Choking
Choking occurs when breathing is impeded by a constricted or obstructed throat or windpipe.[1] In some cases the air flow is completely blocked, in other cases some amount of air can pass to the lungs. Insufficient oxygen being delivered to the body will result in oxygen deprivation. Although oxygen stored in the blood and lungs can keep a person alive for several minutes after breathing stops,[2] this sequence of events can lead to death. Choking was the fourth most common cause of unintentional injury-related death in the US in 2011.[3]
| Choking | |
|---|---|
| Other names | Foreign body airway obstruction |
 | |
| A demonstration of abdominal thrusts on a person showing signs of choking | |
| Specialty | Emergency medicine |
Deaths from choking most often occur in the very young (children under 2 years old) and in the elderly (adults over 75 years).[1] Obstruction of the airway can occur at the level of the pharynx or the trachea. Foods that can adapt their shape to that of the pharynx (such as bananas, marshmallows, or gelatinous candies) can be a danger not just for children but for persons of any age.[4]
Choking is one type of airway obstruction, which includes any blockage of the air-conducting passages, including blockage due to tumors, swelling of the airway tissues, and compression of the laryngopharynx, larynx or vertebrate trachea in strangulation.
Cause
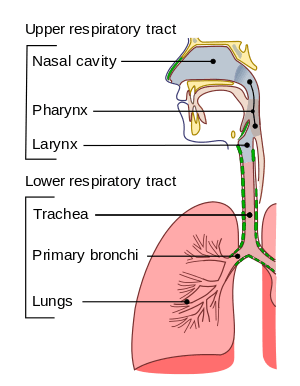
Choking is often caused by an object from outside the body, also called a foreign body, blocking the airway.[5] The object can block the upper or lower airway passages.[6] The airway obstruction is usually partial, but can also be complete.[6]
Among children, the most common causes of choking are food, coins, toys, and balloons.[5] In one study, peanuts were the most common object found in the airway of children evaluated for suspected foreign body aspiration.[7] Foods that pose a high risk of choking include hot dogs, hard candy, nuts, seeds, whole grapes, raw carrots, apples, popcorn, peanut butter, marshmallows, chewing gum, and sausages.[5] The most common cause of choking death in children is latex balloons.[5] Small, round non-food objects such as balls, marbles, toys, and toy parts are also associated with a high risk of choking death because of their potential to completely block a child's airway.[5]
Children younger than age three are especially at risk of choking because they explore their environment by putting objects in their mouth.[5] Also, young children are still developing the ability to chew food completely.[5] Molar teeth, which come in around 1.5 years of age, are necessary for grinding food.[5] Even after molar teeth are present, children continue developing the ability to chew food completely and swallow throughout early childhood.[5] In addition, a child's airway is smaller in diameter than an adult's airway, which means that smaller objects can cause an airway obstruction in children. Infants and young children generate a less forceful cough than adults, so coughing may not be as effective in relieving an airway obstruction.[5] Finally, children with neuromuscular disorders, developmental delay, traumatic brain injury, and other conditions that affect swallowing are at an increased risk of choking.[5]
In adults, choking often involves food blocking the airway.[8] Risk factors include using alcohol or sedatives, undergoing a procedure involving the oral cavity or pharynx, wearing oral appliances, or having a medical condition that causes difficulty swallowing or impairs the cough reflex.[8] Conditions that can cause difficulty swallowing and/or impaired coughing include neurological conditions such as strokes, Alzheimer's disease, or Parkinson's disease.[9] In older adults, risk factors also include living alone, wearing dentures, and having difficulty swallowing.[8]
Children and adults with neurological, cognitive, or psychiatric disorders may experience a delay in diagnosis because there may not be a known history of a foreign body entering the airway.[8]
Prevention
In choking, the time to react is quite short, and the worst cases are deadly. For these reasons, it is convenient to prevent it,[10][11][12] so it does not even happen.
Basic prevention
Choking typically happens when swallowing too large or too abundant mouthfuls that are badly chewed. This risk disappears when one obtains the discipline to split the food in pieces of moderated size, and to chew them completely, not swallowing them before. If a food can be chewed, it must be chewed, whatever it is, even if it is very soft or gelatinous, such as spreads and soft desserts. Eating in handfuls (it can happen with foods as popcorn, different peeled nuts, etc.), requires to chew with more control than normal, and not exceeding in the amounts that enter into the mouth. Having at hand some liquid to drink is useful to help to finish swallowing (before the choking has happened).To swallow well, it is recommended that the neck is in a normal position, straight for the eater's body, with the head looking forward, being seated or standing up (not lying or too reclined).
