Orthognathic surgery
Orthognathic surgery (/ˌɔːrθəɡˈnæθɪk/); also known as corrective jaw surgery or simply jaw surgery, is surgery designed to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion problems owing to skeletal disharmonies, or other orthodontic problems that cannot be easily treated with braces. Originally coined by Harold Hargis, this surgery is also used to treat congenital conditions such as cleft palate.[1] Typically during oral surgery, bone is cut, moved, modified, and realigned to correct a dentofacial deformity. The word "osteotomy" means the division, or excision of bone. The dental osteotomy allows surgeons to visualize the jawbone, and work accordingly.
| Orthognathic surgery | |
|---|---|
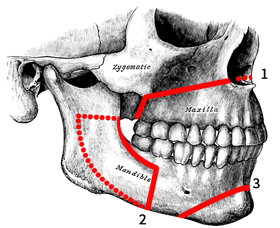 Osteotomies of the jaws: 1. Lefort I 2. Sagittal split 3. Genioplasty | |
| ICD-9-CM | 76.6 |
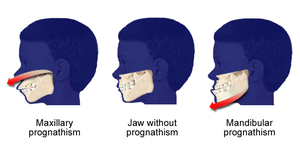
The operation is used to correct jaw problems in about 5% of general population[2][3][4] presenting with dentofacial deformities like maxillary prognathisms, mandibular prognathisms, open bites, difficulty chewing, difficulty swallowing, temporomandibular joint dysfunction pains, excessive wear of the teeth, and receding chins.
Medical uses
It is estimated that nearly 5% of the UK or USA population present with dentofacial deformities that are not amenable to orthodontic treatment requiring orthognathic surgery as a part of their definitive treatment.[5][3][4] Orthognathic surgery can be used to correct:
- Gross jaw discrepancies (anteroposterior, vertical, or transverse discrepancies)[6]
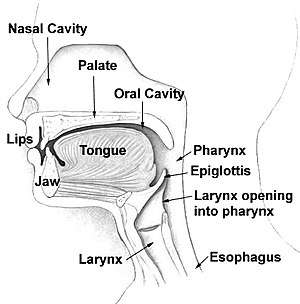
- Skeletofacial discrepancies associated with documented sleep apnea, airway defects, and soft tissue discrepancies
- Skeletofacial discrepancies associated with documented temporomandibular joint pathology
A disproportionately grown upper or lower jaw causes dentofacial deformities. Chewing becomes problematic, and may also cause pain due to straining of the jaw muscle and bone. Deformities range from micrognathia, which is when the mandible doesn't grow far forward enough (over bite), and when the mandible grows too much, causing an under bite; all of which are uncomfortable. Also, a total maxilla osteotomy is used to treat the "long face syndrome," known as the skeptical open bite, idiopathic long face, hyper divergent face, total maxillary alveolar hyperplasia, and vertical maxillary excess. Prior to surgery, surgeons should take x-rays of the patient's jaw to determine the deformity, and to make a plan of procedures.[7] Mandible osteotomies, or corrective jaw surgeries, benefit individuals who suffer from difficulty chewing, swallowing, TMJ pains, excessive wear of the teeth, open bites, overbites, underbites, or a receding chin. The deformities listed above can be perfected by an osteotomy surgery of either the maxilla or mandible (whichever the deformity calls for), which is performed by an oral surgeon who is specialized in the working with both the upper and lower jaws.[8] Orthognathic surgery is also available as a very successful treatment (90–100%) for obstructive sleep apnea.[9]
- Cleft lip and palate
Orthognathic surgery is a well established and widely used treatment option for insufficient growth of the maxilla in patients with an orofacial cleft.[10] There is some debate regarding the timing of orthognathic procedures, to maximise the potential for natural growth of the facial skeleton.[11] Patient reported aesthetic outcomes of orthognathic surgery for cleft lip and palate appear to be of overall satisfaction,[12][13] despite complications that may arise. A potentially significant long-term outcome of orthognathic surgery is impaired maxillary growth, due to scar tissue formation.[14] A 2013 systematic review comparing traditional orthognathic surgery with maxillary distraction osteogenesis found that the evidence was of low quality; it appeared that both procedures might be effective, but suggested distraction osteogenesis might reduce the incidence of long-term relapse.[15]
Risks
