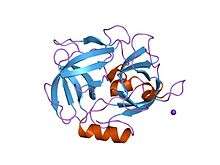
Glutamyl endopeptidase GluV8
Glutamyl endopeptidase (EC 3.4.21.19, SspA, V8 protease, GluV8, endoproteinase Glu-C, staphylococcal serine proteinase) is an extracellular bacterial serine protease of the glutamyl endopeptidase I family that was initially isolated from the Staphylococcus aureus strain V8. The protease is, hence, commonly referred to as "V8 protease", or alternatively SspA from its corresponding gene.[1][2][3]
| Glutamyl endopeptidase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 | |||||||||
| Identifiers | |||||||||
| EC number | 3.4.21.19 | ||||||||
| CAS number | 137010-42-5 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| |||||||||
Genetics
Glutamyl endopeptidase is in S. aureus expressed from the gene sspA within the operon ssp. Downstream of sspA, the operon also includes the genes of the cysteine protease staphopain B (sspB) and of staphostatin B (sspC; specific inhibitor of staphopain B).[4][5]
Glutamyl endopeptidase is largely co-expressed with the other major proteases of S. aureus: aureolysin, staphopain A, and staphopain B. The transcription of ssp, that occurs via a promoter controlled by "housekeeping" sigma factor σA, is up-regulated by accessory gene regulator agr, while it is repressed by staphylococcal accessory regulator sarA and by alternative sigma factor σB (a stress response modulator of Gram-positive bacteria). ssp expression is highly expressed in post-exponential growth phase.[4] A more complex network of modulators and of environmental conditions affecting ssp expression have been suggested, however.[6][7]
The sspA gene has a high prevalence in the genome of both commensal- and pathogenic-type S. aureus strains.[8]
Activation
Glutamyl endopeptidase is expressed as a zymogen that, in order to become fully active, has been modified both through autocatalysis and through cleavage by the metalloprotease aureolysin.[1][4][9]
Function
Glutamyl endopeptidase proteolytically activates the zymogen of the cysteine protease staphopain B (staphopain A is activated through and independent process).[10][11][12][10]
The bacterial protease has a narrow specificity, with a strict preference for catalyzing hydrolysis of proteins after negatively charged amino acids, especially glutamic acid, and to some extent aspartic acid.<Houmard J, Drapeau GR | title Staphylococcal protease: a proteolytic enzyme specific for glutamoyl bonds | journal = Proc Natl Acad Sci USA | volume = 69 | issue = 12 | pages = 3506-3509 | date = december 1972| pmid = 4509307 | doi = 10.1073/pnas.69.12.3506=":0" />[2]
Glutamyl endopeptidase has been shown to cleave certain target proteins among human inflammatory regulators and immune components. It can process kininogen into kinin, and cleave immunoglobulins. The protease also cleaves and inactivates α1-antitrypsin, but is successfully inhibited by α2-macroglubulin.[1] Glutamyl endopeptidase can inhibit the activation of targets within the complement system. It is indicated to cause inhibition to all three pathways of complement activation.[13]
Glutamyl endopeptidase can furthermore cleave a wide array bacterial surface proteins, including fibronectin-binding proteins and protein A, potentially acting as a self-regulatory mechanism.[14][15][16]
Biological significance
An immunization survey of human serum samples suggests that exposure to glutamyl endopeptidase is common, although a correlation to any specific type of infection could not be established.[8] The numerous targets of bacterial proteases, adding the complexity of other virulence factors and their genetic regulation, makes it difficult to attribute a specific role of the protease for the bacteria. In vivo trials with S. aureus with inactivation of ssp or sspA controlling glutamyl endopeptidase gives a contradictory picture for its importance, although it has shown impact for bacterial survival in human whole blood. It has been suggested, however, that the protease promotes S. aureus dissemination through cleavage of self-proteins and through kinin-induced vasodilation, simultaneously protecting against immunological responses, i.e. through corruption of the regulation of the complement system and of neutrophil-derived proteases.[1][13][17][18]
Glutamyl endopeptidase is indicated to participate in control and dissemination in bacterial biofilms.[19]
The protease can contribute to infection symptoms, e.g. pain and edema through increased vascular permeability by activating kinin.[1] De-regulation of neutrophil proteases through inactivation of α1-antitrypsin has been suggested as a potential cause of dysfunctional coagulation in sepsis.[20]
References
- Dubin G (2002-07-01). "Extracellular proteases of Staphylococcus spp". Biological Chemistry. 383 (7–8): 1075–86. doi:10.1515/BC.2002.116. PMID 12437090.
- Stennicke HR, Breddam K (2013-01-01). Rawlings ND, Salvesen G (eds.). Handbook of Proteolytic Enzymes. Academic Press. pp. 2534–2538. doi:10.1016/b978-0-12-382219-2.00561-5. ISBN 9780123822192.
- Birktoft JJ, Breddam K (1994). "Chapter 8: Glutamyl endopeptidases". Methods in Enzymology. 244. pp. 114–126. doi:10.1016/0076-6879(94)44010-7.
- Shaw L, Golonka E, Potempa J, Foster SJ (January 2004). "The role and regulation of the extracellular proteases of Staphylococcus aureus". Microbiology. 150 (Pt 1): 217–28. doi:10.1099/mic.0.26634-0. PMID 14702415.
- Filipek R, Rzychon M, Oleksy A, Gruca M, Dubin A, Potempa J, Bochtler M (October 2003). "The Staphostatin-staphopain complex: a forward binding inhibitor in complex with its target cysteine protease". The Journal of Biological Chemistry. 278 (42): 40959–66. doi:10.1074/jbc.M302926200. PMID 12874290.
