Influenza treatment
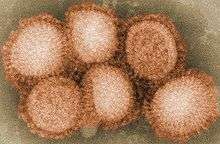
Treatments for influenza include a range of medications and therapies that are used in response to disease influenza. Treatments may either directly target the influenza virus itself; or instead they may just offer relief to symptoms of the disease, while the body's own immune system works to recover from infection.[1]
| Influenza (Flu) |
|---|
 |
|
The two main classes of antiviral drugs used against influenza are neuraminidase inhibitors, such as zanamivir and oseltamivir, or inhibitors of the viral M2 protein, such as amantadine and rimantadine. These drugs can reduce the severity of symptoms if taken soon after infection and can also be taken to decrease the risk of infection. However, virus strains have emerged that show drug resistance to both classes of drug.
Symptomatic treatment
The United States authority on disease prevention, the Centers for Disease Control and Prevention (CDC), recommends that persons suffering from influenza infections:
- Stay at home
- Get plenty of rest
- Drink a lot of liquids
- Do not smoke or drink alcohol
- Consider over-the-counter medications to relieve flu symptoms
- Consult a physician early on for best possible treatment
- Remain alert for emergency warning signs[2]
Warning signs are symptoms that indicate that the disease is becoming serious and needs immediate medical attention. These include:
- Difficulty breathing or shortness of breath
- Pain or pressure in the chest or abdomen
- Dizziness
- Confusion
- Severe or persistent vomiting
In children other warning signs include irritability, failing to wake up and interact, rapid breathing, and a blueish skin color. Another warning sign in children is if the flu symptoms appear to resolve, but then reappear with fever and a bad cough.[2]
Antiviral drugs
Antiviral drugs directly target the viruses responsible for influenza infections. Generally, anti-viral drugs work optimally when taken within a few days of the onset of symptoms.[3] Certain drugs are used prophylactically, that is they are used in uninfected individuals to guard against infection.
Four licensed influenza antiviral agents are available in the United States: amantadine, rimantadine, zanamivir, and oseltamivir.[4] They are available through prescription only. These drugs fall into categories as either M2-inhibitors (admantane derivatives) or neuraminidase inhibitors as illustrated in the following table.
| Class | Effective Against | Drug Name (INN) | Brand Name | Year Approved | Manufacturer |
|---|---|---|---|---|---|
| M2 inhibitors (adamantane derivatives) |
Influenza A | Amantadine | Symmetrel | 1976 | Endo Pharmaceuticals |
| Rimantadine | Flumadine | 1994 | Forest Laboratories | ||
| Neuraminidase inhibitors | Influenza A & B | Zanamivir | Relenza | 1999 | GlaxoSmithKline |
| Oseltamivir | Tamiflu | 1999 | Hoffmann-La Roche | ||
| Cap-dependent endonuclease inhibitor | Influenza A & B | Baloxavir marboxil | Xofluza | 2018 | Shionogi & Company、 |
| Note: Neuraminidase inhibitors are approved for prophylaxis use in children and adults. | |||||
In Russia and China a drug called arbidol is also used as a treatment. Testing of the drug has predominantly occurred in these countries and, although no clinical trials have been published demonstrating this is an effective drug, some data suggest that this could be a useful treatment for influenza.[5][6]
Peramivir
Peramivir, an experimental anti-influenza drug, developed by BioCryst Pharmaceuticals has not yet been approved for sale in the United States.[7][8] This drug can be given as an injection, so may be particularly useful in serious cases of influenza where the patient is unconscious and oral or inhaled drug administration is therefore difficult.[9][10]
In October 2009, it was reported that the experimental antiviral drug Peramivir had been effective in treating serious cases of swine flu.[11] On October 23, the U.S. Food and Drug Administration (FDA) issued an Emergency Use Authorization for Peramivir (now expired), leading to wider and faster availability for patients. Since the FDA's decisions and actions are closely watched around the world, this move is likely to also increase demand for Peramivir internationally.[12][13]
Interferons
Interferons are cellular signalling factors produced in response to viral infection. Research into the use of interferons to combat influenza began in the 1960s in the Soviet Union, culminating in a trial of 14,000 subjects at the height of the Hong Kong Flu of 1969, in which those treated prophylactically with interferon were more than 50% less likely to suffer symptoms, though evidence of latent infection was present.[14] In these early studies leukocytes were collected from donated blood and exposed to a high dose of Newcastle disease, causing them to release interferons. Although interferon therapies became widespread in the Soviet Union, the method was doubted in the United States after high doses of interferon proved ineffective in trials. Though the 1969 study used 256 units of interferon, subsequent studies used up to 8.4 million units. It has since been proposed that activity of interferon is highest at low concentrations.[15] Phase III trials in Australia are planned for 2010, and initial trials are planned in the U.S. for late 2009.[16]