Dangerous foods
The foods that produce the most complicated choking are those whose shape adapts to the shape of the pharynx or trachea: hot dogs and sausages, bananas, food in blocks, etc. It is easier to choke on foods that dry the mouth (overcooked meat, sponge cake, cold pizza, etc.), which require the help of drinking liquid, or to be accompanied of purees or sauces. It is also easier to choke on foods that are tough (meat of octopus or cuttlefish, major size animals, some reptiles, etc.), they may need to be eaten together with something that helps the teeth to grind them (as loaf bread), or any concrete way to be prepared or cooked.
Groups of risk
Some population groups have a higher choking risk, as: the elderly, the children, the disabled (physically or mentally), people under the effects of alcohol or drugs, people who have taken medications that seriously reduce the ability to salivate or react, patients with difficulties to swallow (dysphagia), suicidal people, epileptics, people on the autism spectrum, individuals with disorders such as pica that lead them to consume inedible objects, etc. They may require more assistance to feed themselves and it may be necessary to supervise them while they eat. If they are unable to chew properly, their food can not be hard nor tough. If they have difficulty eating normally, it is not recommended to give them food that may cause issues, or to separate it into very small pieces. In cases where a person is unable to safely eat, food can be supplied by feeding syringes that pour a liquid content into the patient's mouth. If the problem is that they have taken any medication or substance that reduces saliva, they cannot eat solid food until their salivation is restored.
Prevention in babies and children
All little children require care in eating. They must learn to chew their food completely to avoid choking. Feeding them while they do another activity (when they run, play, laugh, etc.) increases the risk of choking. Caregivers can supervise children while eating or playing.[13] Providers such as pediatricians and dentists can provide information to parents and caregivers about what food and toys are appropriate by age to prevent choking.[5] The American Academy of Pediatricians recommends waiting until 6 months of age before introducing solid foods to infants.[14] Caregivers can avoid giving children, when they are younger than 5 years-old, foods that pose a high risk of choking such as hot dog pieces, bananas, cheese sticks, cheese chunks, hard candy, nuts, grapes, marshmallows or popcorn.[13] Later, when they are accustomed to these foods, it is normal to give them split into small pieces. For example: if they are going to eat hot dogs, it is possible to split the sausage lengthwise, sliced, or both. And the same in the case of bananas, grapes, grains, etc. Parents, teachers, child care providers and other caregivers for children are advised to be trained in choking first-aid and cardiopulmonary resuscitation (CPR).[5]
Children can put small objects into their mouths (deflated balloons, marbles, small pieces, buttons, coins, button batteries, etc.), which could lead to the child swallowing or choking on them. When babies choke on deflated balloons or plastic bags (as the sacks for wrapping the dirty diapers, the nappy sacks, which are a sort of bag sometimes dangerously placed near the babies),[15] it produces a complicated obstruction that would require it to be directly removed with the fingers, if it is visible. To prevent children from swallowing things, it is needed to take precautions on their environment by placing dangerous objects out of their reach. Besides, they must be supervised, paying enough attention to what they do. It is necessary to teach the children to avoid putting things into their mouths. They may try to eat small pieces of toys. Toys and games may indicate on their packages the ages for which they are safe. In the US, manufacturers of children's toys and products are required by law to apply appropriate warning labels to their packaging.[5] However, toys that are resold may not be marked with warning labels.[5] Caregivers can try to prevent choking by considering the features of a toy (such as size, shape, consistency, small parts) before giving it to a child.[5] Children's products that are found to pose a choking risk can be taken off the market.[5]
(How to recognize airway obstruction)
Symptoms, signs and times
Symptoms and signs:
- Difficulty or inability to speak or cry out.
- Inability or difficulty in breathing. Labored breathing, including gasping or wheezing, may be present.
- Violent and largely involuntary coughing, gurgling, or vomiting noises may be present.
- More serious choking victims will have a limited (if any) ability to produce these symptoms since they require at least some air movement.
