sports Traumatology, Arthroscopy. 24 (11): 3565–3574. doi:10.1007/s00167-016-4337-1. ISSN 1433-7347. PMID 27704159. S2CID 2627370.
- Chow, Jimmy; Law, Tsun Yee; Roche, Martin (2018). "Sensor-Based Soft Tissue Balancing in Total Knee Arthroplasty". Advances in Experimental Medicine and Biology. 1093: 327–334. doi:10.1007/978-981-13-1396-7_25. ISBN 978-981-13-1395-0. ISSN 0065-2598. PMID 30306492.
- Khlopas, Anton; Sodhi, Nipun; Sultan, Assem A.; Chughtai, Morad; Molloy, Robert M.; Mont, Michael A. (July 2018). "Robotic Arm-Assisted Total Knee Arthroplasty". The Journal of Arthroplasty. 33 (7): 2002–2006. doi:10.1016/j.arth.2018.01.060. ISSN 1532-8406. PMID 29506926.
- Toftdahl, K; Nikolajsen, L; Haraldsted, V; Madsen, F; Tønnesen, EK; Søballe, K (April 2007). "Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial". Acta Orthopaedica. 78 (2): 172–9. doi:10.1080/17453670710013645. PMID 17464603.
- American Society of Anesthesiologists Task Force on Acute Pain Management (February 2012). "Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management". Anesthesiology. 116 (2): 248–273. doi:10.1097/ALN.0b013e31823c1030. PMID 22227789.
- Essving, P; Axelsson, K; Åberg, E; Spännar, H; Gupta, A; Lundin, A (October 2011). "Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial". Anesthesia & Analgesia. 113 (4): 926–33. doi:10.1213/ANE.0b013e3182288deb. PMID 21821506. S2CID 45897828.
- Nakama, Gilberto Yoshinobu; Peccin, Maria Stella; Almeida, Gustavo JM; Lira Neto, Ozório de Almeida; Queiroz, Antônio AB; Navarro, Ricardo Dizioli (17 October 2012). "Cemented, cementless or hybrid fixation options in total knee arthroplasty for osteoarthritis and other non-traumatic diseases". Cochrane Database of Systematic Reviews. 10: CD006193. doi:10.1002/14651858.cd006193.pub2. ISSN 1465-1858. PMID 23076921.
- Miller, Adam J.; Stimac, Jeffrey D.; Smith, Langan S.; Feher, Anthony W.; Yakkanti, Madhusudhan R.; Malkani, Arthur L. (April 2018). "Results of Cemented vs Cementless Primary Total Knee Arthroplasty Using the Same Implant Design". The Journal of Arthroplasty. 33 (4): 1089–1093. doi:10.1016/j.arth.2017.11.048. ISSN 1532-8406. PMID 29275115.
- Pulavarti, Ramnadh S.; Raut, Videsh V.; McLauchlan, George J. (May 2014). "Patella denervation in primary total knee arthroplasty - a randomized controlled trial with 2 years of follow-up". The Journal of Arthroplasty. 29 (5): 977–981. doi:10.1016/j.arth.2013.10.017. ISSN 1532-8406. PMID 24291230.
- Motififard, Mehdi; Nazem, Khalilollah; Zarfeshani, Aida; Zarfeshani, Kaveh (2018). "Effect of Patellar Electrocautery Neurectomy on Postoperative Pain among Patients Referred for Total Knee Arthroplasty". Advanced Biomedical Research. 7: 9. doi:10.4103/abr.abr_154_16. ISSN 2277-9175. PMC 5812092. PMID 29456980.
- Zmistowski, Benjamin M.; Fillingham, Yale A.; Salmons, Harold I.; Ward, Derek T.; Good, Robert P.; Lonner, Jess H. (September 2019). "Routine Patellar Resurfacing During Total Knee Arthroplasty Is Not Cost-Effective in Patients Without Patellar Arthritis". The Journal of Arthroplasty. 34 (9): 1963–1968. doi:10.1016/j.arth.2019.04.040. ISSN 1532-8406. PMID 31104838.
- Migliorini, Filippo; Eschweiler, Jörg; Niewiera, Marc; El Mansy, Yasser; Tingart, Markus; Rath, Björn (October 2019). "Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study". Archives of Orthopaedic and Trauma Surgery. 139 (10): 1445–1454. doi:10.1007/s00402-019-03246-z. ISSN 1434-3916. PMID 31367842. S2CID 199056777.
- Maruyama, Shigeki; Yoshiya, Shinichi; Matsui, Nobuzo; Kuroda, Ryosuke; Kurosaka, Masahiro (1 April 2004). "Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty1 1No benefits or funds were received in support of this study". The Journal of Arthroplasty. 19 (3): 349–353. doi:10.1016/j.arth.2003.09.010. ISSN 0883-5403. PMID 15067650.