Although infrequent, there can be complications such as bleeding, swelling, infection, nausea and vomiting.[16] Infection rates of up to 7% are reported after orthognathic surgery; antibiotic prophylaxis reduces the risk of surgical site infections when the antibiotics are given during surgery and continued for longer than a day after the operation.[17]
There can also be some post operative facial numbness due to nerve damage.[18] Diagnostics for nerve damage consist of: brush-stroke directional discrimination (BSD), touch detection threshold (TD), warm/cold (W/C) and sharp/blunt discrimination (S/B), electrophysiological tests (mental nerve blink reflex (BR), nerve conduction study (NCS), and cold (CDT) and warm (WDT) detection thresholds.[19] The inferior alveolar nerve, which is a branch of the mandibular nerve, must be identified during surgery and worked around carefully in order to minimize nerve damage. The numbness may be either temporary, or more rarely, permanent.[20] Recovery from the nerve damage typically occurs within 3 months after repair.
Surgery
Orthognathic surgery is performed by an oral surgeon in collaboration with an orthodontist. It often includes braces before and after surgery, and retainers after the final removal of braces. Orthognathic surgery is often needed after reconstruction of cleft palate or other major craniofacial anomalies. Careful coordination between the surgeon and orthodontist is essential to ensure that the teeth will fit correctly after the surgery.
Planning
Planning for the surgery usually involves input from a multidisciplinary team, including oral and maxillofacial surgeons, orthodontists, and occasionally a speech and language therapist. Although it depends on the reason for surgery, working with a speech and language therapist in advance can help minimize potential relapse. The surgery usually results in a noticeable change in the patient's face; a psychological assessment is occasionally required to assess patient's need for surgery and its predicted effect on the patient. Radiographs and photographs are taken to help in the planning. There is also advanced software that can predict the shape of the patient's face after surgery,[21][22] which is useful for the planning and also explaining the surgery to the patient and the patient's family.[23]
The main goals of orthognathic surgery are to achieve a correct bite, an aesthetic face, and an enlarged airway. While correcting the bite is important, if the face is not considered, the resulting bone changes might lead to an unaesthetic result.[24] Great care needs to be taken during the planning phase to maximize airway patency.
Technique
All dentofacial osteotomies are performed under general anesthesia, causing total unconsciousness. General anesthesia allows surgeons to perform dentofacial osteotomies effectively without involuntary muscle movement or complaints about minor pain. Prior to any Osteotomy, third molars (wisdom teeth) are extracted to reduce the chance of infection. Dentofacial osteotomy is usually performed using oscillating and reciprocating saws, burs, and manual chisels. Reciprocating saws are straight and are used for making straight bone cuts. Oscillating saws are angled, to different degrees, in order to make deep curved cuts for certain osteotomies like mandible angle reduction. The recent advent of piezoelectric saws has simplified bone cutting, but such equipment has not yet become the norm outside of the most developed countries. The surgery might involve one jaw or both jaws concurrently. The modification is done by making cuts in the bones of the mandible and/or maxilla, and repositioning the cut pieces in the desired alignment. This surgery is usually performed with the use of general anaesthetic and a nasal tube for intubation. The nasal tube enables the teeth to be wired together during surgery. The surgery usually does not involve cutting the skin. Instead, the surgeon is often able to go through the interior of the mouth. Cutting one bone is known as an osteotomy, while performing the surgery on both jaws simultaneously is known as a bi-maxillary osteotomy (cutting the bone of both jaws) or a maxillomandibular advancement.