Interferons have also been investigated as adjuvants to enhance to effectiveness of influenza vaccines. This work was based on experiments in mice that suggested that type I interferons could enhance the effectiveness of influenza vaccines in mice.[17] However, a clinical trial in 2008 found that oral dosing of elderly patients with interferon-alpha actually reduced their immune response to an influenza vaccine.[18]
Viferon is a suppository of (non-pegylated[19]) interferon alpha-2b, ascorbic acid (vitamin C), and tocopherol (vitamin E) which was reported in two small studies to be as effective as arbidol.[20][21] It is sold in Russia for $4–$9 per suppository depending on dose. Another interferon alfa-2b medicine, "Grippferon", nasal drops, is used for treatment and emergency prevention of Influenza and cold.[22] Its manufacturers have appealed to the WHO to consider its use against avian influenza and H1N1 Influenza 09 (Human Swine Flu), stating that it was used successfully in Russia for eight years, but that "the medical profession in Europe and the USA is not informed about this medicine".[23]
Drug resistance
Influenza viruses can show resistance to anti-viral drugs. Like the development of bacterial antibiotic resistance, this can result from over-use of these drugs. For example, a study published in the June 2009 Issue of Nature Biotechnology emphasized the urgent need for augmentation of oseltamivir (Tamiflu) stockpiles with additional antiviral drugs including zanamivir (Relenza) based on an evaluation of the performance of these drugs in the scenario that the 2009 H1N1 'Swine Flu' neuraminidase (NA) were to acquire the tamiflu-resistance (His274Tyr) mutation which is currently widespread in seasonal H1N1 strains.[24] Yet another example is in the case of the amantadines treatment may lead to the rapid production of resistant viruses, and over-use of these drugs has probably contributed to the spread of resistance.[25] In particular, this high-level of resistance may be due to the easy availability of amantadines as part of over-the-counter cold remedies in countries such as China and Russia,[26] and their use to prevent outbreaks of influenza in farmed poultry.[27][28]
On the other hand, a few strains resistant to neuraminidase inhibitors have emerged and circulated in the absence of much use of the drugs involved, and the frequency with which drug resistant strains appears shows little correlation with the level of use of these drugs.[29] However, laboratory studies have shown that it is possible for the use of sub-optimal doses of these drugs as a prophylactic measure might contribute to the development of drug resistance.[29]
During the United States 2005–2006 influenza season, increasing incidence of drug resistance by strain H3N2 to amantadine and rimantadine led the CDC to recommend oseltamivir as a prophylactic drug, and the use of either oseltamivir or zanamivir as treatment.[4] [30]
Over-the-counter medication
Antiviral drugs are prescription-only medication in the United States. Readily available over-the-counter medications do not directly affect the disease, but they do provide relief from influenza symptoms, as illustrated in the table below.
| Symptom(s) | OTC Medicine |
|---|---|
| fever, aches, pains, sinus pressure, sore throat | analgesics |
| nasal congestion, sinus pressure | decongestants |
| sinus pressure, runny nose, watery eyes, cough | antihistamines |
| cough | cough suppressant |
| sore throat | local anesthetics |
Children and teenagers with flu symptoms (particularly fever) should avoid taking aspirin as taking aspirin in the presence of influenza infection (especially Influenzavirus B) can lead to Reye's syndrome, a rare but potentially fatal disease of the brain.[32]
Off-label uses of other drugs
Several generic prescription medications might prove useful to treat a potential H5N1 avian flu outbreak, including statins, fibrates, and chloroquine.[33][34][35]
Nutritional supplements and herbal medicines
Malnutrition can reduce the ability of the body to resist infections and is a common cause of immunodeficiency in the developing world.[36] For instance, in a study in Ecuador, micronutrient deficiencies were found to be common in the elderly, especially for vitamin C, vitamin D, vitamin B-6, vitamin B-12, folic acid, and zinc, and these are thought to weaken the immune system or cause anemia and thus place people at greater risk of respiratory infections such as influenza.[37] Seasonal variation in sunlight exposure, which is required for vitamin D synthesis within the body, has been proposed as one of the factors accounting for the seasonality of influenza.[38] A meta-analysis of 13 studies indicated some support for adjunctive vitamin D therapy for influenza, but called for more rigorous clinical trials to settle the issue conclusively.[39]