- Longo, Umile Giuseppe; Ciuffreda, Mauro; Mannering, Nicholas; D'Andrea, Valerio; Locher, Joel; Salvatore, Giuseppe; Denaro, Vincenzo (April 2018). "Outcomes of Posterior-Stabilized Compared with Cruciate-Retaining Total Knee Arthroplasty". The Journal of Knee Surgery. 31 (4): 321–340. doi:10.1055/s-0037-1603902. ISSN 1938-2480. PMID 28666292. S2CID 4185540.
- Gray, Hans A.; Guan, Shanyuanye; Young, Tony J.; Dowsey, Michelle M.; Choong, Peter F.; Pandy, Marcus G. (29 January 2020). "Comparison of posterior-stabilized, cruciate-retaining, and medial-stabilized knee implant motion during gait". Journal of Orthopaedic Research. doi:10.1002/jor.24613. ISSN 1554-527X. PMID 31994751.
- Dowsey, Michelle M.; Gould, Daniel J.; Spelman, Timothy; Pandy, Marcus G.; Choong, Peter F. (7 February 2020). "A Randomized Controlled Trial Comparing a Medial Stabilized Total Knee Prosthesis to a Cruciate Retaining and Posterior Stabilized Design: A Report of the Clinical and Functional Outcomes Following Total Knee Replacement". The Journal of Arthroplasty. 35 (6): 1583–1590.e2. doi:10.1016/j.arth.2020.01.085. ISSN 1532-8406. PMID 32139194.
- Pelt, Christopher E.; Sandifer, Phillip A.; Gililland, Jeremy M.; Anderson, Mike B.; Peters, Christopher L. (September 2019). "Mean Three-Year Survivorship of a New Bicruciate-Retaining Total Knee Arthroplasty: Are Revisions Still Higher Than Expected?". The Journal of Arthroplasty. 34 (9): 1957–1962. doi:10.1016/j.arth.2019.04.030. ISSN 1532-8406. PMID 31160154.
- Hofstede, Stefanie N.; Nouta, Klaas Auke; Jacobs, Wilco; van Hooff, Miranda L.; Wymenga, Ate B.; Pijls, Bart G.; Nelissen, Rob G. H. H.; Marang-van de Mheen, Perla J. (2015). "Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis". The Cochrane Database of Systematic Reviews (2): CD003130. doi:10.1002/14651858.CD003130.pub3. ISSN 1469-493X. PMID 25650566.
- Barrack, Robert L. (November 2001). "Evolution of the Rotating Hinge for Complex Total Knee Arthroplasty". Clinical Orthopaedics and Related Research. 392 (392): 292–299. doi:10.1097/00003086-200111000-00038. ISSN 0009-921X. PMID 11716398. S2CID 10331507.
- Pal, Subrata (31 August 2013). Design of Artificial Human Joints & Organs. Springer Science & Business Media. ISBN 978-1-4614-6255-2.
- Chawla, Harshvardhan; van der List, Jelle P.; Christ, Alexander B.; Sobrero, Maximiliano R.; Zuiderbaan, Hendrik A.; Pearle, Andrew D. (1 March 2017). "Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis". The Knee. 24 (2): 179–190. doi:10.1016/j.knee.2016.11.006. ISSN 0968-0160. PMID 27916580.
- Meneghini, R. Michael; Mont, Michael A.; Backstein, David B.; Bourne, Robert B.; Dennis, Doug A.; Scuderi, Giles R. (2015). "Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty". The Journal of Arthroplasty. 30 (12): 2311–2314. doi:10.1016/j.arth.2015.05.049. ISSN 0883-5403. PMID 26122112.
- Napier, Richard J.; O’Neill, Christopher; O’Brien, Seamus; Doran, Emer; Mockford, Brian; Boldt, Jens; Beverland, David E. (2018). "A prospective evaluation of a largely cementless total knee arthroplasty cohort without patellar resurfacing: 10-year outcomes and survivorship". BMC Musculoskeletal Disorders. 19 (1): 205. doi:10.1186/s12891-018-2128-1. ISSN 1471-2474. PMC 6020353. PMID 29945574.
- Kumar, Nishikant; Yadav, Chandrashekhar; Raj, Rishi; Anand, Sumit (2014). "How to Interpret Postoperative X-rays after Total Knee Arthroplasty". Orthopaedic Surgery. 6 (3): 179–186. doi:10.1111/os.12123. ISSN 1757-7853. PMC 6583264. PMID 25179351.
- "Knee Replacement Surgery in Bangalore - Vydehi Institute of Medical Sciences".