The maxilla can be adjusted using a "Lefort I" level osteotomy (most common). Additionally, the midface can be mobilized by using a Lefort II, or Lefort III osteotomy. These techniques are utilized extensively for children that suffer from various craniofacial abnormalities, such as Crouzon syndrome.
The jaws will be wired together (inter-maxillary fixation) using stainless steel wires during the surgery to ensure the correct re-positioning of the bones. In most cases, these wires are released before the patient wakes up. However, some surgeons prefer to wire the jaws shut instead.
In some instances, the change in jaw structure will cause the cheeks to become depressed and shallow. Some procedures will call for the insertion of implants to give the patient's face a fuller look.

Maxilla osteotomy (upper jaw)
This procedure is intended for patients with an upper jaw deformity, or with an open bite. Operating on the upper jaw requires surgeons to make incisions below both eye sockets, making it a bilateral osteotomy, enabling the whole upper jaw, along with the roof of the mouth and upper teeth, to move as one unit. At this time, the upper jaw can be moved and aligned correctly in order to fit the upper teeth in place with the lower teeth. Then, the jaw is stabilized using titanium screws that will eventually be grown over by bone, permanently staying in the mouth.
Mandible osteotomy (lower jaw)
The mandible osteotomy is intended for those with a receded mandible (lower jaw) or an open bite, which may cause difficulty chewing and jaw pain. For this procedure cuts are made behind the molars, in between the first and second molars, and lengthwise, detaching the front of the jaw so the palate (including the teeth and all) can move as one unit. From here, the surgeon can smoothly slide the mandible into its new position. Stabilization screws are used to support the jaw until the healing process is done.[25]
Sagittal split osteotomy

This procedure is used to correct mandible retrusion and mandibular prognathism (over and under bite). First, a horizontal cut is made on the inner side of the ramus mandibulae, extending anterally to the anterior portion of the ascending ramus. The cut is then made inferiorly on the ascending ramus to the descending ramus, extending to the lateral border of the mandible in the area between the first and second molar. At this time, a vertical cut is made extending inferior to the body of the mandible, to the inferior border of the mandible. All cuts are made into the middle of the bone, where bone marrow is present. Then, a chisel is inserted into the pre existing cuts and tapped gently in all areas to split the mandible of the left and right side. From here, the mandible can be moved either forwards or backwards. If sliding backwards, the distal segment must be trimmed to provide room in order to slide the mandible backwards. Lastly, the jaw is stabilized using stabilizing screws that are inserted extra-orally. The jaw is then wired shut for approximately 4–5 weeks.[25]
Genioplasty osteotomy (intra-oral)
This procedure is used for the advancement (movement forward) or retraction (movement backwards) of the chin. First, incisions are made from the first bicuspid to the first bicuspid, exposing the mandible. Then, soft tissue of the mandible is detached from the bone; done by stripping attaching tissues. A horizontal incision is then made inferior to the first bicuspids, bilaterally, where bone cuts (osteotomies) are made vertically inferior, extending to the inferior border of the mandible, thereby detaching the bony segments of the mandible. The bony segments are stabilized with titanium plates; no fixation (binding of the jaw) necessary. If advancement is indicated for the chin, there are inert products available to implant onto the mandible, utilizing titanium screws, bypassing bone cuts.[25]
Rapid palatal expansion osteotomy
When a patient has a constricted (oval shape) maxilla, but normal mandible, many orthodontists request a rapid palatal expansion. This consists of the surgeon making horizontal cuts on the lateral board of the maxilla, extending anterally to the inferior border of the nasal cavity. At this time, a chisel designed for the nasal septum is utilized to detach the maxilla from the cranial base. Then, a pterygoid chisel, which is a curved chisel, is used on the left and right side of the maxilla to detach the pterygoid palates. Care must be taken as to not injure the inferior palatine artery. Prior to the procedure, the orthodontist has an orthopedic appliance attached to the maxilla teeth, bilaterally, extending over the palate with an attachment so the surgeon may use a hex-like screw to place into the device to push from anterior to posterior to start spreading the bony segments.[25] The expansion of the maxilla may take up to 8 weeks with the surgeon advancing the expander hex lock, sideways (← →), once a week.