- Oscarsson J, Tegmark-Wisell K, Arvidson S (October 2006). "Coordinated and differential control of aureolysin (aur) and serine protease (sspA) transcription in Staphylococcus aureus by sarA, rot and agr (RNAIII)". International Journal of Medical Microbiology. 296 (6): 365–80. doi:10.1016/j.ijmm.2006.02.019. PMID 16782403.
- Lindsay JA, Foster SJ (September 1999). "Interactive regulatory pathways control virulence determinant production and stability in response to environmental conditions in Staphylococcus aureus". Molecular & General Genetics. 262 (2): 323–31. doi:10.1007/s004380051090. PMID 10517329.
- Zdzalik M, Karim AY, Wolski K, Buda P, Wojcik K, Brueggemann S, Wojciechowski P, Eick S, Calander AM, Jonsson IM, Kubica M, Polakowska K, Miedzobrodzki J, Wladyka B, Potempa J, Dubin G (November 2012). "Prevalence of genes encoding extracellular proteases in Staphylococcus aureus - important targets triggering immune response in vivo". FEMS Immunology and Medical Microbiology. 66 (2): 220–9. doi:10.1111/j.1574-695X.2012.01005.x. PMID 22762789.
- Nickerson NN, Prasad L, Jacob L, Delbaere LT, McGavin MJ (November 2007). "Activation of the SspA serine protease zymogen of Staphylococcus aureus proceeds through unique variations of a trypsinogen-like mechanism and is dependent on both autocatalytic and metalloprotease-specific processing". The Journal of Biological Chemistry. 282 (47): 34129–38. doi:10.1074/jbc.M705672200. PMID 17878159.
- Nickerson N, Ip J, Passos DT, McGavin MJ (January 2010). "Comparison of Staphopain A (ScpA) and B (SspB) precursor activation mechanisms reveals unique secretion kinetics of proSspB (Staphopain B), and a different interaction with its cognate Staphostatin, SspC". Molecular Microbiology. 75 (1): 161–77. doi:10.1111/j.1365-2958.2009.06974.x. PMID 19943908.
- Rice K, Peralta R, Bast D, de Azavedo J, McGavin MJ (January 2001). "Description of staphylococcus serine protease (ssp) operon in Staphylococcus aureus and nonpolar inactivation of sspA-encoded serine protease". Infection and Immunity. 69 (1): 159–69. doi:10.1128/IAI.69.1.159-169.2001. PMC 97868. PMID 11119502.
- Massimi I, Park E, Rice K, Muller-Esterl W, Sauder D, McGavin MJ (November 2002). "Identification of a novel maturation mechanism and restricted substrate specificity for the SspB cysteine protease of Staphylococcus aureus". The Journal of Biological Chemistry. 277 (44): 41770–7. doi:10.1074/jbc.M207162200. PMID 12207024.
- Jusko M, Potempa J, Kantyka T, Bielecka E, Miller HK, Kalinska M, Dubin G, Garred P, Shaw LN, Blom AM (2014-01-01). "Staphylococcal proteases aid in evasion of the human complement system". Journal of Innate Immunity. 6 (1): 31–46. doi:10.1159/000351458. PMC 3972074. PMID 23838186.
- Karlsson A, Saravia-Otten P, Tegmark K, Morfeldt E, Arvidson S (August 2001). "Decreased amounts of cell wall-associated protein A and fibronectin-binding proteins in Staphylococcus aureus sarA mutants due to up-regulation of extracellular proteases". Infection and Immunity. 69 (8): 4742–8. doi:10.1128/IAI.69.8.4742-4748.2001. PMC 98560. PMID 11447146.
- McGavin MJ, Zahradka C, Rice K, Scott JE (July 1997). "Modification of the Staphylococcus aureus fibronectin binding phenotype by V8 protease". Infection and Immunity. 65 (7): 2621–8. PMC 175371. PMID 9199429.
- Kolar SL, Ibarra JA, Rivera FE, Mootz JM, Davenport JE, Stevens SM, Horswill AR, Shaw LN (February 2013). "Extracellular proteases are key mediators of Staphylococcus aureus virulence via the global modulation of virulence-determinant stability". MicrobiologyOpen. 2 (1): 18–34. doi:10.1002/mbo3.55. PMC 3584211. PMID 23233325.
- Potempa J, Pike RN (2009-01-01). "Corruption of innate immunity by bacterial proteases". Journal of Innate Immunity. 1 (2): 70–87. doi:10.1159/000181144. PMC 2743019. PMID 19756242.
- Koziel J, Potempa J (February 2013). "Protease-armed bacteria in the skin". Cell and Tissue Research. 351 (2): 325–37. doi:10.1007/s00441-012-1355-2. PMC 3560952. PMID 22358849.
- Chen C, Krishnan V, Macon K, Manne K, Narayana SV, Schneewind O (October 2013). "Secreted proteases control autolysin-mediated biofilm growth of Staphylococcus aureus". The Journal of Biological Chemistry. 288 (41): 29440–52. doi:10.1074/jbc.M113.502039. PMC 3795244. PMID 23970550.
- Potempa J, Watorek W, Travis J (October 1986). "The inactivation of human plasma alpha 1-proteinase inhibitor by proteinases from Staphylococcus aureus". The Journal of Biological Chemistry. 261 (30): 14330–4. PMID 3533918.
External links
- Staphylococcus aureus glutamyl+endopeptidase at the US National Library of Medicine Medical Subject Headings (MeSH)