- Tayton, E. R.; Frampton, C.; Hooper, G. J.; Young, S. W. (1 March 2016). "The impact of patient and surgical factors on the rate of infection after primary total knee arthroplasty". Bone Joint J. 98-B (3): 334–340. doi:10.1302/0301-620X.98B3.36775. ISSN 2049-4394. PMID 26920958. S2CID 11627819.
- Kerkhoffs, GM; Servien, E; Dunn, W; Dahm, D; Bramer, JA; Haverkamp, D (17 October 2012). "The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review". The Journal of Bone and Joint Surgery. American Volume. 94 (20): 1839–44. doi:10.2106/JBJS.K.00820. PMC 3489068. PMID 23079875.
- Samson AJ, Mercer GE, Campbell DG (September 2010). "Total knee replacement in the morbidly obese: a literature review". ANZ J Surg. 80 (9): 595–9. doi:10.1111/j.1445-2197.2010.05396.x. PMID 20840400.
- Cyteval, C. (2016). "Imaging of knee implants and related complications". Diagnostic and Interventional Imaging. 97 (7–8): 809–821. doi:10.1016/j.diii.2016.02.015. ISSN 2211-5684. PMID 27423710.
- Leone JM, Hanssen AD (2006). "Management of infection at the site of a total knee arthroplasty". Instr Course Lect. 55: 449–61. PMID 16958480.
- Parvizi, Javad; Zmistowski, Benjamin; Berbari, Elie F.; Bauer, Thomas W.; Springer, Bryan D.; Della Valle, Craig J.; Garvin, Kevin L.; Mont, Michael A.; Wongworawat, Montri D.; Zalavras, Charalampos G. (22 September 2011). "New Definition for Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society". Clinical Orthopaedics and Related Research. 469 (11): 2992–2994. doi:10.1007/s11999-011-2102-9. PMC 3183178. PMID 21938532.
- Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB (1999). "Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections". J Bone Joint Surg Am. 81 (10): 1434–45. doi:10.2106/00004623-199910000-00008. PMID 10535593.
- Chiu FY, Chen CM (2007). "Surgical débridement and parenteral antibiotics in infected revision total knee arthroplasty". Clin. Orthop. Relat. Res. 461: 130–5. doi:10.1097/BLO.0b013e318063e7f3. PMID 17438469. S2CID 21867921.
- S.G.F. Abram, A.G Marsh, F. Nicol, A.S. Brydone, A. Mohammed, S.J. Spencer (21 February 2018). "The Impact Of Tibial Component Overhang On Outcome Scores And Pain In Total Knee Replacement". Orthopaedic Proceedings.CS1 maint: multiple names: authors list (link)
- Inui, Hiroshi; Taketomi, Shuji; Nakamura, Kensuke; Takei, Seira; Takeda, Hideki; Tanaka, Sakae; Nakagawa, Takumi (2013). "Influence of navigation system updates on total knee arthroplasty". Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology. 5 (1): 10. doi:10.1186/2052-1847-5-10. ISSN 1758-2555. PMC 3653716. PMID 23638774. (CC-BY-2.0)
- Gromov, Kirill; Korchi, Mounim; Thomsen, Morten G; Husted, Henrik; Troelsen, Anders (2014). "What is the optimal alignment of the tibial and femoral components in knee arthroplasty?". Acta Orthopaedica. 85 (5): 480–487. doi:10.3109/17453674.2014.940573. ISSN 1745-3674. PMC 4164865. PMID 25036719.
- Lee, Ju Hong; Wang, Seong-Il (2015). "Risk of Anterior Femoral Notching in Navigated Total Knee Arthroplasty". Clinics in Orthopedic Surgery. 7 (2): 217–24. doi:10.4055/cios.2015.7.2.217. ISSN 2005-291X. PMC 4515463. PMID 26217469.
- Carter, Evelene M; Potts, Henry WW (2014). "Predicting length of stay from an electronic patient record system: a primary total knee replacement example". BMC Medical Informatics and Decision Making. 14 (1): 26. doi:10.1186/1472-6947-14-26. ISSN 1472-6947. PMC 3992140. PMID 24708853.
- "Rehabilitation" (PDF). massgeneral.org.
- Valtonen, Anu; Pöyhönen, Tapani; Heinonen, Ari; Sipilä, Sarianna (1 October 2009). "Muscle Deficits Persist After Unilateral Knee Replacement and Have Implications for Rehabilitation". Physical Therapy. 89 (10): 1072–1079. doi:10.2522/ptj.20070295. ISSN 0031-9023. PMID 19713269.
- Yang, Michael M. H.; Hartley, Rebecca L.; Leung, Alexander A.; Ronksley, Paul E.; Jetté, Nathalie; Casha, Steven; Riva-Cambrin, Jay (1 April 2019). "Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis". BMJ Open. 9 (4): e025091. doi:10.1136/bmjopen-2018-025091. ISSN 2044-6055. PMC 6500309. PMID 30940757.