Post operation
After orthognathic surgery, patients are often required to adhere to an all-liquid diet for a time. Weight loss due to lack of appetite and the liquid diet is common. Normal recovery time can range from a few weeks for minor surgery, to up to a year for more complicated surgery. For some surgeries, pain may be minimal due to minor nerve damage and lack of feeling. Doctors will prescribe pain medication and prophylactic antibiotics to the patient. There is often a large amount of swelling around the jaw area, and in some cases bruising. Most of the swelling will disappear in the first few weeks, but some may remain for a few months.
Recovery
All dentofacial osteotomies require an initial healing time of 2–6 weeks with secondary healing (complete bony union and bone remodeling) taking an additional 2–4 months. The jaw is sometimes immobilized (movement restricted by wires or elastics) for approximately 1–4 weeks. However, the jaw will still require two to three months for proper healing. Lastly, if screws were inserted in the jaw, bone will typically grow over them during the two to three month healing period. Patients also may not drive or operate vehicles or large machinery during the consumption of painkillers, which are typically taken for six to eight days after the surgery, depending on the pain experienced. Immediately after surgery, patients must adhere to certain infection preventing instructions such as daily cleaning, and the consumption of antibiotics. Cleaning of the mouth should always be done regardless of surgery to ensure healthy, strong teeth. Patients are able to return to work 2–6 weeks after the surgery, but must follow the specific rules for recovery for ~8 weeks.[26]
History
Mandible and maxilla osteotomies date to the 1940s. They were used to correct dentofacial deformities like a malocclusion, and a prognathism.[27] Advances have been made in the procedures, and in the anesthesia used. In 1985, mandible and maxilla osteotomies were effectively used to correct more extreme deformities like receding chins, and to relieve pain from temporomandibular joint disorder (TMJ).
Prior to 1991, some patients undergoing a dentofacial osteotomy still had third molars (wisdom teeth), and had them removed during surgery. An extensive study done by Dr. M Lacy and Dr. R Colcleugh, was used to identify threats of combining the two surgeries used 83 patients from the time span of 1987 and 1991. Patients were reviewed, and divided into two groups; those who had, and those who didn't have their third molars extracted during the dentofacial Osteotomy. The study showed that 73% of patients developed an infection of the hardware inserted into the jaw when having their third molars removed during an osteotomy. The data indicated that getting the osteotomy and the third molar extraction at the same time highly increases the chances of infection development.[28]
Advances in the surgical techniques allow surgeons to perform the surgery under local anesthesia with assistance from intravenous sedation. Dr. Raffaini introduced this technique in 2002 after a four-year study done with local anesthesia and assistance from intravenous sedation. Prior to this, surgeons would fully sedate patients, hospitalizing them shortly after the surgery for a 2-3 day recovery, specifically from the anesthesia. Advancements allow surgeons to expand the use of an osteotomy on more parts of the jaws with faster recovery time, less pain, and no hospitalization, making the surgery more effective with respect to time and recovery.[29] The procedure, which is strictly used for a mandibular (jaw) deformity and mobilization, has advanced from similar, very effective procedures performed since 1985. The original mandible and maxilla osteotomy procedure still remains almost unchanged, as it is the simplest and still the most effective for dentofacial deformity correction.
References
- Bill J, Proff P, Bayerlein T, Blens T, Gedrange T, Reuther J (September 2006). "Orthognathic surgery in cleft patients". J Craniomaxillofac Surg. 34 (Suppl 2): 77–81. doi:10.1016/S1010-5182(06)60017-6. PMID 17071397.