A recent review discussing herbal and alternative medicines in influenza treatment details evidence suggesting that N-acetylcysteine, elderberry, or a combination of Eleutherococcus senticosus and Andrographis paniculata may help to shorten the course of influenza infection. The article cites more limited evidence including animal or in vitro studies to suggest possible benefit from vitamin C, DHEA, high lactoferrin whey protein, Echinacea spp., Panax quinquefolium, Larix occidentalis arabinogalactans, elenolic acid (a constituent of olive leaf extract), Astragalus membranaceus, and Isatis tinctoria or Isatis indigotica. [40] Another review assessed the quality of evidence for alternative influenza treatments, it concluded that there was "no compelling evidence" that any of these treatments were effective and that the available data on these products is particularly weak, with trials in this area suffering from many shortcomings, such as being small and poorly-designed and not testing for adverse effects.[41]
N-Acetylcysteine
The activity of N-acetylcysteine (NAC) against influenza was first suggested in 1966.[42] In 1997 a randomized clinical trial found that volunteers taking 1.2 grams of N-acetylcysteine daily for six months were as likely as those taking placebo to be infected by influenza, but only 25% of them experienced clinical symptoms, as contrasted with 67% of the control group. The authors concluded that resistance to flu symptoms was associated with a shift in cell mediated immunity from anergy toward normoergy, as measured by the degree of skin reactivity to seven common antigens such as tetanus and Candida albicans.[43]
Several animal studies found that in a mouse model of lethal infection with a high dose of influenza, oral supplementation with one gram of N-acetylcysteine per kilogram of body weight daily increased the rate of survival, either when administered alone or in combination with the antiviral drugs ribavirin or oseltamivir.[44][45][46] NAC was shown to block or reduce cytopathic effects in influenza-infected macrophages,[47] to reduce DNA fragmentation (apoptosis) in equine influenza-infected canine kidney cells,[48] and to reduce RANTES production in cultured airway cells in response to influenza virus by 18%.[49] The compound has been proposed for treatment of influenza.[50]
Elderberry
A few news reports have suggested the use of an elderberry (Sambucus nigra) extract as a potential preventative against the 2009 flu pandemic.[51][52][53][54] The preparation has been reported to reduce the duration of influenza symptoms by raising levels of cytokines.[55][56][57] However, the use of the preparation has been described as "imprudent" when an influenza strain causes death in healthy adults by cytokine storm leading to primary viral pneumonia.[58] The manufacturer cites a lack of evidence for cytokine-related risks, but labels the product only as an antioxidant and food supplement.[59]
"Kan Jang"
The mixture of Eleutherococcus senticosus ("Siberian ginseng") and Andrographis paniculata, sold under the trade name Kan Jang, was reported in the Journal of Herbal Pharmacotherapy to outperform amantadine in reducing influenza-related sick time and complications in a Volgograd pilot study of 71 patients in 2003.[60] Prior to this, an extract of Eleutherococcus senticosus was shown to inhibit replication of RNA but not DNA viruses in vitro.[61] Among nine Chinese medicinal herbs tested, Andrographis paniculata was shown to be most effective in inhibiting RANTES secretion by H1N1 influenza infected cells in cell culture, with an IC50 for the ethanol extract of 1.2 milligrams per liter.[62]
Green Tea
High dietary intake of green tea (specifically, catechins and theanine that is found in tea products) has been correlated with reduced risk of contracting influenza, as well as having an antiviral effect upon types A and B.[63][64][65] Specifically, the high levels of epigallocatechin gallate, epicatechin gallate, and epigallocatechin present in green tea were found to inhibit influenza virus replication.[66] Additionally, topical application has been suggested to possibly act as a mild disinfectant.[67] Regular dietary intake of green tea has been associated with stronger immune response to infection, through the enhancement of T-Cell function.[68]
Passive immunity
Transfused antibodies
An alternative to vaccination used in the 1918 flu pandemic was the direct transfusion of blood, plasma, or serum from recovered patients. Though medical experiments of the era lacked some procedural refinements, eight publications from 1918-1925 reported that the treatment could approximately halve the mortality in hospitalized severe cases with an average case-fatality rate of 37% when untreated.[69][70]
Bovine colostrum might also serve as a source of antibodies for some applications.[71]
Ex vivo culture of T lymphocytes
Human T lymphocytes can be expanded in vitro using beads holding specific antigens to activate the cells and stimulate growth. Clonal populations of CD8+ cytotoxic T cells have been grown which carry T cell receptors specific to influenza. These work much like antibodies but are permanently bound to these cells. (See cellular immunity). High concentrations of N-acetylcysteine have been used to enhance growth of these cells. This method is still in early research.[72][73]
References
- Montalto NJ, Gum KD, Ashley JV (December 2000). "Updated treatment for influenza A and B". Am Fam Physician. 62 (11): 2467–76. PMID 11130232.