- The person may begin clutching of the throat or mouth, or attempting to induce vomiting by putting fingers down the throat.
- The person's face turns blue (cyanosis) from lack of oxygen, if breathing is not restored.
- The person may become unconscious, if breathing is not restored.
Times:
- Brain damage typically occurs if the body is deprived of air for three minutes.
- Death will usually occur if breathing is not restored in six to eight minutes. Life can be extended some more by the use of cardiopulmonary resuscitation (CPR) on unconscious victims of choking (see more details further below).
Treatment
Choking is treated with a number of different procedures, which form the airway management. This consist in basic techniques available for first aiders and more advanced techniques available for health professionals.

Basic treatment (First-Aid)
Basic treatment of choking includes a number of non-invasive techniques to help remove foreign bodies from the airways. Most modern protocols, including those of the American Heart Association and the American Red Cross, recommend several stages, designed to apply increasingly more pressure. For the conscious choking victim, most protocols recommend encouraging the victim to cough, followed by hard back slaps and, if none of these things work, abdominal thrusts (Heimlich maneuver) or chest thrusts. Once the choking victims loses consciousness, initiating CPR is recommended.[16]
Cough
If the choking individual is conscious and coughing, the American Red Cross recommends encouraging the individual to stay calm and continue coughing freely, and it may be easier to take air through the nose to refill the lungs. If the person choking is unable to cough or if coughing is not effective, the American Red Cross recommends to move onto other methods, detailed below.[17]
_against_choking_for_adult_people.jpg)
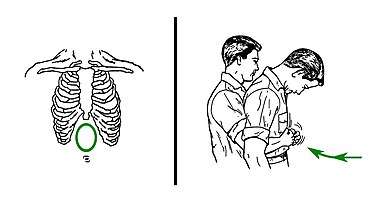
Back blows (Back slaps)
Many associations, as the American Red Cross and the Mayo Clinic, recommend the use of back blows (back slaps) to aid in the rescue of choking victims. This technique starts by bending the choking victim forward as much as possible, even trying to place his head lower than the chest, to avoid the risk of the slaps could drive the object deeper into the person's throat (that is a rare complication, but possible). The bending is in the back, the neck should not be excessively bent. Back blows are performed by delivering forceful slaps with the heel of the hand on the victim's back, between the shoulder blades.[18][19]
The back slaps push behind the blockage, being able to dislodge the foreign object. In some cases, the physical vibration of the action may cause enough movement of the object to assist the patient in clearing the airway.
Abdominal Thrusts (Heimlich Maneuver)
Abdominal thrusts[20] are performed with the rescuer standing behind the choking victim. The rescuer closes his skillful hand, grasps it with the other hand, and presses forcefully inwards and upwards with both of them on the area located between the chest and the belly button of the victim. The pressure is not focused directly against the ribs, to avoid breaking any of them. If the first thrust doesn't solve the choking, it can be repeated several times. Usage of abdominal thrusts is not recommended in infants under 1 year of age due to risk of causing injury; there exist adapted techniques for them (see more further below). Abdominal thrusts should not be used, either, when the patient's abdomen presents problems to receive them, like pregnancy or excessive size; then chest thrusts are advised (see further below).
The purpose of abdominal thrusts is to create a pressure capable to expel the object lodged upwards in the airway, relieving the obstruction. This method was discovered by Dr. Henry Heimlich in 1974, so it is referred to as "The Heimlich Maneuver." Dr. Henry Heimlich claimed that his maneuver was better than the back blows, arguing that back blows could cause the obstruction to become more deeply lodged in the victim's airway. That claim started a debate[21] into the medical community, that ended up with the recommendation of alternating both techniques, but making the patient to bend the back before receiving the slaps.[22][18][19] So the Heimlich Maneuver itself uses only abdominal thrusts, but is also part of anti-choking protocols that include the back blows (back slaps) technique.