- Posnick, Jeffrey C. (September 2013). Orthognatic Surgery: Principles and Practice. Amsterdam: Elsevier. pp. 61–68. doi:10.1016/B978-1-4557-2698-1.00003-4. ISBN 978-145572698-1.
- Harrington C, Gallagher JR, Borzabadi-Farahani A (April 2015). "A retrospective analysis of dentofacial deformities and orthognathic surgeries using the index of orthognathic functional treatment needs (IOFTN)". Int J Pediatr Otorhinolaryngol. 79 (7): 1063–6. doi:10.1016/j.ijporl.2015.04.027. PMID 25957779.
- Borzabadi-Farahani A, Eslamipour F, Shahmoradi M (2016). "Functional needs of subjects with dentofacial deformities: A study using the index of orthognathic functional treatment need (IOFTN)". J Plast Reconstr Aesthet Surg. 69 (6): 796–801. doi:10.1016/j.bjps.2016.03.008. PMID 27068664.
- Posnick, Jeffrey C. (September 2013). Orthognatic Surgery: Principles and Practice. Amsterdam: Elsevier. pp. 61–68. doi:10.1016/B978-1-4557-2698-1.00003-4. ISBN 978-145572698-1.
- "Ortho Criteria". AAOMS.org. American Association of Oral and Maxillofacial Surgeons. Retrieved 2014-11-05.
- Arnet, Gary F., and Linda M. Basehore. "Dentofacial reconstruction." The American Journal of Nursing. 12. 84 (1984): 1488-490.
- William H. Bell; William R. Proffit; Raymond P. White (1980). Surgical correction of dentofacial deformities. Saunders. ISBN 978-0-7216-1675-9.
- Prinsell JR (December 1999). "Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients". Chest. 116 (6): 1519–29. doi:10.1378/chest.116.6.1519. PMID 10593771.
- DeLuke, Dean M; Marchand, Anick; Robles, Elizabeth C; Fox, Patricia (1997). "Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases". Journal of Oral and Maxillofacial Surgery. 55 (7): 694–697. doi:10.1016/s0278-2391(97)90579-6. PMID 9216501.
- Wolford, Larry M.; Stevao, Eber L.L. (2016-11-10). "Correction of jaw deformities in patients with cleft lip and palate". Proceedings (Baylor University. Medical Center). 15 (3): 250–254. doi:10.1080/08998280.2002.11927848. ISSN 0899-8280. PMC 1276618. PMID 16333445.
- Munz, S. M.; Edwards, S. P.; Inglehart, M. R. (2011-08-01). "Oral health-related quality of life, and satisfaction with treatment and treatment outcomes of adolescents/young adults with cleft lip/palate: an exploration". International Journal of Oral and Maxillofacial Surgery. 40 (8): 790–796. doi:10.1016/j.ijom.2011.03.002. PMID 21474288.
- Gkantidis, Nikolaos; Papamanou, Despina A.; Christou, Panagiotis; Topouzelis, Nikolaos (2013). "Aesthetic outcome of cleft lip and palate treatment. Perceptions of patients, families, and health professionals compared to the general public". Journal of Cranio-Maxillofacial Surgery. 41 (7): e105–e110. doi:10.1016/j.jcms.2012.11.034. PMID 23287059.
- Daskalogiannakis, John; Mehta, Manisha (2009-10-05). "The Need for Orthognathic Surgery in Patients With Repaired Complete Unilateral and Complete Bilateral Cleft Lip and Palate". The Cleft Palate-Craniofacial Journal. 46 (5): 498–502. doi:10.1597/08-176.1. PMID 19929100.
- Kloukos, Dimitrios; Fudalej, Piotr; Sequeira-Byron, Patrick; Katsaros, Christos; Kloukos, Dimitrios (2013). "Maxillary distraction osteogenesis versus orthognathic surgery for cleft lip and palate patients". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD010403.