- "Taking Care of Yourself: What to Do if You Get Sick with Flu". Disease and Conditions: Seasonal Flu. CDC. 2008-02-06. Archived from the original on 2019-01-04. Retrieved 2008-10-24.
- Stiver, Grant (2003). "The treatment of influenza with antiviral drugs". Canadian Medical Association Journal. 168: 49–57. PMC 139319 – via Pub Med.
- Smith, Nicole M.; Joseph S. Bresee; David K. Shay; Timothy M. Uyeki; Nancy J. Cox; Raymond A. Strikas (2006-07-28). "Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP)". Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. Retrieved 2007-05-25.
- Leneva, IA; Fediakina, IT; Gus'kova, TA; Glushkov, RG (2005). "[Sensitivity of various influenza virus strains to arbidol. Influence of arbidol combination with different antiviral drugs on reproduction of influenza virus A]". Терапевтический Архив (Therapeutic Archive). Moscow, Russia: ИЗДАТЕЛЬСТВО "МЕДИЦИНА". 77 (8): 84–88. PMID 16206613. Retrieved 2008-10-24.
- Shi L, Xiong H, He J, et al. (2007). "Antiviral activity of arbidol against influenza A virus, respiratory syncytial virus, rhinovirus, coxsackie virus and adenovirus in vitro and in vivo". Arch. Virol. 152 (8): 1447–55. doi:10.1007/s00705-007-0974-5. PMID 17497238.
- "Peramivir Fact Sheet" (PDF). BioCryst Pharmaceuticals Inc. Archived from the original (PDF) on 2007-05-07. Retrieved 2007-05-25.
- Sidwell RW, Smee DF (June 2002). "Peramivir (BCX-1812, RWJ-270201): potential new therapy for influenza". Expert Opin Investig Drugs. 11 (6): 859–69. doi:10.1517/13543784.11.6.859. PMID 12036429.
- Yun NE, Linde NS, Zacks MA, et al. (April 2008). "Injectable peramivir mitigates disease and promotes survival in ferrets and mice infected with the highly virulent influenza virus, A/Vietnam/1203/04 (H5N1)". Virology. 374 (1): 198–209. doi:10.1016/j.virol.2007.12.029. PMC 2680697. PMID 18234269.
- Bantia S, Arnold CS, Parker CD, Upshaw R, Chand P (January 2006). "Anti-influenza virus activity of peramivir in mice with single intramuscular injection". Antiviral Res. 69 (1): 39–45. doi:10.1016/j.antiviral.2005.10.002. PMID 16325932.
- "Life-Saving H1N1 Drug Unavailable to Most". CBS Evening News. Atlanta, GA, USA: CBS Interactive. 2009-10-19. Retrieved 2009-10-20.
- http://www.prnewswire.com/news-releases/emergency-use-authorization-granted-for-biocrysts-peramivir-65876107.html
- http://www.prnewswire.com/news-releases/fda-authorizes-emergency-use-of-intravenous-antiviral-peramivir-for-2009-h1n1-influenza-for-certain-patients-settings-65875662.html
- V.D. Solov'ev (1969). "The results of controlled observations on the prophylaxis of influenza with interferon" (PDF). Bulletin of the World Health Organization. 41 (3): 683–688. PMC 2427762. PMID 5309493.
- Joseph M. Cummins, DVM, Chad G. Thompson, BA (December 2004). "Low Dose Interferon, Immune Modulation and Emergency Influenza Prophylaxis". Pathobiologics International.CS1 maint: multiple names: authors list (link) - see also "Systemic effects of interferons after oral administration in animals and humans" (PDF). AJVR. 66 (1). January 2005.
- "Amarillo Biosciences Selects Accelovance for Its Next Influenza Study". MarketWire. 2009-05-20.
- Bracci L, Canini I, Venditti M, et al. (April 2006). "Type I IFN as a vaccine adjuvant for both systemic and mucosal vaccination against influenza virus". Vaccine. 24 (Suppl 2): S56–7. doi:10.1016/j.vaccine.2005.01.121. PMID 16823927.