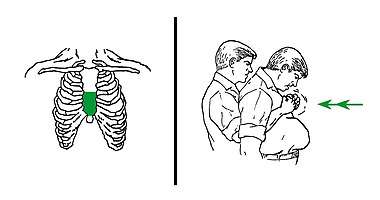
Chest thrusts
When abdominal thrusts can not be performed on the victim (in case of pregnant or too obese victims, and others) chest thrusts are advised instead.[23]
Chest thrusts are performed with the rescuer standing behind the choking victim. The rescuer closes his skillful hand and grasp it with the other hand. This can produce several kinds of fists, but any of them can be valid if it can be placed on the chest of the victim without sinking there a knuckle too painfully. Keeping the fist with both hands, the rescuer uses it to press forcefully inwards on the lower half of the chest bone (approximately), but not in the very endpoint (which is the xiphoid process). It can be noted, as a general reference, that, when the victim is a woman, the zone of pressure of the chest thrusts would be normally upper than the level of the breasts. The pressure is not focused against the xiphoid process, to avoid breaking it. If the first thrust doesn't solve the choking, it can be repeated several times.
"Five and Five" strategy
The American Red Cross recommends a protocol of alternating five back blows and five abdominal thrusts for conscious choking victims until the object blocking the airway is dislodged. For pregnant or too obese victims, the protocol is the same, but chest thrusts are advised instead of the abdominal ones. If the victim becomes unconscious, basic CPR is recommended.[17] Anyway, it's convenient to make someone call to emergency medical services before it happens.
The Red Cross does not specifically refer to its choking victim protocol as the "Five and Five Technique", and it differs from the Heimlich Maneuver since it includes administering back blows to the victim, contrary to Dr. Heimlich's procedure which specifically omitted back blows and was based only on his technique.
Anti-choking devices
During the 2010-2020 decade, some effective anti-choking devices have been developed and released to the market. They have superseded primitive inventions appeared during the 20th century. The current anti-choking devices have some advantages compared with manual techniques. The usage of these devices is always quite easy. They can be especially useful in difficult cases, like disabled patients, elderly people, unconscious victims or when the victim is oneself. Also, they can be helpful in public places and crowded events. And, finally, they achieve levels of pressure in suction that can not be matched by manual methods. In the worst choking cases, no manual technique would dislodge the foreign object, being necessary the usage of one of these devices or a sort of surgery. That's why physicians recommend to put some care in eating.
The design of these devices is based in a vacuum mechanical effect, with no need of batteries or electric current. They usually present an attached mask, in order to make a vacuum from the patient's nose and mouth. The current models of anti-choking devices are quite similar: a direct plunger tool (LifeVac),[24] or a vacuum syringe (backward syringe) that keeps the tongue in place by inserting a tube in the mouth (Dechoker).[25] Both have received certifications[26][27] and have been proven effective in many real cases reported by the media.[28][29] Some other mechanical models are in development, this is the case of Lifewand[30] (now being released to market), which makes the vacuum by direct pressure against patient's face, and the prototype of Dr. De Luca (now seeking funds ), which uses a button. The challenges for the future of the anti-choking inventions are just to improve their portability reducing more their size and to develop a device that specifically works in babies (despite all the previous ones have any model for little children).
Unconscious victims

When a choking victim becomes unconscious, it's mandatory to call to emergency medical services if this has not been done yet.

For the rest, an unconscious choking victim should receive a first-aid treatment that is similar to the case of any other non-breathing patient: a cardiopulmonary resuscitation (CPR), alternating series of around 30 compressions (on the lower half of the chest bone) with series of 2 rescue breaths (pinching the victim's nose and puffing air inside of the mouth; it's also possible to tilt the victim's head up or down and give 2 additional breaths, so the air could find an entrance through the blockage). The difference between CPR in choking victims and a normal CPR is that CPR in choking victims includes an attempt to remove the obstructing object (mainly using finger sweeping when the object is already visible) at the end of each compressions serie. The chest compressions of cardiopulmonary resuscitation (CPR) produce coincidentally the same anti-choking effect than the chest thrusts technique, so the CPR itself could expel the object. If the object is expelled and followingly removed, CPR must continue until the victim recovers breathing.[31] Babies (infants under 1 year old) require a special adaptation of the procedure (described further below).
An anti-choking device can unblock the airway on unconscious victims, but not necessarily can take the obstructing object out of the mouth (it may need a manual removal). Anyway, the victim will require cardiopulmonary resuscitation (CPR) after that, as it has been described above, but only alternating the 30 compressions and the 2 rescue breaths.