- Silva AC, O'Ryan F, Poor DB (September 2006). "Postoperative nausea and vomiting (PONV) after orthognathic surgery: a retrospective study and literature review". J. Oral Maxillofac. Surg. 64 (9): 1385–97. doi:10.1016/j.joms.2006.05.024. PMID 16916674.
- Brignardello-Petersen, Romina; Carrasco-Labra, Alonso; Araya, Ignacio; Yanine, Nicolás; Cordova Jara, Luis; Villanueva, Julio (2015-01-05). "Antibiotic prophylaxis for preventing infectious complications in orthognathic surgery". The Cochrane Database of Systematic Reviews. 1: CD010266. doi:10.1002/14651858.CD010266.pub2. ISSN 1469-493X. PMID 25561078.

- Panula K, Finne K, Oikarinen K (October 2001). "Incidence of complications and problems related to orthognathic surgery: a review of 655 patients". J. Oral Maxillofac. Surg. 59 (10): 1128–36, discussion 1137. doi:10.1053/joms.2001.26704. PMID 11573165.
- Teerijoki-Oksa T, Jääskeläinen SK, Forssell K, Forssell H (2004). "Recovery of nerve injury after mandibular sagittal split osteotomy. Diagnostic value of clinical and electrophysiologic tests in the follow-up". Int J Oral Maxillofac Surg. 33 (2): 134–40. doi:10.1054/ijom.2003.0463. PMID 15050068.
- Eckert AW, Maurer P, Kriwalsky MS, Schubert J (September 2006). "P.292 Complications in orthognathic surgery". J Craniomaxillofac Surg. 34 (Suppl 1): 206. doi:10.1016/S1010-5182(06)60797-X.
- Mischkowski RA, Zinser MJ, Kübler AC, Krug B, Seifert U, Zöller JE (December 2006). "Application of an augmented reality tool for maxillary positioning in orthognathic surgery — a feasibility study". J Craniomaxillofac Surg. 34 (8): 478–83. doi:10.1016/j.jcms.2006.07.862. PMID 17157519.
- Uechi J, Okayama M, Shibata T, et al. (December 2006). "A novel method for the 3-dimensional simulation of orthognathic surgery by using a multimodal image-fusion technique". Am J Orthod Dentofacial Orthop. 130 (6): 786–98. doi:10.1016/j.ajodo.2006.03.025. PMID 17169742.
- Tsuji M, Noguchi N, Shigematsu M, et al. (September 2006). "A new navigation system based on cephalograms and dental casts for oral and maxillofacial surgery". Int J Oral Maxillofac Surg. 35 (9): 828–36. doi:10.1016/j.ijom.2006.02.024. PMID 16690251.
- Arnett GW, Gunson MJ (September 2004). "Facial planning for orthodontists and oral surgeons". Am J Orthod Dentofacial Orthop. 126 (3): 290–5. doi:10.1016/j.ajodo.2004.06.006. PMID 15356488.
- Dr. Charles A. Loschiavo. Personal. 2 April 2009.
- Mandible (Lower Jaw) Osteotomy. 2007. British Association of Oral and Maxillofacial Surgeon (BAOMS). 29 Feb. 2009 http://www.baoms.org.uk
- Puricelli, Edela. "A new technique for mandibular osteotomy." Head & Face Medicine 3.15 (2007). Head & Face Medicine. 13 Mar. 2007. BioMed Central Ltd. 27 Feb. 2009 http://www.head-face-med.com
- Lacey MS, Colcleugh RG (1995). "Infected screws in patients treated by mandibular sagittal split osteotomy". J. Oral Maxillofac. Surg. 53 (5): 510–2, discussion 513. doi:10.1016/0278-2391(95)90059-4. PMID 7722717.
- Raffaini M, Hernandez Alfaro F, Ghilardi R, Garcia Lopez A (2002). "The sagittal mandibular osteotomy under local anesthesia and intravenous sedation: four years of multicenter experience". Int J Adult Orthodon Orthognath Surg. 17 (4): 267–71. PMID 12592998.