- Launay O, Grabar S, Bloch F, et al. (July 2008). "Effect of sublingual administration of interferon-alpha on the immune response to influenza vaccination in institutionalized elderly individuals". Vaccine. 26 (32): 4073–9. doi:10.1016/j.vaccine.2008.05.035. PMID 18602725.
- "Russia through the prism of the world biopharmaceutical market" (PDF). Archived from the original (PDF) on 2012-02-24. Retrieved 2009-06-14.
- Gatich RZ, Kolobukhina LV, Vasil'ev AN, Isaeva EI, Burtseva EI, Orlova TG, Voronina FV, Kol'tsov VD, Malinovskaia VV (2008). "Viferon suppositories in the treatment of influenza in adults (article in Russian)". Antibiot Khimioter. 53 (3–4): 13–7. PMID 18942420.
- Kolobukhina LV, Malinovskaia VV, Gatich RZ, et al. (2008). "[Evaluation of the efficacy of wiferon and arbidol in adult influenza]". Vopr. Virusol. 53 (1): 31–3. PMID 18318133.
- "Clinical Investigations of Grippferon". Archived from the original on 2011-07-06. Retrieved 2009-07-04.
- "OPEN LETTER to: Director-General's office of the World Health Organization". February 2006. Archived from the original on 2011-07-06. Retrieved 2009-06-15.
- Venkataramanan Soundararajan; Kannan Tharakaraman; Rahul Raman; S. Raguram; Zachary Shriver; V. Sasisekharan; Ram Sasisekharan (9 June 2009). "Extrapolating from sequence — the 2009 H1N1 'swine' influenza virus". Nature Biotechnology. 27 (6): 510–3. doi:10.1038/nbt0609-510. PMID 19513050.
- Lynch JP, Walsh EE (April 2007). "Influenza: evolving strategies in treatment and prevention". Semin Respir Crit Care Med. 28 (2): 144–58. doi:10.1055/s-2007-976487. PMID 17458769.
- Bright RA, Medina MJ, Xu X, et al. (October 2005). "Incidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concern". Lancet. 366 (9492): 1175–81. doi:10.1016/S0140-6736(05)67338-2. PMID 16198766.
- Ilyushina NA, Govorkova EA, Webster RG (October 2005). "Detection of amantadine-resistant variants among avian influenza viruses isolated in North America and Asia" (PDF). Virology. 341 (1): 102–6. doi:10.1016/j.virol.2005.07.003. PMID 16081121.
- Parry J (July 2005). "Use of antiviral drug in poultry is blamed for drug resistant strains of avian flu". BMJ. 331 (7507): 10. doi:10.1136/bmj.331.7507.10. PMC 558527. PMID 15994677.
- Lackenby A, Thompson CI, Democratis J (December 2008). "The potential impact of neuraminidase inhibitor resistant influenza". Curr. Opin. Infect. Dis. 21 (6): 626–38. doi:10.1097/QCO.0b013e3283199797. PMID 18978531.
- Altman, Lawrence K. (2006-01-15). "This Season's Flu Virus Is Resistant to 2 Standard Drugs". New York Times. The New York Times Company. Retrieved 2007-05-25.
- "Cold and Flu Guidelines: Influenza". American Lung Association. Archived from the original on April 1, 2007. Retrieved 2007-09-16.
- Molotsky, Irvin (1986-02-15). "Consumer Saturday - Warning on Flu and Aspirin". New York Times. Retrieved 2007-05-25.
- D.S. Fedson (September 2008). "Confronting an influenza pandemic with inexpensive generic agents: can it be done?". The Lancet Infectious Diseases. 8 (9): 571–6. doi:10.1016/S1473-3099(08)70070-7. PMC 7128266. PMID 18420459.
- Fedson DS (July 2006). "Pandemic influenza: a potential role for statins in treatment and prophylaxis". Clin. Infect. Dis. 43 (2): 199–205. doi:10.1086/505116. PMID 16779747.
- Fedson DS, Dunnill P (2007). "Commentary: From scarcity to abundance: pandemic vaccines and other agents for "have not" countries". J Public Health Policy. 28 (3): 322–40. doi:10.1057/palgrave.jphp.3200147. PMID 17717543.
- Katona P, Katona-Apte J (May 2008). "The interaction between nutrition and infection". Clin. Infect. Dis. 46 (10): 1582–8. doi:10.1086/587658. PMID 18419494.