About the finger sweeping in unconscious victims
In unconscious victims of choking, the American Medical Association advocates sweeping the fingers across the back of the throat to attempt to dislodge airway obstructions.[32] However, many modern protocols recommend against the use of the finger sweep. Red Cross procedures specifically direct rescuers not to perform a finger sweep unless an object can be clearly seen in the victim's mouth due to the risk of driving the obstruction deeper into the victim's airway. Other protocols suggest that if the patient is conscious they will be able to remove the foreign object themselves, or if they are unconscious, the rescuer should simply place them in the recovery position as this allows (to a certain extent) the drainage of fluids out of the mouth instead of down the trachea due to gravity. There is also a risk of causing further damage (for instance inducing vomiting) by using a finger sweep technique. There are no studies that have examined the usefulness of the finger sweep technique when there is no visible object in the airway. Recommendations for the use of the finger sweep have been based on anecdotal evidence.[16]
In special populations
Babies (under 1 year old)
For babies (infants under 1 year old), the American Heart Association recommends[33] to perform cycles of back blows (5 back slaps) followed by chest thrusts (5 chest compressions, that are adapted).
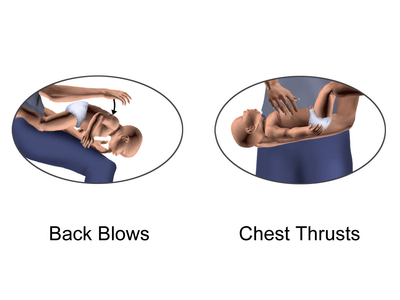
In the back blows, it's recommended that, before applying them, the baby is slightly leaned upside-down, being supported by a forearm of the rescuer and its respective hand (the baby's head must be carefully held in this maneuver, usually from the jaw). To achieve this position, the rescuer can sit down on any seat with the baby, so the baby's body (supported by the forearm and hand of the rescuer) can be leaned along the rescuer's thighs. As an alternative to this (in case of the baby is too big or any other problem), the rescuer can sit on a bed or sofa, or even on the floor (when no seat is near), supporting on the lap the baby's body, to make the upside-down leaning from the lap, at the right or at the left. If the rescuer can not sit down, at least could try to do the maneuver low over a soft surface (to reduce a possible fall). In case of the previous options are not possible, but the rescuer is skillful enough, the rescuer can still kneel on a knee, and place the baby's body along the thigh that is higher (with the forearm still supporting between the thigh and the baby), so the baby can be leaned a bit moving forward that thigh. When the baby is already leaned (using any of the systems), the rescuer applies the slaps.
In the chest thrusts maneuver, the baby's body is placed lying. Then the rescuer does the compressions on the chest bone, pressing with only two fingers on its lower half (the nearer to the abdomen). Abdominal thrusts are not recommended in children less than 1 year, because they can cause liver damage.[33]
The cycles of 5 back blows and 5 chest compressions are alternated until the object comes out of the infant's airway or until the infant becomes unconscious.[33]
If the infant becomes unconscious, the American Heart Association[33] recommends starting a cardiopulmonary resuscitation (CPR), which must be adapted to babies. In that procedure, the baby is placed face up on a horizontal surface, with the head in straight position (tilting too much a baby's head backwards can close the access to the trachea). Then it must be applied an alternating cycle of 30 chest compressions (but modified: the rescuer presses with only two fingers in the lower part of the chest bone), and 2 rescue breaths (also modified: the rescuer's mouth puffs air covering the baby's mouth and nose at the same time). Between chest compressions and rescue breaths, the rescuer looks into the mouth searching if the obstructing object has come out (because of the effect of the compressions) and, if it is visible, attempts to extract it (mainly using a finger sweeping). If the object is extracted, the cardiopulmonary resuscitation continues until the baby's breath is successfully recovered or until medical services arrive.
Pregnant or too obese people
The American Heart Association recommends the chest thrusts rather than the abdominal thrusts for pregnant or too obese persons who are choking.[16] Chest thrusts are performed in a similar way to the abdominal thrusts, but with the hands placed on the lower part of the choking victim's chest, at the lower half of the breast bone (sternum), rather than over the middle of the abdomen, as in the traditional abdominal thrusts. Strong inward thrusts are then applied.[18] As a reference, in women, the zone of pressure of the chest thrusts (the lower half of sternum) would be normally upper than the level of the breasts. The chest thrusts can be alternated with back blows (back slaps), which are applied on the back of the victim when it is very bent forward.