- Monaghan, B; Caulfield, B; O'Mathúna, DP (20 January 2010). "Surface neuromuscular electrical stimulation for quadriceps strengthening pre and post total knee replacement" (PDF). The Cochrane Database of Systematic Reviews (1): CD007177. doi:10.1002/14651858.CD007177.pub2. PMC 7211999. PMID 20091621.
- Leah, 2013
- &Na; Dickinson, S (2013). "Foreword". Critical Care Nursing Quarterly. 36 (1): 1–2. doi:10.1097/cnq.0b013e3182750631. PMID 23221435.
- Teodoro, 2016
- Ong & Pua, 2011
- American Physical Therapy Association (15 September 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Physical Therapy Association, retrieved 15 September 2014
- Harvey, Lisa A.; Brosseau, Lucie; Herbert, Robert D. (6 February 2014). "Continuous passive motion following total knee arthroplasty in people with arthritis". The Cochrane Database of Systematic Reviews (2): CD004260. doi:10.1002/14651858.CD004260.pub3. ISSN 1469-493X. PMID 24500904. S2CID 4123895.
- Adie, S; Kwan, A; Naylor, JM; Harris, IA; Mittal, R (12 September 2012). "Cryotherapy following total knee replacement". The Cochrane Database of Systematic Reviews (9): CD007911. doi:10.1002/14651858.CD007911.pub2. PMID 22972114.
- American Academy of Orthopaedic Surgeons (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Academy of Orthopaedic Surgeons, retrieved 19 May 2013, which cites
- Members of 2007 and 2011 AAOS Guideline Development Work Groups on PE/VTED Prophylaxis; Mont, M; Jacobs, J; Lieberman, J; Parvizi, J; Lachiewicz, P; Johanson, N; Watters, W (18 April 2012). "Preventing venous thromboembolic disease in patients undergoing elective total hip and knee arthroplasty". The Journal of Bone and Joint Surgery. American Volume. 94 (8): 673–4. doi:10.2106/JBJS.9408edit. PMC 3326687. PMID 22517384.
- Hamilton, TW; Strickland, LH; Pandit, HG (17 August 2016). "A Meta-Analysis on the Use of Gabapentinoids for the Treatment of Acute Postoperative Pain Following Total Knee Arthroplasty". The Journal of Bone and Joint Surgery. American Volume. 98 (16): 1340–50. doi:10.2106/jbjs.15.01202. PMID 27535436.
- Khan, Fary; Ng, Louisa; Gonzalez, Senen; Hale, Tom; Turner-Stokes, Lynne (23 April 2008). "Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy". Cochrane Database of Systematic Reviews (2): CD004957. doi:10.1002/14651858.cd004957.pub3. ISSN 1465-1858. PMID 18425906.
- Pfuntner A., Wier L.M., Stocks C. Most Frequent Procedures Performed in U.S. Hospitals, 2011. HCUP Statistical Brief #165. October 2013. Agency for Healthcare Research and Quality, Rockville, MD. .
- Weiss AJ, Elixhauser A, Andrews RM (February 2014). "Characteristics of Operating Room Procedures in U.S. Hospitals, 2011". HCUP Statistical Brief #170. Rockville, MD: Agency for Healthcare Research and Quality.
- Weiss AJ, Elixhauser A (March 2014). "Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011". HCUP Statistical Brief #171. Rockville, MD: Agency for Healthcare Research and Quality.
- Fingar KR, Stocks C, Weiss AJ, Steiner CA (December 2014). "Most Frequent Operating Room Procedures Performed in U.S. Hospitals, 2003-2012". HCUP Statistical Brief #186. Rockville, MD: Agency for Healthcare Research and Quality.
- Dreyer HC, Strycker LA, Senesac HA, Hocker AD, Smolkowski K, Shah SN, Jewett BA (2013). "Essential amino acid supplementation in patients following total knee arthroplasty". J Clin Invest. 123 (11): 4654–4666. doi:10.1172/JCI70160. PMC 3809795. PMID 24135139.
External links
- A New Set of Knees Comes at a Price: A Whole Lot of Pain By Jane E. Brody, The New York Times, 8 February 2005
- When It Comes to Severe Pain, Doctors Still Have Much to Learn By Jane E. Brody, The New York Times, 15 February 2005
- A Year With My New Knees: Much Pain but Much Gain By Jane E. Brody, The New York Times, 20 December 2005
- 3 Years Later, Knees Made for Dancing, By Jane E. Brody, The New York Times, 3 June 2008
- Relief for Joints Besieged by Arthritis, By Jane E. Brody, The New York Times, 9 July 2012
| Classification |
|---|