- Hamer DH, Sempértegui F, Estrella B, et al. (January 2009). "Micronutrient deficiencies are associated with impaired immune response and higher burden of respiratory infections in elderly Ecuadorians". J. Nutr. 139 (1): 113–9. doi:10.3945/jn.108.095091. PMC 2646211. PMID 19056665.
- Cannell JJ, Zasloff M, Garland CF, Scragg R, Giovannucci E (2008). "On the epidemiology of influenza". Virol. J. 5: 29. doi:10.1186/1743-422X-5-29. PMC 2279112. PMID 18298852.
- Yamshchikov AV, Desai NS, Blumberg HM, Ziegler TR, Tangpricha V (2009). "Vitamin D for treatment and prevention of infectious diseases: a systematic review of randomized controlled trials". Endocr Pract. 15 (5): 438–49. doi:10.4158/EP09101.ORR. PMC 2855046. PMID 19491064.
- Mario Roxas, ND and Julie Jurenka, MT (ASCP) (2007). "Colds and Influenza: A Review of Diagnosis and Conventional, Botanical, and Nutritional Considerations" (PDF). Alternative Medicine Review. 12 (1): 25–48. PMID 17397266. Archived from the original (PDF) on 2011-07-28. Retrieved 2009-06-13.CS1 maint: multiple names: authors list (link)
- Guo R, Pittler MH, Ernst E (November 2007). "Complementary medicine for treating or preventing influenza or influenza-like illness". Am. J. Med. 120 (11): 923–929.e3. doi:10.1016/j.amjmed.2007.06.031. PMID 17976414.
- Streightoff F, Redman CE, DeLong DC (1966). "In vivo antiviral chemotherapy. II. Anti-influenza action of compounds affecting mucous secretions". Antimicrob Agents Chemother. 6: 503–8. PMID 5985279.
- S. De Flora; C. Grassi; L. Carati (1997). "Attenuation of influenza-like symptomatology and improvement of cell-mediated immunity with long-term N-acetylcysteine treatment" (PDF). Eur Respir J. 10 (7): 1535–1541. doi:10.1183/09031936.97.10071535. PMID 9230243. (Open access article)
- Ungheri D, Pisani C, Sanson G, et al. (2000). "Protective effect of n-acetylcysteine in a model of influenza infection in mice". Int J Immunopathol Pharmacol. 13 (3): 123–128. PMID 12657201.
- Ghezzi P, Ungheri D (2004). "Synergistic combination of N-acetylcysteine and ribavirin to protect from lethal influenza viral infection in a mouse model". Int J Immunopathol Pharmacol. 17 (1): 99–102. doi:10.1177/039463200401700114. PMID 15000873.
- Garozzo A, Tempera G, Ungheri D, Timpanaro R, Castro A (2007). "N-acetylcysteine synergizes with oseltamivir in protecting mice from lethal influenza infection". Int J Immunopathol Pharmacol. 20 (2): 349–54. doi:10.1177/039463200702000215. PMID 17624247.
- Lowy RJ, Dimitrov DS (August 1997). "Characterization of influenza virus-induced death of J774.1 macrophages" (PDF). Exp. Cell Res. 234 (2): 249–58. doi:10.1006/excr.1997.3602. PMID 9260892.
- Saito T, Tanaka M, Yamaguchi I (November 1996). "Effect of brefeldin A on influenza A virus-induced apoptosis in vitro". J. Vet. Med. Sci. 58 (11): 1137–9. doi:10.1292/jvms.58.11_1137. PMID 8959666.
- Mugnier A, Manoha E, Drapier M (1976). "[Relation between the orofacial musculature and vertebral statics]". Orthod Fr. 47: 69–73. PMID 1070671.
- "N-acetylcysteine". Altern Med Rev. 5 (5): 467–71. October 2000. PMID 11056417.
- Kristin Chambers (2009-05-02). "2 flu cases found in state". Archived from the original on 2012-07-16. Retrieved 2009-06-13.
- La'Tasha Givens (2009-05-05). "Thomasville Residents Concerned About H1N1". WCTV News.
- Louis Cooper (2009-04-28). "No swine flu cases in state; officials on alert". Pensacola News-Journal.
- Matthew Stein (2009-04-28). "When a Super-Bug Strikes Close to Home, How Will You Deal With it?". Huffington Post.
- Barak, V; Halperin, T; Kalickman, I (June 2001). "The effect of Sambucol, a black elderberry-based, natural product, on the production of human cytokines: I. Inflammatory cytokines". European Cytokine Network. 12 (2): 290–296. PMID 11399518.