Disabled people in wheelchair
If the choking victim is a disabled person and is using a wheelchair, the first-aid procedure is quite similar than in the case of the other victims. The difference is in trying to apply the techniques directly, while the victim is still seated on the wheelchair.[34]
The back blows (back slaps) can be used after bending forward the back of the victim very much, as much as possible. To perform the abdominal thrusts (Heimlich maneuver), the back of the victim must be bent too, and the rescuer has to get behind the wheelchair. Then, the rescuer can embrace the victim's abdomen from behind and up, leaning over the top of the wheelchair's backrest. If this is too difficult, the rescuer can get down to embrace the victim's abdomen and the wheelchair's backrest all together. The same can be tried from a side or in another way. Finally, the rescuer has to apply the sudden inward and upward pressures on the abdomen. It must be remembered that, if the victim can not receive abdominal thrusts (this is the case of the pregnant or too obese people), chest thrusts must be used instead. They are applied while the victim is in the wheelchair too, but making sudden inward pressures on the lower part of the chest bone against the wheelchair's backrest and the rescuer's body. If there are difficulties for this, the same maneuver can be tried from a side or in another way.
Due to the additional difficulties in helping to the disabled, it is convenient to avoid placing them in too narrow and encased spaces at the mealtimes. The opened spaces give an easier access to them for the rescuers.
The presence of an anti-choking device at hand can be specially useful when a disabled person is near.
Self-treatment
The Heimlich Maneuver (abdominal thrusts) can be performed or can be self-administered. Self-administration of this maneuver requires positioning of one's own abdomen over a chair, railing, or countertop and driving the abdomen upon the object with sharp, upward thrust. This serves as a substitute for thrusts made with the hands by another person. One study showed that these self-administered abdominal thrusts were just as effective as those performed by another person, although obese individuals were not included in the study.[35] Alternatively, multiple sources of evidence suggest that one of promising approaches for self treatment during choking could be by applying the head-down (inverse) position.[16]
On the other hand, using a modern anti-choking device is one the best, and most realistic, options for self-treatment in case of suffering a serious choking episode.
Advanced treatment
There are many advanced medical treatments to relieve choking or airway obstruction. These include inspection of the airway with a laryngoscope or bronchoscope and removal of the object under direct vision. Severe cases where there is an inability to remove the object may require cricothyrotomy (emergency tracheostomy). Cricothyrotomy involves making an incision in a patient's neck and inserting a tube into the trachea in order to bypass the upper airways.[36] The procedure is usually only performed when other methods have failed. In many cases, an emergency tracheostomy can save a patient's life, but if performed incorrectly, it may end the patient's life.
Epidemiology
Choking is the fourth most common cause of unintentional injury-related death in the US.[3] Many episodes are not reported because they are brief and resolve without seeking medical attention.[5] Among reported events, the majority of episodes (80%) occur among children younger than age 15, with fewer episodes (20%) among age 15 and older.[3] The death rate from choking is low at most ages but increases starting around age 74.[3] Choking due to a foreign object resulted in 162,000 deaths (2.5 per 100,000) in 2013, compared to 140,000 deaths (2.9 per 100,000) in 1990.[37]
Notable cases
References
- National Safety Council. Research and Statistics Department. (2015). Injury facts (2015 ed.). Itasca, IL. ISBN 9780879123345. OCLC 910514461.
- Ross, Darrell Lee; Chan, Theodore C (2006). Sudden Deaths in Custody. ISBN 978-1-59745-015-7.
- "Injury Facts 2015 Edition" (PDF). National Safety Council. Archived from the original (PDF) on 26 September 2017. Retrieved 1 December 2017.
- Sayadi, Roya (May 2010). Swallow Safely: How Swallowing Problems Threaten the Elderly and Others (First ed.). Natick, MA: Inside/Outside Press. pp. 46–47. ISBN 9780981960128.
- Committee on Injury, Violence (2010-03-01). "Prevention of Choking Among Children". Pediatrics. 125 (3): 601–607. doi:10.1542/peds.2009-2862. ISSN 0031-4005. PMID 20176668.
- Dominic Lucia; Jared Glenn (2008). CURRENT Diagnosis & Treatment: Emergency Medicine. New York, NY: McGraw-Hill. ISBN 978-0-07-184061-3.