- Barak V, Birkenfeld S, Halperin T, Kalickman I (November 2002). "The effect of herbal remedies on the production of human inflammatory and anti-inflammatory cytokines". Isr Med Assoc J. 4 (11 Suppl): 919–922. PMID 12455180.
- "Elderberry Fights Flu Symptoms". WebMD. 2003-12-22.
- Jeffrey R. Ryan (2008). Pandemic Influenza. CRC Press. ISBN 978-1-4200-6087-4.
- "Sambucol FAQs". Manufacturer Web site. Archived from the original on 2009-07-25. Retrieved 2009-06-13.
- Kulichenko LL, Kireyeva LV, Malyshkina EN, Wikman G (2003). "A randomized, controlled study of Kan Jang versus amantadine in the treatment of influenza in Volgograd". J Herb Pharmacother. 3 (1): 77–93. doi:10.1080/j157v03n01_04. PMID 15277072.
- Glatthaar-Saalmüller B, Sacher F, Esperester A (June 2001). "Antiviral activity of an extract derived from roots of Eleutherococcus senticosus". Antiviral Res. 50 (3): 223–8. doi:10.1016/S0166-3542(01)00143-7. PMID 11397509.
- Ko HC, Wei BL, Chiou WF (September 2006). "The effect of medicinal plants used in Chinese folk medicine on RANTES secretion by virus-infected human epithelial cells". J Ethnopharmacol. 107 (2): 205–10. doi:10.1016/j.jep.2006.03.004. PMID 16621378.
- Matsumoto, K; Yamada, H; Takuma, N; Niino, H; Sagesaka, YM (2005). "Effects of green tea catechins and theanine on preventing influenza infection among healthcare workers: a randomized controlled trial". BMC Complement Altern Med. 11: 15. doi:10.1186/1472-6882-11-15. PMC 3049752. PMID 21338496.
- Park, M; Yamada, H; Matsushita, K; Kaji, S; Goto, T; Okada, Y; Kosuge, K; Kitagawa, T (2011). "Green tea consumption is inversely associated with the incidence of influenza infection among schoolchildren in a tea plantation area of Japan". J. Nutr. 141 (10): 1862–70. doi:10.3945/jn.110.137547. PMID 21832025.
- Imanishi, N; Tuji, Y; Katada, Y; Maruhashi, M; Konosu, S; Mantani, N; Terasawa, K; Ochiai, H (2002). "Additional inhibitory effect of tea extract on the growth of influenza A and B viruses in MDCK cells". Microbiol. Immunol. 46 (7): 491–4. doi:10.1111/j.1348-0421.2002.tb02724.x. PMID 12222936.
- Song, JM; Lee, KH; Seong, BL (2005). "Antiviral effect of catechins in green tea on influenza virus". Antiviral Research. 68 (2): 66–74. doi:10.1016/j.antiviral.2005.06.010. PMID 16137775.
- Shin, WJ; Kim, YK; Lee, KH; Seong, BL (2012). "Evaluation of the antiviral activity of a green tea solution as a hand-wash disinfectant". Biosci. Biotechnol. Biochem. 76 (3): 581–4. doi:10.1271/bbb.110764. PMID 22451404.
- Rowe, CA; Nantz, MP; Bukowski, JF; Percival, SS (2007). "Specific formulation of Camellia sinensis prevents cold and flu symptoms and enhances gamma, delta T cell function: a randomized, double-blind, placebo-controlled study". J Am Coll Nutr. 26 (5): 445–52. doi:10.1080/07315724.2007.10719634. PMID 17914132.
- Thomas C. Luke, MD, MTMH; Edward M. Kilbane, MD, MPH; Jeffrey L. Jackson, MD, MPH; and Stephen L. Hoffman, MD, DTMH (2006-10-17). "Meta-Analysis: Convalescent Blood Products for Spanish Influenza Pneumonia: A Future H5N1 Treatment?". Annals of Internal Medicine. 145 (8): 599–609. doi:10.7326/0003-4819-145-8-200610170-00139. PMID 16940336.CS1 maint: multiple names: authors list (link)
- Jeffrey R. Ryan (2008). Pandemic Influenza. CRC Press. ISBN 978-1-4200-6087-4.
- Korhonen H, Marnila P, Gill HS (November 2000). "Bovine milk antibodies for health". Br. J. Nutr. 84 Suppl 1: S135–46. PMID 11242458.