- Yadav, S. P.; Singh, J.; Aggarwal, N.; Goel, A. (September 2007). "Airway foreign bodies in children: experience of 132 cases". Singapore Medical Journal. 48 (9): 850–853. ISSN 0037-5675. PMID 17728968.
- Warshawsky, Martin (31 December 2015). "Foreign Body Aspiration". Medscape. Retrieved 1 December 2017.
- Boyd, Michael; Chatterjee, Arjun; Chiles, Caroline; Chin, Robert (2009). "Tracheobronchial Foreign Body Aspiration in Adults". Southern Medical Journal. 102 (2): 171–174. doi:10.1097/smj.0b013e318193c9c8. PMID 19139679.
- "Choking Prevention" (PDF). Arizona Department of Economic Security. Archived (PDF) from the original on 2017-10-31.
- Kramarow, Ellen; Warner, Margaret; Chen, Li-Hui (2014). "Food-related choking deaths among the elderly". Injury Prevention. 20 (3): 200–203. doi:10.1136/injuryprev-2013-040795. ISSN 1475-5785. PMID 24003082.
- "Choking is a leading cause of injury and death among children". ScienceDaily. Retrieved 2020-02-02.
- "Choking Prevention for Babies". Safe Kids Worldwide. Retrieved 2017-12-15.
- "Infant Food and Feeding". www.aap.org. Retrieved 2017-12-15.
- "Campaign Against Nappy Sacks". Royal Society for the Prevention of Accidents.
- "Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality – ECC Guidelines". eccguidelines.heart.org. Retrieved 4 December 2017.
- "STEP 3: Be Informed – Conscious Choking | Be Red Cross Ready". www.redcross.org. Retrieved 4 December 2017.
- "Choking: First aid". Mayo Clinic. Mayo Foundation for Medical Education and Research (MFMER). Retrieved 4 December 2017.
- "Conscious Choking" (PDF). American Red Cross. Archived (PDF) from the original on 2020-01-31.
- "First Aid Tips". Red Cross. Archived from the original on 2009-02-03.
- Mills Senn, Pamela (April 2007). "Cincinnati Magazine, April 2007, page 92".
- American Red Cross. "New First Aid and CPR/AED Training Programs". Archived from the original on 2006-04-29.
- "Choking and CPR safety talk". Oklahoma State University. Archived from the original on 2020-01-30.
- "How to use LifeVac". Lifevac.life. 2016-08-02. Retrieved 2020-01-20.
- Dechoker. "How to Use Dechoker Anti-Choking Device (ACD)". Dechoker. Retrieved 2020-01-20.
- "About LifeVac". Lifevac.life. 2016-08-02. Retrieved 2020-01-20.
- Dechoker. "Clinical Studies". Dechoker. Retrieved 2020-01-20.
- "Advocates say anti-choking device saved two lives in Idaho | Local | idahostatejournal.com". 2019-02-03. Archived from the original on 2019-02-03. Retrieved 2020-01-20.
- "Carers used suction device to save woman who choked on sausage". Worcester News. Retrieved 2020-01-20.
- "lifewand - keep kids safe". lifewand.com. Retrieved 2020-01-20.
- "Instructor's Corner". americanredcross.force.com. Retrieved 2020-01-19.
- American Medical Association (2009-05-05). American Medical Association Handbook of First Aid and Emergency Care. Random House. ISBN 978-1-4000-0712-7.
dislodge the object.
- Wilkins, Lippincott Williams & (2010-11-02). "Editorial Board". Circulation. 122 (18 suppl 3): S639. doi:10.1161/CIR.0b013e3181fdf7aa. ISSN 0009-7322.
- "Choking Awareness, wheelchair user" (PDF). Belfast Health and Social Care Trust.
- Pavitt MJ, Swanton LL, Hind M, et al. (12 April 2017). "Choking on a foreign body: a physiological study of the effectiveness of abdominal thrust manoeuvres to increase thoracic pressure". Thorax. 72 (6): 576–578. doi:10.1136/thoraxjnl-2016-209540. PMC 5520267. PMID 28404809.
- "What is a trahceostomy?". Retrieved 25 February 2014.
- GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
External links
| Classification |
|---|