- Kalamasz D, Long SA, Taniguchi R, Buckner JH, Berenson RJ, Bonyhadi M (2004). "Optimization of human T-cell expansion ex vivo using magnetic beads conjugated with anti-CD3 and Anti-CD28 antibodies". J. Immunother. 27 (5): 405–18. doi:10.1097/00002371-200409000-00010. PMID 15314550.
- Boon AC, Vos AP, Graus YM, Rimmelzwaan GF, Osterhaus AD (January 2002). "In vitro effect of bioactive compounds on influenza virus specific B- and T-cell responses". Scand. J. Immunol. 55 (1): 24–32. doi:10.1046/j.1365-3083.2002.01014.x. PMID 11841689.
Further reading
- American Academy of Pediatrics Committee on Infectious Diseases (April 2008). "Prevention of influenza: recommendations for influenza immunization of children, 2007-2008". Pediatrics. 121 (4): e1016–31. doi:10.1542/peds.2008-0160. PMID 18381500.
- Andre FE, Booy R, Bock HL, et al. (February 2008). "Vaccination greatly reduces disease, disability, death and inequity worldwide". Bull. World Health Organ. 86 (2): 140–6. doi:10.2471/BLT.07.040089. PMC 2647387. PMID 18297169.
- Basta NE, Halloran ME, Matrajt L, Longini IM (December 2008). "Estimating influenza vaccine efficacy from challenge and community-based study data". Am. J. Epidemiol. 168 (12): 1343–52. doi:10.1093/aje/kwn259. PMC 2638553. PMID 18974084.CS1 maint: multiple names: authors list (link)
- Beigel J, Bray M (April 2008). "Current and future antiviral therapy of severe seasonal and avian influenza". Antiviral Res. 78 (1): 91–102. doi:10.1016/j.antiviral.2008.01.003. PMC 2346583. PMID 18328578.
- Hampson AW (June 2008). "Vaccines for pandemic influenza. The history of our current vaccines, their limitations and the requirements to deal with a pandemic threat" (PDF). Ann. Acad. Med. Singap. 37 (6): 510–7. PMID 18618064.
- Lipatov AS, Govorkova EA, Webby RJ, et al. (September 2004). "Influenza: emergence and control". J. Virol. 78 (17): 8951–9. doi:10.1128/JVI.78.17.8951-8959.2004. PMC 506949. PMID 15308692.
- Mossad SB (December 2008). "2008-2009 Influenza update: a better vaccine match". Cleve Clin J Med. 75 (12): 865–70. doi:10.3949/ccjm.75a.08088. PMID 19088005.
- Mossad SB (December 2007). "Influenza update 2007-2008: vaccine advances, pandemic preparation". Cleve Clin J Med. 74 (12): 889–94. doi:10.3949/ccjm.74.12.889. PMID 18183839.
- Nichols WG, Peck Campbell AJ, Boeckh M (April 2008). "Respiratory viruses other than influenza virus: impact and therapeutic advances". Clin. Microbiol. Rev. 21 (2): 274–90, table of contents. doi:10.1128/CMR.00045-07. PMC 2292575. PMID 18400797.
- Oshitani H, Kamigaki T, Suzuki A (June 2008). "Major issues and challenges of influenza pandemic preparedness in developing countries". Emerging Infect. Dis. 14 (6): 875–80. doi:10.3201/eid1406.070839. PMC 2600290. PMID 18507896.
- Sugrue RJ, Tan BH, Yeo DS, Sutejo R (June 2008). "Antiviral drugs for the control of pandemic influenza virus" (PDF). Ann. Acad. Med. Singap. 37 (6): 518–24. PMID 18618065.
- Tosh PK, Boyce TG, Poland GA (January 2008). "Flu myths: dispelling the myths associated with live attenuated influenza vaccine". Mayo Clin. Proc. 83 (1): 77–84. doi:10.4065/83.1.77. PMID 18174020.
- von Itzstein M (December 2007). "The war against influenza: discovery and development of sialidase inhibitors". Nat Rev Drug Discov. 6 (12): 967–74. doi:10.1038/nrd2400. PMID 18049471.
- Wu J, Yan P, Archibald C (2007). "Modelling the evolution of drug resistance in the presence of antiviral drugs". BMC Public Health. 7: 300. doi:10.1186/1471-2458-7-300. PMC 2148062. PMID 17953775.
External links
- Health-EU Portal EU response to influenza.
- European Commission - Public Health EU coordination on Pandemic (H1N1) 2009
- Flu treatment WebMD recommendations
- Influenza Merck Manual, February 2007